The Anterior Attentional–Intentional System in Patients with Parkinson’s Disease—A Pilot and Feasibility Study
Abstract
:1. Introduction
- (1)
- Feasibility of recruitment
- (1a)
- What percentage of eligible patients and their caregivers consent to participate in the study?
- (1b)
- What percentage of patients drop out after neurological examination and before neuropsychological assessment?
- (1c)
- Do PD patients differ in willingness to participate based on disease severity?
- (1d)
- What percentage of the comparison group (CG; who volunteered to participate in the study) meet the inclusion criteria?
- (2)
- Feasibility of study procedures
- (2a)
- What percentage of the patients with PD are able to complete all planned neuropsychological procedures?
- (3)
- Preliminary data
- (3a)
- Do patients diagnosed with PD-NC and PD-MCI demonstrate deterioration in energization compared with the CG?
- (3b)
- Do patients diagnosed with PD-NC and PD-MCI demonstrate deterioration in monitoring compared with the CG?
- (3c)
- Do patients diagnosed with PD-NC and PD-MCI demonstrate deterioration in energization compared with the CG?
2. Materials and Methods
2.1. Study Design
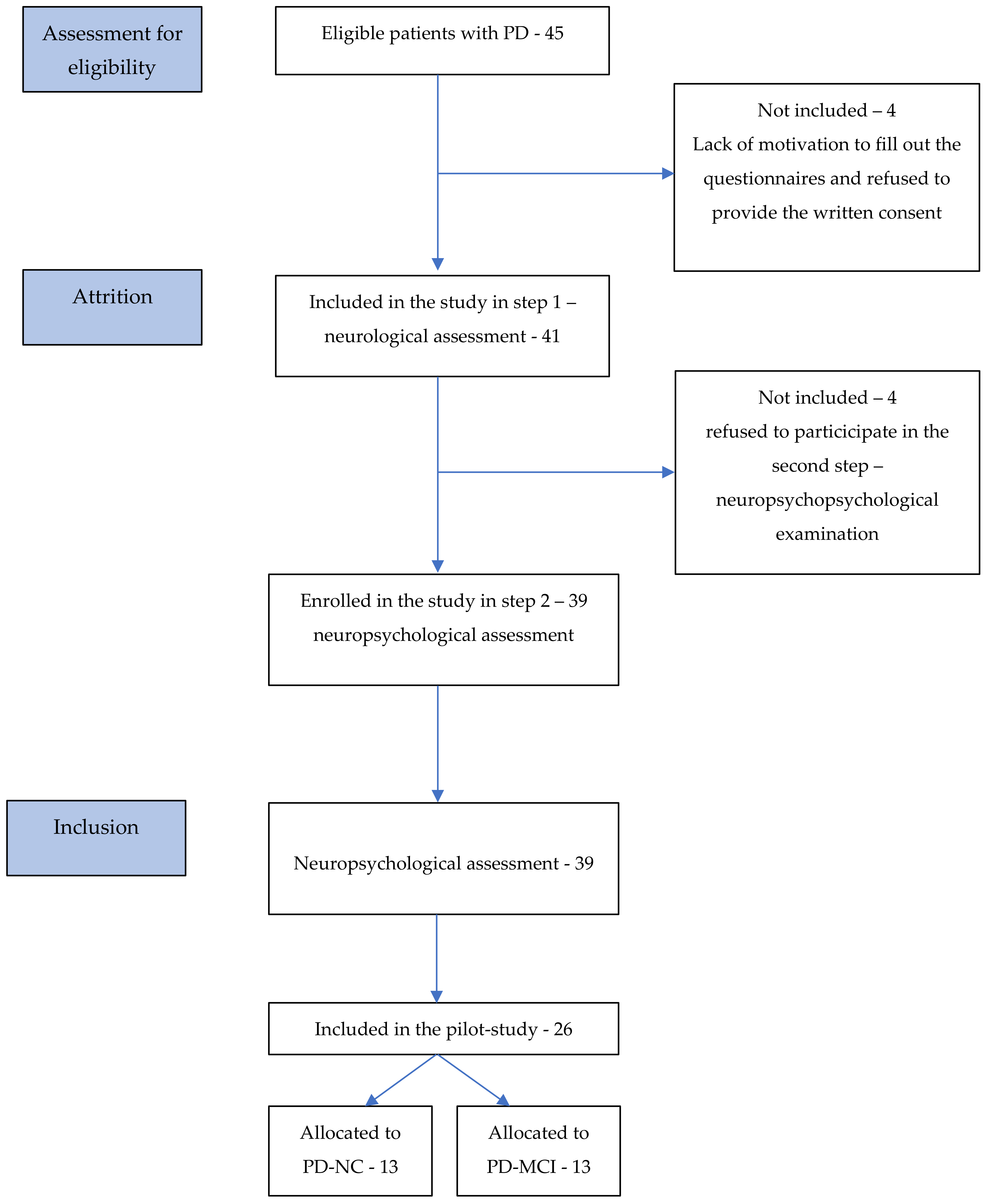
2.2. Participants and Setting
2.2.1. Participants from Clinical Groups
2.2.2. Participants from the Comparison Group
2.3. Study Procedures
2.3.1. Clinical Group
2.3.2. Comparison Group
2.4. Data Collection and Outcome Measures
2.4.1. Feasibility Data
2.4.2. Preliminary Data
The ROtman–Baycrest Battery for Investigating Attention (ROBBIA)
2.5. Statistical Analyses
3. Results
3.1. Study Characteristics
3.1.1. Feasibility Data
3.1.2. Preliminary Data
3.2. Results of Feasibility and Pilot Study
3.2.1. Feasibility Data Results in Terms of Study Procedures
3.2.2. Preliminary Data Results
Energization Results
Monitoring Results
Task-Setting Results
4. Discussion
4.1. Feasibility Data
4.2. Preliminary Data
4.3. Limitations and Strengths
Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tysnes, O.B.; Storstein, A. Epidemiology of Parkinson’s disease. J. Neural Transm. 2017, 124, 901–905. [Google Scholar] [CrossRef]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- Pfeiffer, H.C.; Løkkegaard, A.; Zoetmulder, M.; Friberg, L.; Werdelin, L. Cognitive impairment in early-stage non-demented Parkinson’s disease patients. Acta Neurol. Scand. 2014, 129, 307–318. [Google Scholar] [CrossRef]
- Xu, J.; Zhang, J.; Wang, J.; Li, G.; Hu, Q.; Zhang, Y. Abnormal fronto-striatal functional connectivity in Parkinson’s disease. Neurosci. Lett. 2016, 613, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Kudlicka, A.; Clare, L.; Hindle, J.V. Executive Functions in Parkinson’s Disease: Systematic Review and Meta-Analysis. Mov. Disord. 2011, 26, 2305–2315. [Google Scholar] [CrossRef]
- Stuss, D.T.; Shallice, T.; Alexander, M.P.; Piction, T.W. A multidisciplinary approach to anterior attentional functions. Ann. N. Y. Acad. Sci. 1995, 769, 191–211. [Google Scholar] [CrossRef] [PubMed]
- Vallesi, A.; Shallice, T.; Walsh, V. Role of the prefrontal cortex in the foreperiod effect: TMS evidence for dual mechanisms in temporal preparation. Cereb. Cortex 2007, 17, 466–474. [Google Scholar] [CrossRef] [Green Version]
- Stuss, D.T.; Alexander, M.P. Is there a dysexecutive syndrome? Philos. Trans. R. Soc. 2007, 62, 901–915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vallesi, A. Organisation of executive functions: Hemispheric asymmetries. J. Cogn. Psychol. 2012, 24, 367–386. [Google Scholar] [CrossRef]
- Stuss, D.T.; Alexander, M.P.; Shallice, T.; Piction, T.W.; Binns, M.A.; Macdonald, R.; Katz, D.I. Multiple frontal system controlling response speed. Neuropsychologia 2005, 43, 369–417. [Google Scholar] [CrossRef] [PubMed]
- Alexander, G.E.; DeLong, M.R.; Strick, P.L. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu. Rev. Neurosci. 1986, 9, 357–381. [Google Scholar] [CrossRef]
- De Long, M.; Wichmann, T. Update on models of basal ganglia function and dysfunction. Parkinsonism Relat. Disord. 2014, 15 (Suppl. S3), S237–S240. [Google Scholar] [CrossRef] [Green Version]
- Henri-Bhargava, A.; Stuss, D.T.; Freedman, M. Clinical Assessment of Prefrontal Lobe Functions. Continuum 2018, 24, 704–726. [Google Scholar] [CrossRef] [PubMed]
- Litva, I.; Goldman, J.G.; Tróster, A.I.; Schmand, B.A.; Weintraub, D.; Petersen, R.C.; Mollenhauer, B.; Adler, C.H.; Marder, K.; Williams-Gray, C.H.; et al. Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement Disorder Society. Task Force guidelines. Mov. Disord. 2012, 27, 349–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomlinson, C.L.; Stowe, R.; Patel, S.; Rick, C.; Gray, R.; Clarke, C.E. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 2010, 25, 2649–2653. [Google Scholar] [CrossRef] [PubMed]
- Schrag, A.; Barone, P.; Brown, R.G.; Leentjens, A.F.G.; McDonald, W.M.; Starkstein, S.; Weintraub, D.; Poewe, W.; Rascol, O.; Sampaio, C.; et al. Depression rating scales in Parkinson’s disease: Critique and recommendations. Mov. Disord. 2007, 22, 1077–1092. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Folstein, M.F.; Folstein, S.F.; McHugh, P.R. “Mini Mental State”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Harciarek, M.; Williamson, J.B.; Biedunkiewicz, B.; Lichodziejewska-Niemierko, M.; Dębska-Ślizień, A.; Rutkowski, B. Risk Factors for Selective Cognitive Decline in Dialyzed Patients with End-Stage Renal Disease: Evidence from Verbal Fluency Analysis. J. Int. Neuropsychol. 2012, 18, 162–167. [Google Scholar] [CrossRef]
- Brzeziński, J.; Gaul, M.; Hornowska, E.; Machowski, A.; Zakrzewska, M. Polish Adaptation of the Wechsler Intelligence Scale-Revised for Adults; Psychological Test; Laboratory of the Polish Psychological Association: Warsaw, Poland, 1991. (In Polish) [Google Scholar]
- Caffara, P.; Vezzadini, G.; Dieci, F.; Zonato, F.; Venneri, A. Rey-Osterrieth complex figure: Normative values in an Italian population sample. J. Neurol. Sci. 2002, 22, 443–447. [Google Scholar] [CrossRef]
- Peirce, J.W.; Gray, J.R.; Simpson, S.; MacAskill, M.R.; Höchenberger, R.; Sogo, H.; Kastman, E.; Lindeløv, J. PsychoPy2: Experiments in behavior made easy. Behav. Res. Methods 2019, 51, 195–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harciarek, M.; Michałowski, J.; Biedunkiewicz, B.; Wiliamson, J.; Dębska-Ślizień, A.; Rutkowski, B.; Heilman, K.M. Disorders of the anterior attentional-intentional system in patients with end stage renal disease: Evidence from reaction time studies. Brain Cogn. 2016, 107, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Minsterova, A.S.; Klobusiakova, P.; Pies, A.; Galaz, Z.; Mekyska, J.; Novakova, L.; Nemcova Elfmarkova, N.; Rektorova, I. Patterns of diffusion kurtosis changes in Parkinson’s subtypes. Parkinsonism Relat. Disord. 2020, 81, 96–102. [Google Scholar] [CrossRef]
- Yang, J.; Pourzinal, D.; McMahon, K.L.; Byrne, G.J.; Copland, D.A.; O’Sullivan, J.D.; Dissanayaka, N.N. Neural correlates of attentional deficits in Parkinson’s disease patients with mild cognitive impairment. Parkinsonism Relat. Disord. 2021, 85, 17–22. [Google Scholar] [CrossRef]
- Berman, B.D.; Smucny, J.; Wylie, K.P.; Shelton, E.; Kronberg, E.; Leehey, M.; Tregellas, J.R. Levodopa Modulates Small-World Architecture of Functional Brain Networks in Parkinson’s Disease. Mov. Disord. 2016, 31, 77–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zgaljardic, D.J.; Borod, J.C.; Foldi, N.S.; Mattis, P. A Review of the Cognitive and Behavioral Sequelae of Parkinson’s Disease: Relationship to Frontostriatal Circuitry. Cog. Behav. Neurol. 2003, 16, 193–210. [Google Scholar] [CrossRef] [PubMed]

| ROBBIA Subtest | Variables | Hypothesized Component Process |
|---|---|---|
| Simple Reaction Time (task 1) | Reaction time | Energizing |
| Change in reaction time in relation to interstimulus intervals (ISI) | Monitoring | |
| Choice Reaction Time (task 2) | Reaction time (especially in relation to the Prepare RT task) | Energizing |
| Change in reaction time in relation to ISI | Monitoring | |
| Total number of errors | Monitoring | |
| Relation of false-positive to false-negative errors | Task setting | |
| Prepare Reaction Time (tasks 3 and 4) | Reaction time (especially in relation to the Choice RT task) | Energizing |
| Total number of errors | Monitoring | |
| Relation of false-positive to false-negative errors | Task setting |
| PD-NC | D-MCI | Comparison Group | Comparison Statistics | |
|---|---|---|---|---|
| M (SD)/n (%) Range | ||||
| Age | 62.62 (5.94) 52–71 | 67.77 (5.48) 60–79 | 65.54 (7.37) 51–74 | F(2,36) = 2.18, p = 0.128 |
| Gender (Male) | 5 (38.5%) | 6 (46.2%) | 6 (42.2%) | χ2(1) = 0.21, p = 0.901 |
| Education level Primary Lower Secondary Upper Secondary Bachelor’s or equivalent Master’s or equivalent | 0 0 7 (53.8%) 1 (7.7%) 5 (38.5%) | 1 (7.7%) 2 (15.4%) 7 (53.8%) 1 (7.7%) 2 (15.4%) | 0 0 7 (53.8%) 1 (7.7%) 5 (38.5%) | H(2) = 4.32, p = 0.115 |
| Geriatric Depression Scale | 8.15 (7.03) 0–19 | 9.85 (4.79) 2–16 | 7.46 (4.79) 1–15 | F(2,36) = 0.62, p = 0.546 |
| PD duration (months) | 93.54 (70.08) 9–288 | 83.92 (65.20) 13–252 | - | t(24) = 0.28, p = 0.779 |
| Total daily Levodopa dose | 1019.62 (795.82) 280–2600 | 948.46 (429.36) 350–1740 | - | t(24) = 0.36, p = 0.720 |
| Hoehn and Yahr stage | χ2(3) = 8.11, p = 0.044 | |||
| Stage 0 | 1 (7.7%) | 0 | - | |
| Stage I | 7 (53.8%) | 2 (15.4%) | - | |
| Stage II | 5 (38.5%) | 7 (53.8%) | - | |
| Stage III | 0 | 4(30.8%) | - | |
| Side of onset | χ2(2) = 0.90, p = 0.638 | |||
| Left | 6 (46.2%) | 4 (30.8%) | - | |
| Right | 4 (30.8%) | 4 (30.8%) | - | |
| Bilateral | 3 (23.1%) | 5 (38.5%) | - | |
| PD-NC | PD-MCI | Comparison Group | Comparison Statistics | |
|---|---|---|---|---|
| M(SD) | ||||
| Mini-MentalState Examination | 28.38 (1.71) 25–30 | 27.62 (2.14) 23–30 | 28.77 (1.68) 27–30 | F(2,36) = 1.64, p = 0.208 |
| Phonemic fluency | 15.54 (4.43) 8–22 | 11.92 (5.50) 5–27 | 15.31 (4.70) 9–26 | F(2,36) = 2.22, p = 0.123 |
| Semantic fluency | 21.54 (3.07) 18–28 | 17.85 (4.63) 10–27 | 22.15 (3.48) 12–25 | F(2,36) = 4.92, p = 0.013 |
| Rey Complex Figure-copy | 33.73 (2.09) 31–36 | 29.08 (5.51) 20–35 | 34.85 (2.54) 27–36 | F(2,36) = 8.87, p = 0.001 |
| Rey Complex Figure-recall | 17.62 (8.41) 2–30 | 11.27 (7.27) 0–24.5 | 16.88 (4.91) 11–30 | F(2,36) = 3.18, p = 0.053 |
| Rey Complex Figure—percent recall score | 52.13 (24.40) 5.88–89.60 | 37.48 (20.53) 0–70 | 48.86 (14.90) 34–91.67 | F(2,36) = 1.86, p = 0.170 |
| CVLT-TOTAL 1 | 52.08 (12.52) 27–72 | 42.31 (9.60) 25–57 | 50.54 (8.33) 38–63 | F(2,36) = 3.38, p = 0.045 |
| CVLT-TOTALREP 2 | 5.00 (7.77) 0–29 | 3.85 (4.08) 0–13 | 1.92 (1.85) 0–6 | F(2,36) = 1.17, p = 0.321 |
| CVLT-LDFR 3 | 10.77 (3.39) 5–16 | 7.69 (3.35) 1–12 | 10.46 (3.15) 5–15 | F(2,36) = 3.43, p = 0.043 |
| CVLT-LDFRREP 4 | 0.69 (1.18) 0–4 | 0.46 (0.52) 0–1 | 0.23 (0.46) 0–1 | F(2,36) = 1.12, p = 0.338 |
| CVLT-RECOG 5 | 15.38 (0.96) 13–16 | 13.69 (2.84) 6–16 | 14.62 (1.98) 10–16 | F(2,36) = 2.17, p = 0.129 |
| CVLT-RECOGFALS 6 | 2.85 (2.34) 0–6 | 4.38 (4.15) 0–14 | 1.31 (1.93) 0–7 | F(2,36) = 3.49, p = 0.041 |
| Digit span 7 | 11.62 (1.76) 9–15 | 9.31 (2.21) 6–14 | 10.46 (2.54) 7–15 | F(2,36) = 3.60, p = 0.038 |
| PD-NC | PD-MCI | Comparison Group | |
|---|---|---|---|
| M (SD) | |||
| Simple RT | 453 (54) | 584 (198) | 442 (95) |
| Choice | 734 (94) | 876 (272) | 776 (115) |
| Prepare (1 s) | 650 (89) | 828 (350) | 686 (128) |
| Prepare (3 s) | 724 (130) | 848 (247) | 728 (64) |
| Reaction times in short and long ISI across studied groups | |||
| Simple RT task | |||
| Short ISI | 498 (68) | 630 (224) | 450 (91) |
| Long ISI | 420 (91) | 524 (175) | 433 (102) |
| Choice RT task | |||
| Short ISI | 728 (83) | 893 (260) | 781 (183) |
| Long ISI | 744 (119) | 868 (269) | 778 (125) |
| PD-NC | PD-MCI | Comparison Group | |
|---|---|---|---|
| M (SD) | |||
| Choice | 0.85 (0.99) | 1.08 (1.00) | 1.31 (1.03) |
| Prepare (1 s) | 0.92 (1.04) | 5.25 (9.23) | 0.85 (0.90) |
| Prepare (3 s) | 0.69 (0.85) | 1.92 (1.44) | 1.00 (1.29) |
| Number of false-negative and false-positive errors | |||
| Choice RT task | |||
| False positive | 0.46 (0.52) | 0.23 (0.60) | 0.54 (0.52) |
| False negative | 0.39 (0.65) | 0.69 (1.03) | 0.77 (0.93) |
| Prepare RT task with 1 s warning interval | |||
| False positive | 0.46 (0.78) | 2.00 (4.34) | 0.38 (0.65) |
| False negative | 0.46 (0.77) | 2.00 (4.04) | 0.46 (0.88) |
| Prepare RT task with 3 s warning interval | |||
| False positive | 0.31 (0.75) | 0.58 (0.51) | 0.31 (0.63) |
| False negative | 0.38 (0.65) | 1.08 (1.24) | 0.54 (0.66) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Golińska, P.B.; Sawicki, A.J.; Bieleninik, Ł.; Bidzan, M. The Anterior Attentional–Intentional System in Patients with Parkinson’s Disease—A Pilot and Feasibility Study. Brain Sci. 2021, 11, 1013. https://doi.org/10.3390/brainsci11081013
Golińska PB, Sawicki AJ, Bieleninik Ł, Bidzan M. The Anterior Attentional–Intentional System in Patients with Parkinson’s Disease—A Pilot and Feasibility Study. Brain Sciences. 2021; 11(8):1013. https://doi.org/10.3390/brainsci11081013
Chicago/Turabian StyleGolińska, Paulina Beata, Artur Józef Sawicki, Łucja Bieleninik, and Mariola Bidzan. 2021. "The Anterior Attentional–Intentional System in Patients with Parkinson’s Disease—A Pilot and Feasibility Study" Brain Sciences 11, no. 8: 1013. https://doi.org/10.3390/brainsci11081013
APA StyleGolińska, P. B., Sawicki, A. J., Bieleninik, Ł., & Bidzan, M. (2021). The Anterior Attentional–Intentional System in Patients with Parkinson’s Disease—A Pilot and Feasibility Study. Brain Sciences, 11(8), 1013. https://doi.org/10.3390/brainsci11081013







