Evidence-Based Physical Therapy for Individuals with Rett Syndrome: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Eligibility Criteria and Report Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
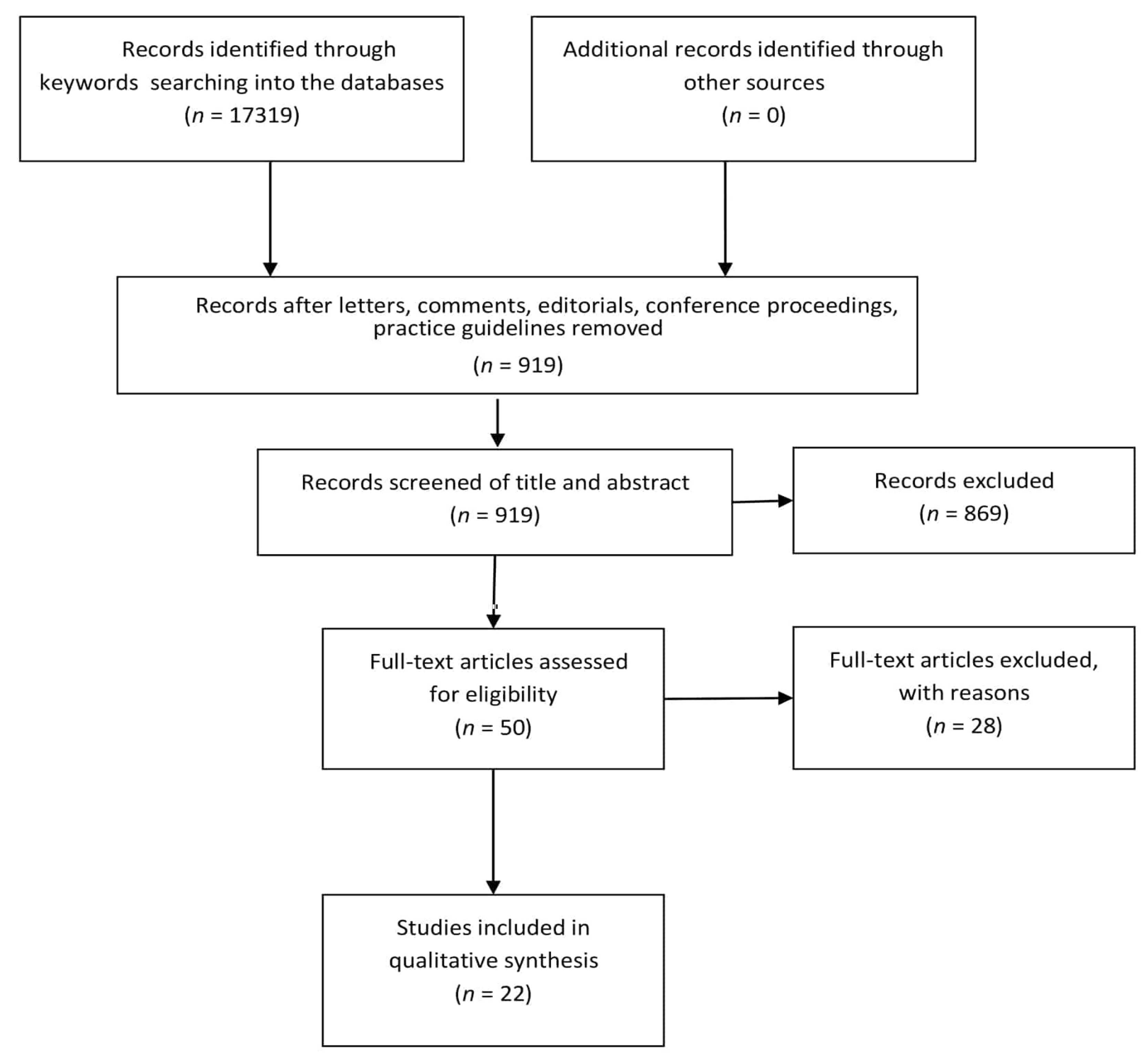
2.4. Study Selection
2.5. Data Collection Process
2.6. Level of Evidence Assessment Process
3. Results
3.1. Applied Behavior Analysis (ABA)
3.2. Conductive Education (CE)
3.3. Environmental Enrichment (EE)
3.4. Traditional Physical Therapy with or without Aids
3.5. Hydrotherapy
3.6. Treadmill
3.7. Music Therapy
3.8. Computerized Systems
3.9. Sensory-Based Treatment (Snoezelen)
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gold, W.A.; Krishnarajy, R.; Ellaway, C.; Christodoulou, J. Rett Syndrome: A Genetic Update and Clinical Review Focusing on Comorbidities. ACS Chem. Neurosci. 2018, 9, 167–176. [Google Scholar] [CrossRef]
- Percy, A.K. Rett Syndrome: Seeing the Way Forward. In Health Care for People with Intellectual and Developmental. Disabilities Across the Lifespan, 3rd ed.; Rubin, I.L., Merrick, J., Greydanus, D.E., Patel, D.R., Eds.; Springer: Cham, Switzerland, 2016; pp. 765–777. ISBN 978-3-319-18096-0. [Google Scholar]
- Vidal, S.; Xiol, C.; Pascual-Alonso, A.; O’Callaghan, M.; Pineda, M.; Armstrong, J. Genetic Landscape of Rett Syndrome Spectrum: Improvements and Challenges. Int. J. Mol. Sci. 2019, 20, 3925. [Google Scholar] [CrossRef] [PubMed]
- Feldman, D.; Banerjee, A.; Sur, M. Developmental Dynamics of Rett Syndrome. Neural Plast. 2016, 2016, 6154080. [Google Scholar] [CrossRef] [PubMed]
- Liyanage, V.R.; Rastegar, M. Rett syndrome and MeCP2. Neuromol. Med. 2014, 16, 231–264. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.R.; Bird, A.P. MeCP2 mutations: Progress towards understanding and treating Rett syndrome. Genome Med. 2017, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Hanefeld, F. The clinical pattern of the Rett syndrome. Brain Dev. 1985, 7, 320–325. [Google Scholar] [CrossRef]
- Leven, Y.; Wiegand, F.; Wilken, B. Sleep Quality in Children and Adults with Rett Syndrome. Neuropediatrics 2020, 6. [Google Scholar] [CrossRef]
- Bianco, E.; Rota, D. Oral findings in Rett syndrome: An update and review of the literature. Dent. Med. Probl. 2018, 55, 441–445. [Google Scholar] [CrossRef]
- Henriksen, M.W.; Breck, H.; Von Tetzchner, S.; Paus, B.; Skjeldal, O.H.; Brodtkorb, E. Epilepsy in classic Rett syndrome: Course and characteristics in adult age. Epilepsy Res. 2018, 145, 134–139. [Google Scholar] [CrossRef]
- Tarquinio, D.C.; Hou, W.; Neul, J.L.; Berkmen, G.K.; Drummond, J.; Aronoff, E.; Harris, J.; Lane, J.B.; Kaufmann, W.E.; Motil, K.J.; et al. The course of awake breathing disturbances across the lifespan in Rett syndrome. Brain Dev. 2018, 40, 515–529. [Google Scholar] [CrossRef]
- National Organization for Rare Disorders. Available online: https://rarediseases.org/rare-diseases/rett-syndrome/ (accessed on 30 December 2019).
- Killian, J.T.; Lane, J.B.; Lee, H.S.; Skinner, S.A.; Kaufmann, W.E.; Glaze, D.G.; Neul, J.L.; Percy, A.K. Scoliosis in Rett Syndrome: Progression, Comorbidities, and Predictors. Pediatr. Neurol. 2017, 70, 20–25. [Google Scholar] [CrossRef]
- Jefferson, A.; Leonard, H.; Siafarikas, A.; Woodhead, H.; Fyfe, S.; Ward, L.M.; Munns, C.; Motil, K.; Tarquinio, D.; Shapiro, J.R.; et al. Clinical Guidelines for Management of Bone Health in Rett Syndrome Based on Expert Consensus and Available Evidence. PLoS ONE 2016, 11, e0146824. [Google Scholar] [CrossRef] [PubMed]
- Townend, G.S.; Van De Berg, R.; De Breet, L.; Hiemstra, M.; Wagter, L.; Smeets, E.; Widdershoven, J.; Kingma, H.; Curfs, L. Oculomotor Function in Individuals with Rett Syndrome. Pediatr. Neurol. 2018, 88, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Lotan, M.; Zysman, L. The digestive system and nutritional considerations for individuals with Rett syndrome. Sci. World J. 2006, 6, 1737–1749. [Google Scholar] [CrossRef] [PubMed]
- Kirby, R.S.; Lane, J.B.; Childers, J.; Skinner, S.A.; Annese, F.; Barrish, J.O.; Glaze, D.G.; Macleod, P.; Percy, A.K. Longevity in Rett syndrome: Analysis of the North American Database. J. Pediatr. 2010, 156, 135–138. [Google Scholar] [CrossRef]
- Ellaway, C.; Christodoulou, J. Rett syndrome: Clinical characteristics and recent genetic advances. Disabil. Rehabil. 2001, 23, 98–106. [Google Scholar] [CrossRef]
- Lotan, M. Rett Syndrome. Guidelines for Individual Intervention. Sci. World J. 2006, 6, 1504–1516. [Google Scholar] [CrossRef]
- Cup, E.H.; Pieterse, A.J.; Ten Broek-Pastoor, J.M.; Munneke, M.; Van Engelen, B.G.; Hendricks, H.T.; Van Der Wilt, G.J.; Oostendorp, R.A. Exercise therapy and other types of physical therapy for patients with neuromuscular diseases: A systematic review. Arch. Phys. Med. Rehabil. 2007, 88, 1452–1464. [Google Scholar] [CrossRef]
- Johnson, L.B.; Florence, J.M.; Abresch, R.T. Physical therapy evaluation and management in neuromuscular diseases. Phys. Med. Rehabil. Clin. N. Am. 2012, 23, 633–651. [Google Scholar] [CrossRef]
- Corrado, B.; Ciardi, G. Facioscapulohumeral distrophy and physiotherapy: A literary review. J. Phys. Ther. Sci. 2015, 27, 2381–2385. [Google Scholar] [CrossRef]
- Corrado, B.; Ciardi, G.; Bargigli, C. Rehabilitation Management of the Charcot-Marie-Tooth Syndrome: A Systematic Review of the Literature. Medicine 2016, 95, e3278. [Google Scholar] [CrossRef] [PubMed]
- Corrado, B.; Ciardi, G.; Iammarrone, C.S. Rehabilitation management of Pompe disease, from childhood trough adulthood: A systematic review of the literature. Neurol. Int. 2019, 11, 7983. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.M.; Cassidy, E.E.; Noorduyn, S.G.; O’Connell, N.E. Exercise interventions for cerebral palsy. Cochrane Database Syst. Rev. 2017, 6, CD011660. [Google Scholar] [CrossRef] [PubMed]
- Quinn, L.; Busse, M.; Carrier, J.; Fritz, N.; Harden, J.; Hartel, L.; Kegelmeyer, D.; Kloos, A.; Rao, A. Physical therapy and exercise interventions in Huntington’s disease: A mixed methods systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 1783–1799. [Google Scholar] [CrossRef] [PubMed]
- Corrado, B.; Sommella, N.; Ciardi, G.; Raiano, E.; Scala, I.; Strisciuglio, P.; Servodio Iammarrone, C. Can early physical therapy positively affect the onset of independent walking in infants with Down syndrome? A retrospective cohort study. Minerva Pediatr. 2018. [Google Scholar] [CrossRef]
- Corrado, B.; Ciardi, G.; Fortunato, L.; Servodio Iammarrone, C. Burnout syndrome among Italian physiotherapists: A cross-sectional study. Eur. J. Physiother. 2019, 21, 240–245. [Google Scholar] [CrossRef]
- Silva, I.S.; Pedrosa, R.; Azevedo, I.G.; Forbes, A.M.; Fregonezi, G.A.; Dourado, M.E., Jr.; Lima, S.R.; Ferreira, G.M. Respiratory muscle training in children and adults with neuromuscular disease. Cochrane Database Syst. Rev. 2019, 9, CD011711. [Google Scholar] [CrossRef]
- Bartels, B.; Montes, J.; Van Der Pol, W.L.; De Groot, J.F. Physical exercise training for type 3 spinal muscular atrophy. Cochrane Database Syst. Rev. 2019, 3, CD012120. [Google Scholar] [CrossRef]
- Vola, E.A.; Albano, M.; Di Luise, C.; Servodidio, V.; Sansone, M.; Russo, S.; Corrado, B.; Servodio Iammarrone, C.; Caprio, M.G.; Vallone, G. Use of ultrasound shear wave to measure muscle stiffness in children with cerebral palsy. J. Ultrasound 2018, 21, 241–247. [Google Scholar] [CrossRef]
- Corrado, B.; Di Luise, C.; Servodio Iammarrone, C. Management of Muscle Spasticity in Children with Cerebral Palsy by Means of Extracorporeal Shockwave Therapy: A Systematic Review of the Literature. Dev. Neurorehabil. 2019, 1–7. [Google Scholar] [CrossRef]
- Santos, C.M.D.C.; Pimenta, C.A.D.M.; Nobre, M.R.C. The PICO strategy for the research question construction and evidence search. Rev. Lat. Am. Enferm. 2007, 15, 508–511. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- OCEBM Levels of Evidence Working Group. OCEBM Levels of Evidence. Available online: http://www.cebm.net/index.aspx?o=5653 (accessed on 30 December 2019).
- Larsson, G.; Engerström, I.W. Gross motor ability in Rett syndrome-the power of expectation, motivation and planning. Brain Dev. 2001, 23, S77–S81. [Google Scholar] [CrossRef]
- Yasuhara, A.; Sugiyama, Y. Music therapy for children with Rett syndrome. Brain Dev. 2001, 23, S82–S84. [Google Scholar] [CrossRef]
- Bumin, G.; Uyanik, M.; Yilmaz, I.; Kayihan, H.; Topçu, M. Hydrotherapy for Rett Syndrome. J. Rehabil. Med. 2003, 35, 44–45. [Google Scholar] [CrossRef] [PubMed]
- Lotan, M.; Isakov, E.; Merrick, J. Improving functional skills and physical fitness in children with Rett syndrome. J. Intellect. Disabil. 2004, 48, 730–735. [Google Scholar] [CrossRef] [PubMed]
- Elefant, C.; Lotan, M. Rett Syndrome: Dual Intervention—Music and Physical Therapy. Nord J. Music Ther. 2004, 13, 172–182. [Google Scholar] [CrossRef]
- Lotan, M.; Merrick, J.; Carmeli, E. Managing Scoliosis in a Young Child with Rett Syndrome: A Case Study. Sci. World J. 2005, 5, 264–273. [Google Scholar] [CrossRef]
- Lotan, M. Management of Rett Syndrome in the Controlled Multisensory (snoezelen) Environment. A Review with Three Case Stories. Sci. World J. 2006, 6, 791–807. [Google Scholar] [CrossRef]
- Lotan, M. Alternative Therapeutic Intervention for Individuals with Rett Syndrome. Sci. World J. 2007, 7, 698–714. [Google Scholar] [CrossRef]
- Pizzamiglio, M.R.; Nasti, M.; Piccardi, L.; Zotti, A.; Vitturini, C.; Spitoni, G.; Nanni, M.V.; Guariglia, C.; Morelli, D. Sensory-Motor Rehabilitation in Rett Syndrome: A Case Report. Focus Autism Other Dev. Disabl. 2008, 23, 49–62. [Google Scholar] [CrossRef]
- Lotan, M.; Barmatz, C. Hydrotherapy for a young child with Rett syndrome. Review of the literature and a case study. Int. J. Disabil. Hum. Dev. 2009, 8, 349–357. [Google Scholar] [CrossRef]
- Lotan, M.; Schenker, R.; Wine, J.; Downs, J. The conductive environment enhances gross motor function of girls with Rett syndrome. A pilot study. Dev. Neurorehabil. 2012, 15, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Lotan, M.; Gootman, A. Regaining walking ability in individuals with Rett syndrome: A case study. Int. J. Disabil. Hum. Dev. 2012, 11, 163–169. [Google Scholar] [CrossRef]
- Hackett, S.; Morison, C.; Pullen, C. A retrospective practice based evaluation of music therapy: A Single-case study of a four-year-old girl with Rett syndrome- Rebecca’s story. Arts Psychother. 2013, 40, 473477. [Google Scholar] [CrossRef]
- Stasolla, F.; Caffò, A.O. Promoting adaptative behaviors by two girls with Rett syndrome through a microswitch-based program. Res. Autism Spectr. Disord. 2013, 7, 1256–1272. [Google Scholar] [CrossRef]
- Lancioni, G.E.; Singh, N.N.; O’Reilly, M.F.; Sigafoos, J.; Boccasini, A.; La Martire, M.L.; Buonocunto, F.; Biancardi, E.M.; Sacco, V. Microswitch-aided Programs for a Woman with Rett Syndrome and a Boy with Extensive Neuro-motor and Intellectual Disabilities. J. Dev. Phys. Disabil. 2014, 26, 135–143. [Google Scholar] [CrossRef]
- Lotan, M.; Shavit, E.; Merrick, J. Enhancing Walking Ability in Individuals with Rett Syndrome Through the Use of Applied Behavioral Analysis (ABA): Review and a Case Study. Open Rehabil. J. 2015, 8, 1–8. [Google Scholar] [CrossRef]
- Scheafer-Champion, C.; Johnson, N.L. Fostering Ambulation for a Preschool Child with Rett Syndrome: A Case Report. Phys. Occup. Ther. Pediatr. 2015, 35, 354–364. [Google Scholar] [CrossRef]
- Stasolla, F.; Perilli, V.; Di Leone, A.; Damiani, R.; Albano, V.; Stella, A.; Damato, C. Technological Aids to Support Choice Strategies by Three Girls with Rett Syndrome. Res. Dev. Disabil. 2015, 36, 36–44. [Google Scholar] [CrossRef]
- Mraz, K.M.; Amadio, G.; Diener, P.; Eisenberg, G.; Engsberg, J.R. Improving Upper Extremity Motor Skills in Girls with Rett Syndrome Using Virtual Reality. Intellect. Disabil. Diagn. J. 2016, 4, 142–151. [Google Scholar] [CrossRef]
- McAmis, N.E.; Foreman, M.H.; Himmelrich, M.D.; Diener, P.S.; Engsberg, J.R. Development of a Method to Use a Color Tracker for Motor Therapy for Individuals with Rett Syndrome. SM J. Pediatr. 2017, 2, 1012. [Google Scholar]
- Downs, J.; Rodger, J.; Li, C.; Tan, X.; Hu, N.; Wong, K.; De Klerk, N.; Leonard, H. Environmental enrichment intervention for Rett syndrome: An individually randomised stepped wedge trial. Orphanet J. Rare Dis. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Larsson, G.; Julu, P.O.O.; Engerström, I.W.; Sandlund, M.; Lindström, B. Walking on treadmill with Rett syndrome—Effects on the autonomic nervous system. Res. Dev. Disabil. 2018, 83, 99–107. [Google Scholar] [CrossRef]
- Downs, J.; Bergman, A.; Carter, P.; Anderson, A.; Palmer, G.M.; Roye, D.; Van Bosse, H.; Bebbington, A.; Larsson, E.L.; Smith, B.G.; et al. Guidelines for Management of Scoliosis in Rett Syndrome Patients Based on Expert Consesus and Clinical Evidence. Spine 2009, 34, E607–E617. [Google Scholar] [CrossRef] [PubMed]
- Neul, J.L.; Kaufmann, W.E.; Glaze, D.G.; Christodoulou, J.; Clarke, A.J.; Bahi-Buisson, N.; Leonard, H.; Bailey, M.E.S.; Schanen, N.C.; Zappella, M.; et al. Rett Syndrome: Revised Diagnostic Criteria and Nomenclature. Ann. Neurol. 2010, 68, 944–950. [Google Scholar] [CrossRef]
- Rath, A.; Salamon, V.; Peixoto, S.; Hivert, V.; Laville, M.; Segrestin, B.; Neugebauer, E.; Eikermann, M.; Bertele, V.; Garattini, S.; et al. A systematic literature review of evidence-based clinical practice for rare diseases: What are the perceived and real barriers for improving the evidence and how can they be overcome? Trials 2017, 18, 556. [Google Scholar] [CrossRef]
- Herbert, R.; Jamtvedt, G.; Birger Hagen, K.; Mead, J. Practical Evidence-Based Physiotherapy, 2nd ed.; Churchill Livingstone Elsevier: London, UK, 2011; ISBN 978-0-7020-4713-8. [Google Scholar]
| Lead Author and Year of Publication | Study Design | Physical Therapy Approach | Number of Participants | Assessment Tool | Follow-up Duration | Main Results/Findings | Level of Evidence (Grade of Recom- Mendation) |
|---|---|---|---|---|---|---|---|
| Larsson G. 2001 [36] | Case report | Kinesiotherapy + orthoses + aids (following surgery) | 3 | Narrative summary | Different for each case |
| 4 (C) |
| Yasuhara A. 2001 [37] | Case report | Music therapy (individual session of 30 min/week) | 3 |
| 40 weeks for two patients and 20 weeks for the third patient | The children showed some degree of mental and physical development: improvement of the purposive hand use, development of language comprehension, development of the ability to communicate by using cards or gestures, development in listening and playing instruments | 4 (C) |
| Bumin G. 2003 [38] | Case report | Hydrotherapy (Halliwick method) | 1 | The tests included:
| 8 weeks |
| 4 (C) |
| Lotan M. 2004 [39] | Case series | A daily training program on a treadmill | 4 |
| 2 months |
| 4 (C) |
| Elefant C. 2004 [40] | Case report | Dual intervention: physical and music therapy | 1 | Narrative summary | N.S. |
| 4 (C) |
| Lotan M. 2005 [41] | Case report | A management plan consisting of: opposing asymmetry postures, walking and/or standing, maintaining spinal mobility through passive manual manipulation, individualized aids, parental and staff guidance | 1 | Measurement of the Cobb angle by X-ray in supine and suspended position | 1 year and 6 months |
| 4 (C) |
| Lotan M. 2006 [42] | Case report | Snoezelen (Controlled Multisensory Environment) | 3 (case 1 stage II; case 2 stage III; case 3 stage IV) | Narrative summary |
| Case 1: Agitation diminished and the patient was much more relaxed throughout the day Case 2: falls have completely ceased although posture did not seem to visually change Case 3: JROM increased throughout the body, enough to ease patient’s daily suffering and alleviate caregivers’ difficulties | 4 (C) |
| Lotan M. 2007 [43] | Case report | Different alternative therapeutic interventions: Animal-Assisted Therapy (AAT), Auditory Integration Training (AIT), hyperbaric chamber, acupuncture/acupressure, aromatherapy, craniosacral therapy, Mayo fascial release, chiropractor, Reiki, Treager massage, cognitive rehabilitation, Applied Behavior Analysis (ABA), Advanced Biomechanical Rehabilitation (ABR), Doman-Delacato approach, Yoga | 1 | Narrative summary | 3 years | The patient definitely made meaningful and significant progress for herself | 4 (C) |
| Pizzamiglio M.R. 2008 [44] | Case report | Acclimating to the therapeutic setting + computerized visual-motor coordination training + sensory-motor rehabilitative program | 1 |
| 3 years |
| 4 (C) |
| Lotan M. 2009 [45] | Case report | Hydrotherapy | 1 | Narrative summary | 3 years | The patient gained control over the body, thereby improving his functional abilities. Such gains, accompanied by improved communication skills, enhanced the child’s control over his daily situations, thereby achieving a feeling of self-worth and empowerment. | 4 (C) |
| Lotan M. 2012 [46] | Single-case A-B design | Conductive Environment (CE) | 3 |
| 2 years |
| 4 (C) |
| Lotan M. 2012 [47] | Case report | The intervention program includes two sections:
| 1 | Functional Independence Measure (FIM) | 3 years | The FIM score switched from 18 to 25. | 4 (C) |
| Hackett S. 2013 [48] | Case report | Music therapy | 1 | Retrospective video analysis | 6 months | Hand movements have become more purposeful. Motor skills (specifically holding) enhanced. Intentional communication improved through promoting turn-tasking. | 4 (C) |
| Stasolla F. 2013 [49] | Multiple Baseline | Microswitch-based program | 2 |
| About 6 months |
| 4 (C) |
| Lancioni G.E. 2014 [50] | Single-case A-B-A-B | Microswitch-aided program (2 interventions) | 1 with RTT and 1 with congenital encephalopathy |
| N.S. | Increase in microswitch responses and level of happiness for both participants during the intervention phases | 4 (C) |
| Lotan M. 2015 [51] | Case report | Applied Behavioral Analysis (ABA) | 1 | Number of steps taken daily (accelerometer) | 3 months | From 800 to 8000 steps/day | 4 (C) |
| Schaefer- Campion C. 2015 [52] | Case report | A series of assistive device trials:
| 1 | Gait analysis including:
| 6 months | The anterior four-wheeled walker with a horizontal bar and lateral handholds was chosen | 4 (C) |
| Stasolla F. 2015 [53] | Multiple baseline | Technological aids | 3 |
| About 6 months (225 sessions) |
| 4 (C) |
| Mraz K.M. 2016 [54] | Case series | Virtual Reality Intervention for Rett Syndrome (RTT-IVR) | 6 | Narrative summary + interviews | N.S. | Interviews and observation revealed successful game play when games were motivating, clearly established cause and effect, and matched level of cognitive ability of the participant | 4 (C) |
| McAmis N.H. 2017 [55] | Case report | Virtual reality | 1 | System Usability Scale (SUS) | 8 months | The ultimate feasibility percentile was calculated to be in the seventieth percentile which ranks in the “good” category. | 4 (C) |
| Downs J. 2018 [56] | Modified individually randomized stepped wedge | Environmental Enrichment (EE) | 12 |
| 6 months |
| 2b (B) |
| Larsson G. 2018 [57] | Case-control study | To walk on a treadmill at the maximum comfortable walking speed | 12 RTT girls and 14 healthy females |
| Six-minute single test | The changes in cardiac sensitivity to baroreflex and cardiac vagal tone in people with RTT compared to controls indicated more arousal, but only when the treadmill was started; as they continued walking, the arousal dropped to control level. People with RTT exhibited little changes in pCO2 whereas the controls showed increased values during walking. | 3 (C) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fonzo, M.; Sirico, F.; Corrado, B. Evidence-Based Physical Therapy for Individuals with Rett Syndrome: A Systematic Review. Brain Sci. 2020, 10, 410. https://doi.org/10.3390/brainsci10070410
Fonzo M, Sirico F, Corrado B. Evidence-Based Physical Therapy for Individuals with Rett Syndrome: A Systematic Review. Brain Sciences. 2020; 10(7):410. https://doi.org/10.3390/brainsci10070410
Chicago/Turabian StyleFonzo, Marta, Felice Sirico, and Bruno Corrado. 2020. "Evidence-Based Physical Therapy for Individuals with Rett Syndrome: A Systematic Review" Brain Sciences 10, no. 7: 410. https://doi.org/10.3390/brainsci10070410
APA StyleFonzo, M., Sirico, F., & Corrado, B. (2020). Evidence-Based Physical Therapy for Individuals with Rett Syndrome: A Systematic Review. Brain Sciences, 10(7), 410. https://doi.org/10.3390/brainsci10070410







