Magnetic Resonance Imaging Measurement of Entorhinal Cortex in the Diagnosis and Differential Diagnosis of Mild Cognitive Impairment and Alzheimer’s Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. MRI Acquisition
2.3. MR Morphometric Image Analysis
2.4. Statistical Analyses
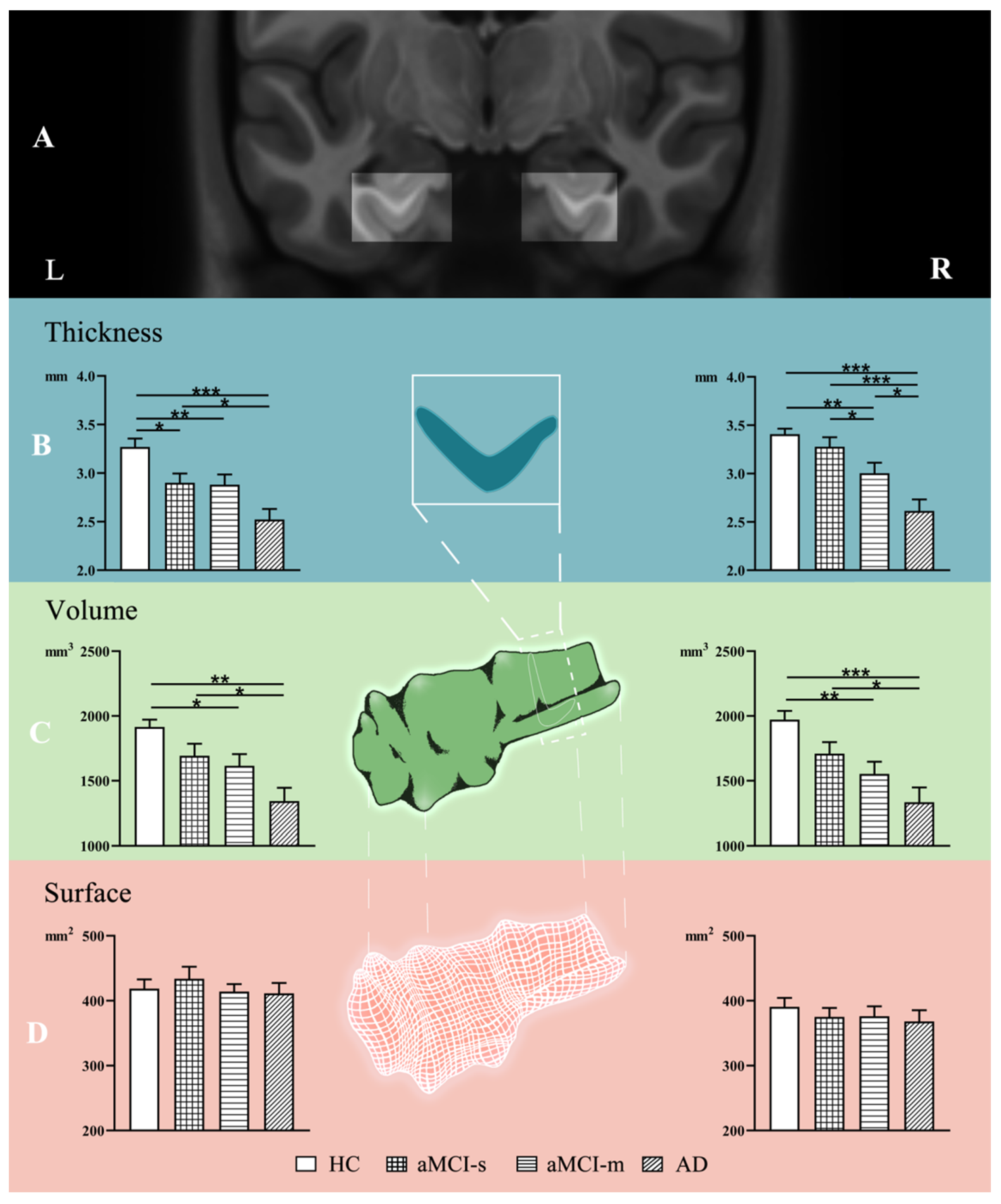
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mehta, D.; Jackson, R.; Paul, G.; Shi, J.; Sabbagh, M. Why do trials for Alzheimer’s disease drugs keep failing? A discontinued drug perspective for 2010–2015. Expert Opin. Investig. Drug 2017, 26, 735–739. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C.; Doody, R.; Kurz, A.; Mohs, R.; Morris, J.C.; Rabins, P.V.; Ritchie, K.; Rossor, M.; Thal, L.; Winblad, B. Current Concepts in Mild Cognitive Impairment. Arch. Neurol. 2001, 58, 1985–1992. [Google Scholar] [CrossRef]
- Lenzi, D.; Serra, L.; Perri, R.; Pantano, P.; Lenzi, G.L.; Paulesu, E.; Caltagirone, C.; Bozzali, M.; Macaluso, E. Single domain amnestic MCI: A multiple cognitive domains fMRI investigation. Neurobiol. Aging 2011, 32, 1542–1557. [Google Scholar] [CrossRef]
- McEvoy, L.K.; Fennema-Notestine, C.; Roddey, J.C.; Hagler, D.J.; Holland, D.; Karow, D.S.; Pung, C.J.; Brewer, J.B.; Dale, A.M. Alzheimer Disease: Quantitative Structural Neuroimaging for Detection and Prediction of Clinical and Structural Changes in Mild Cognitive Impairment. Radiology 2009, 251, 195–205. [Google Scholar] [CrossRef]
- Petersen, R.C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med. 2004, 256, 183–194. [Google Scholar] [CrossRef]
- Seo, S.W.; Im, K.; Lee, J.M.; Kim, Y.H.; Kim, S.T.; Kim, S.Y.; Yang, D.W.; Kim, S.I.; Cho, Y.S.; Na, D.L. Cortical thickness in single-versus multiple-domain amnestic mild cognitive impairment. Neuroimage 2007, 36, 289–297. [Google Scholar] [CrossRef]
- Ryu, S.Y.; Lim, E.Y.; Na, S.; Shim, Y.S.; Cho, J.H.; Yoon, B.; Hong, Y.J.; Yang, D.W. Hippocampal and entorhinal structures in subjective memory impairment: A combined MRI volumetric and DTI study. Int. Psychogeriatr. 2017, 29, 785–792. [Google Scholar] [CrossRef]
- Fjell, A.M.; Westlye, L.T.; Grydeland, H.; Amlien, I.; Espeseth, T.; Reinvang, I.; Raz, N.; Dale, A.M.; Walhovd, K.B. Accelerating Cortical Thinning: Unique to Dementia or Universal in Aging? Cereb. Cortex 2014, 24, 919–934. [Google Scholar] [CrossRef] [Green Version]
- Albert, M.S.; DeKosky, S.T.; Dickson, D.; Dubois, B.; Feldman, H.H.; Fox, N.C.; Gamst, H.; Holtzman, D.M.; Jagust, W.J.; Petersen, R.C.; et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement. 2011, 7, 270–279. [Google Scholar] [CrossRef] [Green Version]
- Zhou, M.; Zhang, F.; Zhao, L.; Qian, J.; Dong, C. Entorhinal cortex: A good biomarker of mild cognitive impairment and mild Alzheimer’s disease. Rev. Neurosci. 2016, 27, 185–195. [Google Scholar] [CrossRef]
- Khan, U.A.; Liu, L.; Provenzano, F.A.; Berman, D.E.; Profaci, C.P.; Sloan, R.; Mayeux, R.; Duff, K.E.; Small, S.A. Molecular drivers and cortical spread of lateral entorhinal cortex dysfunction in preclinical Alzheimer’s disease. Nat. Neurosci. 2014, 17, 304–311. [Google Scholar] [CrossRef] [Green Version]
- Hogstrom, L.J.; Westlye, L.T.; Walhovd, K.B.; Fjell, A.M. The Structure of the Cerebral Cortex Across Adult Life: Age-Related Patterns of Surface Area, Thickness, and Gyrification. Cereb. Cortex 2013, 23, 2521–2530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickerson, B.C.; Feczko, E.; Augustinack, J.C.; Pacheco, J.; Morris, J.C.; Fischl, B.; Buckner, R.L. Differential effects of aging and Alzheimer’s disease on medial temporal lobe cortical thickness and surface area. Neurobiol. Aging 2009, 30, 432–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sowell, E.R.; Thompson, P.M.; Leonard, C.M.; Welcome, S.E.; Kan, E.; Toga, A.W. Longitudinal Mapping of Cortical Thickness and Brain Growth in Normal Children. J. Neurosci. 2004, 24, 223–8231. [Google Scholar] [CrossRef]
- Li, C.; Wang, J.; Gui, L.; Zheng, J.; Liu, C.; Du, H. Alterations of Whole-Brain Cortical Area and Thickness in Mild Cognitive Impairment and Alzheimer’s Disease. J. Alzheimer’s Dis. 2011, 27, 281–290. [Google Scholar] [CrossRef]
- Salat, D.H.; Buckner, R.L.; Snyder, A.Z.; Greve, D.N.; Desikan, R.S.R.; Busa, E.; Morris, J.C.; Dale, A.M.; Fischl, B. Thinning of the Cerebral Cortex in Aging. Cereb. Cortex 2004, 14, 721–730. [Google Scholar] [CrossRef] [Green Version]
- Sun, P.; Lou, W.; Liu, J.; Shi, L.; Li, K.; Wang, D.; Mok, V.C.; Liang, P. Mapping the patterns of cortical thickness in single- and multiple-domain amnestic mild cognitive impairment patients: A pilot study. Aging 2019, 11, 10000–10015. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5™, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013; Volume 25, p. 191. [Google Scholar]
- Morris, J.C. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology 1993, 43, 2412–2414. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; Mchugh, P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Sunderland, T.; Hill, J.L.; Mellow, A.M.; Lawlor, B.A.; Grafman, J.H. Clock drawing in Alzheimer’s disease. A novel measure of dementia severity. J. Am. Geriatr. Soc. 1989, 37, 725–729. [Google Scholar] [CrossRef] [PubMed]
- Davids, A.; Goldenberg, L.; Laufer, M.W. The relation of the Archimedes spiral aftereffect and the trail making test to brain damage in children. J. Consult. Psychol. 1957, 21, 429. [Google Scholar] [CrossRef]
- Cheung, R.W.; Cheung, M.C.; Chan, A.S. Confrontation naming in Chinese patients with left, right or bilateral brain damage. J. Int. Neuropsychol. Soc. 2004, 10, 46–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, Q.; Zhao, Q.; Chen, M.; Ding, D.; Hong, Z. A Comparison Study of Mild Cognitive Impairment with 3 Memory Tests among Chinese Individuals. Alzheimer Dis. Assoc. Disord. 2009, 23, 253–259. [Google Scholar] [CrossRef]
- Enkirch, S.J.; Traschütz, A.; Müller, A.; Widmann, C.N.; Gielen, G.H.; Heneka, M.T.; Jurcoane, A.; Schild, H.H.; Hattingen, E. The ERICA Score: An MR Imaging-based Visual Scoring System for the Assessment of Entorhinal Cortex Atrophy in Alzheimer Disease. Radiology 2018, 288, 226–333. [Google Scholar] [CrossRef]
- Guzman, V.A.; Carmichael, O.T.; Schwarz, C.; Tosto, G.; Zimmerman, M.E.; Brickman, A.M. White matter hyperintensities and amyloid are independently associated with entorhinal cortex volume among individuals with mild cognitive impairment. Alzheimer’s Dement. 2013, 9, S124–S131. [Google Scholar] [CrossRef] [Green Version]
- Du, A.T.; Schuff, N.; Chao, L.L.; Kornak, J.; Weiner, M.W. Age effects on atrophy rates of entorhinal cortex and hippocampus. Neurobiol. Aging 2006, 27, 733–740. [Google Scholar] [CrossRef] [Green Version]
- Du, A.T.; Schuff, N.; Kramer, J.H.; Ganzer, S.; Zhu, X.P.; Jagust, W.J.; Miller, B.L.; Reed, B.R.; Mungas, D.; Yaffe, K.; et al. Higher atrophy rate of entorhinal cortex than hippocampus in AD. Neurology 2004, 62, 422–427. [Google Scholar] [CrossRef]
- Du, A.T.; Schuff, N.; Zhu, X.P.; Jagust, W.J.; Miller, B.L.; Reed, B.R.; Kramer, J.H.; Mungas, D.; Yaffe, K.; Chui, H.C.; et al. Atrophy rates of entorhinal cortex in AD and normal aging. Neurology 2003, 60, 481–486. [Google Scholar] [CrossRef] [Green Version]
- Busse, A.; Hensel, A.; Guhne, U.; Angermeyer, M.C.; Riedel-Heller, S.G. Mild cognitive impairment: Long-term course of four clinical subtypes. Neurology 2006, 67, 2176–2185. [Google Scholar] [CrossRef]
- Long, J.M.; Perez, E.J.; Roberts, J.A.; Roberts, M.T.; Rapp, P.R. Reelin in the Years: Decline in the number of reelin immunoreactive neurons in layer II of the entorhinal cortex in aged monkeys with memory impairment. Neurobiol. Aging 2020, 87, 132–137. [Google Scholar] [CrossRef]
- Panizzon, M.S.; Fennema-Notestine, C.; Eyler, L.T.; Jernigan, T.L.; Prom-Wormley, E.; Neale, M.; Jacobson, K.; Lyons, M.J.; Grant, M.D.; Franz, C.E.; et al. Distinct Genetic Influences on Cortical Surface Area and Cortical Thickness. Cereb. Cortex 2009, 19, 2728–2735. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Yuan, X.; Pu, F.; Li, D.; Fan, Y.; Wu, L.; Chao, W.; Chen, N.; He, Y.; Han, Y. Abnormal Changes of Multidimensional Surface Features Using Multivariate Pattern Classification in Amnestic Mild Cognitive Impairment Patients. J. Neurosci. 2014, 34, 10541–10553. [Google Scholar] [CrossRef] [Green Version]
- Huttenlocher, P.R. Morphometric study of human cerebral cortex development. Neuropsychologia 1990, 28, 517–527. [Google Scholar] [CrossRef]
- Feczko, E.; Augustinack, J.C.; Fischl, B.; Dickerson, B.C. An MRI-based method for measuring volume, thickness and surface area of entorhinal, perirhinal, and posterior parahippocampal cortex. Neurobiol. Aging 2009, 30, 420–431. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pennanen, C.; Kivipelto, M.; Tuomainen, S.; Hartikainen, P.; Hänninen, T.; Laakso, M.P.; Hallikainen, M.; Vanhanen, M.; Nissinen, A.; Helkala, E.L.; et al. Hippocampus and entorhinal cortex in mild cognitive impairment and early AD. Neurobiol. Aging 2004, 25, 303–310. [Google Scholar] [CrossRef]
- Gomez-Isla, T.; Price, J.L.; McKeel, D.J.; Morris, J.C.; Growdon, J.H.; Hyman, B.T. Profound loss of layer II entorhinal cortex neurons occurs in very mild Alzheimer’s disease. J. Neurosci. 1996, 16, 4491–4500. [Google Scholar] [CrossRef]
- Cox, S.R.; Bastin, M.E.; Ritchie, S.J.; Dickie, D.A.; Liewald, D.C.; Muñoz Maniega, S.; Redmond, P.; Royle, N.A.; Pattie, A.; Valdés Hernández, M.; et al. Brain cortical characteristics of lifetime cognitive ageing. Brain Struct. Funct. 2018, 223, 509–518. [Google Scholar] [CrossRef] [Green Version]
- Rajah, M.N.; Wallace, L.M.K.; Ankudowich, E.; Yu, E.H.; Swierkot, A.; Patel, R.; Chakravarty, M.M.; Naumova, D.; Pruessner, J.; Joober, R.; et al. Family history and APOE4 risk for Alzheimer’s disease impact the neural correlates of episodic memory by early midlife. NeuroImage Clin. 2017, 14, 760–774. [Google Scholar] [CrossRef]
- Schmid, N.S.; Taylor, K.I.; Foldi, N.S.; Berres, M.; Monsch, A.U. Neuropsychological Signs of Alzheimer’s Disease 8 Years Prior to Diagnosis. J. Alzheimer’s Dis. 2013, 34, 537–546. [Google Scholar] [CrossRef] [Green Version]
- Hirni, D.I.; Kivisaari, S.L.; Sabine, K.; Monsch, A.U.; Manfred, B.; Fatma, O.; Julia, R.; Stephan, U.; Kressig, R.W.; Christoph, S. Neuropsychological Markers of Medial Perirhinal and Entorhinal Cortex Functioning are Impaired Twelve Years Preceding Diagnosis of Alzheimer’s Dementia. J. Alzheimer’s Dis. 2016, 52, 573–580. [Google Scholar] [CrossRef] [Green Version]
- Devanand, D.P.; Bansal, R.; Liu, J.; Hao, X.; Pradhaban, G.; Peterson, B.S. MRI hippocampal and entorhinal cortex mapping in predicting conversion to Alzheimer’s disease. Neuroimage 2012, 60, 1622–1629. [Google Scholar] [CrossRef] [Green Version]
- Stoub, T.R.; Rogalski, E.J.; Leurgans, S.; Bennett, D.A.; DeToledo-Morrell, L. Rate of entorhinal and hippocampal atrophy in incipient and mild AD: Relation to memory function. Neurobiol. Aging 2010, 31, 1089–1098. [Google Scholar] [CrossRef] [Green Version]
- Devanand, D.P.; Pradhaban, G.; Liu, X.; Khandji, A.; De Santi, S.; Segal, S.; Rusinek, H.; Pelton, G.H.; Honig, L.S.; Mayeux, R. Hippocampal and entorhinal atrophy in mild cognitive impairment: Prediction of Alzheimer disease. Neurology 2007, 68, 828–836. [Google Scholar] [CrossRef]
- Braak, H.; Braak, E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 1991, 4, 239–259. [Google Scholar] [CrossRef]
- Safont, G.; Salazar, A.; Vergara, L. Multiclass Alpha Integration of Scores from Multiple Classifiers. Neural Comput. 2019, 31, 806–825. [Google Scholar] [CrossRef]
| AD Mean (SD) | aMCI-m Mean (SD) | aMCI-s Mean (SD) | HC Mean (SD) | p Value | |
|---|---|---|---|---|---|
| Gender (Females/Males) | 11/7 | 10/12 | 14/15 | 15/11 | 0.69 # |
| Age | 70.94 (9.77) | 71.09 (8.41) | 71.21 (6.48) | 70.38 (5.36) | 0.979 * |
| Education (years) | 7.06 (3.69) | 10.32 (3.72) | 8.07 (3.85) | 12.19 (3.26) | <0.001 * |
| MMSE | 15.89 (7.05) | 24.45 (4.04) | 24.07 (3.47) | 28.19 (1.47) | <0.001 * |
| MoCA | 11.56 (5.35) | 20.36 (4.47) | 19.45 (4.24) | 26.58 (1.70) | <0.001 * |
| AVLT | 12.06 (7.21) | 29.50 (11.12) | 27.14 (5.74) | 48.08 (9.29) | <0.001 * |
| CDR (0, 0.5, 1–2) | 0.5 = 1, 1–2 = 17 | 0.5 = 22 | 0.5 = 29 | 0 = 26 | <0.001 # |
| BNT | 11.94 (6.26) | 23.36 (2.15) | 27.76 (1.35) | 28.96 (0.96) | <0.001 * |
| TMT | 260.89 (49.53) | 114.09 (29.88) | 79.55 (23.35) | 86.27 (34.51) | <0.001 * |
| CDT (0, 1, 2, 3) | 2 = 6, 1 = 7, 0 = 5 | 1 = 6, 2 = 9, 3 = 7 | 2 = 5, 3 = 24 | 2 = 1, 3 = 25 | <0.001 # |
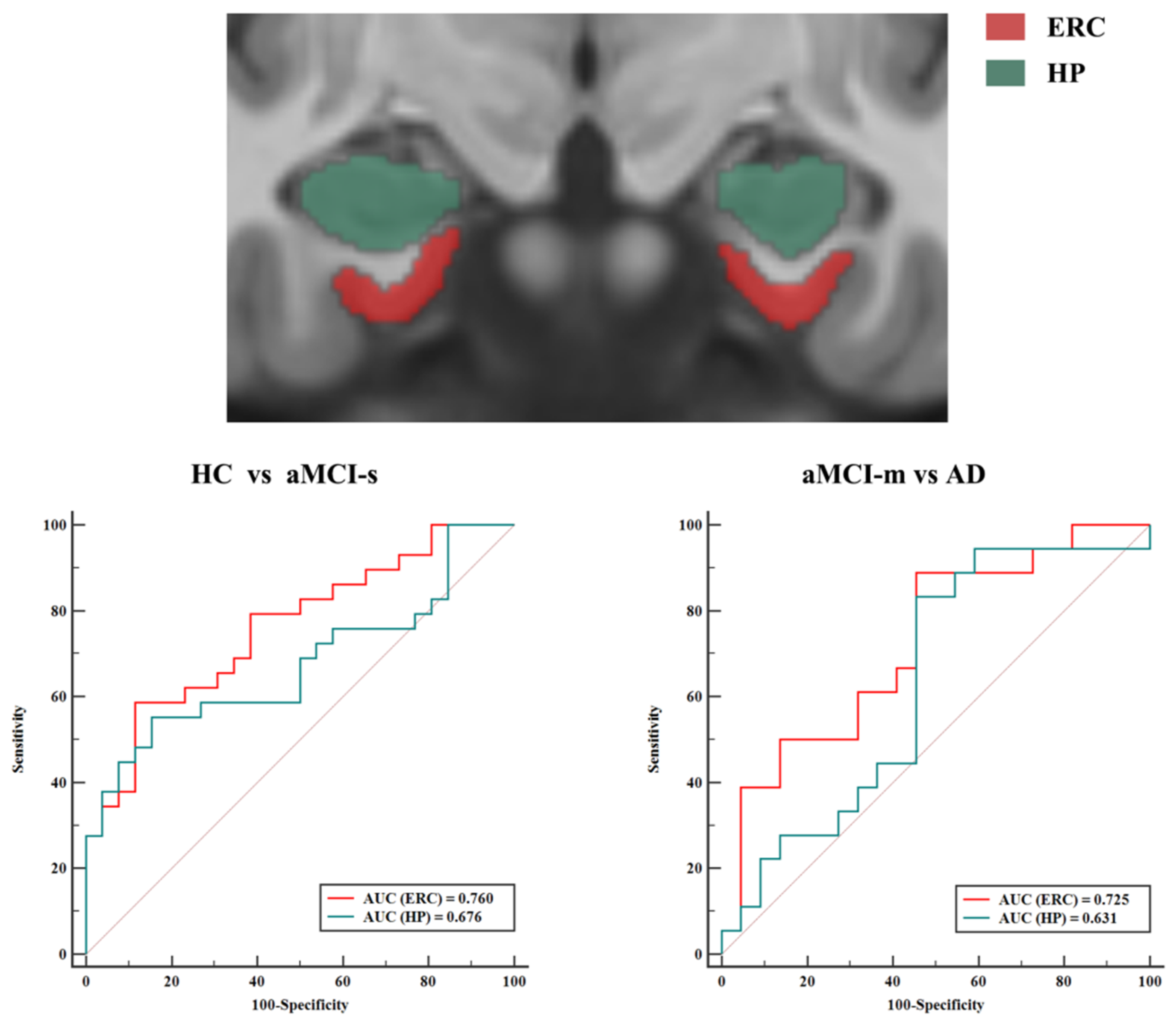
| Right Thickness | Left Thickness | Combined Thickness and Volume | |
|---|---|---|---|
| HC vs. aMCI-s | 0.558 | 0.711 | 0.760 |
| HC vs. aMCI-m | 0.736 | 0.729 | 0.788 |
| HC vs. AD | 0.908 | 0.876 | 0.919 |
| aMCI-s vs. aMCI-m | 0.647 | 0.505 | 0.687 |
| aMCI-s vs. AD | 0.824 | 0.711 | 0.833 |
| aMCI-m vs. AD | 0.694 | 0.707 | 0.725 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Q.; Wang, J.; Liu, J.; Wang, Y.; Li, K. Magnetic Resonance Imaging Measurement of Entorhinal Cortex in the Diagnosis and Differential Diagnosis of Mild Cognitive Impairment and Alzheimer’s Disease. Brain Sci. 2021, 11, 1129. https://doi.org/10.3390/brainsci11091129
Li Q, Wang J, Liu J, Wang Y, Li K. Magnetic Resonance Imaging Measurement of Entorhinal Cortex in the Diagnosis and Differential Diagnosis of Mild Cognitive Impairment and Alzheimer’s Disease. Brain Sciences. 2021; 11(9):1129. https://doi.org/10.3390/brainsci11091129
Chicago/Turabian StyleLi, Qianqian, Junkai Wang, Jianghong Liu, Yumeng Wang, and Kuncheng Li. 2021. "Magnetic Resonance Imaging Measurement of Entorhinal Cortex in the Diagnosis and Differential Diagnosis of Mild Cognitive Impairment and Alzheimer’s Disease" Brain Sciences 11, no. 9: 1129. https://doi.org/10.3390/brainsci11091129
APA StyleLi, Q., Wang, J., Liu, J., Wang, Y., & Li, K. (2021). Magnetic Resonance Imaging Measurement of Entorhinal Cortex in the Diagnosis and Differential Diagnosis of Mild Cognitive Impairment and Alzheimer’s Disease. Brain Sciences, 11(9), 1129. https://doi.org/10.3390/brainsci11091129





