Myoelectric Gaming in the Rehabilitation of Patients with C7 Spinal Cord Injury
Abstract
:1. Introduction
2. Methods
2.1. Subjects
- SCI at C7-level;
- American Spinal Injury Association Impairment Scale (AIS) [9]: Grade C or D;
- Flexor and extensor carpi muscles preserved;
- Patients must be in the rehabilitation period;
- Admission into the NHPT in the acute phase;
- Possibility of functional improvement. Sequelae phase not yet reached;
- The maximum time elapsed since the injury cannot exceed six months;
- Written informed consent prior to the beginning of the experiment.
2.2. Human-Machine Interface
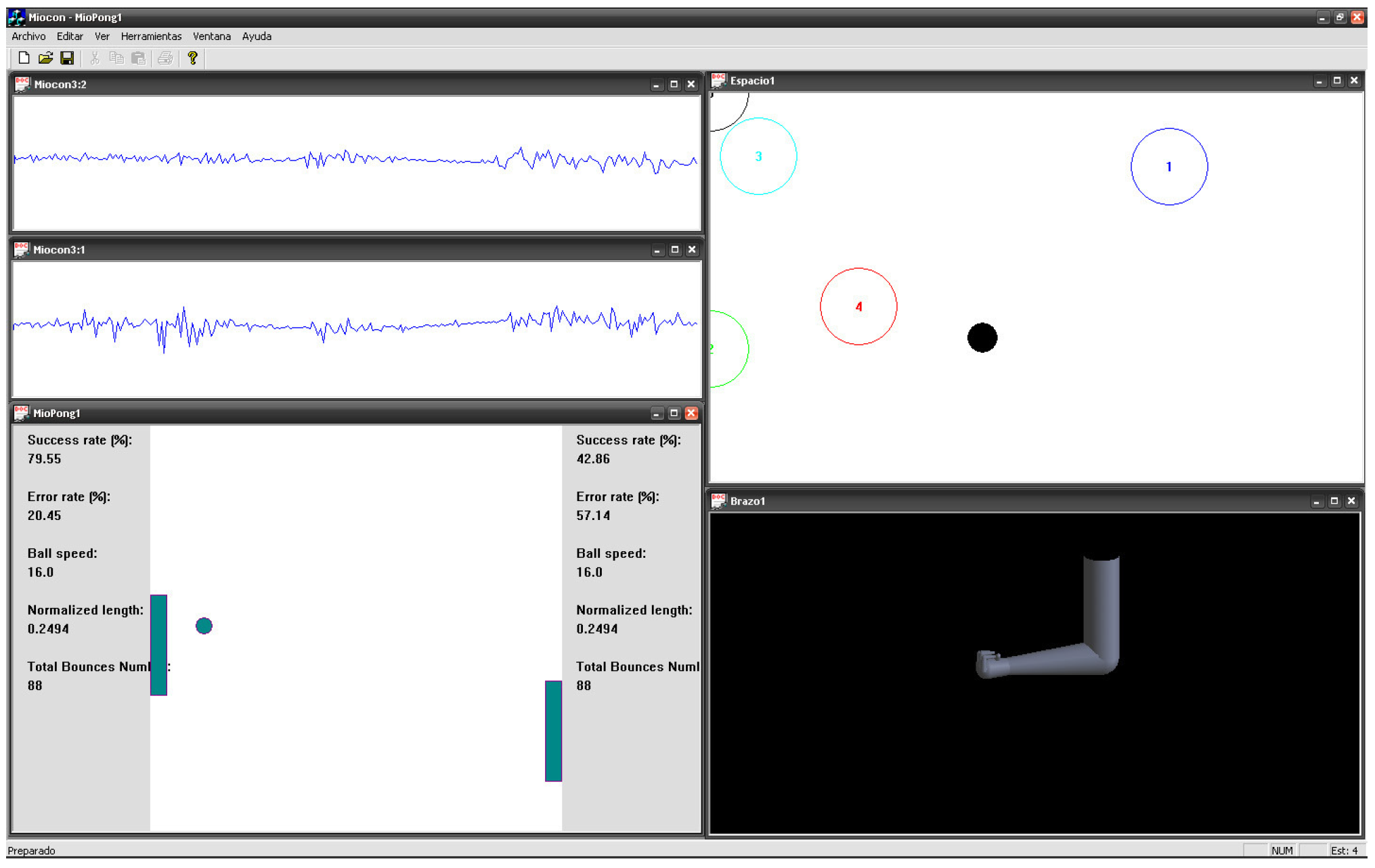
- The signal viewer, where EMG signals are checked in the time domain;
- The state navigator, allowing two-dimensional movements of a screen pointer depending on the detected EMG amplitude of two muscles and hence their contraction level. x-axis and y-axis displacements are related to the EMG amplitude of each muscle involved. In this way, targets can be located on screen by the user by contracting his or her muscles. These targets are plotted as circles as shown in Figure 1;
- The virtual arm, a 3D-design arm allowing the simulation of movements for prosthetic training. This tool uses the targets defined in the state navigator. Thus, each movement of the virtual arm can be associated with each of the defined targets. This application is intended to provide an approximation to what would be the real myoelectric prosthesis control. Hence, the application can assess the prosthesis adequation to the patient;
- Myo-Pong, which is a version of a table tennis video game [12]. In this game, two paddles are meant to maintain the control of a ball. Therefore, each paddle is controlled by the EMG amplitude from a different muscle suitably chosen depending on the type of disability. The paddle displacement downwards is proportional to the muscle contraction level.
2.3. Performance Indexes
- Time to reach the target (TRT), the time to achieve a defined effort from the rest state, i.e., the time to reach each target with the pointer from the top left corner of the tool;
- Time to rest (TR), the time to reach the rest state, i.e., the top left corner;
- Time on target (ToT), the time the user can maintain the pointer on a given target;
- Fatigue time (FT), defined as the elapsed time before the user cannot continue to keep lock on the targets. This time is defined since the user starts navigating, although other definitions are possible depending on the task.
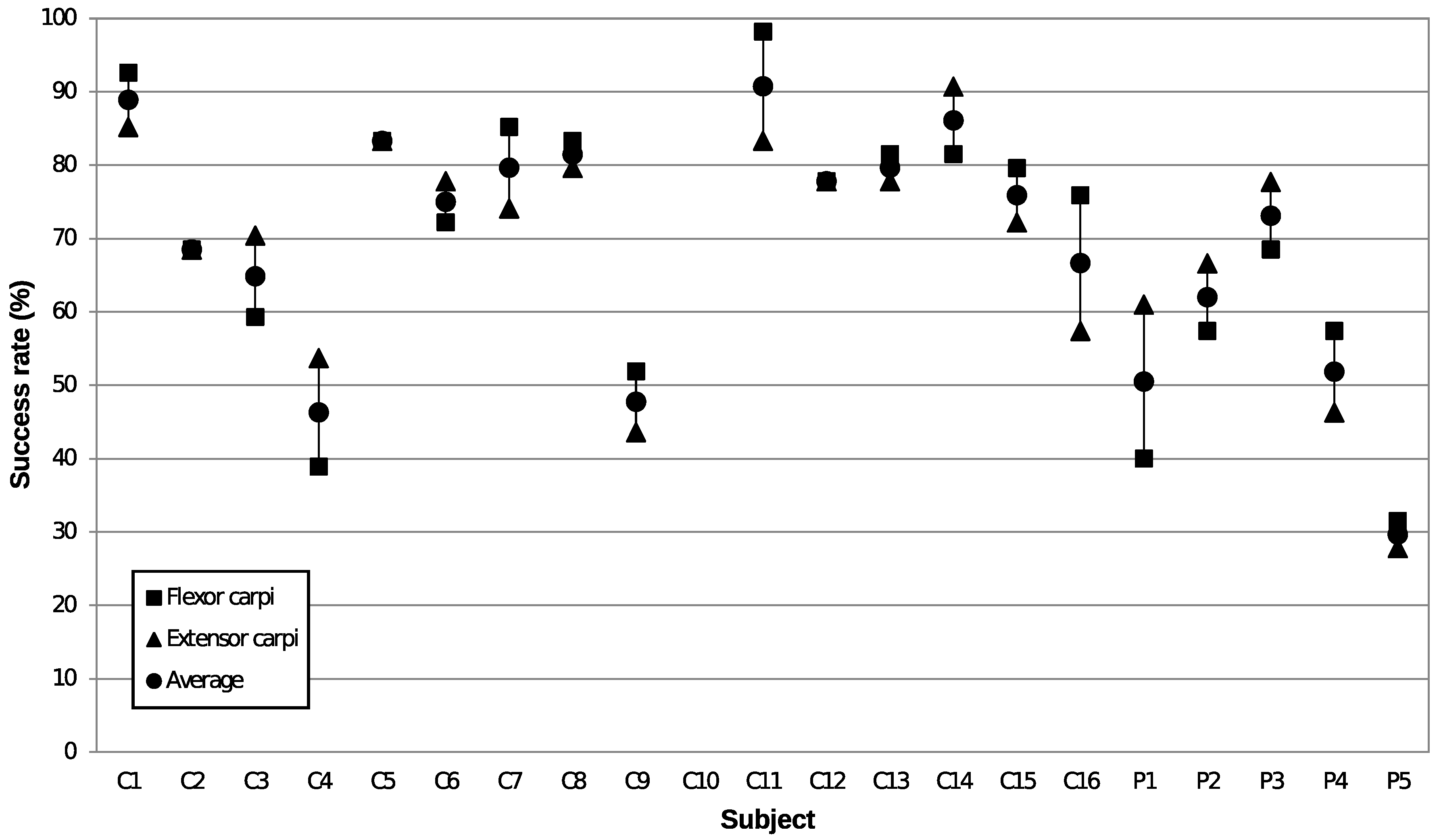
- Success rate (SR), the ratio of successful hits to unsuccessful hits, the latter being defined as the total amount of collisions against the player’s wall (left or right side of the window). The complementary is the Error Rate (ER), which is the failure ratio related to the total amount of collisions;
- Admissible speed (AS), measures the maximum ball speed the user can track, without exceeding a given error rate. The AS can be related to the ability to perform rapid actions with a prosthetic limb;
- Precision control (PC), measures the accuracy in the actions. The measurement is performed by changing the bar length, i.e., the shorter the bar, the more difficult the hits. The bar size setting is suitable for practicing accuracy in proportional control of prosthetic limbs;
- Fatigue time (FT), measures the time interval that maintains a steady ER once this rate is stabilised. The measure is finished when the ER is increased due to muscle fatigue.
2.4. Evaluation Protocol
2.5. Data Analysis
3. Results
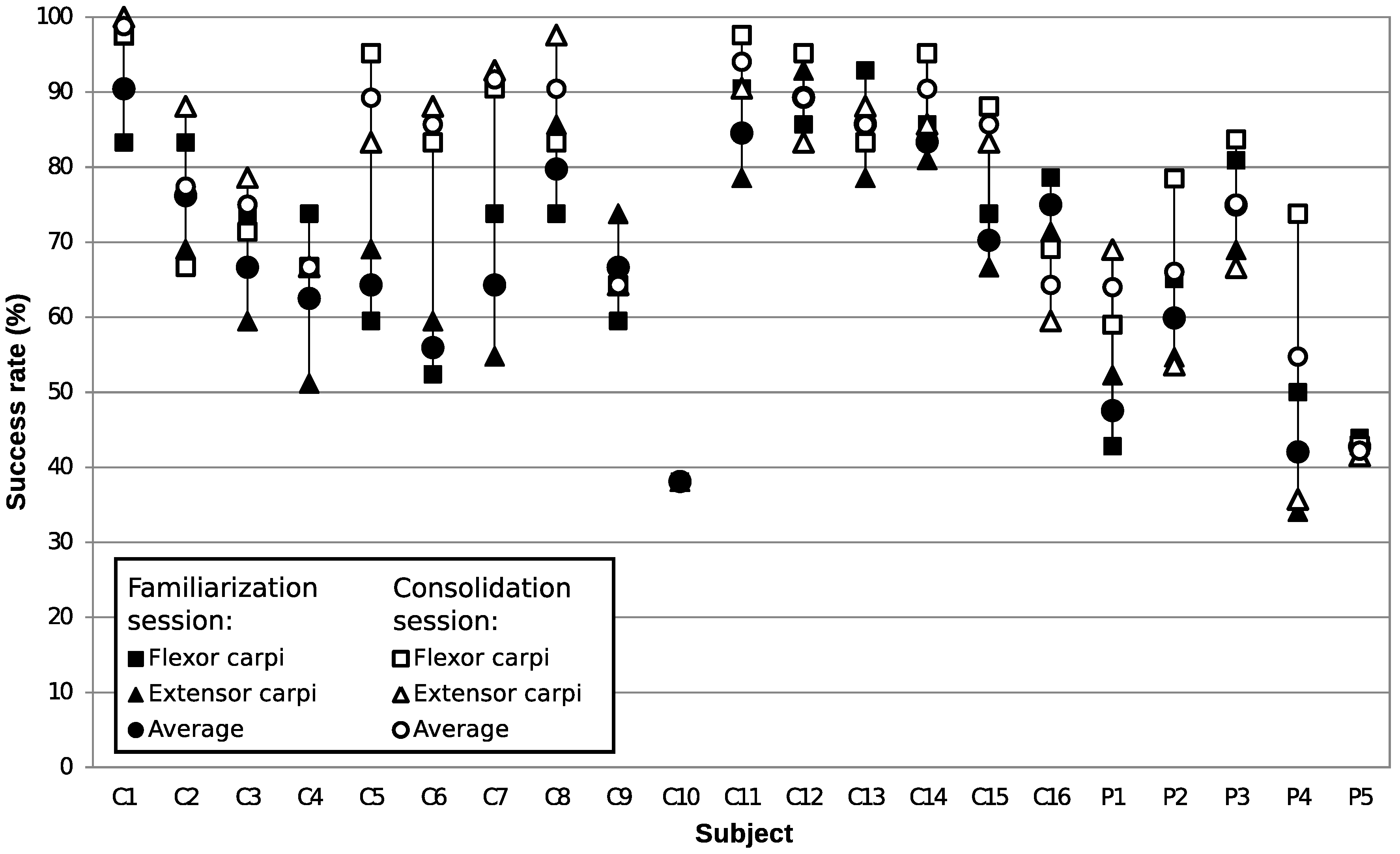
3.1. Evolution with the State Navigator
3.2. Adaptation to the State Navigator
3.3. Homogeneity of the Populations
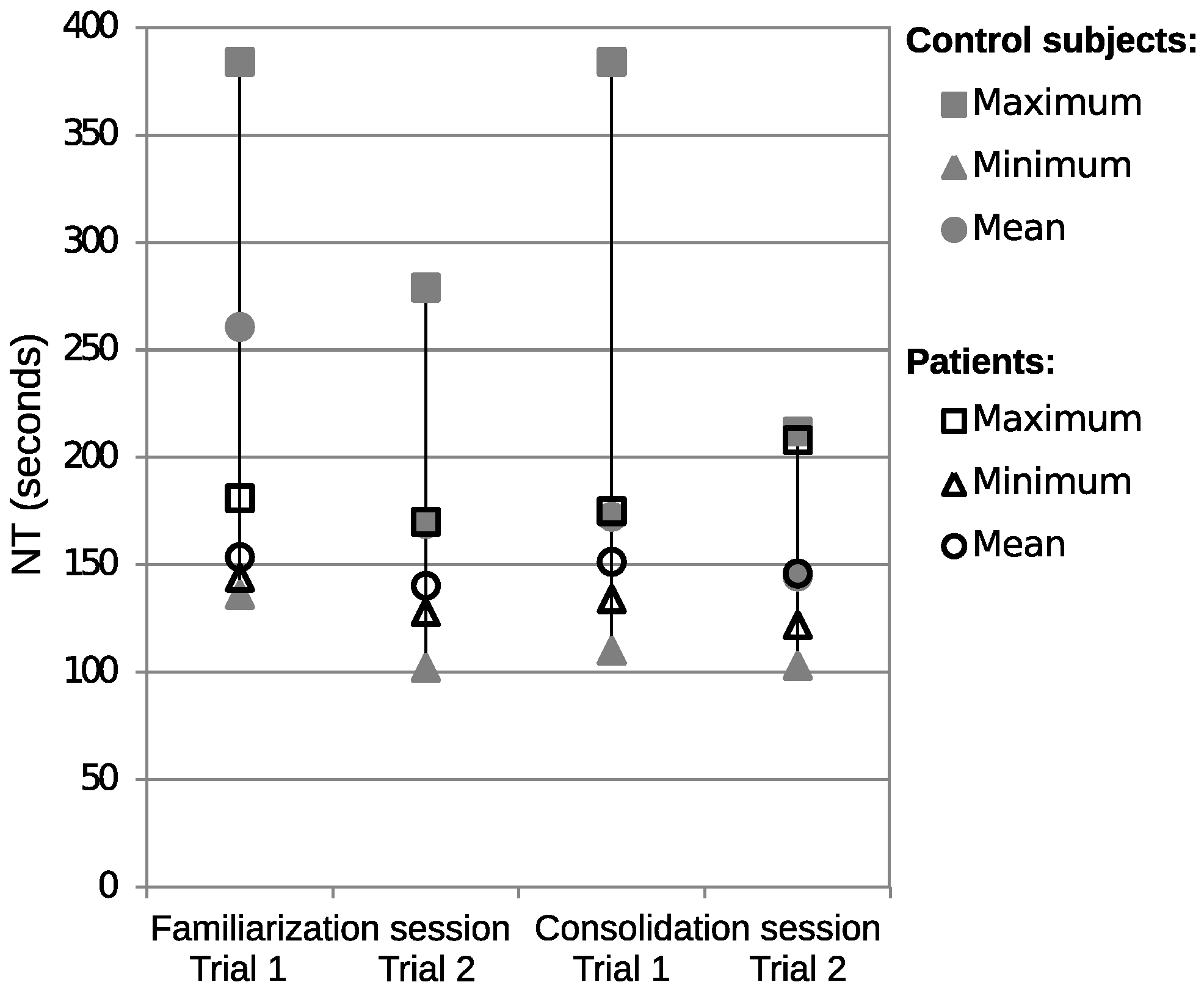
3.4. Evolution with the Myo-Pong Tool
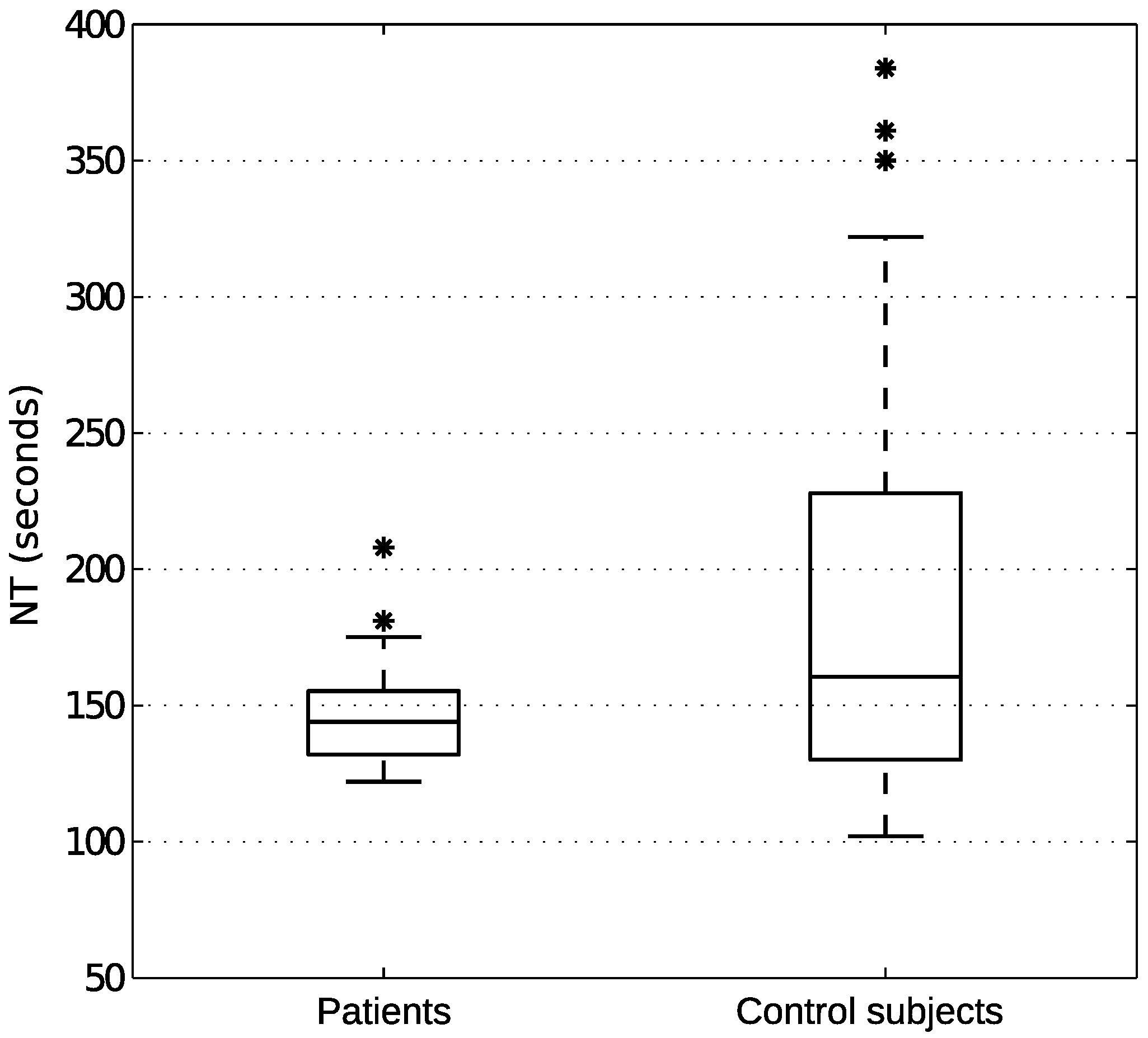
3.5. Myo-Pong between Populations
4. Discussion
4.1. State Navigator
4.2. The Myo-Pong Tool
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| UVa | University of Valladolid (Universidad de Valladolid) |
| UVa-NTS | UVa neuromuscular training system |
| CS | Control subjects |
| SCI | Spinal cord injury |
| EMG | Electromyography |
| VR | Virtual reality |
| NHPT | National Hospital for Paraplegics of Toledo |
| TRT | Time to reach the target |
| TR | Time to rest |
| ToT | Time on target |
| FT | Fatigue time |
| SR | Success rate |
| AS | Admissible speed |
| PC | Precision control |
| NT | Navigation time |
| DMVC | Desired maximum voluntary contraction |
| MVC | Maximal voluntary contraction |
| DMC | Desired medium contraction |
References
- Snoek, G.J.; IJzerman, M.J.; Hermens, H.J.; Maxwell, D.; Biering-Sorensen, F. Survey of the needs of patients with spinal cord injury: Impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004, 42, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Janssen-Potten, Y.; Seelen, H.; Bongers-Janssen, H.; van der Woude, L. Assessment of upper extremity muscle function in persons with tetraplegia. J. Electromyogr. Kinesiol. 2008, 18, 516–526. [Google Scholar] [CrossRef] [PubMed]
- Colombo, R.; Pisano, F.; Mazzone, A.; Delconte, C.; Micera, S.; Carrozza, M.C.; Dario, P.; Minuco, G. Design strategies to improve patient motivation during robot-aided rehabilitation. J. NeuroEng. Rehabil. 2007, 4, 3. [Google Scholar] [CrossRef] [PubMed]
- Van de Meent, H.; Baken, B.; Van Opstal, S.; Hogendoorn, P. Critical illness VR rehabilitation device (X-VR-D): Evaluation of the potential use for early clinical rehabilitation. J. Electromyogr. Kinesiol. 2008, 18, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Armagan, O.; Tascioglu, F.; Oner, C. Electromyographic Biofeedback in the Treatment of the Hemiplegic Hand. Am. J. Phys. Med. Rehabil. 2003, 82, 856–861. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.K.; Sherwood, A.M. Reliability of surface electromyographic measurements from subjects with spinal cord injury during voluntary motor tasks. J. Rehabil. Res. Dev. 2005, 42, 413. [Google Scholar] [CrossRef] [PubMed]
- Song, R.; Tong, K.-Y.; Hu, X.; Li, L. Assistive Control System Using Continuous Myoelectric Signal in Robot-Aided Arm Training for Patients After Stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2008, 16, 371–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De la Rosa, R.; Alonso, A.; Carrera, A.; Durán, R.; Fernández, P. Man-machine interface system for neuromuscular training and evaluation based on EMG and MMG signals. Sensors 2010, 10, 11100–11125. [Google Scholar] [CrossRef] [PubMed]
- Maynard, F.M., Jr.; Bracken, M.B.; Creasey, G.; Ditunno, J.F., Jr.; Donovan, W.H.; Ducker, T.B.; Garber, S.L.; Marino, R.J.; Stover, S.L.; Tator, C.H.; et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. Spinal Cord 1997, 35, 266–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carrera, A.; de la Rosa, R.; Alonso, A. Programmable gain amplifiers with DC suppression and low output offset for bioelectric sensors. Sensors 2013, 13, 13123–13142. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.J.; Feng, X.; Johnson, L.M.; Winters, J.M. Potential of a suite of robot/computer-assisted motivating systems for personalized, home-based, stroke rehabilitation. J. NeuroEng. Rehabil. 2007, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- De la Rosa, R.; Alonso, A.; de la Rosa, S.; Abasolo, D. Myo-Pong: A neuromuscular game for the UVa-neuromuscular training system platform. In Proceedings of the 2008 Virtual Rehabilitation, Vancouver, BC, Canada, 25–27 August 2008; p. 61. [Google Scholar] [CrossRef]
- Yang, J.F.; Winter, D.A. Electromyography reliability in maximal and submaximal isometric contractions. Arch. Phys. Med. Rehabil. 1983, 64, 417–420. [Google Scholar] [PubMed]
- Yang, J.F.; Winter, D.A. Electromyographic amplitude normalization methods: Improving their sensitivity as diagnostic tools in gait analysis. Arch. Phys. Med. Rehabil. 1984, 65, 517–521. [Google Scholar] [PubMed]
- Dowdy, S.; Weardon, S.; Chilko, D. Statistics for Research, 3rd ed.; Wiley Series in Probability and Statistics; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004; p. 627. [Google Scholar]
- Van Dijk, L.; van der Sluis, C.K.; van Dijk, H.W.; Bongers, R.M. Learning an EMG Controlled Game: Task-Specific Adaptations and Transfer. PLoS ONE 2016, 11, e0160817. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, S.; Erlandson, B.E.; Gerdle, B. A Personal Computer-based System for Real-time Analysis of Surface EMG Signals during Static and Dynamic Contractions. J. Electromyogr. Kinesiol. 1994, 4, 170–180. [Google Scholar] [CrossRef]
- Tabor, A.; Bateman, S.; Scheme, E. Evaluation of Myoelectric Control Learning Using Multi-Session Game-Based Training. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1680–1689. [Google Scholar] [CrossRef] [PubMed]
- Cremoux, S.; Amarantini, D.; Tallet, J.; Dal Maso, F.; Berton, E. Increased antagonist muscle activity in cervical SCI patients suggests altered reciprocal inhibition during elbow contractions. Clin. Neurophysiol. 2016, 127, 629–634. [Google Scholar] [CrossRef] [PubMed]



| Patient | Age | Gender |
|---|---|---|
| 1 | 34 | Female |
| 2 | 38 | Male |
| 3 | 41 | Male |
| 4 | 66 | Male |
| 5 | 37 | Male |
| Gender | Age | Mean Age | Number |
|---|---|---|---|
| Male | 24–46 | 31.3 | 10 |
| Female | 23–38 | 28.8 | 6 |
| Session, | Control Subjects | Patients | ||
|---|---|---|---|---|
| Level | p | Variance | p | Variance |
| familiarisation, | 0.558 | p = 0.835 | 0.528 | p = 0.709 |
| low | F(15,15) = 0.896 | F(4,4) = 1.488 | ||
| consolidation, | 0.970 | p = 0.831 | 0.188 | p = 0.709 |
| low | F(14,14) = 0.831 | F(4,4) = 1.261 | ||
| consolidation, | 0.662 | p = 0.493 | 0.664 | p = 0.626 |
| high | F(14,14) = 1.453 | F(4,4) = 0.594 | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
de la Rosa, R.; Carrera, A.; Alonso, A.; Peñasco-Martín, B.; Gil-Agudo, A.; Abril, E.J. Myoelectric Gaming in the Rehabilitation of Patients with C7 Spinal Cord Injury. Appl. Sci. 2019, 9, 1912. https://doi.org/10.3390/app9091912
de la Rosa R, Carrera A, Alonso A, Peñasco-Martín B, Gil-Agudo A, Abril EJ. Myoelectric Gaming in the Rehabilitation of Patients with C7 Spinal Cord Injury. Applied Sciences. 2019; 9(9):1912. https://doi.org/10.3390/app9091912
Chicago/Turabian Stylede la Rosa, Ramón, Albano Carrera, Alonso Alonso, Benito Peñasco-Martín, Angel Gil-Agudo, and Evaristo J. Abril. 2019. "Myoelectric Gaming in the Rehabilitation of Patients with C7 Spinal Cord Injury" Applied Sciences 9, no. 9: 1912. https://doi.org/10.3390/app9091912
APA Stylede la Rosa, R., Carrera, A., Alonso, A., Peñasco-Martín, B., Gil-Agudo, A., & Abril, E. J. (2019). Myoelectric Gaming in the Rehabilitation of Patients with C7 Spinal Cord Injury. Applied Sciences, 9(9), 1912. https://doi.org/10.3390/app9091912






