Morning Headache as an Obstructive Sleep Apnea-Related Symptom among Sleep Clinic Patients—A Cross-Section Analysis
Abstract
1. Introduction
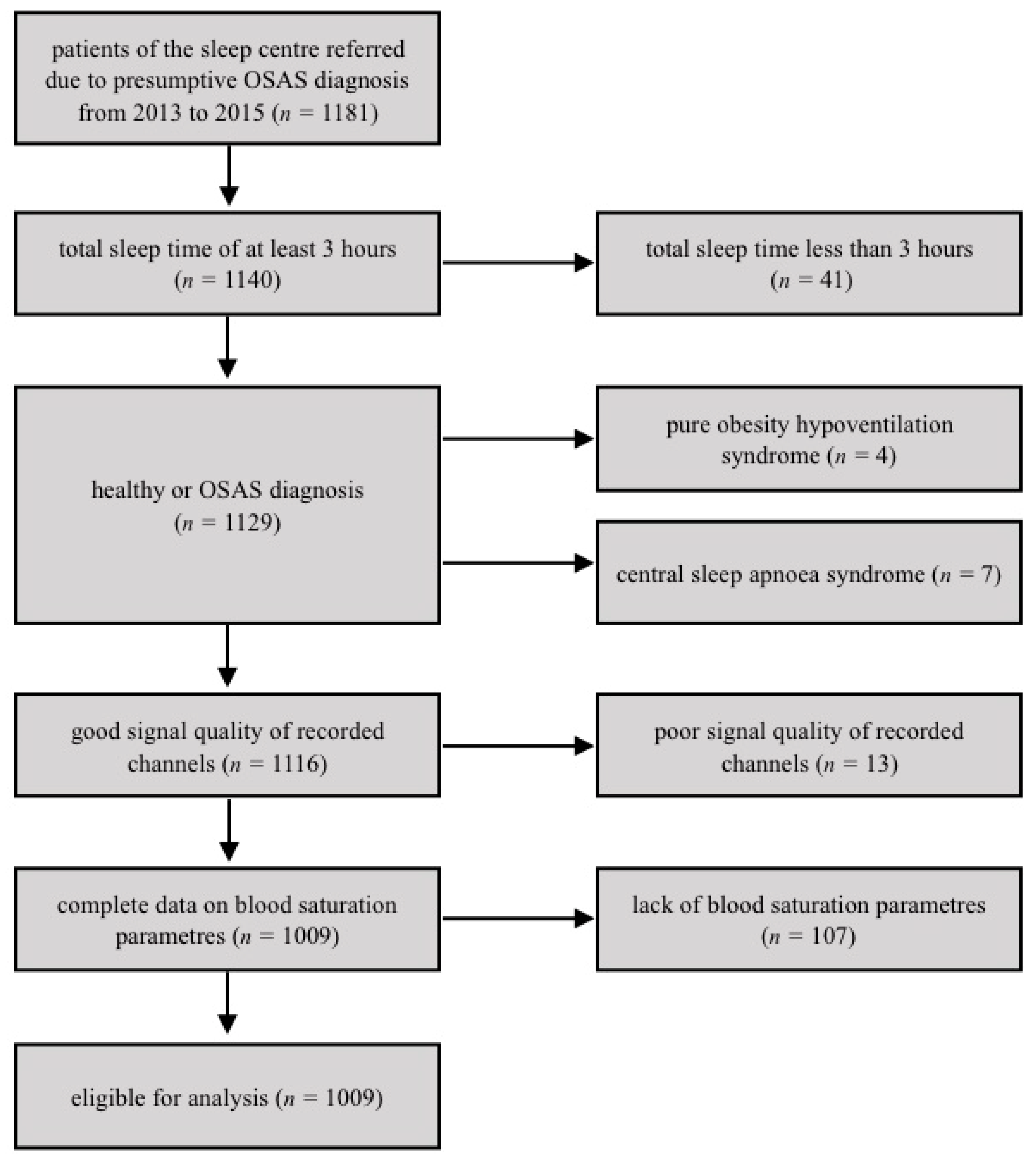
2. Materials and Methods
2.1. Compliance with Ethical Standards
2.2. Data Availability Statement
2.3. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Strollo, P.J.; Rogers, R.M. Obstructive Sleep Apnea. N. Engl. J. Med. 1996, 334, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Lévy, P.; Ryan, S.; Oldenburg, O.; Parati, G. Sleep apnea and the heart. Eur. Respir. Rev. 2013, 22, 333–352. [Google Scholar] [CrossRef] [PubMed]
- Selim, B.; Won, C.; Yaggi, H.K. Cardiovascular Consequences of Sleep Apnea. Clin. Chest Med. 2010, 31, 203–220. [Google Scholar] [CrossRef] [PubMed]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef]
- Heinzer, R.; Marti-Soler, H.; Haba-Rubio, J. Prevalence of sleep apnea syndrome in the middle to old age general population. Lancet Respir. Med. 2016, 4, e5–e6. [Google Scholar] [CrossRef]
- Jennum, P.; Jensen, R. Sleep and headache. Sleep Med. Rev. 2002, 6, 471–479. Available online: http://www.ncbi.nlm.nih.gov/pubmed/12505479 (accessed on 26 September 2019). [CrossRef]
- Song, T.J.; Lee, M.J.; Choi, Y.-J.; Kim, B.-K.; Chung, P.-W.; Park, J.-W.; Chu, M.K.; Kim, B.-S.; Sohn, J.-H.; Oh, K.; et al. Differences in Characteristics and Comorbidity of Cluster Headache According to the Presence of Migraine. J. Clin. Neurol. 2019, 15, 334–338. [Google Scholar] [CrossRef]
- EEG arousals: Scoring rules and examples: A preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 1992, 15, 173–184. [CrossRef]
- Lovati, C. Sleep apnea headache and headaches with sleep apnea: The importance of being secondary. Expert Rev. Neurother. 2013, 13, 1135–1137. [Google Scholar] [CrossRef][Green Version]
- Evers, S.; Barth, B.; Frese, A.; Husstedt, I.-W.; Happe, S. Sleep apnea in patients with cluster headache: A case-control study. Cephalalgia 2014, 34, 828–832. [Google Scholar] [CrossRef]
- Buse, D.C.; Rains, J.C.; Pavlovic, J.M.; Fanning, K.M.; Reed, M.L.; Manack Adams, A.; Lipton, R.B. Sleep Disorders Among People with Migraine: Results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study. Headache 2019, 59, 32–45. [Google Scholar] [CrossRef] [PubMed]
- Lyngberg, A.C.; Rasmussen, B.K.; Jorgensen, T.; Jensen, R. Has the prevalence of migraine and tension-type headache changed over a 12-year period? A Danish population survey. Eur. J. Epidemiol. 2005, 20, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.; Glozier, N.; Ratnavadivel, R.; Grunstein, R.R. Obstructive sleep apnea and depression. Sleep Med. Rev. 2009, 13, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Maurice, M. Prevalence and Risk Factors of Morning Headaches in the General Population. Arch. Intern. Med. 2004, 164, 97–102. [Google Scholar] [CrossRef]
- Sand, T.; Hagen, K.; Schrader, H. Sleep Apnoea and Chronic Headache. Cephalalgia 2003, 23, 90–95. [Google Scholar] [CrossRef]
- Kristiansen, H.A.; Kværner, K.J.; Akre, H.; Øverland, B.; Sandvik, L.; Russell, M.B. Sleep apnea headache in the general population. Cephalalgia 2012, 32, 451–458. [Google Scholar] [CrossRef]
- Russell, M.B.; Kristiansen, K.A.; Kværner, K.J. Headache in sleep apnea syndrome: Epidemiology and pathophysiology. Cephalalgia 2014, 34, 752–755. [Google Scholar] [CrossRef]
- Basoglu, O.K.; Tasbakan, M.S. Gender differences in clinical and polysomnographic features of obstructive sleep apnea: A clinical study of 2827 patients. Sleep Breath. 2018, 22, 241–249. [Google Scholar] [CrossRef]
- O’Connor, C.; Thornley, K.S.; Hanly, P.J. Gender Differences in the Polysomnographic Features of Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2000, 161, 1465–1472. [Google Scholar] [CrossRef]
- Rains, J.C.; Poceta, J.S. Sleep and Headache. Curr. Treat. Options Neurol. 2010, 12, 1–15. [Google Scholar] [CrossRef]
- Stark, C.D.; Stark, R.J. Sleep and chronic daily headache. Curr. Pain Headache Rep. 2015, 19, 468. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Nanovska, S.; Regen, W.; Spiegelhalder, K.; Feige, B.; Nissen, C.; Reynolds, C., III; Riemann, D. Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychol. Bull. 2016, 142, 969–990. [Google Scholar] [CrossRef] [PubMed]
- Wittchen, H.U.; Jacobi, F.; Rehm, J.; Gustavsson, A.; Svensson, M.; Jönsson, B.; Olesen, J.; Allgulander, C.; Alonso, J.; Faravelli, C.; et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 655–679. [Google Scholar] [CrossRef] [PubMed]
- Morris, C.J.; Purvis, T.E.; Hu, K.; Scheer, F.A. Circadian misalignment increases cardiovascular disease risk factors in humans. Proc. Natl. Acad. Sci. USA 2016, 113, E1402–E1411. [Google Scholar] [CrossRef] [PubMed]
- Sforza, E.; Roche, F.; Chapelle, C.; Pichot, V. Internight Variability of Apnea-Hypopnea Index in Obstructive Sleep Apnea Using Ambulatory Polysomnography. Front. Physiol. 2019, 10, 849. [Google Scholar] [CrossRef]
| MH ≥ 1 per Week | ||||||
|---|---|---|---|---|---|---|
| No MH (n = 711) | MH (n = 298) | |||||
| M | SD | M | SD | F | p | |
| age | 52.00 | 12.09 | 52.11 | 11.31 | 0.02 | 0.90 |
| BMI | 31.92 | 5.83 | 32.55 | 6.58 | 2.06 | 0.15 |
| Neck circumference | 41.92 | 4.12 | 41.45 | 4.54 | 2.61 | 0.11 |
| TST | 5.85 | 1.09 | 5.71 | 1.09 | 3.47 | 0.06 |
| Arousal index | 23.11 | 17.88 | 20.13 | 16.42 | 6.57 * | 0.01 |
| AHI | 28.46 | 26.94 | 23.66 | 25.78 | 7.11 * | 0.01 |
| Basal SpO2 | 92.21 | 3.52 | 92.04 | 3.60 | 0.50 | 0.48 |
| Mean SpO2 of desaturations | 86.87 | 7.53 | 87.13 | 7.35 | 0.25 | 0.61 |
| SpO2 nadir | 77.79 | 10.51 | 78.17 | 11.37 | 0.27 | 0.60 |
| % of time below 90% | 19.00 | 23.00 | 17.00 | 22.00 | 2.31 | 0.13 |
| Epworth sleepiness scale | 8.39 | 4.47 | 8.49 | 4.22 | 0.11 | 0.74 |
| No MH (n = 711) | MH (n = 298) | Chi2 | p | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Female | 143 | 20.11% | 98 | 32.89% | 18.846 | < 0.001 |
| Hypertension | 388 | 54.57% | 194 | 65.10% | 9.538 | 0.002 |
| Smoking | 349 | 49.09% | 133 | 44.63% | 1.670 | 0.196 |
| Snoring | 565 | 79.47% | 226 | 75.84% | 1.631 | 0.202 |
| Observed apneas | 524 | 73.70% | 209 | 70.13% | 1.343 | 0.247 |
| Excessive sleepiness | 240 | 33.76% | 99 | 33.33% | 0.017 | 0.897 |
| Unrefreshing sleep | 108 | 15.19% | 75 | 25.17% | 14.081 | < 0.001 |
| Choking at night | 120 | 16.88% | 75 | 25.17% | 9.256 | 0.002 |
| OR | OR 95% CI | Wald | p | ||
|---|---|---|---|---|---|
| Female sex | 1.375 | 1.080 | 1.751 | 6.694 | 0.010 |
| Hypertension | 1.246 | 1.064 | 1.461 | 7.417 | 0.006 |
| Smoking | 0.951 | 0.822 | 1.100 | 0.453 | 0.501 |
| Snoring | 0.866 | 0.729 | 1.028 | 2.694 | 0.101 |
| Observed apneas | 1.077 | 0.912 | 1.271 | 0.758 | 0.384 |
| Sleepiness | 0.937 | 0.800 | 1.097 | 0.654 | 0.419 |
| Unrefreshing sleep | 1.424 | 1.192 | 1.700 | 15.231 | 0.000 |
| Choking at night | 1.253 | 1.051 | 1.495 | 6.313 | 0.012 |
| Age | 0.987 | 0.974 | 1.001 | 3.322 | 0.068 |
| BMI | 1.017 | 0.978 | 1.057 | 0.689 | 0.406 |
| Neck circumference | 1.002 | 0.939 | 1.070 | 0.005 | 0.943 |
| TST | 0.872 | 0.763 | 0.998 | 3.952 | 0.047 |
| Arousal index | 0.997 | 0.984 | 1.009 | 0.292 | 0.589 |
| AHI | 0.990 | 0.979 | 1.000 | 3.675 | 0.055 |
| Basal SpO2 | 0.947 | 0.894 | 1.004 | 3.373 | 0.066 |
| Mean SpO2 of desaturations | 1.013 | 0.985 | 1.041 | 0.809 | 0.368 |
| SpO2 nadir | 0.988 | 0.966 | 1.010 | 1.148 | 0.284 |
| % time below 90% | 0.619 | 0.209 | 1.832 | 0.751 | 0.386 |
| Epworth sleepiness scale score | 1.012 | 0.978 | 1.047 | 0.484 | 0.487 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spałka, J.; Kędzia, K.; Kuczyński, W.; Kudrycka, A.; Małolepsza, A.; Białasiewicz, P.; Mokros, Ł. Morning Headache as an Obstructive Sleep Apnea-Related Symptom among Sleep Clinic Patients—A Cross-Section Analysis. Brain Sci. 2020, 10, 57. https://doi.org/10.3390/brainsci10010057
Spałka J, Kędzia K, Kuczyński W, Kudrycka A, Małolepsza A, Białasiewicz P, Mokros Ł. Morning Headache as an Obstructive Sleep Apnea-Related Symptom among Sleep Clinic Patients—A Cross-Section Analysis. Brain Sciences. 2020; 10(1):57. https://doi.org/10.3390/brainsci10010057
Chicago/Turabian StyleSpałka, Jakub, Konrad Kędzia, Wojciech Kuczyński, Aleksandra Kudrycka, Aleksandra Małolepsza, Piotr Białasiewicz, and Łukasz Mokros. 2020. "Morning Headache as an Obstructive Sleep Apnea-Related Symptom among Sleep Clinic Patients—A Cross-Section Analysis" Brain Sciences 10, no. 1: 57. https://doi.org/10.3390/brainsci10010057
APA StyleSpałka, J., Kędzia, K., Kuczyński, W., Kudrycka, A., Małolepsza, A., Białasiewicz, P., & Mokros, Ł. (2020). Morning Headache as an Obstructive Sleep Apnea-Related Symptom among Sleep Clinic Patients—A Cross-Section Analysis. Brain Sciences, 10(1), 57. https://doi.org/10.3390/brainsci10010057







