Impact of Virtual Reality in Arterial Anatomy Detection and Surgical Planning in Patients with Unruptured Anterior Communicating Artery Aneurysms
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Enrolment
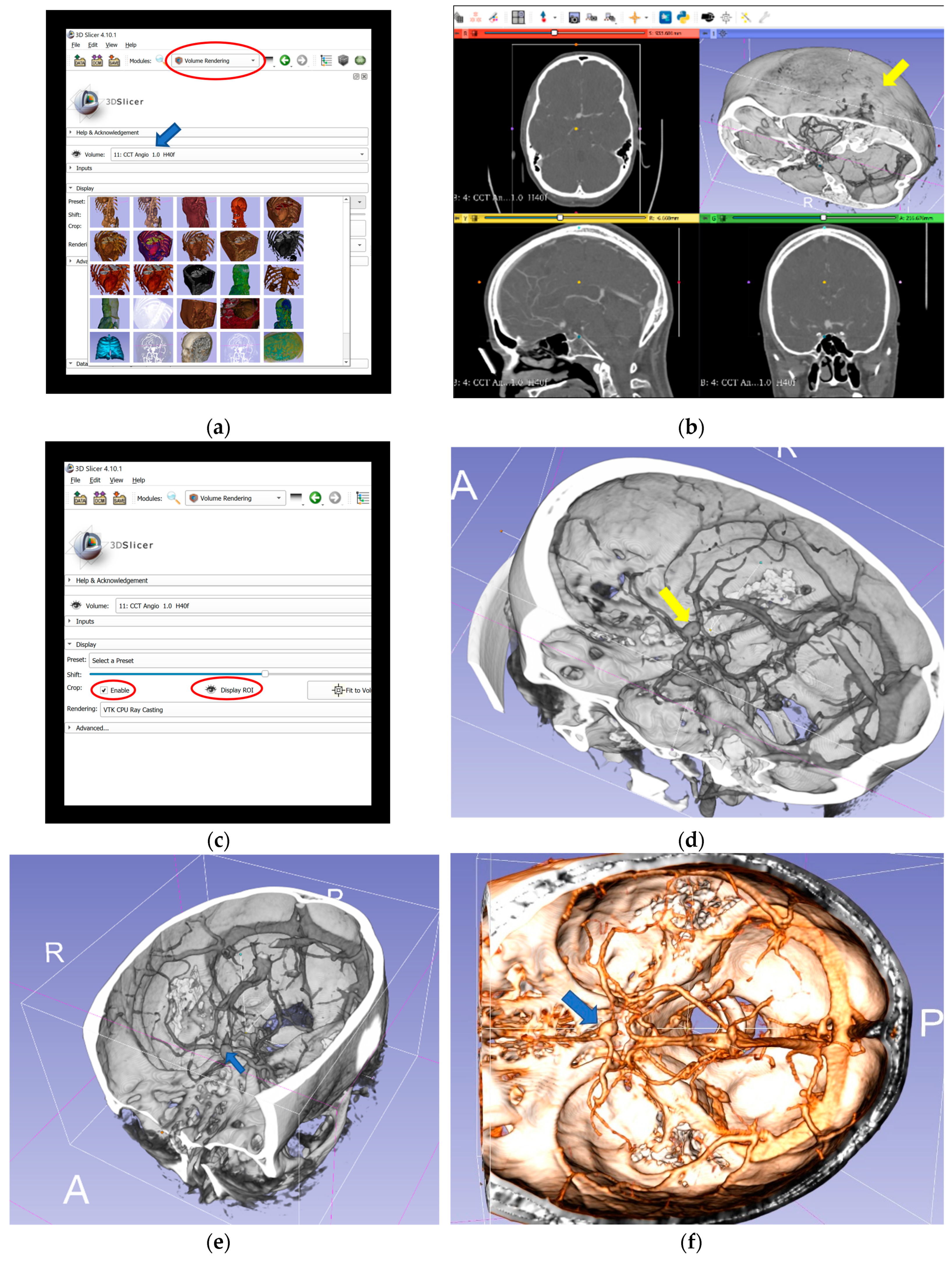
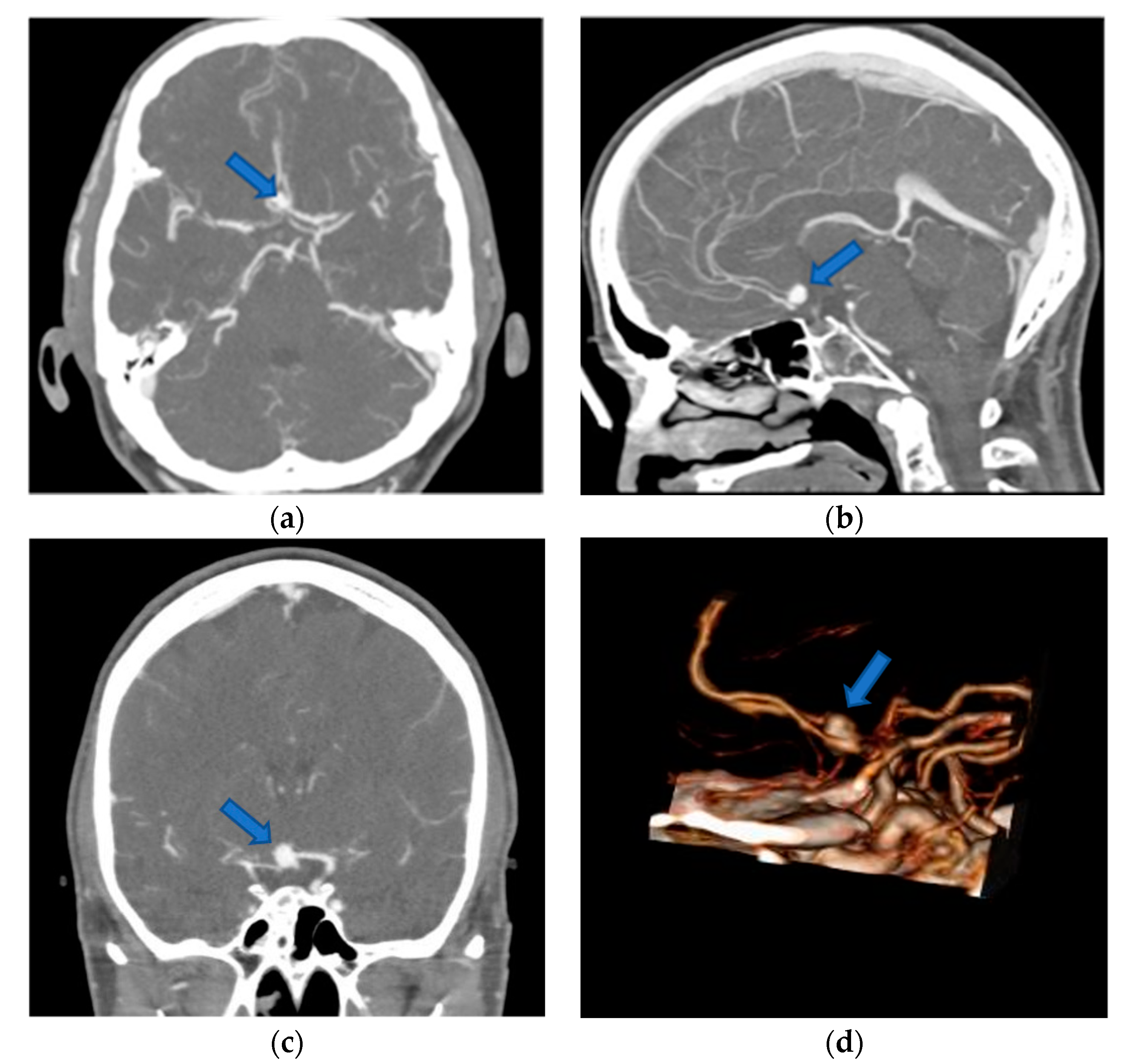
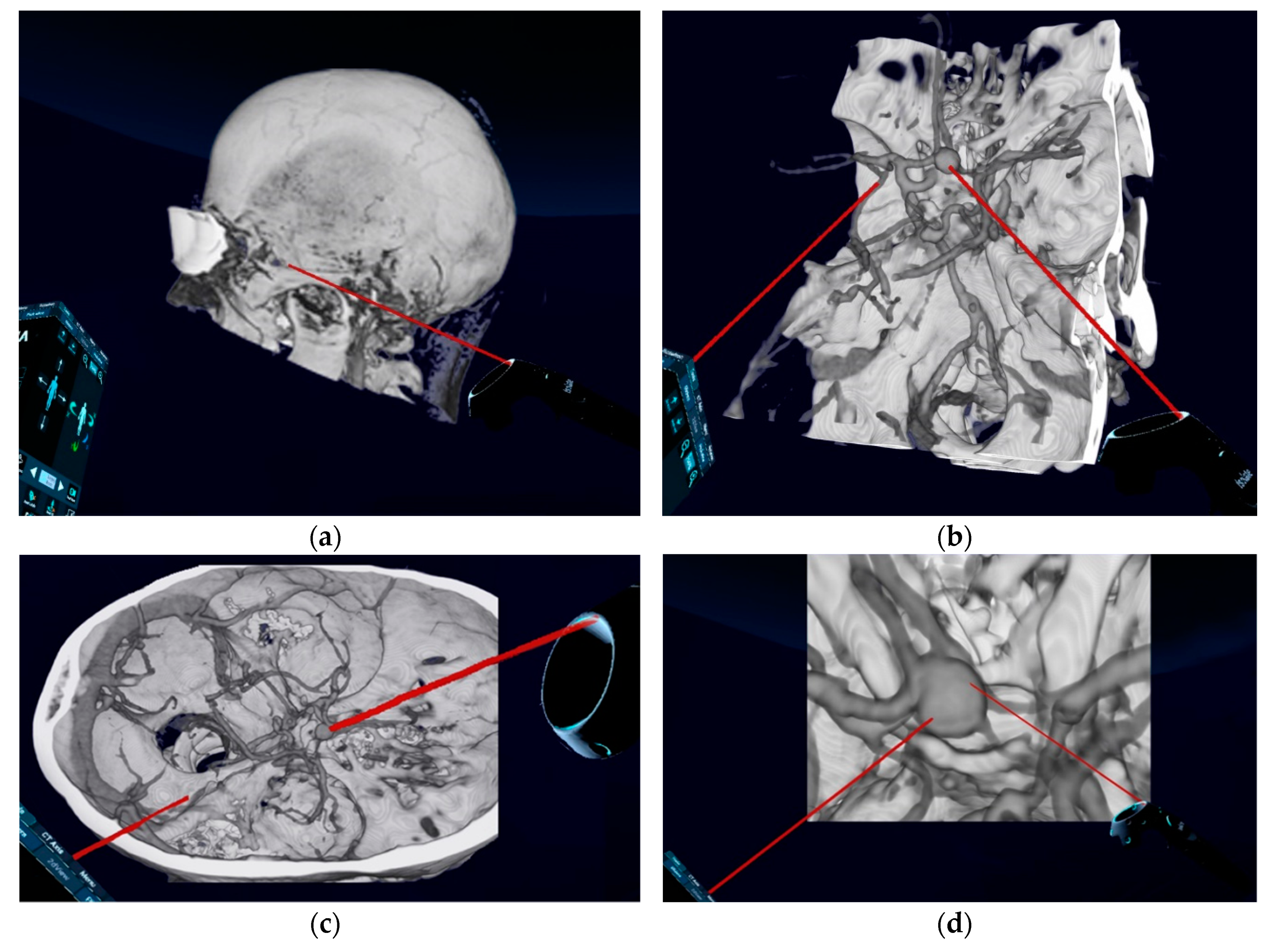
2.2. Data Acquisition and Handling
2.3. Neurosurgical Technique
2.4. Virtual Reality Visualization Technique
2.5. Study Design
2.6. Statistical Analysis
3. Results
3.1. Patient- and Disease-Related Data
3.2. Role of Image Presentation Modality in the Identification of Anatomical Structures and Surgical Planning
3.2.1. Impact on Identification of Anatomical Structures
3.2.2. Impact on Selection of Patient and Head Positioning
3.2.3. Impact on Selection of Surgical Approach and Approach Side
3.2.4. Impact on Selection of Clipping Strategy
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Thompson, B.G.; Brown, R.D.; Amin-Hanjani, S.; Broderick, J.P.; Cockroft, K.M.; Connolly, E.S.; Duckwiler, G.R.; Harris, C.C.; Howard, V.J.; Johnston, S.C.C.; et al. Guidelines for the Management of Patients With Unruptured Intracranial Aneurysms: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2015, 46, 2368–2400. [Google Scholar] [CrossRef] [PubMed]
- Vlak, M.H.M.; Algra, A.; Brandenburg, R.; Rinkel, G.J.E. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 2011, 10, 626–636. [Google Scholar] [CrossRef]
- Tutino, V.M.; Poppenberg, K.E.; Li, L.; Shallwani, H.; Jiang, K.; Jarvis, J.N.; Sun, Y.; Snyder, K.V.; Levy, E.I.; Siddiqui, A.H.; et al. Biomarkers from circulating neutrophil transcriptomes have potential to detect unruptured intracranial aneurysms. J. Transl. Med. 2018, 16, 373. [Google Scholar] [CrossRef] [PubMed]
- Ajiboye, N.; Chalouhi, N.; Starke, R.M.; Zanaty, M.; Bell, R. Unruptured Cerebral Aneurysms: Evaluation and Management. Sci. World J. 2015, 2015, 954954. [Google Scholar] [CrossRef]
- Etminan, N.; Dörfler, A.; Steinmetz, H. Unruptured Intracranial Aneurysms- Pathogenesis and Individualized Management. Dtsch. Arztebl. Int. 2020, 117, 235–242. [Google Scholar] [CrossRef]
- Hernesniemi, J.; Dashti, R.; Lehecka, M.; Niemelä, M.; Rinne, J.; Lehto, H.; Ronkainen, A.; Koivisto, T.; Jääskeläinen, J.E. Microneurosurgical management of anterior communicating artery aneurysms. Surg. Neurol. 2008, 70, 8–28. [Google Scholar] [CrossRef]
- Kassell, N.F.; Torner, J.C.; Haley, E.C.; Jane, J.A.; Adams, H.P.; Kongable, G.L. The International Cooperative Study on the Timing of Aneurysm Surgery. Part 1: Overall management results. J. Neurosurg. 1990, 73, 18–36. [Google Scholar] [CrossRef]
- Lee, U.Y.; Jung, J.; Kwak, H.S.; Lee, D.H.; Chung, G.H.; Park, J.S.; Koh, E.J. Wall Shear Stress and Flow Patterns in Unruptured and Ruptured Anterior Communicating Artery Aneurysms Using Computational Fluid Dynamics. J. Korean Neurosurg. Soc. 2018, 61, 689–699. [Google Scholar] [CrossRef]
- Darsaut, T.E.; Findlay, J.M.; Magro, E.; Kotowski, M.; Roy, D.; Weill, A.; Bojanowski, M.W.; Chaalala, C.; Iancu, D.; Lesiuk, H.; et al. Surgical clipping or endovascular coiling for unruptured intracranial aneurysms: A pragmatic randomised trial. J. Neurol. Neurosurg. Psychiatry 2017, 88, 663–668. [Google Scholar] [CrossRef]
- Ivan, M.E.; Safaee, M.M.; Martirosyan, N.L.; Rodríguez-Hernández, A.; Sullinger, B.; Kuruppu, P.; Habdank-Kolaczkowski, J.; Lawton, M.T. Anatomical triangles defining routes to anterior communicating artery aneurysms: The junctional and precommunicating triangles and the role of dome projection. J. Neurosurg. 2019, 1–12. [Google Scholar] [CrossRef]
- Algra, A.M.; Lindgren, A.; Vergouwen, M.D.I.; Greving, J.P.; van der Schaaf, I.C.; van Doormaal, T.P.C.; Rinkel, G.J.E. Procedural Clinical Complications, Case-Fatality Risks, and Risk Factors in Endovascular and Neurosurgical Treatment of Unruptured Intracranial Aneurysms: A Systematic Review and Meta-analysis. JAMA Neurol. 2019, 76, 282–293. [Google Scholar] [CrossRef]
- Villablanca, J.P.; Duckwiler, G.R.; Jahan, R.; Tateshima, S.; Martin, N.A.; Frazee, J.; Gonzalez, N.R.; Sayre, J.; Vinuela, F.V. Natural history of asymptomatic unruptured cerebral aneurysms evaluated at CT angiography: Growth and rupture incidence and correlation with epidemiologic risk factors. Radiology 2013, 269, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Kockro, R.A.; Killeen, T.; Ayyad, A.; Glaser, M.; Stadie, A.; Reisch, R.; Giese, A.; Schwandt, E. Aneurysm Surgery with Preoperative Three-Dimensional Planning in a Virtual Reality Environment: Technique and Outcome Analysis. World Neurosurg. 2016, 96, 489–499. [Google Scholar] [CrossRef] [PubMed]
- Burtscher, J.; Kremser, C.; Seiwald, M.; Obwegeser, A.; Wagner, M.; Aichner, F.; Twerdy, K.; Felber, S. Three-dimensional computer assisted magnetic resonance imaging for neurosurgical planning in parasagittal and parafalcine central region tumors. Comput. Aided Surg. 1998, 3, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Kin, T.; Nakatomi, H.; Shono, N.; Nomura, S.; Saito, T.; Oyama, H.; Saito, N. Neurosurgical Virtual Reality Simulation for Brain Tumor Using High-definition Computer Graphics: A Review of the Literature. Neurol. Med. Chir. 2017, 57, 513–520. [Google Scholar] [CrossRef]
- Kockro, R.A.; Stadie, A.; Schwandt, E.; Reisch, R.; Charalampaki, C.; Ng, I.; Yeo, T.T.; Hwang, P.; Serra, L.; Perneczky, A. A collaborative virtual reality environment for neurosurgical planning and training. Neurosurgery 2007, 61, 379–391. [Google Scholar] [CrossRef]
- Kersten-Oertel, M.; Jannin, P.; Collins, D.L. The state of the art of visualization in mixed reality image guided surgery. Comput. Med. Imaging Graph. 2013, 37, 98–112. [Google Scholar] [CrossRef]
- Ong, C.S.; Deib, G.; Yesantharao, P.; Qiao, Y.; Pakpoor, J.; Hibino, N.; Hui, F.; Garcia, J.R. Virtual Reality in Neurointervention. J. Vasc. Interv. Neurol. 2018, 10, 17–22. [Google Scholar]
- De Ribaupierre, S.; Eagleson, R. Editorial: Challenges for the usability of AR and VR for clinical neurosurgical procedures. Healthc. Technol. Lett. 2017, 4, 151. [Google Scholar] [CrossRef]
- Zanier, E.R.; Zoerle, T.; Di Lernia, D.; Riva, G. Virtual Reality for Traumatic Brain Injury. Front. Neurol. 2018, 9, 345. [Google Scholar] [CrossRef]
- Drouin, S.; Kochanowska, A.; Kersten-Oertel, M.; Gerard, I.J.; Zelmann, R.; de Nigris, D.; Bériault, S.; Arbel, T.; Sirhan, D.; Sadikot, A.F.; et al. IBIS: An OR ready open-source platform for image-guided neurosurgery. Int. J. Comput. Assist. Radiol. Surg. 2017, 12, 363–378. [Google Scholar] [CrossRef] [PubMed]
- Kawamata, T.; Iseki, H.; Shibasaki, T.; Hori, T. Endoscopic augmented reality navigation system for endonasal transsphenoidal surgery to treat pituitary tumors: Technical note. Neurosurgery 2002, 50, 1393–1397. [Google Scholar] [CrossRef]
- Stadie, A.T.; Kockro, R.A.; Reisch, R.; Tropine, A.; Boor, S.; Stoeter, P.; Perneczky, A. Virtual reality system for planning minimally invasive neurosurgery. Technical note. J. Neurosurg. 2008, 108, 382–394. [Google Scholar] [CrossRef]
- Krayenbühl, H.; Brihaye, J.; Loew, F.; Logue, V.; Mingrino, S.; Pertuiset, B.; Symon, L.; Troupp, H.; Yaşargil, M.G. (Eds.) Advances and Technical Standards in Neurosurgery; Springer: Vienna, Austria, 1975; ISBN 978-3-7091-7090-8. [Google Scholar]
- Hendricks, B.K.; Cohen-Gadol, A.A. The Extended Pterional Craniotomy: A Contemporary and Balanced Approach. Oper. Neurosurg. 2020, 18, 225–231. [Google Scholar] [CrossRef]
- Park, J. Supraorbital Keyhole Approach for Intracranial Aneurysms: Transitioning from Concerns to Confidence. J. Korean Neurosurg. Soc. 2020, 63, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Chavan, V.S.; Yamada, Y.; Chandratej, K.; Gowtham, D.; Riccardo, S.; Firuz, S.; Yoko, K. Intraoperative Use of Microscope-Integrated Flow 800—A Valuable Tool in Surgical Management of Anterior Communicating Artery Aneurysm: Our Institutional Experience. Asian J. Neurosurg. 2020, 15, 26–30. [Google Scholar] [CrossRef]
- Oda, J.; Kato, Y.; Chen, S.F.; Sodhiya, P.; Watabe, T.; Imizu, S.; Oguri, D.; Sano, H.; Hirose, Y. Intraoperative near-infrared indocyanine green-videoangiography (ICG-VA) and graphic analysis of fluorescence intensity in cerebral aneurysm surgery. J. Clin. Neurosci. 2011, 18, 1097–1100. [Google Scholar] [CrossRef] [PubMed]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.-C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R.A. On the interpretation of χ2 from contingency tables, and the calculation of P. J. R. Stat. Soc. 1922, 85, 87–94. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef]
- Bekelis, K.; Missios, S.; MacKenzie, T.A.; Desai, A.; Fischer, A.; Labropoulos, N.; Roberts, D.W. Predicting inpatient complications from cerebral aneurysm clipping: The Nationwide Inpatient Sample 2005–2009. J. Neurosurg. 2014, 120, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Moroi, J.; Hadeishi, H.; Suzuki, A.; Yasui, N. Morbidity and mortality from surgical treatment of unruptured cerebral aneurysms at Research Institute for Brain and Blood Vessels-Akita. Neurosurgery 2005, 56, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Kotowski, M.; Naggara, O.; Darsaut, T.E.; Nolet, S.; Gevry, G.; Kouznetsov, E.; Raymond, J. Safety and occlusion rates of surgical treatment of unruptured intracranial aneurysms: A systematic review and meta-analysis of the literature from 1990 to 2011. J. Neurol. Neurosurg. Psychiatry 2013, 84, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Ogilvy, C.S.; Carter, B.S. Stratification of outcome for surgically treated unruptured intracranial aneurysms. Neurosurgery 2003, 52, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; Kato, Y.; Chen, L.; Karagiozov, K.; Yoneda, M.; Imizu, S.; Sano, H.; Kanno, T. Anterior communicating artery aneurysms: An overview. Minim. Invasive Neurosurg. 2008, 51, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Cai, W.; Hu, C.; Gong, J.; Lan, Q. Anterior Communicating Artery Aneurysm Morphology and the Risk of Rupture. World Neurosurg. 2018, 109, 119–126. [Google Scholar] [CrossRef]
- Nossek, E.; Setton, A.; Karimi, R.; Dehdashti, A.R.; Langer, D.J.; Chalif, D.J. Analysis of superiorly projecting anterior communicating artery aneurysms: Anatomy, techniques, and outcome. A proposed classification system. Neurosurg. Rev. 2016, 39, 225–235. [Google Scholar] [CrossRef]
- Hasan, M.N.; Hoque, M.A.; Rahman, K.M.; Hoque, M.H.; Amin, M.R.; Haque, M.; Joarder, A.I.; Helal, A.H. Clinical and digital subtraction angiographic (DSA) evaluation of patients of subarachnoid haemorrhage (SAH) in a tertiary level hospital. Bangladesh Med. J. 2016, 44, 125–129. [Google Scholar] [CrossRef][Green Version]
- Yoon, N.K.; McNally, S.; Taussky, P.; Park, M.S. Imaging of cerebral aneurysms: A clinical perspective. Neurovasc. Imaging 2016, 2, 660. [Google Scholar] [CrossRef]
- Tarulli, E.; Fox, A.J. Potent risk factor for aneurysm formation: Termination aneurysms of the anterior communicating artery and detection of A1 vessel asymmetry by flow dilution. AJNR Am. J. Neuroradiol. 2010, 31, 1186–1191. [Google Scholar] [CrossRef]
- Mo, D.-P.; Bao, S.-D.; Li, L.; Yi, Z.-Q.; Zhang, J.-Y.; Zhang, Y. Virtual reality system for diagnosis and therapeutic planning of cerebral aneurysms. Chin. Med. J. 2010, 123, 2206–2210. [Google Scholar] [PubMed]
- Alaraj, A.; Luciano, C.J.; Bailey, D.P.; Elsenousi, A.; Roitberg, B.Z.; Bernardo, A.; Banerjee, P.P.; Charbel, F.T. Virtual reality cerebral aneurysm clipping simulation with real-time haptic feedback. Neurosurgery 2015, 11 (Suppl. 2), 52–58. [Google Scholar] [CrossRef] [PubMed]
- Zawy Alsofy, S.; Sakellaropoulou, I.; Stroop, R. Evaluation of Surgical Approaches for Tumor Resection in the Deep Infratentorial Region and Impact of Virtual Reality Technique for the Surgical Planning and Strategy. J. Craniofac. Surg. 2020, 31, 1865–1869. [Google Scholar] [CrossRef] [PubMed]
- Kasinathan, S.; Yamada, Y.; Cheikh, A.; Teranishi, T.; Kawase, T.; Kato, Y. Prognostic factors influencing outcome in unruptured anterior communicating artery aneurysm after microsurgical clipping. Asian J. Neurosurg. 2019, 14, 28. [Google Scholar] [CrossRef]
- Chaddad-Neto, F.; Doria-Netto, H.L.; de Campos-Filho, J.M.; Ribas, E.S.C.; Ribas, G.C.; de Oliveira, E. Head positioning for anterior circulation aneurysms microsurgery. Arq. Neuropsiquiatr. 2014, 72, 832–840. [Google Scholar] [CrossRef][Green Version]
- Bhattarai, R.; Liang, C.-F.; Chen, C.; Wang, H.; Huang, T.-C.; Guo, Y. Factors determining the side of approach for clipping ruptured anterior communicating artery aneurysm via supraorbital eyebrow keyhole approach. Chin. J. Traumatol. 2020, 23, 20–24. [Google Scholar] [CrossRef]
- Wong, G.K.C.; Zhu, C.X.L.; Ahuja, A.T.; Poon, W.S. Craniotomy and clipping of intracranial aneurysm in a stereoscopic virtual reality environment. Neurosurgery 2007, 61, 564–568. [Google Scholar] [CrossRef]
- Soares, F.P.; Velho, M.C.; Antunes, A.C.M. Clinical and morphological profile of aneurysms of the anterior communicating artery treated at a neurosurgical service in Southern Brazil. Surg. Neurol. Int. 2019, 10, 193. [Google Scholar] [CrossRef]
- Koyama, T.; Hongo, K.; Tanaka, Y.; Kobayashi, S. Simulation of the surgical manipulation involved in clipping a basilar artery aneurysm: Concepts of virtual clipping. Technical note. J. Neurosurg. 2000, 93, 355–360. [Google Scholar] [CrossRef]
- Scerrati, A.; Trovalusci, F.; Albanese, A.; Ponticelli, G.S.; Tagliaferri, V.; Sturiale, C.L.; Cavallo, M.A.; Marchese, E. A workflow to generate physical 3D models of cerebral aneurysms applying open source freeware for CAD modeling and 3D printing. Interdiscip. Neurosurg. 2019, 17, 1–6. [Google Scholar] [CrossRef]
| Surgeon’s Name: |
|---|
| Patient-ID: |
1. How is the identification of anatomical structures according to the presented images?
|
2. Is a preoperative cerebral digital subtraction angiography (DSA) necessary?
|
3. Which type of patient position would you choose for the surgical treatment according to the presented images?
|
4. Which type of head position would you choose for the surgical treatment according to the presented images?
|
5. Which approach would you choose for the surgical treatment according to the presented images?
|
6. Which approach side would you choose for the surgical treatment according to the presented images?
|
7. Would you use a temporary clip for the the surgical treatment according to the presented images?
|
8. Which type of permanent clip would you choose for the surgical treatment according to the presented images?
|
| Characteristics | n (%), Unless otherwise Stated |
|---|---|
| age (years), mean ± SD (min-max) | 54 ± 7 (30–74) |
| gender: | |
| male | 12 (46) |
| female | 14 (54) |
| preoperative imaging: | |
| CTA | 26 (100) |
| DSA | 12 (46) |
| MRA | 20 (77) |
| aneurysm size: | |
| <11 mm | 20 (77) |
| 11–25 mm | 5 (19) |
| >25 mm | 1 (4) |
| morphological parameters | |
| mean ± SD: | |
| neck width | 5.7 (2.3) |
| dome/neck ratio | 1.03 (0.6) |
| aspect ratio | 1.1 (0.6) |
| aneurysm angle | 83.2 (14.5) |
| flow angle | 110.8 (17.3) |
| aneurysm direction: | |
| anteriorly | 12 (46) |
| inferiorly | 9 (35) |
| superiorly | 4 (15) |
| posteriorly | 1 (4) |
| perioperative complications: | |
| infection | 1 (4) |
| infarction | 1 (4) |
| postoperative leg thrombosis | 1 (4) |
| secondary bleeding | 0 (0) |
| sensomotoric deficits | 1 (4) |
| pseudomeningocele | 2 (8) |
| discharge status: | |
| no new symptoms | 25 (96) |
| new neurological symptoms | 1 (4) |
| Image-Based Assessment, n (%) | CTA (n = 260) | 3D-VR (n = 260) | p-Value |
|---|---|---|---|
| anatomical structure detection: | |||
| appropriate | 104 (40) | 149 (57) | 0.0001 |
| not appropriate | 156 (60) | 111 (43) | (significant) |
| preoperative DSA: | |||
| necessary | 147 (57) | 116 (45) | 0.008 |
| not necessary | 113 (43) | 144 (55) | (significant) |
| Recommendations, n (%) | CTA (n = 260) | 3D-VR (n = 260) | p-Value |
|---|---|---|---|
| recommended patient positioning: | |||
| supine position | 208 (80) | 226 (87) | 0.38 |
| other positions | 52 (20) | 34 (13) | (not significant) |
| recommended head positioning: | |||
| straight “neutral” | 48 (18) | 28 (11) | |
| straight with flexion | 4 (2) | 8 (3) | 0.005 |
| straight with extension | 24 (9) | 12 (5) | (significant) |
| lateral rotation | 184 (71) | 212 (81) |
| Recommendations, n (%) | CTA (n = 260) | 3D-VR (n = 260) | p-Value |
|---|---|---|---|
| recommended surgical approach: | |||
| supraorbital subfrontal | 76 (29) | 48 (18) | 0.001 |
| pterional | 93 (36) | 83 (32) | (significant) |
| extended pterional | 91 (35) | 129 (50) | |
| recommended approach side: | |||
| right | 135 (52) | 149 (57) | 0.25 |
| left | 125 (48) | 111 (43) | (not significant) |
| Recommendations, n (%) | CTA (n = 260) | 3D-VR (n = 260) | p-Value |
|---|---|---|---|
| temporary clipping: | |||
| yes | 74 (28) | 63 (24) | 0.32 |
| no | 186 (72) | 197 (76) | (not significant) |
| type of permanent clip: | |||
| straight/curved | 175 (67) | 185 (71) | 0.54 |
| angled | 77 (30) | 70 (27) | (not significant) |
| fenestrated | 8 (3) | 5 (2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zawy Alsofy, S.; Sakellaropoulou, I.; Nakamura, M.; Ewelt, C.; Salma, A.; Lewitz, M.; Welzel Saravia, H.; Sarkis, H.M.; Fortmann, T.; Stroop, R. Impact of Virtual Reality in Arterial Anatomy Detection and Surgical Planning in Patients with Unruptured Anterior Communicating Artery Aneurysms. Brain Sci. 2020, 10, 963. https://doi.org/10.3390/brainsci10120963
Zawy Alsofy S, Sakellaropoulou I, Nakamura M, Ewelt C, Salma A, Lewitz M, Welzel Saravia H, Sarkis HM, Fortmann T, Stroop R. Impact of Virtual Reality in Arterial Anatomy Detection and Surgical Planning in Patients with Unruptured Anterior Communicating Artery Aneurysms. Brain Sciences. 2020; 10(12):963. https://doi.org/10.3390/brainsci10120963
Chicago/Turabian StyleZawy Alsofy, Samer, Ioanna Sakellaropoulou, Makoto Nakamura, Christian Ewelt, Asem Salma, Marc Lewitz, Heinz Welzel Saravia, Hraq Mourad Sarkis, Thomas Fortmann, and Ralf Stroop. 2020. "Impact of Virtual Reality in Arterial Anatomy Detection and Surgical Planning in Patients with Unruptured Anterior Communicating Artery Aneurysms" Brain Sciences 10, no. 12: 963. https://doi.org/10.3390/brainsci10120963
APA StyleZawy Alsofy, S., Sakellaropoulou, I., Nakamura, M., Ewelt, C., Salma, A., Lewitz, M., Welzel Saravia, H., Sarkis, H. M., Fortmann, T., & Stroop, R. (2020). Impact of Virtual Reality in Arterial Anatomy Detection and Surgical Planning in Patients with Unruptured Anterior Communicating Artery Aneurysms. Brain Sciences, 10(12), 963. https://doi.org/10.3390/brainsci10120963






