Influence of Pain and Discomfort in Stroke Patients on Coping Strategies and Changes in Behavior and Lifestyle
Abstract
1. Introduction
2. Materials and Methods
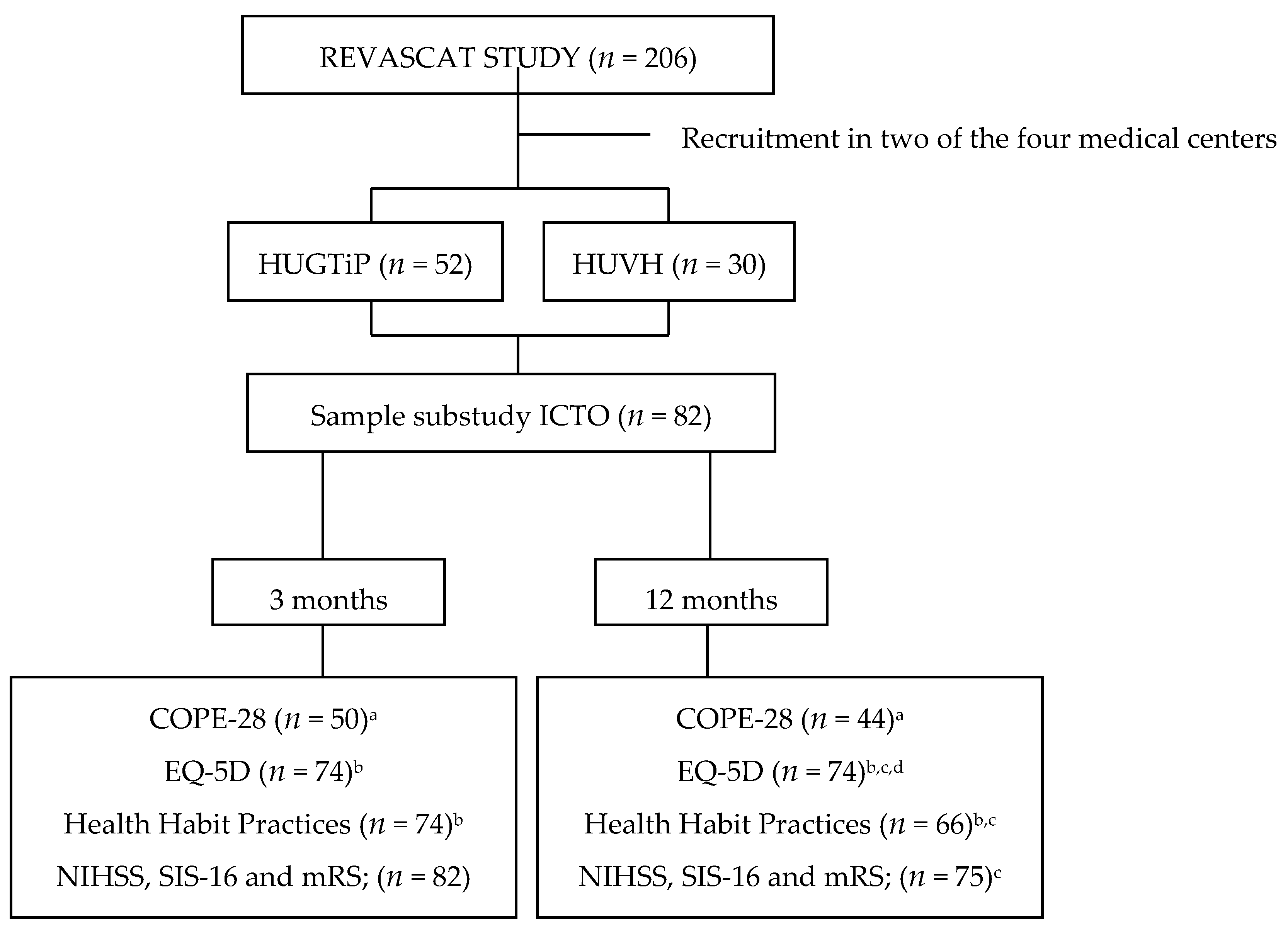
2.1. Study Design
2.2. Patients
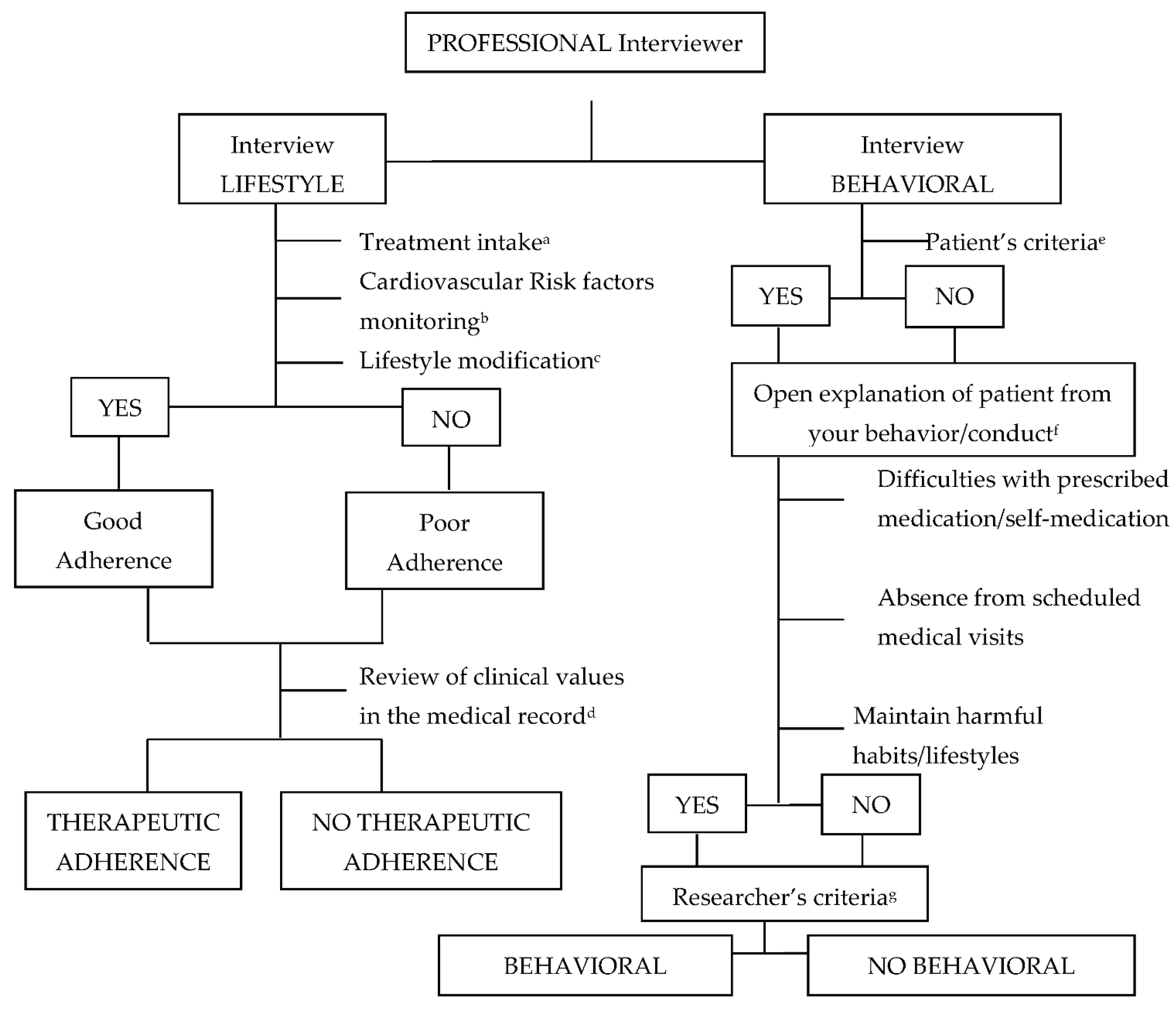
2.3. Data Collection
2.4. Analysis
2.5. Ethical Considerations
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guzik, A.; Bushnell, C. Stroke Epidemiology and Risk Factor Management. Contin. Lifelong Learn. Neurol. 2017, 23, 15–39. [Google Scholar] [CrossRef]
- García, R.C.; Guillem, F.C.; Seco, E.M.; Puente, J.M.G.; Arango, J.S.J.; Manent, J.I.R.; Arango, J.S.J.; Cantera, C.M.; Muñoz, M.J.; Santiago, A.L. Recomendaciones sobre el estilo de vida. Aten. Primaria 2018, 50, 29–40. [Google Scholar] [CrossRef]
- Pandian, J.D.; Gall, S.L.; Kate, M.P.; Silva, G.S.; Akinyemi, R.O.; Ovbiagele, B.I.; Lavados, P.M.; Gandhi, D.B.C.; Thrift, A.G. Prevention of stroke: A global perspective. Lancet 2018, 392, 1269–1278. [Google Scholar] [CrossRef]
- Cabrera, A.; Gustavo, A. El modelo transteórico del comportamiento en salud. Rev. Fac. Nac. Salud Pública 2000, 18, 129–138. [Google Scholar]
- Suñer-Soler, R.; Grau, A.; Gras, M.E.; Font-Mayolas, S.; Silva, Y.; Dávalos, A.; Cruz, V.; Rodrigo, J.; Serena, J. Smoking cessation 1 year poststroke and damage to the insular cortex. Stroke 2012, 43, 131–136. [Google Scholar] [CrossRef]
- Machline-Carrion, M.J.; Santucci, E.V.; Damiani, L.P.; Bahit, M.C.; Málaga, G.; Pontes-Neto, O.M.; Martins, S.C.O.; Zétola, V.F.; Normilio-Silva, K.; Rodrigues De Freitas, G.; et al. Effect of a Quality Improvement Intervention on Adherence to Therapies for Patients with Acute Ischemic Stroke and Transient Ischemic Attack: A Cluster Randomized Clinical Trial. JAMA Neurol. 2019, 76, 932–941. [Google Scholar] [CrossRef] [PubMed]
- Lennon, O.; Blake, C.; Booth, J.; Pollock, A.; Lawrence, M. Interventions for behaviour change and self-management in stroke secondary prevention: Protocol for an overview of reviews. Syst. Rev. 2018, 7, 231. [Google Scholar] [CrossRef]
- SIGN Guidelines.SIGN 149. In Risk Estimation and the Prevention of Cardiovascular Disease Key to Evidence Statements and Recommendations; Scottish Intercollegiate Guidelines Network: Edinburgh, UK, 2017; Volume 1, pp. 1–111.
- Schindel, D.; Schneider, A.; Grittner, U.; Jöbges, M.; Schenk, L. Quality of life after stroke rehabilitation discharge: A 12-month longitudinal study. Disabil Rehabil 2019, 17, 1–10. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping, 1st ed.; Electronic Books; Springer: New York, NY, USA, 1984. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S.; Gruen, R.J.; Delongis, A. Appraisal, Coping, Health Status, and Psychological Symptoms. J. Personal. Soc. Psychol. 1986, 50, 571. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Estrés y Procesos Cognitivos; Martinez Roca: Madrid, Spain, 2008; ISBN 978-84-270-1013-0. [Google Scholar]
- Jovin, T.G.; Chamorro, A.; Cobo, E.; De Miquel, M.A.; Molina, C.A.; Rovira, A.; San Román, L.; Serena, J.; Abilleira, S.; Ribó, M.; et al. Thrombectomy within 8 h after symptom onset in ischemic stroke. N. Engl. J. Med. 2015, 372, 2296–2306. [Google Scholar] [CrossRef]
- Wilson, J.T.L.; Hareendran, A.; Grant, M.; Baird, T.; Schulz, U.G.R.; Muir, K.W.; Bone, I. Improving the assessment of outcomes in stroke: Use of a structured interview to assign grades on the modified Rankin Scale. Stroke 2002, 33, 2243–2246. [Google Scholar] [CrossRef]
- Montaner, J.; Alvarez-Sabin, J. NIH stroke scale and its adaptation to Spanish. Neurologia 2006, 4, 192–202. [Google Scholar]
- Carver, C.S. You Want to Measure Coping But Your Protocol’s Too Long: Consider the Brief COPE; Lawrence Erlbaum Associates (LEA): Mahwah, NJ, USA, 1997; Volume 4. [Google Scholar]
- Pontificia Universidad Javeriana; Landero, R.; González, M.T. Universitas Psychologica [Premium Database Title]; Pontificia Universidad Javeriana: Bogotá, Colombia, 2009; Volume 9. [Google Scholar]
- Group, E. EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Royo-bordonada, M.Á.; Armario, P.; María, J.; Bejarano, L.; Pedro, J.; Alvarez, F.V.; Elosua, R.; Cuixart, C.B.; Cortés, O.; Serrano, B.; et al. Adaptación española de las guías europeas de 2016 sobre prevención de la enfermedad cardiovascular en la práctica clínica. [Spanish Adaptation of the 2016 European Guidelines on Cardiovascular Disease Prevention in Clinical Practice]. Rev. Esp. Salud Pública 2016, 90, e1–e24. [Google Scholar] [PubMed]
- Zhang, J.; Gong, Y.; Zhao, Y.; Jiang, N.; Wang, J.; Yin, X. Post-stroke medication adherence and persistence rates: A meta-analysis of observational studies. J. Neurol. 2019. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Healthy Diet Disponible en. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 8 June 2021).
- Assembly, W.M. Declaration of Helsinki. Law Med. Health Care 1991, 19, 264–265. [Google Scholar] [CrossRef]
- Esenwa, C.; Gutierrez, J. Secondary stroke prevention: Challenges and solutions. Vasc. Health Risk Manag. 2015, 11, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Reverté-Villarroya, S.; Dávalos, A.; Font-Mayolas, S.; Berenguer-Poblet, M.; Sauras-Colón, E.; López-Pablo, C.; Sanjuan-Menéndez, E.; Muñoz-Narbona, L.; Suñer-Soler, R. Coping strategies, quality of life, and neurological outcome in patients treated with mechanical thrombectomy after an acute ischemic stroke. Int. J. Environ. Res. Public Health 2020, 17, 14. [Google Scholar] [CrossRef]
- Chow, E.O.W. The role of meaning in life: Mediating the effects of perceived knowledge of stroke on depression and life satisfaction among stroke survivors. Clin. Rehabil. 2017, 31, 1664–1673. [Google Scholar] [CrossRef]
- Minshall, C.; Ski, C.F.; Apputhurai, P.; Thompson, D.R.; Castle, D.J.; Jenkins, Z.; Knowles, S.R. Exploring the Impact of Illness Perceptions, Self-efficacy, Coping Strategies, and Psychological Distress on Quality of Life in a Post-stroke Cohort. J. Clin. Psychol. Med. Settings 2020. [Google Scholar] [CrossRef]
- Kent, E.E.; Mollica, M.A.; Dionne-Odom, J.N.; Ferrer, R.A.; Jensen, R.E.; Ornstein, K.A.; Smith, A.W. Effect of instrumental support on distress among family caregivers: Findings from a nationally representative study. Palliat. Support. Care 2020. [Google Scholar] [CrossRef] [PubMed]
- Morelli, S.A.; Lee, I.A.; Arnn, M.E.; Zaki, J. Emotional and instrumental support provision interact to predict well-being. Emotion 2015, 15, 484–493. [Google Scholar] [CrossRef] [PubMed]
- Ramazanu, S.; Loke, A.Y.; Chiang, V.C.L. Couples coping in the community after the stroke of a spouse: A scoping review. Nurs. Open 2020, 7, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Lo Buono, V.; Corallo, F.; Bramanti, P.; Marino, S. Coping strategies and health-related quality of life after stroke. J. Health Psychol. 2017, 22, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Oikarinen, A.; Engblom, J.; Kyngäs, H.; Kääriäinen, M. A study of the relationship between the quality of lifestyle counselling and later adherence to the lifestyle changes based on patients with stroke and TIA. Clin. Rehabil. 2018, 32, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Hu, J.; Efird, J.T.; Mccoy, T.P. Social support, coping strategies and health-related quality of life among primary caregivers of stroke survivors in China. J. Clin. Nurs. 2013, 22, 2160–2171. [Google Scholar] [CrossRef]
- Dearborn, J.L.; McCullough, L.D. Perception of risk and knowledge of risk factors in women at high risk for stroke. Stroke 2009, 40, 1181–1186. [Google Scholar] [CrossRef] [PubMed]
- Kraywinkel, K.; Heidrich, J.; Heuschmann, P.U.; Wagner, M.; Berger, K. Stroke risk perception among participants of a stroke awareness campaign. BMC Public Health 2007, 7, 39. [Google Scholar] [CrossRef]
- Aycock, D.M.; Clark, P.C.; Araya, S. Measurement and Outcomes of the Perceived Risk of Stroke: A Review. West. J. Nurs. Res. 2019, 41, 134–154. [Google Scholar] [CrossRef]
- Suñer-Soler, R.; Grau-Martín, A.; Terceno, M.; Silva, Y.; Davalos, A.; Sánchez, J.M.; Font-Mayolas, S.; Gras, E.; Rodrigo, J.; Kazimierczak, M.; et al. Biological and psychological factors associated with smoking abstinence six years post-stroke. Nicotine Tob. Res. 2018, 20, 1182–1188. [Google Scholar] [CrossRef]
- Carey, L.M.; Crewther, S.; Salvado, O.; Lindén, T.; Connelly, A.; Wilson, W.; Howells, D.W.; Churilov, L.; Ma, H.; Tse, T.; et al. STroke imAging pRevention and treatment (START): A longitudinal stroke cohort study: Clinical trials protocol. Int. J. Stroke 2015, 10, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Booth, J.; Connelly, L.; Lawrence, M.; Chalmers, C.; Joice, S.; Becker, C.; Dougall, N. Evidence of perceived psychosocial stress as a risk factor for stroke in adults: A meta-analysis. BMC Neurol. 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Sarah, G.; Clark, L. NHS Improvement-Stroke Psychological Care after Stroke Cognitive and Mood Disorders. Hospitals. 2011. Available online: https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/Psychological-Care-after-Stroke.pdf (accessed on 24 June 2020).
- Westerlind, E.; Singh, R.; Persson, H.C.; Sunnerhagen, K.S. Experienced pain after stroke: A cross-sectional 5-year follow-up study. BMC Neurol. 2020, 20, 4. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Lima, M.J.M.; de Brasileiro, I.C.; de Lima, T.L.; Braga-Neto, P. Quality of life after stroke: Impact of clinical and sociodemographic factors. Clinics 2018, 73. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Characteristics | Total (n = 82) |
|---|---|
| Age (years) [IQR] | 69 [60.0–77.0] |
| Gender (male) (%) | 43 (52.4) |
| Marital status (%) | |
| Married | 62 (75.6) |
| Single | 7 (8.5) |
| Divorced or separated | 4 (4.9) |
| Widower | 9 (11) |
| Level of studies (%) | |
| No studies | 14 (17.1) |
| Primary | 26 (31.7) |
| Secondary | 13 (15.8) |
| Vocational training | 20 (24.4) |
| University | 9 (11) |
| Employment status before stroke (%) | |
| Active | 16 (19.5) |
| Unemployed | 5 (6.1) |
| Retired | 61 (74.4) |
| Baseline family context (%) | |
| Alone | 12 (14.7) |
| With family and/or caregiver | 69 (84.1) |
| Center or residence | 1 (1.2) |
| Alcohol/smoking habits (%) | |
| Alcohol intake | |
| Never | 65 (79.3) |
| Moderate (≤280 g/week) | 13 (15.9) |
| Severe (>280 g/week) | 3 (3.7) |
| Former | 1 (1.2) |
| Smoking | |
| Never | 53 (64.6) |
| Moderate (10–20 cigarettes/day) | 11 (13.4) |
| Excessive (>20 cigarettes/day) 1 | 5 (6.1) |
| Former | 13 (15.9) |
| Etiology of stroke (%) | |
| Atherothrombotic | 12 (14.6) |
| Cardioembolic | 57 (69.5) |
| Unusual cause | 1 (1.2) |
| Undetermined | 12 (14.6) |
| Topography of stroke (%) | |
| PACI | 11 (13.4) |
| TACI | 71 (86.6) |
| Laterality of stroke (%) | |
| Left | 37 (45.1) |
| Right | 45 (54.9) |
| 3 Months (n = 74) | 1 Year (n = 66) | p-Value | |
|---|---|---|---|
| Lifestyle changes | |||
| Therapeutic adherence | 52 (67.5) | 46 (69.7) | 0.549 |
| No therapeutic adherence | 25 (32.5) | 20 (30.3) | |
| Behavioral changes | |||
| Yes | 44 (57.1) | 38 (57.6) | 1.000 |
| No | 33 (42.9) | 28 (42.4) | |
| 3 Months (n = 82) | 1 Year (n = 75) | ||
| NIHSS score | 4 [1.0–11.0] | 3 [1.0–7.25] | 0.412 |
| SIS-16 score | 53 [20.50–73.0] | 61 [45.50–76.25] | 0.274 |
| 3 Months (n = 74) | 1 Year (n = 66) | |||||
|---|---|---|---|---|---|---|
| Pain/Discomfort | Behavioral Changes | No Changes | p-Value | Behavioral Changes | No Changes | p-Value |
| No pain/discomfort | 20 (47.6) | 12 (36.4) | 0.599 | 12 (31.6) | 16 (57.1) | 0.005 |
| Moderate pain/discomfort | 16 (38.1) | 16 (48.5) | 15 (39.5) | 12 (42.9) | ||
| A lot of pain/discomfort | 6 (14.3) | 5 (15.2) | 11 (28.9) | 0 (0.0) | ||
| Pain/Discomfort | Behavioral Changes | No Changes | p-Value | Behavioral Changes | No Changes | p-Value |
| No pain/discomfort | 21 (42.0) | 11 (44.0) | 0.899 | 17 (37.0) | 11 (55.0) | 0.051 |
| Moderate pain/discomfort | 21 (42.0) | 11 (44.0) | 18 (39.1) | 9 (45.0) | ||
| A lot of pain/discomfort | 8 (16.0) | 3 (12.0) | 11 (23.9) | 0 (0.0) | ||
| Active Coping | Planning | Emotional Support | Instrumental Support | Religion | Positive Reframing | Acceptance | |
|---|---|---|---|---|---|---|---|
| 3 months: (n = 50) | |||||||
| Spearman’s ρ | 0.057 | −0.024 | 0.152 | 0.108 | −0.040 | −0.056 | −0.069 |
| p-value | 0.693 | 0.869 | 0.291 | 0.457 | 0.783 | 0.697 | 0.633 |
| 1 year: (n = 44) | |||||||
| Spearman’s ρ | 0.225 | 0.242 | 0.282 | 0.272 | −0.012 | 0.072 | −0.096 |
| p-value | 0.117 | 0.090 | 0.047 | 0.056 | 0.935 | 0.621 | 0.508 |
| Denial | Humor | Self-Distraction | Self-Blame | Behavioral Disengagement | Venting | Use of Substances1 | |
| 3 months: (n = 50) | |||||||
| Spearman’s ρ | −0.172 | 0.057 | 0.052 | 0.126 | −0.025 | 0.084 | −0.142 |
| p-value | 0.233 | 0.694 | 0.717 | 0.385 | 0.864 | 0.562 | 0.325 |
| 1 year: (n = 44) | |||||||
| Spearman’s ρ | 0.163 | −0.149 | 0.106 | 0.009 | 0.094 | −0.019 | 0.275 |
| p-value | 0.259 | 0.302 | 0.466 | 0.948 | 0.518 | 0.894 | 0.053 |
| Variable | B | Standard Error | OR | (CI 95%) | p-Value | |
|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | |||||
| Constant | −8.439 | 6.117 | 0.000 | 0.168 | ||
| Age | 0.018 | 0.036 | 1.018 | 0.949 | 1.093 | 0.614 |
| Gender (male) | 0.624 | 0.681 | 1.867 | 0.492 | 7.089 | 0.359 |
| Pain/discomfort (EQ-5D) | 1.536 | 0.755 | 4.646 | 1.058 | 20.393 | 0.042 |
| Emotional support | 0.202 | 0.218 | 1.223 | 0.798 | 1.876 | 0.356 |
| COPE-28 total score | −0.081 | 0.039 | 0.922 | 0.855 | 0.994 | 0.035 |
| NIHSS score | 0.397 | 0.274 | 1.487 | 0.869 | 2.543 | 0.148 |
| SIS-16 score | 0.088 | 0.054 | 1.092 | 0.983 | 1.213 | 0.101 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reverté-Villarroya, S.; Suñer-Soler, R.; Font-Mayolas, S.; Dávalos Errando, A.; Sauras-Colón, E.; Gras-Navarro, A.; Adell-Lleixà, M.; Casanova-Garrigós, G.; Gil-Mateu, E.; Berenguer-Poblet, M. Influence of Pain and Discomfort in Stroke Patients on Coping Strategies and Changes in Behavior and Lifestyle. Brain Sci. 2021, 11, 804. https://doi.org/10.3390/brainsci11060804
Reverté-Villarroya S, Suñer-Soler R, Font-Mayolas S, Dávalos Errando A, Sauras-Colón E, Gras-Navarro A, Adell-Lleixà M, Casanova-Garrigós G, Gil-Mateu E, Berenguer-Poblet M. Influence of Pain and Discomfort in Stroke Patients on Coping Strategies and Changes in Behavior and Lifestyle. Brain Sciences. 2021; 11(6):804. https://doi.org/10.3390/brainsci11060804
Chicago/Turabian StyleReverté-Villarroya, Silvia, Rosa Suñer-Soler, Sílvia Font-Mayolas, Antonio Dávalos Errando, Esther Sauras-Colón, Andrea Gras-Navarro, Mireia Adell-Lleixà, Georgina Casanova-Garrigós, Elsa Gil-Mateu, and Marta Berenguer-Poblet. 2021. "Influence of Pain and Discomfort in Stroke Patients on Coping Strategies and Changes in Behavior and Lifestyle" Brain Sciences 11, no. 6: 804. https://doi.org/10.3390/brainsci11060804
APA StyleReverté-Villarroya, S., Suñer-Soler, R., Font-Mayolas, S., Dávalos Errando, A., Sauras-Colón, E., Gras-Navarro, A., Adell-Lleixà, M., Casanova-Garrigós, G., Gil-Mateu, E., & Berenguer-Poblet, M. (2021). Influence of Pain and Discomfort in Stroke Patients on Coping Strategies and Changes in Behavior and Lifestyle. Brain Sciences, 11(6), 804. https://doi.org/10.3390/brainsci11060804







