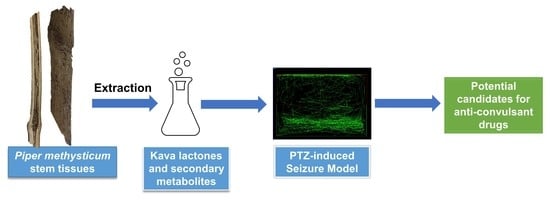
Evaluation of Anti-Convulsive Properties of Aqueous Kava Extract on Zebrafish Using the PTZ-Induced Seizure Model
Abstract
1. Introduction
2. Materials and Methods
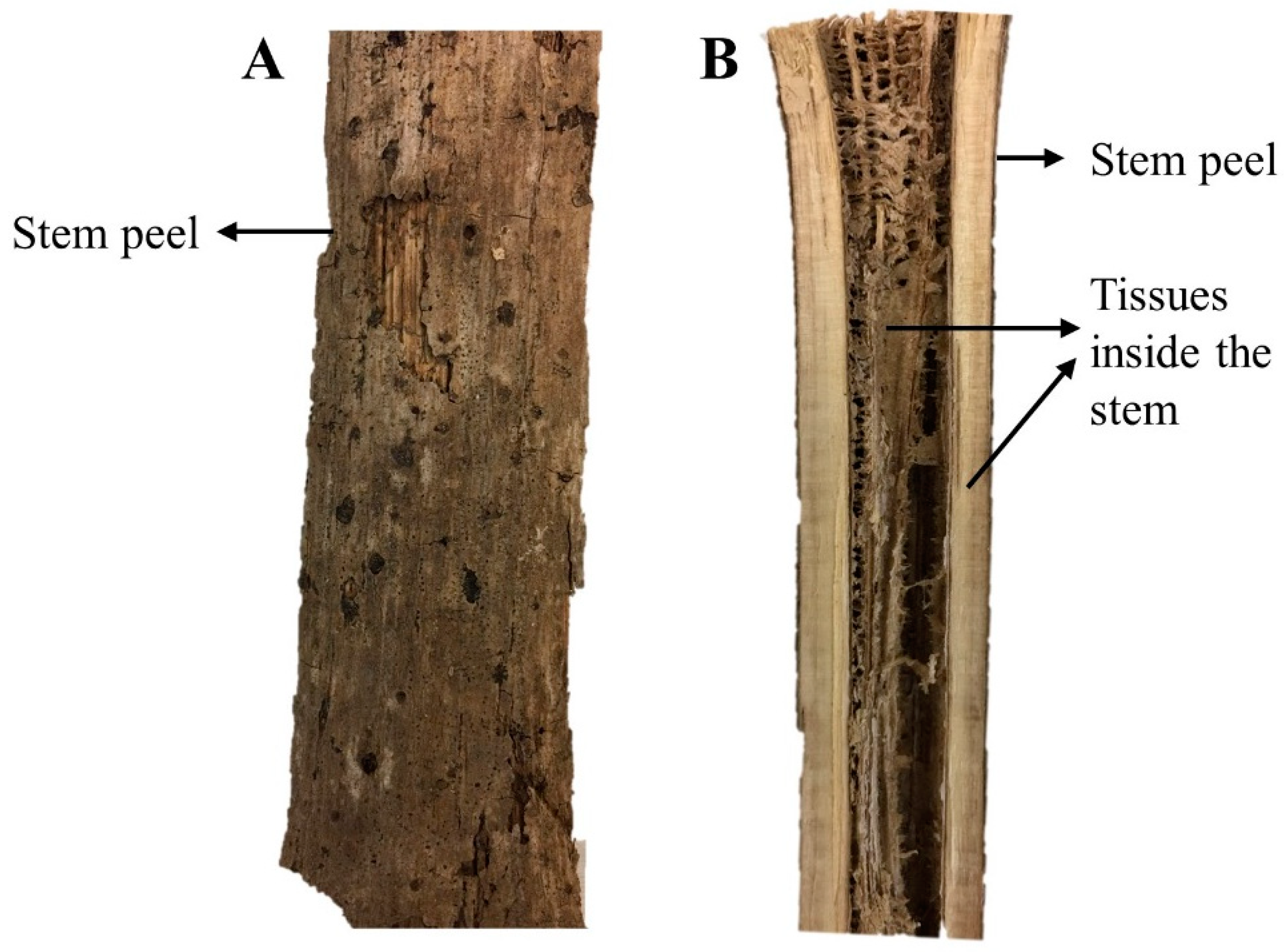
2.1. Extraction and Plant Material
2.2. Reagents and Chemicals
2.3. Animals Studies
2.4. Toxicity Screening
2.5. Behavioral Study
- Group I:
- PTZ (170 mg/kg) used as negative control;
- Group II:
- tank water used as vehicle control;
- Group III:
- DZP (10 mg/L) + PTZ (170 mg/kg) used as positive control;
- Group IV:
- Kava extract SNPA (100 mg/kg) + PTZ (170 mg/kg) used as treatment group 1;
- Group V:
- Kava extract SNPA (50 mg/kg) + PTZ (170 mg/kg) used as treatment group 2;
- Group VI:
- Kava extract SPA (50 mg/kg) + PTZ (170 mg/kg) used as treatment group 3;
- Group VII:
- Kava extract SPA (25 mg/kg) + PTZ (170 mg/kg) used as treatment group 4;
- Group VIII:
- Kava extract SWA (50 mg/kg) + PTZ (170 mg/kg) used as treatment group 5;
- Group IX:
- Kava extract SWA (25 mg/kg) + PTZ (170 mg/kg) used as treatment group 4.
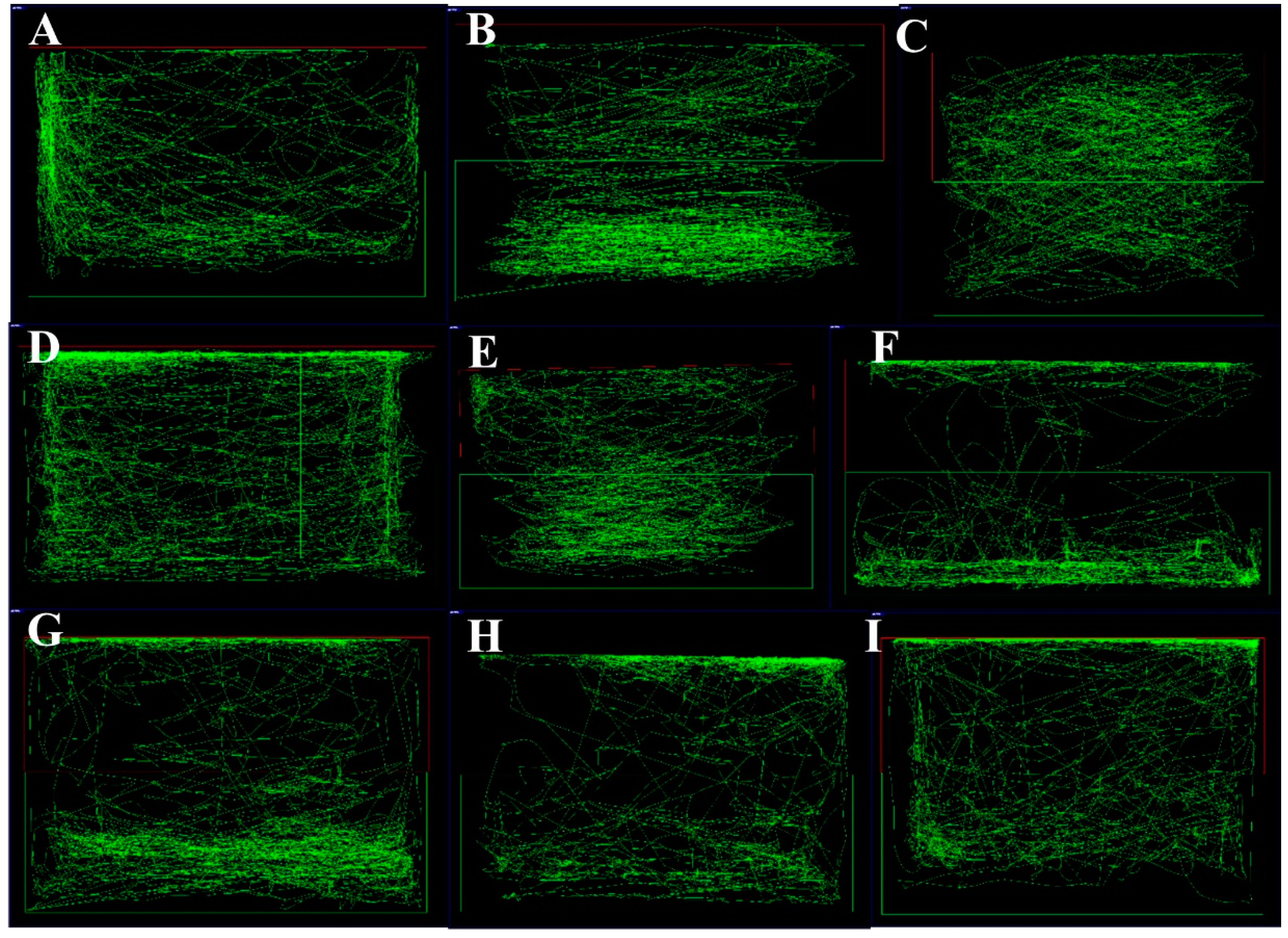
2.6. PTZ-Induced Seizure Model
- Score 1 -
- Short swim indicates swimming mainly at the bottom of the tank;
- Score 2 -
- Increased swimming activity and high frequency indicates opercular movement;
- Score 3 -
- Indicates burst swimming, left and right movements, as well as erratic movements;
- Score 4 -
- Indicates circular movements.
2.7. Gene Expression Study
2.8. Data Analysis
3. Results
3.1. Toxicity Study
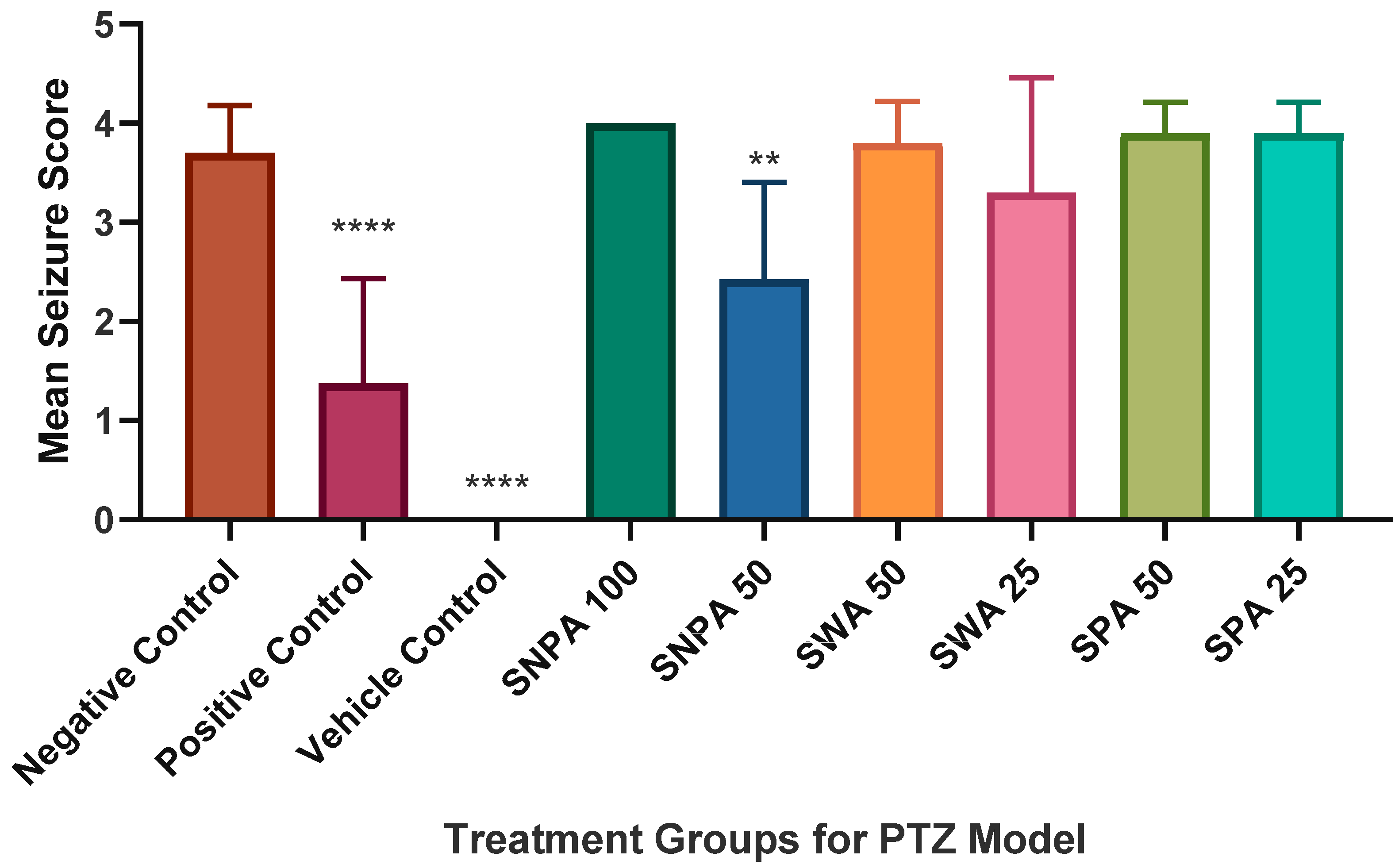
3.2. Behavioral Study
3.2.1. Swimming Pattern
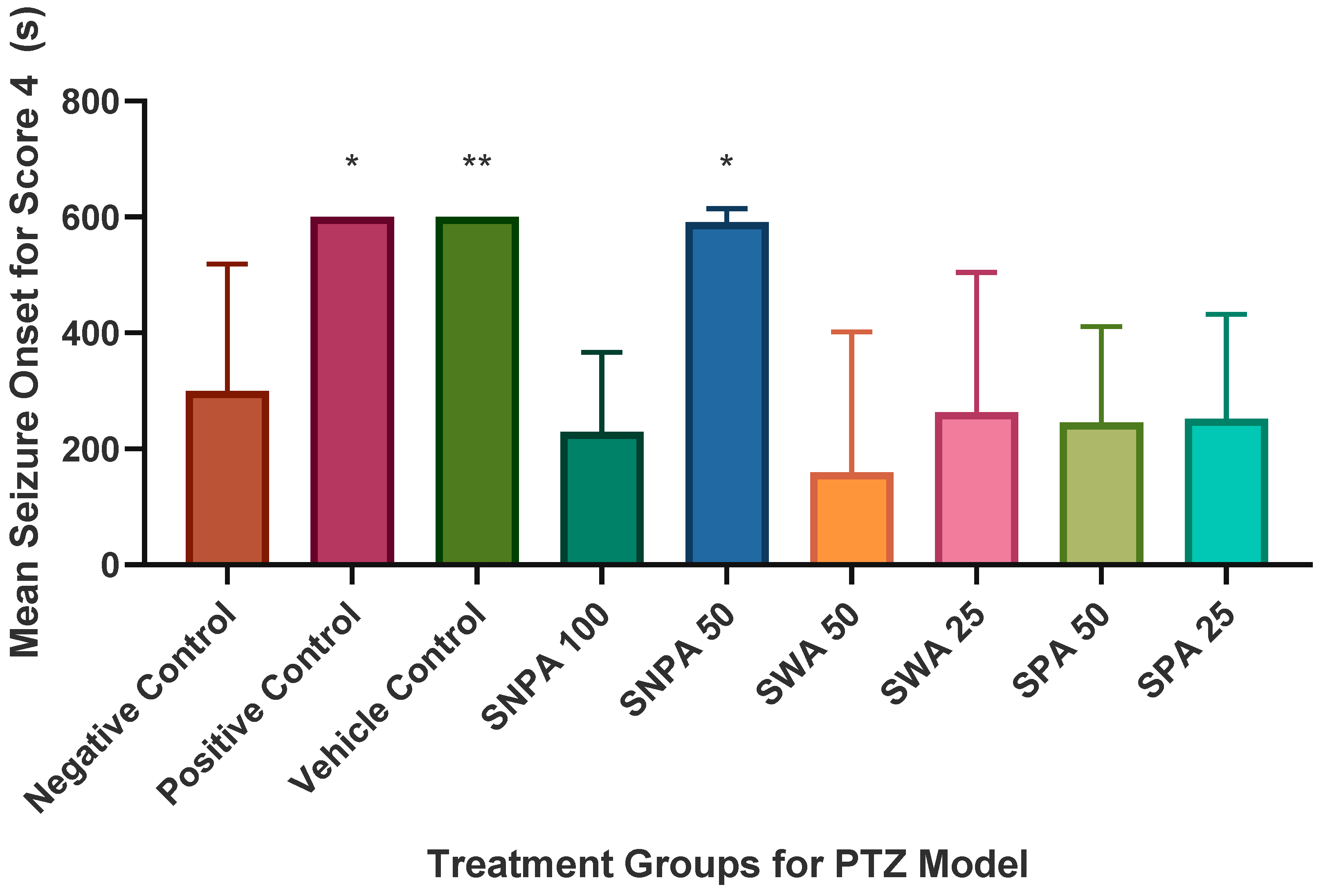
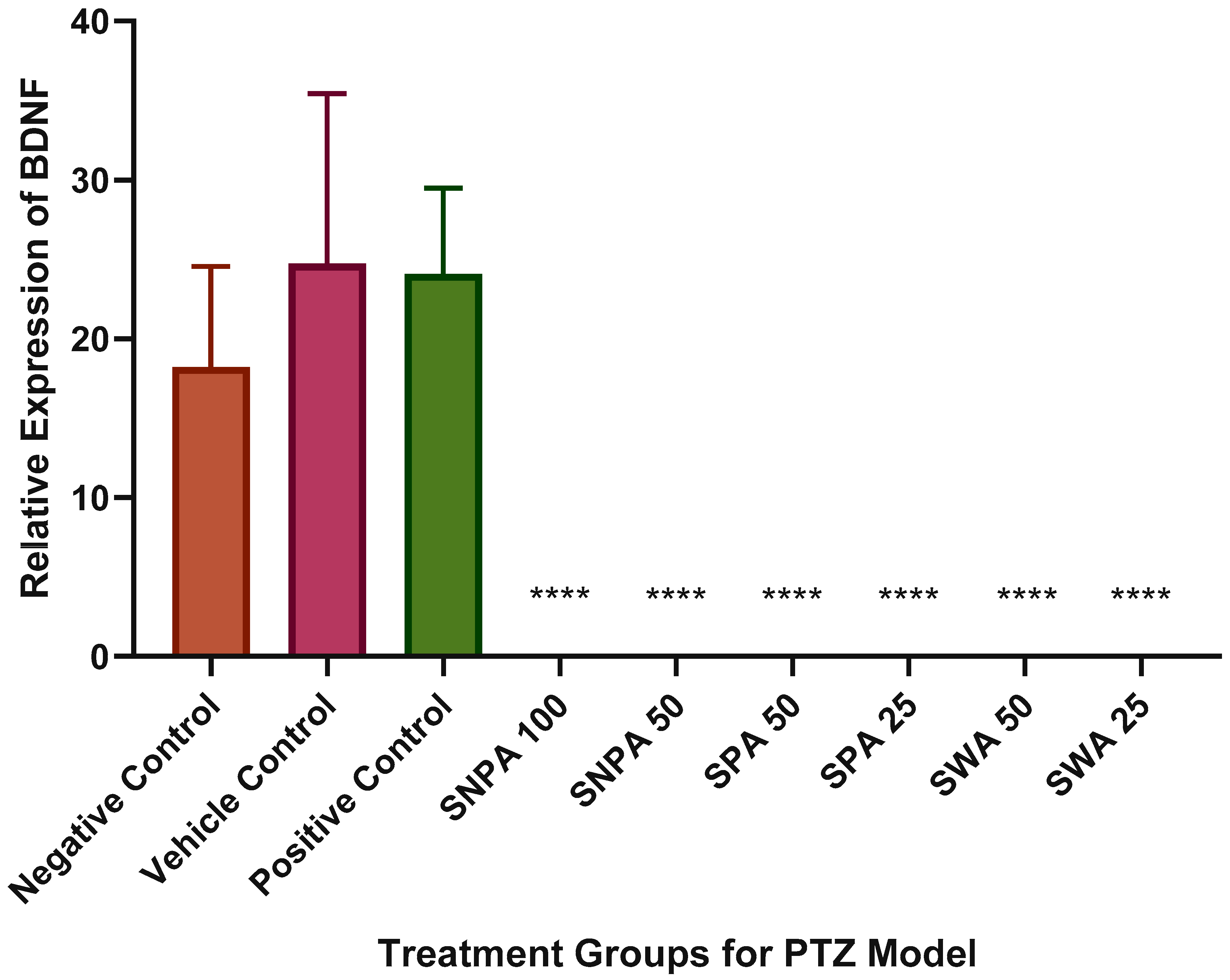
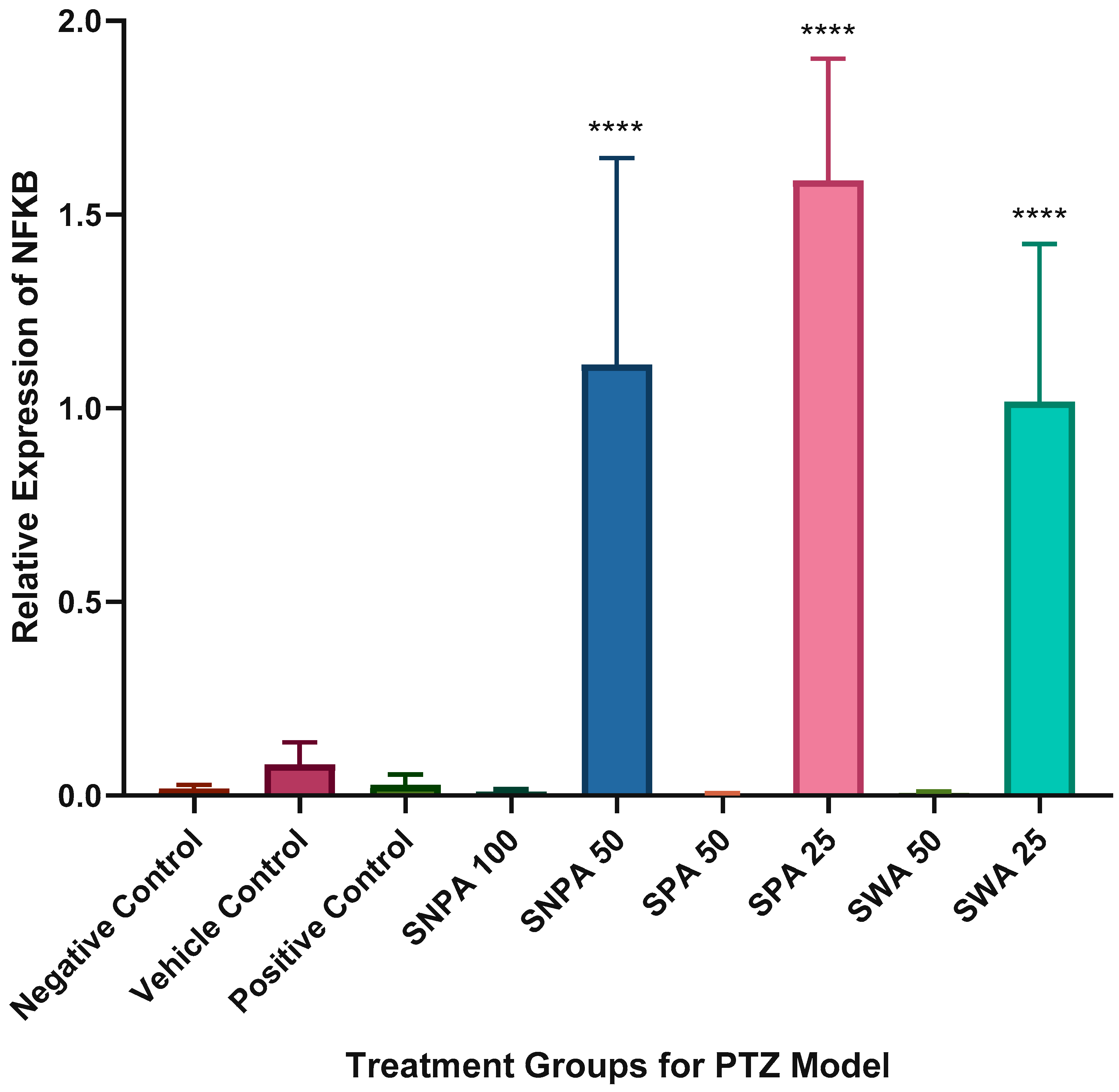
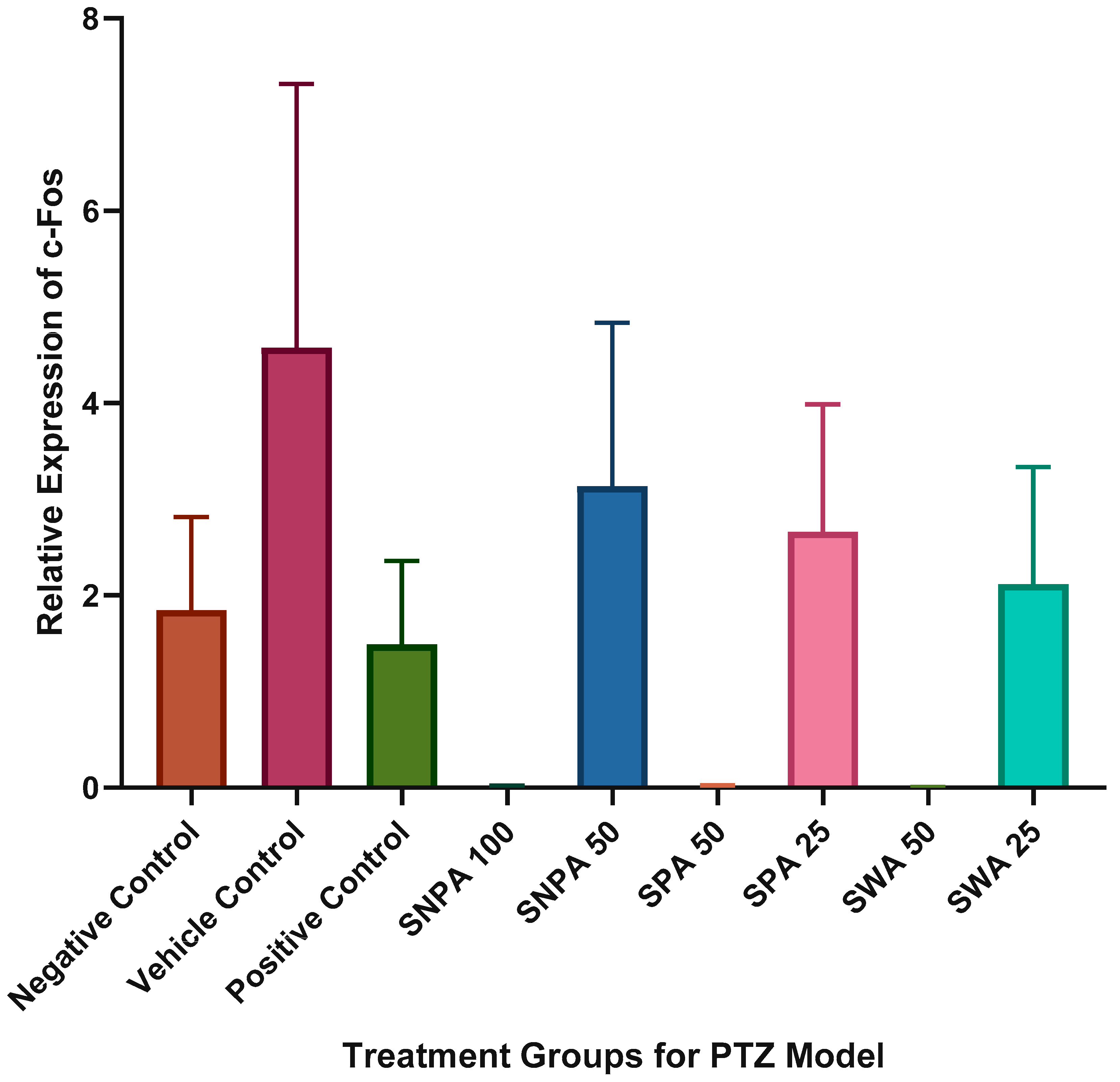
3.2.2. Determination of Seizure Score and Onset Time
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Garrett, K.M.; Basmadjian, G.; Khan, I.A.; Schaneberg, B.T.; Seale, T.W. Extracts of kava (Piper methysticum) induce acute anxiolytic-like behavioral changes in mice. Psychopharmacology 2003, 170, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Gaus, W.; Loew, D. Kava extracts: Safety and risks including rare hepatotoxicity. Phytomedicine 2003, 10, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Schwarzenboeck, A.; Hennermann, K.-H. Kava hepatotoxicity: A clinical survey and critical analysis of 26 suspected cases. Eur. J. Gastroenterol. Hepatol. 2008, 20, 1182–1193. [Google Scholar] [CrossRef] [PubMed]
- Dragull, K.; Yoshida, W.Y.; Tang, C.-S. Piperidine alkaloids from Piper methysticum. Phytochemistry 2003, 63, 193–198. [Google Scholar] [CrossRef]
- Teschke, R. Kava hepatotoxicity: Pathogenetic aspects and prospective considerations. Liver Int. 2010, 30, 1270–1279. [Google Scholar] [CrossRef]
- Brown, A.C.; Onopa, J.; Holck, P.; Kaufusi, P.; Kabasawa, D.; Craig, W.J.; Dragull, K.; Levine, A.M.; Baker, J.D. Traditional kava beverage consumption and liver function tests in a predominantly Tongan population in Hawaii. Clin. Toxicol. 2007, 45, 549–556. [Google Scholar] [CrossRef]
- Backhauss, C.; Krieglstein, J. Extract of kava (Piper methysticum) and its methysticin constituents protect brain tissue against ischemic damage in rodents. Eur. J. Pharmacol. 1992, 215, 265–269. [Google Scholar] [CrossRef]
- Chua, H.C.; Christensen, E.T.H.; Hoestgaard-Jensen, K.; Hartiadi, L.Y.; Ramzan, I.; Jensen, A.A.; Absalom, N.L.; Chebib, M. Kavain, the Major Constituent of the Anxiolytic Kava Extract, Potentiates GABAA Receptors: Functional Characteristics and Molecular Mechanism. PLoS ONE 2016, 11, e0157700. [Google Scholar] [CrossRef]
- Pittler, M.H.; Ernst, E. Efficacy of Kava Extract for Treating Anxiety: Systematic Review and Meta-Analysis. J. Clin. Psychopharmacol. 2000, 20, 84–89. [Google Scholar] [CrossRef]
- Pittler, M.H.; Ernst, E. Kava extract for treating anxiety. Cochrane Database Syst. Rev. 2003. [Google Scholar] [CrossRef]
- OECD. Test. No. 203: Fish., Acute Toxicity Test; OECD Guidelines for the Testing of Chemicals, Section 2; OECD Publishing: Paris, France, 2019. [Google Scholar] [CrossRef]
- Kundap, U.P.; Kumari, Y.; Othman, I.; Shaikh, M.F. Zebrafish as a Model for Epilepsy-Induced Cognitive Dysfunction: A Pharmacological, Biochemical and Behavioral Approach. Front. Pharmacol. 2017, 8, 515. [Google Scholar] [CrossRef] [PubMed]
- Choo, B.K.M.; Kundap, U.P.; Kumari, Y.; Hue, S.-M.; Othman, I.; Shaikh, M.F. Orthosiphon stamineus Leaf Extract Affects TNF-α and Seizures in a Zebrafish Model. Front. Pharmacol. 2018, 9, 139. [Google Scholar] [CrossRef]
- Jhoo, J.-W.; Ang, C.Y.W.; Heinze, T.M.; Deck, J.; Schnackenberg, L.K.; Beger, R.D.; Dragull, K.; Tang, C.-S. Identification of C-glycoside Flavonoids as Potential Mutagenic Compounds in Kava. J. Food Sci. 2007, 72, C120–C125. [Google Scholar] [CrossRef]
- Jhoo, J.-W.; Freeman, J.P.; Heinze, T.M.; Moody, J.D.; Schnackenberg, L.K.; Beger, R.D.; Dragull, K.; Tang, C.-S.; Ang, C.Y.W. In Vitro Cytotoxicity of Nonpolar Constituents from Different Parts of Kava Plant (Piper methysticum). J. Agric. Food Chem. 2006, 54, 3157–3162. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.T.; Dragull, K.; Tang, C.-S.; Bittenbender, H.C.; Efird, J.T.; Nerurkar, P.V. Effects of Kava Alkaloid, Pipermethystine, and Kavalactones on Oxidative Stress and Cytochrome P450 in F-344 Rats. Toxicol. Sci. 2007, 97, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Nerurkar, P.V.; Dragull, K.; Tang, C.-S. In Vitro Toxicity of Kava Alkaloid, Pipermethystine, in HepG2 Cells Compared to Kavalactones. Toxicol. Sci. 2004, 79, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Blaser, R.; Chadwick, L.; McGinnis, G. Behavioral measures of anxiety in zebrafish (Danio rerio). Behav. Brain Res. 2010, 208, 56–62. [Google Scholar] [CrossRef]
- Parker, J.-A.; Kurien, T.T.; Huppatz, C. Hepatitis A outbreak associated with kava drinking. Commun. Dis. Intell. Q. Rep. 2014, 38, 26–28. [Google Scholar]
- Hansen, S.L.; Sperling, B.B.; Sanchez, C. Anticonvulsant and antiepileptogenic effects of GABAA receptor ligands in pentylenetetrazole-kindled mice. Prog. Neuro Psychopharmacol. Boil. Psychiatry 2004, 28, 105–113. [Google Scholar] [CrossRef]
- Hao, F.; Jia, L.-H.; Li, X.-W.; Zhang, Y.-R.; Liu, X.-W. Garcinol Upregulates GABAA and GAD65 Expression, Modulates BDNF-TrkB Pathway to Reduce Seizures in Pentylenetetrazole (PTZ)-Induced Epilepsy. Med. Sci. Monit. 2016, 22, 4415–4425. [Google Scholar] [CrossRef]
- Zhang, H.N.; Ko, M. Seizure activity involved in the up-regulation of BDNF mRNA expression by activation of central Mu opioid receptors. Neuroscience 2009, 161, 301–310. [Google Scholar] [CrossRef] [PubMed]
- Kornblum, H.I.; Sankar, R.; Shin, D.H.; Wasterlain, C.G.; Gall, C.M. Induction of brain derived neurotrophic factor mRNA by seizures in neonatal and juvenile rat brain. Mol. Brain Res. 1997, 44, 219–228. [Google Scholar] [CrossRef]
- Prasad, A.V.; Pilcher, W.H.; Joseph, S.A. Nuclear factor-κB in rat brain: Enhanced DNA-binding activity following convulsant-induced seizures. Neurosci. Lett. 1994, 170, 145–148. [Google Scholar] [CrossRef]
- Barros, V.N.; Mundim, M.V.; Galindo, L.T.; Bittencourt, S.; Porcionatto, M.; Mello, L.E. The pattern of c-Fos expression and its refractory period in the brain of rats and monkeys. Front. Cell. Neurosci. 2015, 9, 72. [Google Scholar] [CrossRef]
- Tawfiq, R.A.; Nassar, N.N.; El-Eraky, W.I.; El-Denshary, E.S. Enhanced efficacy and reduced side effects of diazepam by kava combination. J. Adv. Res. 2013, 5, 587–594. [Google Scholar] [CrossRef]
- Singh, Y.N.; Singh, N.N. Therapeutic Potential of Kava in the Treatment of Anxiety Disorders. CNS Drugs 2002, 16, 731–743. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jaiswal, Y.; Shaikh, M.F.; Wang, I.; Yong, Y.; Lin Lin Lee, V.; Williams, L. Evaluation of Anti-Convulsive Properties of Aqueous Kava Extract on Zebrafish Using the PTZ-Induced Seizure Model. Brain Sci. 2020, 10, 541. https://doi.org/10.3390/brainsci10080541
Jaiswal Y, Shaikh MF, Wang I, Yong Y, Lin Lin Lee V, Williams L. Evaluation of Anti-Convulsive Properties of Aqueous Kava Extract on Zebrafish Using the PTZ-Induced Seizure Model. Brain Sciences. 2020; 10(8):541. https://doi.org/10.3390/brainsci10080541
Chicago/Turabian StyleJaiswal, Yogini, Mohd. Farooq Shaikh, Ilya Wang, Yanning Yong, Vanessa Lin Lin Lee, and Leonard Williams. 2020. "Evaluation of Anti-Convulsive Properties of Aqueous Kava Extract on Zebrafish Using the PTZ-Induced Seizure Model" Brain Sciences 10, no. 8: 541. https://doi.org/10.3390/brainsci10080541
APA StyleJaiswal, Y., Shaikh, M. F., Wang, I., Yong, Y., Lin Lin Lee, V., & Williams, L. (2020). Evaluation of Anti-Convulsive Properties of Aqueous Kava Extract on Zebrafish Using the PTZ-Induced Seizure Model. Brain Sciences, 10(8), 541. https://doi.org/10.3390/brainsci10080541