Risk Calculators in Bipolar Disorder: A Systematic Review
Abstract
1. Introduction
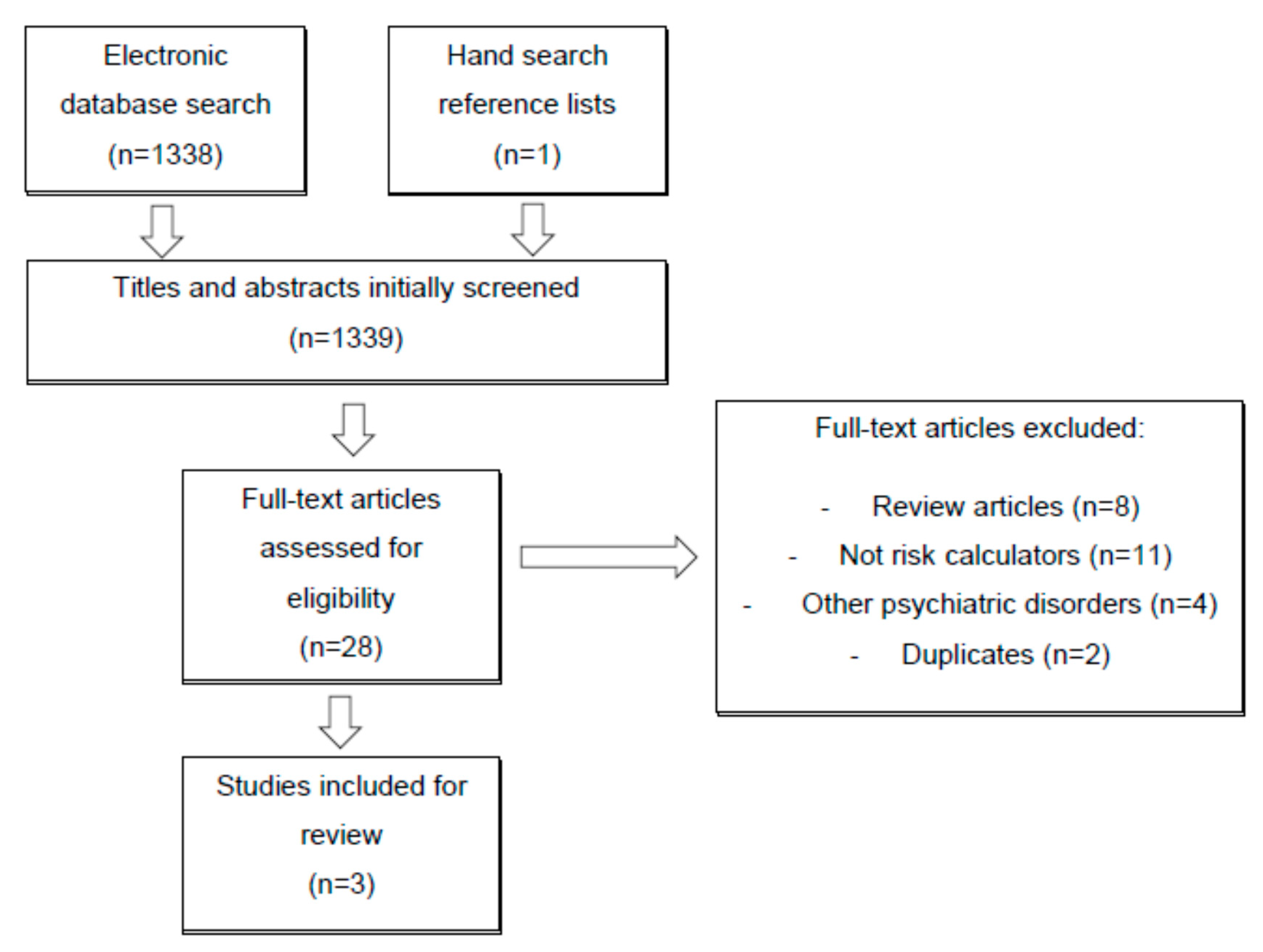
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mantin, D.J.; Smithh, D.J. Is there a clinical prodrome of bipolar disorder? A review of the evidence. Expert Rev. 2013, 13, 89–98. [Google Scholar]
- Bauer, M.; Andreassen, O.A.; Geddes, J.R.; Kessing, L.V.; Lewitzka, U.; Schulze, T.G.; Vieta, E. Areas of uncertainties and unmet needs in bipolar disorders: Clinical and research perspectives. Lancet Psychiatry 2018, 366. [Google Scholar] [CrossRef]
- Vieta, E.; Berk, M.; Schulze, T.G. Bipolar disorders. Nat. Rev. Dis Prim. 2018, 4. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, J.A.; Nelson, B.; Ratheesh, A.; Treen, D.; Mcgorry, P.D. At-risk studies and clinical antecedents of psychosis, bipolar disorder and depression: A scoping review in the context of clinical staging. Psychol. Med. 2018, 49, 177–189. [Google Scholar] [CrossRef]
- Dagani, J.; Signorini, G.; Nielssen, O.; Bani, M.; Pastore, A.; De Girolamo, G.; Large, M. Meta-analysis of the Interval between the onset and management of bipolar disorder. Can. J. Psychiatry 2017, 62, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Grande, I.; Berk, M.; Birmaher, B.; Vieta, E. Bipolar Disorder. Lancet 2016, 387, 1561–1572. [Google Scholar] [CrossRef]
- Phillips, M.L.; Kupfer, D.J. Bipolar disorder diagnosis: Challenges and future directions. Lancet 2013, 381, 1663–1671. [Google Scholar] [CrossRef]
- Malhi, G.S.; Bargh, D.M.; Coulston, C.M.; Das, P.; Berk, M. Predicting bipolar disorder on the basis of phenomenology: Implications for prevention and early intervention. Bipolar Disord. 2014, 16, 455–470. [Google Scholar] [CrossRef]
- Sup, Y.; Hee, I.; Wang, H.; Rim, H. A diagnosis of bipolar spectrum disorder predicts diagnostic conversion from unipolar depression to bipolar disorder: A 5-year retrospective study. J. Affect. Disord. 2015, 174, 83–88. [Google Scholar] [CrossRef]
- Altamura, A.C.; Buoli, M.; Caldiroli, A.; Caron, L.; Melter, C.C.; Dobrea, C.; Cigliobianco, M.; Quarantini, F.Z. Misdiagnosis, duration of untreated illness (DUI) and outcome in bipolar patients with psychotic symptoms: A naturalistic study. J. Affect. Disord. 2015, 182, 70–75. [Google Scholar] [CrossRef]
- Singh, T.; Rajput, M. Misdiagnosis of bipolar disorder. Psychiatry 2006, 57–63. [Google Scholar]
- Murru, A.; Primavera, D.; Oliva, M.; Meloni, M.L.; Vieta, E.; Carpiniello, B. The role of comorbidities in duration of untreated illness for bipolar spectrum disorders. J. Affect. Disord. 2015, 188, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Pinna, M.; Manchia, M. Prognostic models in bipolar disorder: Can the prediction of the long-term clinical course rely on the integration of clinical and molecular data? Biomark. Med. 2014, 8, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Faedda, G.L.; Baldessarini, R.J.; Marangoni, C.; Bechdolf, A.; Berk, M.; Birmaher, B.; Conus, P.; DelBello, M.P.; Duffy, A.; Hillegers, M.H.J.; et al. An international society of bipolar disorders task force report: Precursors and prodromes of bipolar disorder. Bipolar Disord. 2019, 21, 720–740. [Google Scholar] [CrossRef]
- Vieta, E.; Salagre, E.; Grande, I.; Carvalho, A.F.; Fernandes, B.S.; Berk, M.; Birmaher, B.; Tohen, M.; Suppes, T. Early intervention in bipolar disorder. Am. J. Psychiatry 2018, 175, 411–426. [Google Scholar] [CrossRef]
- Van Meter, A.R.; Burke, C.; Youngstrom, E.A.; Faedda, G.L.; Christoph, U.; Correll, M. The bipolar prodrome meta-analyses of symptom prevalence prior to initial or recurrent mood episodes. J. Am. Acad Child. Adolesc. Psychiatry 2016, 55, 543–555. [Google Scholar] [CrossRef]
- Ratheesh, A.; Davey, C.; Hetrick, S.; Alvarez-Jimenez, M.; Voutier, C.; Bechdolf, A.; McGorry, P.D.; Scott, J.; Berk, M.; Cotton, S.M. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr. Scand. 2017, 135, 273–284. [Google Scholar] [CrossRef]
- Birmaher, B.; Merranko, J.A.; Goldstein, T.R.; Gill, M.K.; Goldstein, B.I.; Hower, H.; Yen, S.; Hafeman, D.; Strober, M.; Diler, R.S.; et al. A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. J. Am. Acad Child. Adolesc. Psychiatry 2018, 57, 755–763.e4. [Google Scholar] [CrossRef]
- Cannon, T.D.; Yu, C.; Addington, J.; Bearden, C.E.; Cadenhead, K.S.; Cornblatt, B.A.; Heinssen, R.; Jeffries, C.D.; Mathalon, D.H.; McGlashan, T.H.; et al. An individualized risk calculator for research in prodromal psychosis. Am. J. Psychiatry 2016, 173, 980–988. [Google Scholar] [CrossRef]
- Harrell, F.E., Jr.; Lee, K.L.; Mark, D.B. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat. Med. 1996, 15, 361–387. [Google Scholar] [CrossRef]
- Vigo, D.; Thornicroft, G.; Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016, 3, 171–178. [Google Scholar] [CrossRef]
- Bernardini, F.; Attademo, L.; Cleary, S.D.; Luther, C.; Shim, R.S.; Quartesan, R.; Compton, M.T. Risk prediction models in psychiatry: Toward a new frontier for the prevention of mental illness. J. Clin. Psychiatry 2017, 78, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Werbeloff, N.; Rutigliano, G.; Oliver, D.; Davies, C.; Stahl, D.; McGuire, P.; Osborn, D. Transdiagnostic risk calculator for the automatic detection of individuals at risk and the prediction of Psychosis: Second replication in an independent national health service trust. Schizophr Bull. 2019, 45, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Robertson, J.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses; The Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2013. [Google Scholar]
- Macaskill, P.; Steyerberg, E.W.; Vickers, A.J.; Ransohoff, D.F.; Collins, G.S. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis ( TRIPOD ): Explanation and elaboration. Ann. Intern. Med. 2015, 162, W1–W73. [Google Scholar] [CrossRef]
- Gan, Z.; Diao, F.; Wei, Q.; Wu, X.; Cheng, M.; Guan, N.; Zhang, M.; Zhang, J.-B. A predictive model for diagnosing bipolar disorder based on the clinical characteristics of major depressive episodes in Chinese population. J. Affect. Disord. 2011, 134, 119–125. [Google Scholar] [CrossRef]
- Hafeman, D.M.; Merranko, J.; Goldstein, T.R.; Axelson, D.; Goldstein, B.I.; Monk, K.; Hickey, M.B.; Sakolsky, D.; Diler, R.S.; Iyengar, S.; et al. Assessment of a person-level risk calculator to predict new-onset bipolar spectrum disorder in youth at familial risk. JAMA Psychiatry 2017, 15213, 1–7. [Google Scholar] [CrossRef]
- Moons, K.G.; Kengne, A.P.; Grobbee, D.E.; Royston, P.; Vergouwe, Y.; Altman, U.G.; Woodward, M. Risk prediction models: II. External validation, model updating, and impact assessment. Heart 2012, 98, 691–698. [Google Scholar] [CrossRef]
- Moons, K.G.; Kengne, A.P.; Woodward, M.; Royston, P.; Vergouwe, Y.; Altman, U.G.; Grobbee, D.E. Risk prediction models: I. Development, internal validation, and assessing the incremental value of a new (bio) marker. Heart 2012, 98, 683–690. [Google Scholar] [CrossRef]
- Salagre, E.; Dodd, S.; Aedo, A.; Rosa, A.; Amoretti, S.; Pinzon, J.; Reinares, M.; Berk, M.; Kapczinski, F.P.; Vieta, E.; et al. Toward precision psychiatry in bipolar disorder: Staging 2.0. Front. Psychiatry 2018, 9, 641. [Google Scholar] [CrossRef]
- Fusar-poli, P.; Hijazi, Z.; Stahl, D.; Steyerberg, E.W. The science of prognosis in psychiatry a review. JAMA Psychiatry 2018, 75, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Hijazi, Z.; Stahl, D.; Steyerberg, E.W. Early intervention in bipolar disorder. Am. J. Psychiatry 2018, 175, 411–426. [Google Scholar]
- DelBello, M. A risk calculator for bipolar disorder in youth: Improving the odds for personalized prevention and early intervention? J. Am. Acad Child. Adolesc Psychiatry 2018, 57, 10. [Google Scholar] [CrossRef] [PubMed]
- Grande, I.; Magalhães, P.V.; Chendo, I.; Stertz, L.; Panizutti, B.; Colpo, G.D.; Rosa, A.R.; Gama, C.S.; Kapczinski, F.; Vieta, E. Staging bipolar disorder: Clinical, biochemical, and functional correlates. Acta Psychiatr Scand. 2014, 129, 437–444. [Google Scholar] [CrossRef]
- Rowland, T.; Perry, B.I.; Upthegrove, R.; Barnes, N.; Chatterjee, J.; Gallacher, D.; Marwaha, S. Neurotrophins, cytokines, oxidative stress mediators and mood state in bipolar disorder: Systematic review and meta-analyses. Br. J. Psychiatry 2018, 213, 514–525. [Google Scholar] [CrossRef]
- Oliveira, P.M.S.; Oliveira, P.; Coroa, M.; Ribeiro, J.; Madeira, N.G.G.F. Serum uric acid as a predictor of bipolarity in individuals with a major depressive episode. Bipolar Disord 2018, 21, 235–243. [Google Scholar] [CrossRef]
- Carvalho, A.F.; Firth, J.; Vieta, E. Bipolar Disorder. N. Engl. J. Med. 2020, 383, 58–66. [Google Scholar] [CrossRef]
- Kapczinski, F.; Magalhães, P.V.S.; Martinez, V.B.; Dias, V.V.; Frangou, S.; Gama, C.S.; Pinto, A.G.; Grande, I.; Ha, K.; Kauer-Sant’Anna, M.; et al. Staging systems in bipolar disorder: An international society for bipolar disorders task force report. Acta Psychiatr. Scand. 2014, 130, 354–363. [Google Scholar] [CrossRef]
| Article | Sample Characteristics | Variables Included in the Model | Variables Assessment | Risk Prediction Statistics | Classification Statistics | Main Conclusions/Outcomes | Limitations |
|---|---|---|---|---|---|---|---|
| Gan et al. (2011) | N = 344 patients with major depressive episodes; 268 completing 1-year follow-up Proportion of the outcome = 63% (n = 169) | Age at first onset Maximum duration of depressive episodes Somatalgia Hypersomnia Diurnal variation of mood Irritability | Questionnaire designed by the researchers | SRD = 0.70 AUC = 0.85 | PPV = 0.87 NPV = 0.67 SEN = 75% SPE = 83% | The model based on six clinical characteristics robustly predict the transition from major depressive episodes to BP. | Short follow-up period; possibility of selection bias; the anti-depressant treatment was not assessed; without external validation. |
| Hafeman et al. (2017) | N = 412 Bipolar at-risk (offspring of BP I and II) completing 5-year follow-up | Mania Depression Anxiety Emotional lability Functioning Offspring age at visit Parental age at mood disorder onset | 1. Modified K-SADS Mania Rating Scale (KMRS) 2. Depression items from K-SADS–Present Version (KDRS)-Modified 3. SCARED-Screen for Child Anxiety Related Emotional Disorders (child reported) 4. CALS-Children’s Affective Lability Scale (child reported) 5. CGAS-Children’s Global Assessment Scale | AUC = 0.76 | Risk Score Cutoff 0.5: PPV = 0.15 SEN = 0.82 SPE = 0.49 Risk Score Cutoff 0.10: PPV = 0.22 SEN = 0.53 SPE = 0.80 Risk Score Cutoff 0.15: PPV = 0.30 SEN = 0.37 SPE = 0.91 Risk Score Cutoff 0.20: PPV = 0.32 SEN = 0.21 SPE = 0.95 | A model based on anxiety, manic symptoms, depressive symptoms, mood lability, poor general psychosocial functioning, and earlier parental age at onset individually and collectively assessed the probability of new-onset BPSD within the next 5 years in a population at familial risk for BP. | Few youths were diagnosed with BP I or II; Follow-up visits scheduled every 2 years without external validation. |
| Birmaher et al. (2018) | N = 140 BP-NOS; 120 completing 5-year follow-up | Mania Depression Anxiety Emotional lability Functioning Duration of Bipolar Illness (Years) Child’s Age Race Family History of Mania Gender | 1. Modified KMRS (K-SADS Mania Rating Scale) 2. Modified KDRS (K-SADS–Present Version) 3. SCARED-Screen for Child Anxiety Related Emotional Disorders (child reported) 4. CALS-Children’s Affective Lability Scale (child reported) 5. CGAS-Children’s Global Assessment Scale | AUC = 0.71 | Risk Score Cutoff 0.20: PPV = 0.46 NPV = 0.85 SEN = 0.86 SPE = 0.44 Risk Score Cutoff 0.25: PPV = 0.52 NPV = 0.81 SEN = 0.75 SPE = 0.61 Risk Score Cutoff 0.30: PPV = 0.56 NPV = 0.77 SEN = 0.62 SPE = 0.72 Risk Score Cutoff 0.35: PPV = 0.60 NPV = 0.73 SEN = 0.47 SPE = 0.82 Risk Score Cutoff 0.40: PPV = 0.65 NPV = 0.71 SEN = 0.36 SPE = 0.89 | A model based on family history of hypo/mania and elevated levels of manic, mood lability, and anxiety symptoms can predict the conversion risk from BP-NOS to BP I or II in patients ages 6–17 years old. Results were externally validated in a sample recruited from the community (BIOS) with an even stronger discrimination (75%). If the conversion did not occur within four years of the initial BP-NOS diagnosis, the risk dropped considerably. | Majority of participants were Caucasian recruited from clinical settings; the presence of factors associated with high-risk for conversion are not stable and may change over time |
| Gan et al. | Hafeman et al. | Birmaher et al. | ||
|---|---|---|---|---|
| SELECTION | 1. Representativeness of the exposed cohort | Selected group | Selected group | Selected group |
| 2. Selection of the non-exposed cohort | Same community as the exposed cohort (⁕) | Same community as the exposed cohort (⁕) | Same community as the exposed cohort (⁕) | |
| 3. Ascertainment of exposure | Structured interview (⁕) | Structured interview (⁕) | Structured interview (⁕) | |
| 4. Demonstration that outcome of interest was not present at start of study | Yes (⁕) | Yes (⁕) | Yes (⁕) | |
| COMPARABILITY | 1. Comparability of cohorts based on design or analysis controlled for confounders | Study controls for age and other different sociodemographic and clinical factors (⁕⁕) | Study controls for other different sociodemographic and clinical factors (⁕) | Study controls for other different sociodemographic and clinical factors (⁕) |
| OUTCOME | 1. Assessment of outcome | Independent blind assessment (⁕) | No description | Independent blind assessment (⁕) |
| 2. Follow-up long enough for outcomes to occur (Indicate the median duration) | No (1 year follow-up) | Yes (⁕) (median of 9.5 years) | Yes (⁕) (median of 11.5 years) | |
| 3. Adequacy of follow-up of cohorts | Subjects lost to follow up unlikely to introduce bias (⁕) | No statement | No statement | |
| RESULT | Good Quality | Good Quality | Good Quality |
| Section/Topic | Item | Checklist Item | Gan et al. | Hafeman et al. | Birmaher et al. |
|---|---|---|---|---|---|
| Title and abstract | |||||
| Title | 1 | Identify the study as developing and/or validating a multivariable prediction model, the target population, and the outcome to be predicted. | ✓ | ✓ | ✓ |
| Abstract | 2 | Provide a summary of objectives, study design, setting, participants, sample size, predictors, outcome, statistical analysis, results, and conclusions. | ✓ | ✓ | ✓ |
| Introduction | |||||
| Background and objectives | 3a | Explain the medical context (including whether diagnostic or prognostic) and rationale for developing or validating the multivariable prediction model, including references to existing models. | ✓ | ✓ | ✓ |
| 3b | Specify the objectives, including whether the study describes the development or validation of the model or both. | ✓ | ✓ | ✓ | |
| Methods | |||||
| Source of data | 4a | Describe the study design or source of data (e.g., randomized trial, cohort, or registry data), separately for the development and validation data sets, if applicable. | ✓ | ✓ | ✓ |
| 4b | Specify the key study dates, including start of accrual; end of accrual; and, if applicable, end of follow-up. | ✓ | ✓ | ✓ | |
| Participants | 5a | Specify key elements of the study setting (e.g., primary care, secondary care, general population) including number and location of centers. | ✓ | ✓ | ✓ |
| 5b | Describe eligibility criteria for participants. | ✓ | ✓ | ✓ | |
| 5c | Give details of treatments received, if relevant. | n/a | n/a | n/a | |
| Outcome | 6a | Clearly define the outcome that is predicted by the prediction model, including how and when assessed. | ✓ | ✓ | ✓ |
| 6b | Report any actions to blind assessment of the outcome to be predicted. | ✓ | ✓ | ✓ | |
| Predictors | 7a | Clearly define all predictors used in developing or validating the multivariable prediction model, including how and when they were measured. | ✓ | ✓ | ✓ |
| 7b | Report any actions to blind assessment of predictors for the outcome and other predictors. | ✓ | ✓ | ✓ | |
| Sample size | 8 | Explain how the study size was arrived at. | ✓ | ✓ | ✓ |
| Missing data | 9 | Describe how missing data were handled (e.g., complete-case analysis, single imputation, multiple imputation) with details of any imputation method. | ✓ | ✓ | ✓ |
| Statistical analysis methods | 10a | Describe how predictors were handled in the analyses | ✓ | ✓ | ✓ |
| 10b | Specify type of model, all model-building procedures (including any predictor selection), and method for internal validation | ✓ | ✓ | ✓ | |
| 10c | For validation, describe how the predictions were calculated. | n/a | n/a | ✓ | |
| 10d | Specify all measures used to assess model performance and, if relevant, to compare multiple models. | ✓ | ✓ | ✓ | |
| 10e | Describe any model updating (e.g., recalibration) arising from the validation, if done. | n/a | n/a | n/a | |
| Risk groups | 11 | Provide details on how risk groups were created, if done. | n/a | ✓ | ✓ |
| Development vs. validation | 12 | For validation, identify any differences from the development data in setting, eligibility criteria, outcome, and predictors. | n/a | n/a | ✓ |
| Results | |||||
| Participants | 13a | Describe the flow of participants through the study, including the number of participants with and without the outcome and, if applicable, a summary of the follow-up time. A diagram may be helpful. | ✓ | ✓ | ✓ |
| 13b | Describe the characteristics of the participants (basic demographics, clinical features, available predictors), including the number of participants with missing data for predictors and outcome. | ✓ | ✓ | ✓ | |
| 13c | For validation, show a comparison with the development data of the distribution of important variables (demographics, predictors and outcome). | n/a | n/a | ✓ | |
| Model development | 14a | Specify the number of participants and outcome events in each analysis | ✓ | ✓ | ✓ |
| 14b | If done, report the unadjusted association between each candidate predictor and outcome | ✓ | ✓ | ✓ | |
| Model specification | 15a | Present the full prediction model to allow predictions for individuals (i.e., all regression coefficients, and model intercept or baseline survival at a given time point) | ✓ | ✓ | ✓ |
| 15b | Explain how to use the prediction model | ✓ | ✓ | ✓ | |
| Model performance | 16 | Report performance measures (with CIs) for the prediction model | ✓ | ✓ | ✓ |
| Model updating | 17 | If done, report the results from any model updating (i.e., model specification, model performance) | n/a | n/a | n/a |
| Discussion | |||||
| Limitations | 18 | Discuss any limitations of the study (such as nonrepresentative sample, few events per predictor, missing data). | ✓ | ✓ | ✓ |
| Interpretation | 19a | For validation, discuss the results with reference to performance in the development data, and any other validation data. | n/a | n/a | ✓ |
| 19b | Give an overall interpretation of the results, considering objectives, limitations, results from similar studies, and other relevant evidence. | ✓ | ✓ | ✓ | |
| Implications | 20 | Discuss the potential clinical use of the model and implications for future research. | ✓ | ✓ | ✓ |
| Other information | |||||
| Supplementary information | 21 | Provide information about the availability of supplementary resources, such as study protocol, Web calculator, and data sets. | ✓ | ✓ | ✓ |
| Funding | 22 | Give the source of funding and the role of the funders for the present study. | ✓ | ✓ | ✓ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva Ribeiro, J.; Pereira, D.; Salagre, E.; Coroa, M.; Santos Oliveira, P.; Santos, V.; Madeira, N.; Grande, I.; Vieta, E. Risk Calculators in Bipolar Disorder: A Systematic Review. Brain Sci. 2020, 10, 525. https://doi.org/10.3390/brainsci10080525
Silva Ribeiro J, Pereira D, Salagre E, Coroa M, Santos Oliveira P, Santos V, Madeira N, Grande I, Vieta E. Risk Calculators in Bipolar Disorder: A Systematic Review. Brain Sciences. 2020; 10(8):525. https://doi.org/10.3390/brainsci10080525
Chicago/Turabian StyleSilva Ribeiro, Joana, Daniela Pereira, Estela Salagre, Manuel Coroa, Pedro Santos Oliveira, Vítor Santos, Nuno Madeira, Iria Grande, and Eduard Vieta. 2020. "Risk Calculators in Bipolar Disorder: A Systematic Review" Brain Sciences 10, no. 8: 525. https://doi.org/10.3390/brainsci10080525
APA StyleSilva Ribeiro, J., Pereira, D., Salagre, E., Coroa, M., Santos Oliveira, P., Santos, V., Madeira, N., Grande, I., & Vieta, E. (2020). Risk Calculators in Bipolar Disorder: A Systematic Review. Brain Sciences, 10(8), 525. https://doi.org/10.3390/brainsci10080525






