Structural Changes on MRI Demonstrate Specific Cerebellar Involvement in SLE Patients—A VBM Study
Abstract
1. Introduction
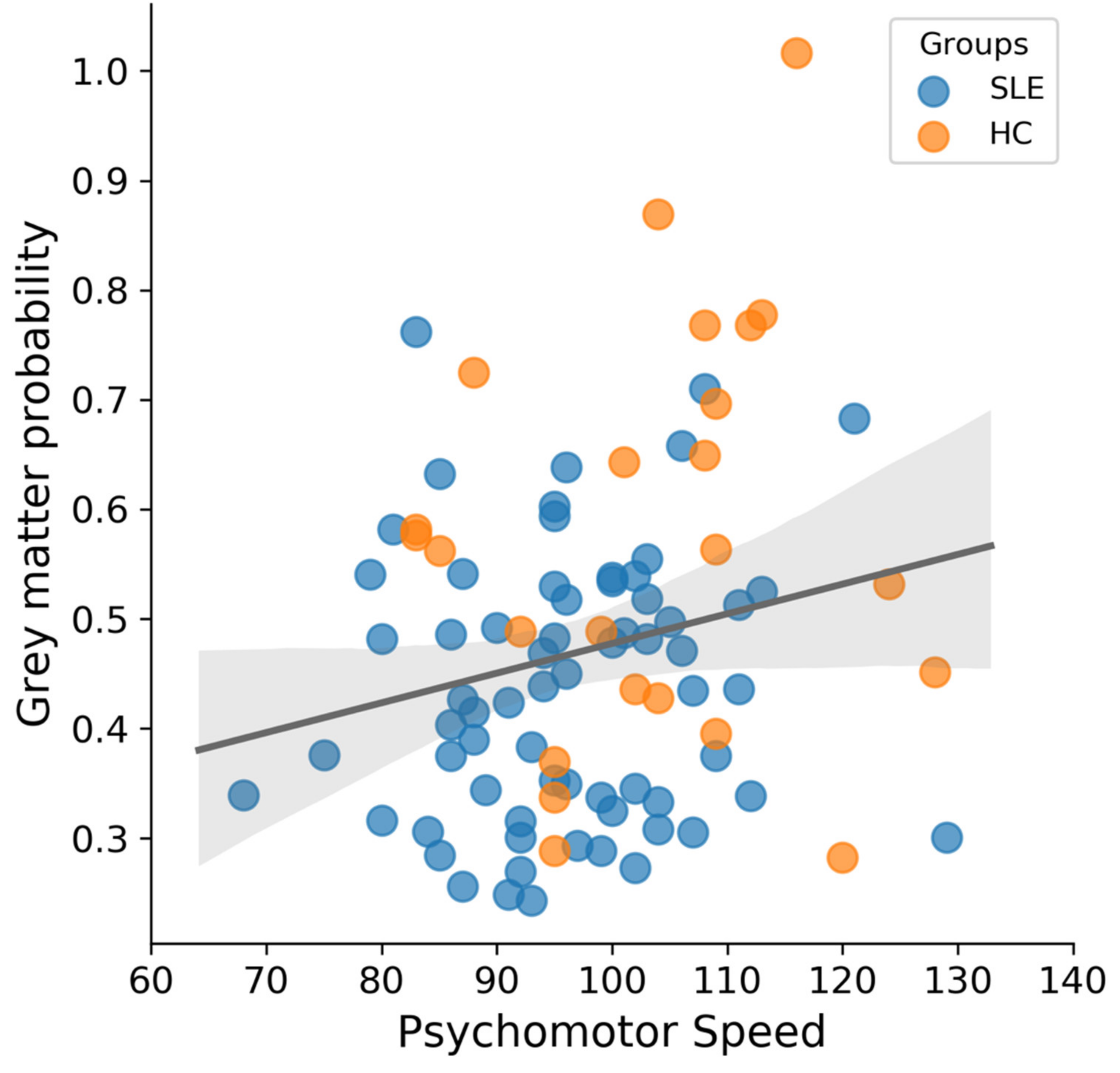
2. Results
3. Discussion
4. Conclusions
5. Materials and Methods
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lisnevskaia, L.; Murphy, G.; Isenberg, D. Systemic lupus erythematosus and other autoimmune rheumatic diseases: Challenges to treatment. Lancet 2014, 384, 1878–1888. [Google Scholar] [CrossRef]
- Isenberg, D.A.; Rahman, A. Systemic lupus erythematosus—Annus mirabilis? Nat. Clin. Pract. Rheumatol. 2006, 2, 145–152. [Google Scholar] [CrossRef]
- Tsokos, G.C. Systemic Lupus Erythematosus. N. Engl. J. Med. 2020, 365, 2110–2121. [Google Scholar] [CrossRef] [PubMed]
- Hanly, J.G. Diagnosis and Management of Neuropsychiatric SLE. Nat. Rev. Rheumatol. 2014, 10, 338–347. [Google Scholar] [CrossRef]
- Ainiala, H.; Loukkola, J.; Peltola, J.; Korpela, M.; Hietaharju, A. The Prevalence of Neuropsychiatric Syndromes in Systemic Lupus Erythematosus. Neurology 2001, 57, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Ainiala, H.; Dastidar, P.; Loukkola, J.; Lehtimaki, T.; Korpela, M.; Peltola, J.; Hietaharju, A. Cerebral MRI Abnormalities and their Association with Neuropsychiatric Manifestations in SLE: A Population-Based Study. Scand. J. Rheumatol. 2005, 34, 376–382. [Google Scholar] [CrossRef]
- Sibbitt, W.L., Jr.; Brooks, W.M.; Kornfeld, M.; Hart, B.L.; Bankhurst, A.D.; Roldan, C.A. Magnetic Resonance Imaging and Brain Histopathology in Neuropsychiatric Systemic Lupus Erythematosus. Semin. Arthritis Rheum. 2010, 40, 32–52. [Google Scholar] [CrossRef]
- Hanly, J.G.; Urowitz, M.B.; Sanchez-Guerrero, J.; Bae, S.C.; Gordon, C.; Wallace, D.J.; Isenberg, D.; Alarcon, G.S.; Clarke, A.; Bernatsky, S.; et al. Systemic Lupus International Collaborating. Neuropsychiatric Events at the Time of Diagnosis of Systemic Lupus Erythematosus: An International Inception Cohort Study. Arthritis Rheum. 2007, 56, 265–273. [Google Scholar] [CrossRef]
- Bachen, E.A.; Chesney, M.A.; Criswell, L.A. Prevalence of Mood and Anxiety Disorders in Women with Systemic Lupus Erythematosus. Arthritis Rheum. 2009, 61, 822–829. [Google Scholar] [CrossRef]
- Patel, P.; Werth, V. Cutaneous Lupus Erythematosus: A Review. Dermatol. Clin. 2002, 20, 373. [Google Scholar] [CrossRef]
- Nishimura, K.; Omori, M.; Katsumata, Y.; Sato, E.; Gono, T.; Kawaguchi, Y.; Harigai, M.; Mimura, M.; Yamanaka, H.; Ishigooka, J. Neurocognitive Impairment in Corticosteroid-Naive Patients with Active Systemic Lupus Erythematosus: A Prospective Study. J. Rheumatol. 2015, 42, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Unterman, A.; Nolte, J.E.; Boaz, M.; Abady, M.; Shoenfeld, Y.; Zandman-Goddard, G. Neuropsychiatric Syndromes in Systemic Lupus Erythematosus: A Meta-Analysis. Semin. Arthritis Rheum. 2011, 41, 1–11. [Google Scholar] [CrossRef]
- Nishimura, K.; Katsumata, Y. Does Lupus Reduce Psychomotor Speed? Int. J. Clin. Rheumatol. 2015, 10, 305–307. [Google Scholar] [CrossRef]
- Nystedt, J.; Mannfolk, P.; Jönsen, A.; Nilsson, P.; Strandberg, T.O.; Sundgren, P.C. Functional Connectivity Changes in Core Resting State Networks are Associated with Cognitive Performance in Systemic Lupus Erythematosus. J. Comp. Neurol. 2019, 527, 1837–1856. [Google Scholar] [CrossRef] [PubMed]
- Gulati, G.; Jones, J.T.; Lee, G.; Altaye, M.; Beebe, D.W.; Meyers-Eaton, J.; Wiley, K.; Brunner, H.I.; DiFrancesco, M.W. Blood Brain Barrier Permeability is Altered in Patients with Systemic Lupus Erythematosus: A Novel Imaging Approach. Arthritis Care Res. 2016, 69, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, S.R.; Kasturi, S.; Costenbader, K.H. The Epidemiology of Atherosclerotic Cardiovascular Disease Among Patients with SLE: A Systematic Review. Semin. Arthritis Rheum. 2013, 43, 77–95. [Google Scholar] [CrossRef] [PubMed]
- Ishimori, M.L.; Martin, R.; Berman, D.S.; Goykhman, P.; Shaw, L.J.; Shufelt, C.; Slomka, P.J.; Thomson, L.E.; Schapira, J.; Yang, Y.; et al. Myocardial Ischemia in the Absence of Obstructive Coronary Artery Disease in Systemic Lupus Erythematosus. JACC Cardiovasc. Imaging 2011, 4, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Schmugge, M.; Revel-Vilk, S.; Hiraki, L.; Rand, M.L.; Blanchette, V.S.; Silverman, E.D. Thrombocytopenia and Thromboembolism in Pediatric Systemic Lupus Erythematosus. J. Pediatrics 2003, 143, 666–669. [Google Scholar] [CrossRef]
- Skaggs, B.J.; Hahn, B.H.; McMahon, M. Accelerated Atherosclerosis in Patients with SLE—Mechanisms and Management. Nat. Rev. Rheumatol. 2012, 8, 214. [Google Scholar] [CrossRef]
- Faria, R.; Goncalves, J.; Dias, R. Neuropsychiatric Systemic Lupus Erythematosus Involvement: Towards a Tailored Approach to our Patients? Rambam. Maimonides Med. J. 2017, 8. [Google Scholar] [CrossRef]
- Jennings, J.E.; Sundgren, P.C.; Attwood, J.; McCune, J.; Maly, P. Value of MRI of the Brain in Patients with Systemic Lupus Erythematosus and Neurologic Disturbance. Neuroradiology 2004, 46, 15–21. [Google Scholar]
- Harboe, E.; Greve, O.J.; Beyer, M.; Gøransson, L.G.; Tjensvoll, A.B.; Maroni, S.; Omdal, R. Fatigue is Associated with Cerebral White Matter Hyperintensities in Patients with Systemic Lupus Erythematosus. J. Neurol. Neurosurg. Psychiatry 2008, 79, 199–201. [Google Scholar] [CrossRef]
- Toledano, P.; Orueta, R.; Rodríguez-Pintó, I.; Valls-Solé, J.; Cervera, R.; Espinosa, G. Peripheral Nervous System Involvement in Systemic Lupus Erythematosus: Prevalence, Clinical and Immunological Characteristics, Treatment and Outcome of a Large Cohort from a Single Centre. Autoimmun. Rev. 2017, 16, 750–755. [Google Scholar] [CrossRef]
- Sibbitt, W.L.; Haseler, L.J.; Griffey, R.R.; Friedman, S.D.; Brooks, W.M. Neurometabolism of active neuropsychiatric lupus determined with proton MR spectroscopy. Am. J. Neuroradiol. 1997, 18, 1271–1277. [Google Scholar] [PubMed]
- Cagnoli, P.; Harris, R.E.; Frechtling, D.; Berkis, G.; Gracley, R.H.; Graft, C.C.; Lowe, S.E.; Chenevert, T.L.; McCune, W.J.; Gebarski, S.; et al. Reduced Insular Glutamine and N-acetylaspartate in Systemic Lupus Erythematosus: A Single-Voxel (1)H-MR Spectroscopy Study. Acad. Radiol. 2013, 20, 1286–1296. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Shastri, R.; Shah, G.; Wang, P.; Cagnoli, P.; Schmidt-Wilcke, T.; McCune, J.; Harris, R.; Sundgren, P. MR Diffusion Tractography to Identify and Characterize Microstructural White Matter Tract Changes in Systemic Lupus Erythematosus Patients. Acad. Radiol. 2016, 23, 1431–1440. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.; Sundgren, P.C.; Fan, X.; Foerster, B.; Nan, B.; Welsh, R.C.; Williamson, J.A.; Attwood, J.; Maly, P.V.; Chenevert, T.L.; et al. Diffusion Tensor Imaging in Patients with Acute Onset of Neuropsychiatric Systemic Lupus Erythematosus: A Prospective Study of Apparent Diffusion Coefficient, Fractional Anisotropy Values, and Eigenvalues in Different Regions of the Brain. Acta Radiol. 2007, 48, 213–222. [Google Scholar] [CrossRef]
- Schmidt-Wilcke, T.; Cagnoli, P.; Wang, P.; Schultz, T.; Lotz, A.; McCune, W.J.; Sundgren, P.C. Diminished White Matter Integrity in Patients with Systemic Lupus Erythematosus. Neuroimage Clin. 2014, 5, 291–297. [Google Scholar] [CrossRef]
- Welsh, R.C.; Rahbar, H.; Foerster, B.; Thurnher, M.; Sundgren, P.C. Brain diffusivity in patients with neuropsychiatric systemic lupus erythematosus with new acute neurological symptoms. J. Magn. Reson. Imaging. Off. J. Int. Soc. Magn. Reson. Med. 2007, 26, 541–551. [Google Scholar] [CrossRef]
- Appenzeller, S.; Bonilha, L.; Rio, P.A.; Li, L.M.; Costallat, L.T.L.; Cendes, F. Longitudinal Analysis of Gray and White Matter Loss in Patients with Systemic Lupus Erythematosus. Neuroimage 2007, 34, 694–701. [Google Scholar] [CrossRef]
- Appenzeller, S.; Cendes, F.; Costallat, L.T.L. Cerebellar Ataxia in Systemic Lupus Erythematosus. Lupus 2008, 17, 1122–1126. [Google Scholar] [CrossRef]
- Singh, R.R.; Prasad, K.; Kumar, A.S.H.O.K.; Misra, A.N.O.O.P.; Padmakumar, K.; Malaviya, A.N. Cerebellar ataxia in systemic lupus erythematosus: Three case reports. Ann. Rheum. Dis. 1988, 47, 954–956. [Google Scholar] [CrossRef]
- Yaginuma, M.; Suenaga, M.; Shiono, Y.; Sakamoto, M. Acute Cerebellar Ataxia of a Patient with SLE. Clin. Neurol. Neurosurg. 2000, 102, 37–39. [Google Scholar] [CrossRef]
- Smith, R.W.; Ellison, D.W.; Jenkins, E.A.; Gallagher, P.J.; Cawley, M.I. Cerebellum and Brainstem Vasculopathy in Systemic Lupus Erythematosus: Two Clinico-Pathological Cases. Ann. Rheum. Dis. 1994, 53, 327–330. [Google Scholar] [CrossRef]
- Zivadinov, R.; Shucard, J.L.; Hussein, S.; Durfee, J.; Cox, J.L.; Bergsland, N.; Dwyer, M.G.; Benedict, R.H.; Ambrus, J.; Shucard, D.W. Multimodal Imaging in Systemic Lupus Erythematosus Patients with Diffuse Neuropsychiatric Involvement. Lupus 2013, 22, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Ercan, E.; Ingo, C.; Tritanon, O.; Magro-Checa, C.; Smith, A.; Smith, S.; Huizinga, T.; van Buchem, M.A.; Ronen, I. A Multimodal MRI Approach to Identify and Characterize Microstructural Brain Changes in Neuropsychiatric Systemic Lupus Erythematosus. NeuroImage Clin. 2015, 8, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Sarbu, N.; Toledano, P.; Calvo, A.; Roura, E.; Sarbu, M.I.; Espinosa, G.; Lladó, X.; Cervera, R.; Bargalló, N. Advanced MRI Techniques: Biomarkers in Neuropsychiatric Lupus. Lupus 2017, 26, 510–516. [Google Scholar] [CrossRef]
- Cannerfelt, B.; Nystedt, J.; Jönsen, A.; Lätt, J.; van Westen, D.; Lilja, A.; Bengtsson, A.; Nilsson, P.; Mårtensson, J.; Sundgren, P.C. White Matter Lesions and Brain Atrophy in Systemic Lupus Erythematosus Patients: Correlation to Cognitive Dysfunction in a Cohort of Systemic Lupus Erythematosus Patients Using Different Definition Models for Neuropsychiatric Systemic Lupus Erythematosus. Lupus 2018, 27, 1140–1149. [Google Scholar] [CrossRef]
- Roldan, P.C.; Jung, R.E.; Sibbitt, W.L.; Qualls, C.R.; Flores, R.A.; Roldan, C.A. Correlation of Neurocognitive Function and Brain Lesion Load on Magnetic Resonance Imaging in Systemic Lupus Erythematosus. Rheumatol. Int. 2018, 38, 1539–1546. [Google Scholar] [CrossRef]
- Balsters, J.H.; Cussans, E.; Diedrichsen, J.; Phillips, K.A.; Preuss, T.M.; Rilling, J.K.; Ramnani, N. Evolution of the Cerebellar Cortex: The Selective Expansion of Prefrontal-Projecting Cerebellar Lobules. Neuroimage 2010, 49, 2045–2052. [Google Scholar] [CrossRef]
- Stoodley, C.J.; Schmahmann, J.D. Functional Topography in the Human Cerebellum: A Meta-Analysis of Neuroimaging Studies. Neuroimage 2009, 44, 489–501. [Google Scholar] [CrossRef]
- Stoodley, C.J.; Schmahmann, J.D. Evidence for Topographic Organization in the Cerebellum of Motor Control Versus Cognitive and Affective Processing. Cortex 2010, 46, 831–844. [Google Scholar] [CrossRef] [PubMed]
- Coombes, S.A.; Misra, G. Pain and Motor Processing in the Human Cerebellum. Pain 2016, 157, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Casciato, S.; Mascia, A.; Quarato, P.P.; D’Aniello, A.; Scoppetta, C.; Di Gennaro, G. Subacute Cerebellar Ataxia as Presenting Symptom of Systemic Lupus Erythematosus. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 7401–7403. [Google Scholar]
- Hanyuda, M.; Yoda, Y.; Shiozawa, T.; Hanaoka, R.; Miwa, Y.; Kaga, S.; Kasama, T.; Negishi, M.; Ide, H. A Case with Systemic Lupus Erythematosus Presenting with Reversible Edematous Lesion in Cerebellum. Ryumachi. Rheum. 2002, 42, 801–806. [Google Scholar]
- Checa, C.M.; Cohen, D.; Bollen, E.L.; van Buchem, M.A.; Huizinga, T.W.; Steup-Beekman, G.M. Demyelinating Disease in SLE: Is it Multiple Sclerosis or Lupus? Best Pract. Res. Clin. Rheumatol. 2013, 27, 405–424. [Google Scholar] [CrossRef]
- Wilkins, A. Cerebellar Dysfunction in Multiple Sclerosis. Front. Neurol. 2017, 8, 312. [Google Scholar] [CrossRef]
- Kutzelnigg, A.; Faber-Rod, J.C.; Bauer, J.; Lucchinetti, C.F.; Sorensen, P.S.; Laursen, H.; Stadelmann, C.; Brück, W.; Rauschka, H.; Schmidbauer, M.; et al. Widespread Demyelination in the Cerebellar Cortex in Multiple Sclerosis. Brain Pathol. Zur. Switz. 2007, 17, 38–44. [Google Scholar] [CrossRef]
- Ramasamy, D.P.; Benedict, R.H.; Cox, J.L.; Fritz, D.; Abdelrahman, N.; Hussein, S.; Minagar, A.; Dwyer, M.G.; Zivadinov, R. Extent of Cerebellum, Subcortical and Cortical Atrophy in Patients with MS: A Case-Control Study. J. Neurol. Sci. 2009, 282, 47–54. [Google Scholar] [CrossRef]
- Valentino, P.; Cerasa, A.; Chiriaco, C.; Nisticò, R.; Pirritano, D.; Gioia, M.; Lanza, P.; Canino, M.; Del Giudice, F.; Gallo, O.; et al. Cognitive Deficits in Multiple Sclerosis Patients with Cerebellar Symptoms. Mult. Scler. Houndmills Basingstoke Engl. 2009, 15, 854–859. [Google Scholar] [CrossRef]
- Tan, E.M.; Cohen, A.S.; Fries, J.F.; Masi, A.T.; McShane, D.J.; Rothfield, N.F.; Schaller, J.G.; Talal, N.; Winchester, R.J. The 1982 Revised Criteria for the Classification of Systemic Lupus Erythematosus. Arthritis Rheum. 1982, 25, 1271–1277. [Google Scholar] [CrossRef]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The Fatigue Severity Scale: Application to Patients with Multiple Sclerosis and Systemic Lupus Erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef]
- Aitken, R.C. Measurement of Feelings Using Visual Analogue Scales. Proc. R Soc. Med. 1969, 62, 989–993. [Google Scholar]
- Fantino, B.; Moore, N. The Self-reported Montgomery-Asberg Depression Rating Scale is a Useful Evaluative Tool in Major Depressive Disorder. BMC Psychiatry 2009, 9, 26. [Google Scholar] [CrossRef] [PubMed]
- Gladman, D.D.; Ibanez, D.; Urowitz, M.B. Systemic Lupus Erythematosus Disease Activity Index 2000. J. Rheumatol. 2002, 29, 288–291. [Google Scholar] [PubMed]
- Petri, M.; Orbai, A.M.; Alarcón, G.S.; Gordon, C.; Merrill, J.T.; Fortin, P.R.; Bruce, I.N.; Isenberg, D.; Wallace, D.J.; Nived, O.; et al. Derivation and Validation of the Systemic Lupus International Collaborating Clinics Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheum. 2012, 64, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Kivity, S.; Agmon-Levin, N.; Zandman-Goddard, G.; Chapman, J.; Shoenfeld, Y. Neuropsychiatric Lupus: A Mosaic of Clinical Presentations. BMC Med. 2015, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Gualtieri, C.T.; Johnson, L.G. Reliability and Validity of a Computerized Neurocognitive Test Battery, CNS Vital Signs. Arch. Clin. Neuropsychol. 2006, 21, 623–643. [Google Scholar] [CrossRef]
- Whitwell, J.L. Voxel-based Morphometry: An Automated Technique for Assessing Structural Changes in the Brain. J. Neurosci. 2009, 29, 9661–9664. [Google Scholar] [CrossRef] [PubMed]
- Good, C.D.; Johnsrude, I.S.; Ashburner, J.; Henson, R.N.; Friston, K.J.; Frackowiak, R.S. A Voxel-based Morphometric Study of Ageing in 465 Normal Adult Human Brains. NeuroImage 2001, 14, 21–36. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.M.; Jenkinson, M.; Woolrich, M.W.; Beckmann, C.F.; Behrens, T.E.; Johansen-Berg, H.; Bannister, P.R.; De Luca, M.; Drobnjak, I.; Flitney, D.E.; et al. Advances in Functional and Structural MR Image Analysis and Implementation as FSL. Advances in Functional and Structural MR Image Analysis and Implementation as FSL. NeuroImage 2004, 23 (Suppl. 1), S208–S219. [Google Scholar] [CrossRef] [PubMed]
- Douaud, G.; Smith, S.; Jenkinson, M.; Behrens, T.; Johansen-Berg, H.; Vickers, J.; James, S.; Voets, N.; Watkins, K.; Matthews, P.M.; et al. Anatomically Related Grey and White Matter Abnormalities in Adolescent-Onset Schizophrenia. Brain 2007, 130, 2375–2386. [Google Scholar] [CrossRef] [PubMed]
- Andersson, J.L.R.; Jenkinson, M.; Smith, S. Non-Linear Registration, aka Spatial Normalisation. FMRIB Tech. Rep. TR07JA2. 2007. Available online: www.fmrib.ox.ac.uk/analysis/techrep (accessed on 16 April 2021).
- Winkler, A.M.; Ridgway, G.R.; Webster, M.A.; Smith, S.M.; Nichols, T.E. Permutation Inference for the General Linear Model. Neuroimage 2014, 92, 381–397. [Google Scholar] [CrossRef] [PubMed]
- The Jamovi Project. Jamovi. (Version 1.0.8.0). 2020. Available online: https://www.jamovi.org (accessed on 16 April 2021).
- R Core Team. R: A Language and Envionment for Statistical Computing. 2018. Available online: https://cran.r-project.org/ (accessed on 16 April 2021).
- JASP Team. JASP (Version 0.12.2). 2020. Available online: https://jasp-stats.org/ (accessed on 16 April 2021).
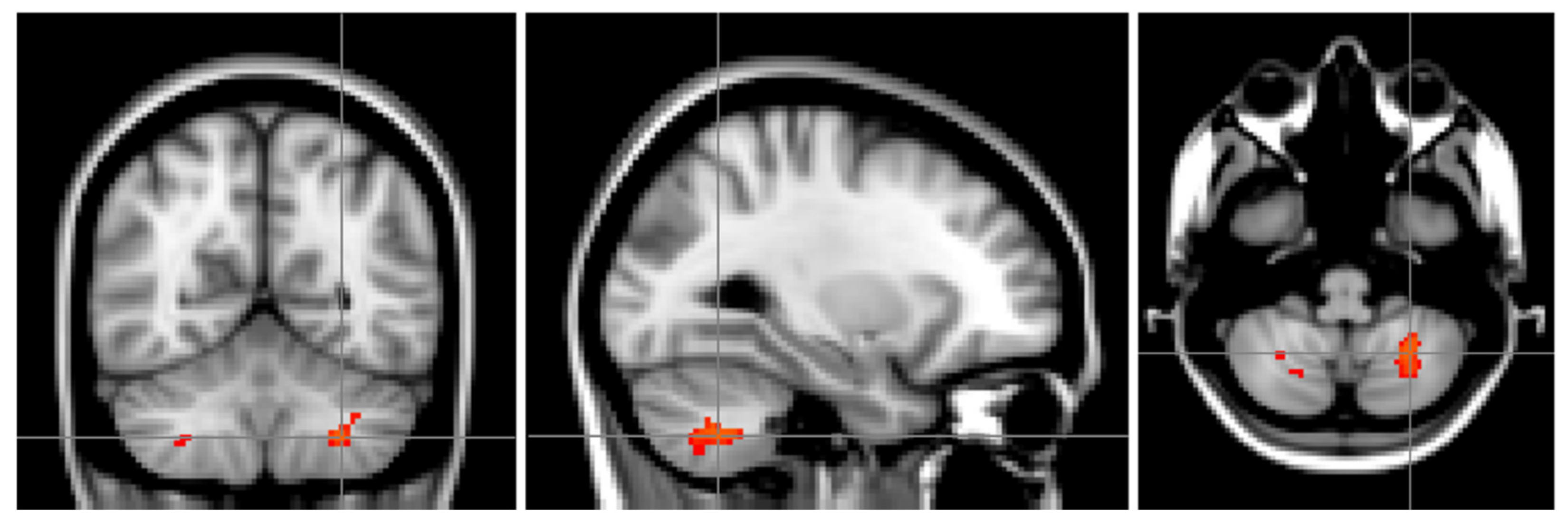


| Location of Maximum Intensity Voxel (mm) | Location of the Centre of Gravity for the Cluster (mm) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Cluster | Voxel Size | Maximum p Value | X | Y | Z | X | Y | Z | Localization |
| 1 | 126 | 0.03 | −26 | −58 | −46 | −27.4 | −60.1 | −44.9 | 35% L. VIIIa, 5% L. VIIb |
| 2 | 52 | 0.04 | 38 | −48 | −52 | 38.5 | −50.8 | −51.5 | 65% R. VIIIa, 30% R. VIIb, 4% R. Crus II |
| 3 | 12 | 0.05 | 16 | −66 | −42 | 17.8 | −65.7 | −43 | 21% R. VIIIa, 15% R. VIIb, 1% R. Crus II |
| 4 | 4 | 0.05 | 28 | −60 | −46 | 29.5 | −59.5 | −46.5 | 36% R. VIIIa, 16% R. VIIb, 1% R. VIIIb |
| 5 | 2 | 0.05 | 8 | −62 | −28 | 8 | −62 | −27 | 3% R. VI, 2% Vermis VI, 1% R. VIIIa, 1% R. V |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mårtensson, J.; Rumetshofer, T.; Nystedt, J.; Lätt, J.; Nilsson, P.; Bengtsson, A.; Jönsen, A.; Sundgren, P.C. Structural Changes on MRI Demonstrate Specific Cerebellar Involvement in SLE Patients—A VBM Study. Brain Sci. 2021, 11, 510. https://doi.org/10.3390/brainsci11040510
Mårtensson J, Rumetshofer T, Nystedt J, Lätt J, Nilsson P, Bengtsson A, Jönsen A, Sundgren PC. Structural Changes on MRI Demonstrate Specific Cerebellar Involvement in SLE Patients—A VBM Study. Brain Sciences. 2021; 11(4):510. https://doi.org/10.3390/brainsci11040510
Chicago/Turabian StyleMårtensson, Johan, Theodor Rumetshofer, Jessika Nystedt, Jimmy Lätt, Petra Nilsson, Anders Bengtsson, Andreas Jönsen, and Pia C. Sundgren. 2021. "Structural Changes on MRI Demonstrate Specific Cerebellar Involvement in SLE Patients—A VBM Study" Brain Sciences 11, no. 4: 510. https://doi.org/10.3390/brainsci11040510
APA StyleMårtensson, J., Rumetshofer, T., Nystedt, J., Lätt, J., Nilsson, P., Bengtsson, A., Jönsen, A., & Sundgren, P. C. (2021). Structural Changes on MRI Demonstrate Specific Cerebellar Involvement in SLE Patients—A VBM Study. Brain Sciences, 11(4), 510. https://doi.org/10.3390/brainsci11040510






