What Do We Know about the Use of EEG Monitoring during Equine Anesthesia: A Review
Abstract
Featured Application
Abstract
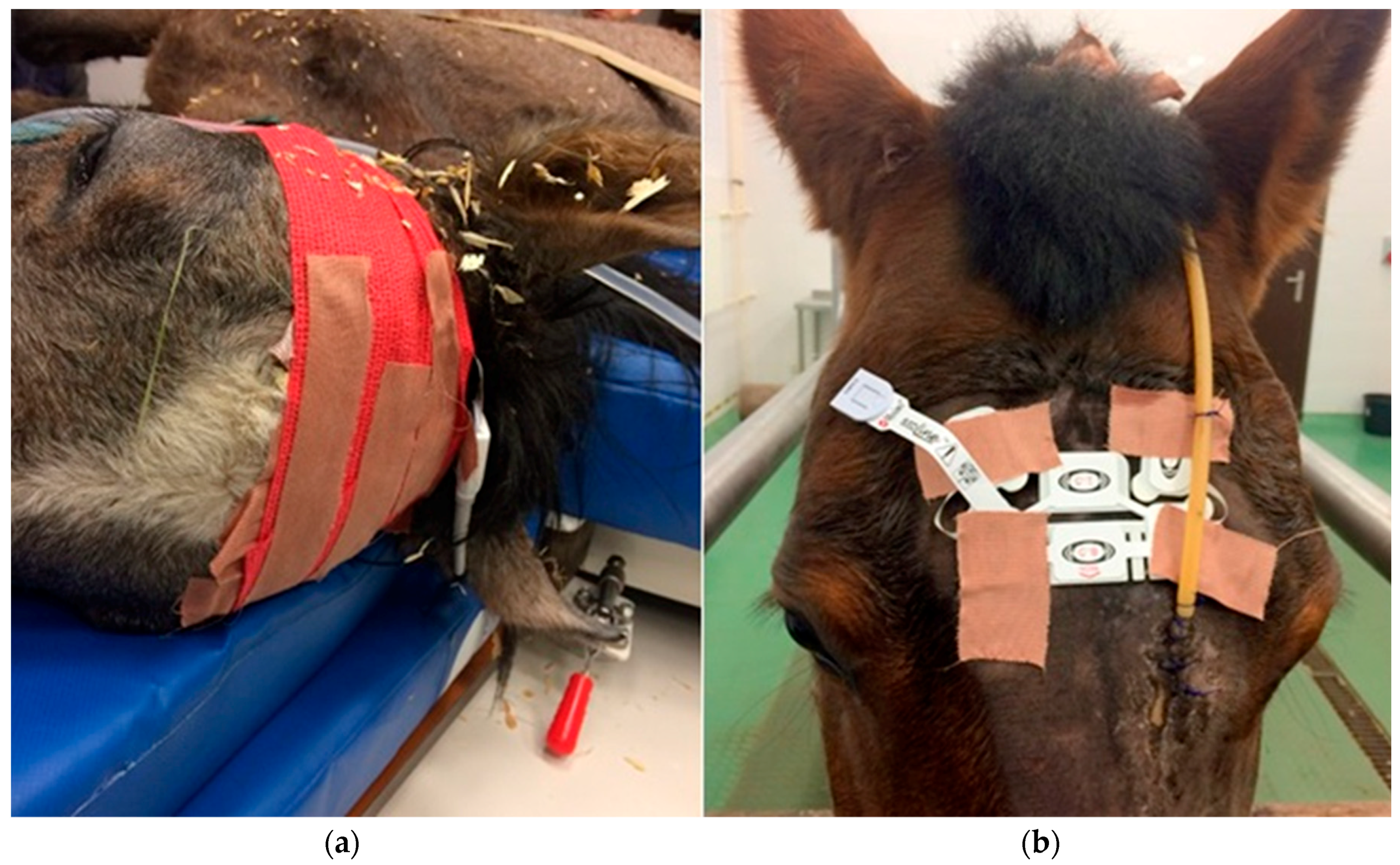
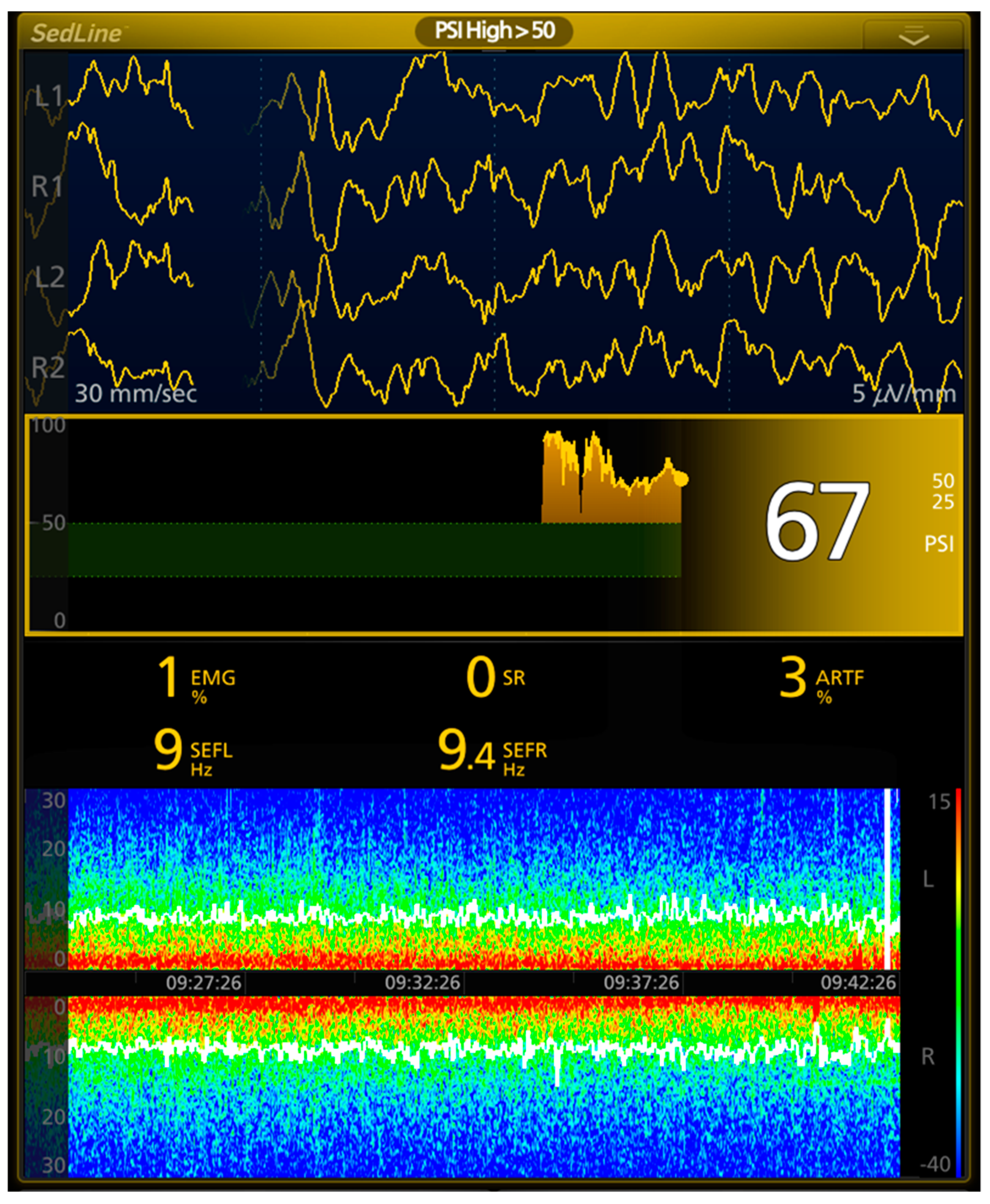
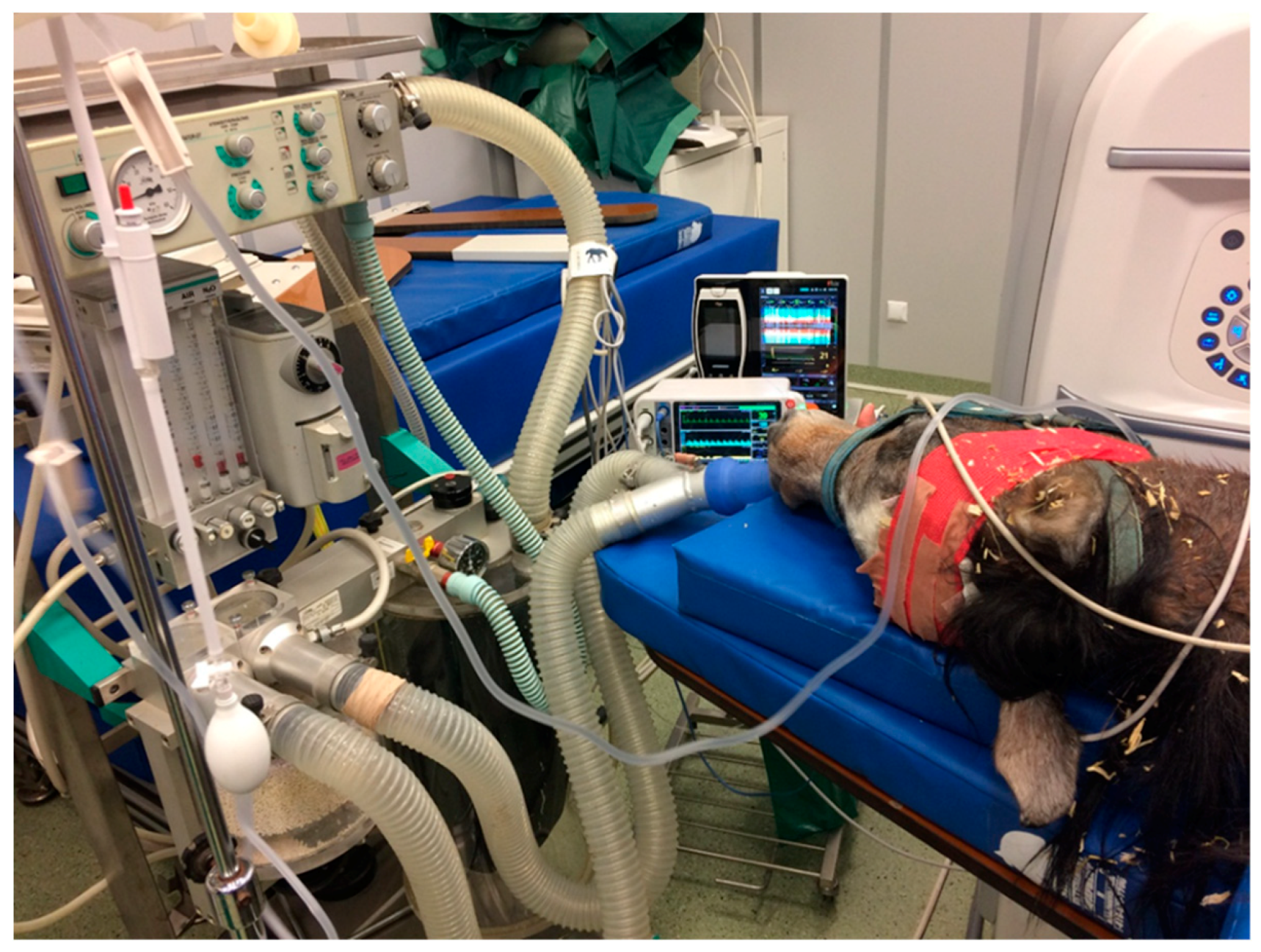
1. Introduction
2. Physiology of Brain Activity—Why Is the EEG so Important in the Management of Anesthesia?
- δ (0–4 Hz)—with a large amplitude, characteristic for deep sleep or anesthesia
- θ (4–8 Hz)—observed in light sleep or anesthesia
- α (8–13 Hz)—in awake but relaxed state
3. EEG Monitoring during General Anesthesia: Does It Improve Anesthetic Management?
- techniques of good EEG practice [9]
4. Analysis of EEG and Its Usefulness in Equine General Anesthesia
5. Limitations of EEG Use and Further Research in Equine Anesthesia
6. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Noachtar, S.; Binnie, C.; Ebersole, J. A glossary of terms most commonly used by clinical electroencephalographers and proposal for the report form for the EEG findings. Klin. Neurophysiol. 2004, 35, 5–21. [Google Scholar]
- Tooley, M.A.; Grant, L.J.; Davies, A.R. A micoprocessor based instrument for the spectral analysis of the EEG in anaesthesia. Clin. Phys. Physiol. Meas. 1984, 5, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Guedel, A.E. Third stage ether anesthesia: A sub-classification regarding the significance of the position and movements of the eyeball. Pa Med. J. 1921, 24, 375–380. [Google Scholar] [CrossRef]
- Rampil, I.J. Monitoring depth of anesthesia. Curr. Opin. Anaesthesiol. 2001, 14, 649–653. [Google Scholar] [CrossRef]
- Aminoff, M.J. Electroencephalography: General principles and clinical applications. In Electrodiagnosis in Clinical Neurology; Aminoff, M.J., Ed.; Churchill Livingstone: New York, NY, USA, 1986; pp. 21–75. [Google Scholar]
- Klemm, W.R. Electroencephalography in the diagnosis of epilepsy. Probl. Vet. Med. 1989, 1, 535–557. [Google Scholar] [PubMed]
- Croft, P.G. The EEG as an aid to diagnoses of nervous diseases in the dog and cat. J. Small Anim. Pract. 1964, 5, 540–541. [Google Scholar]
- Holliday, T.A.; Cunningham, J.G.; Gutnick, M.J. Comparative clinical and electroencephalographic studies of canine epilepsy. Epilepsia 1970, 11, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Redding, R.W. A simple technique for obtaining an electroencephalogram of the dog. Am. J. Vet. Res. 1964, 25, 854–857. [Google Scholar]
- Usenick, M.W.; Kitchell, R.L.; Herschler, R.G. The EEG as an aid to diagnosis of nervous diseases in the dog and cat. J. Small Anim. Pract. 1962, 3, 205–208. [Google Scholar]
- Swanson, L.W. What is the brain? Trends Neurosci. 2000, 23, 519–527. [Google Scholar] [CrossRef]
- Lemke, K.A. Understanding the pathophysiology of perioperative pain. Can. Vet. J. 2004, 45, 405. [Google Scholar] [PubMed]
- Furness, J.B. The organisation of the autonomic nervous system: Peripheral connections. Auton. Neurosci. Basic Clin. 2006, 130, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Deco, G.; Jirsa, V.K.; Robinson, P.A.; Breakspear, M.; Friston, K. The dynamic brain: From spiking neurons to neural masses and cortical fields. PLoS Comput. Biol. 2008, 4, e1000092. [Google Scholar] [CrossRef] [PubMed]
- Hess, A.; Sergejeva, M.; Budinsky, L.; Zeilhofer, H.U.; Brune, K. Imaging of hyperalgesia in rats by functional MRI. Eur. J. Pain 2007, 11, 109–119. [Google Scholar] [CrossRef] [PubMed]
- da Silva, F.L. EEG: Origin and Measurement. In EEG—Fmri; Mulert, C., Lemieux, L., Eds.; Springer: Berlin, Germany, 2009. [Google Scholar]
- Constant, I.; Sabourdin, N. The EEG signal: A window on the cortical brain activity. Pediatric Anesth. 2012, 22, 539–552. [Google Scholar] [CrossRef]
- Jameson, L.C.; Sloan, T.B. Using EEG to monitor anesthesia drug effects during surgery. J. Clin. Monit. Comput. 2006, 20, 445–472. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.M. Characteristics of electroencephalogram signatures in sedated patients induced by various anesthetic agents. J. Dent. Anesth. Pain Med. 2017, 17, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Purdon, P.L.; Sampson, A.; Pavone, K.J.; Brown, E.N. Clinical electroencephalography for anesthesiologists part I: Background and basic signatures. Anesthesiol. J. Am. Soc. Anesthesiol. 2015, 123, 937–960. [Google Scholar]
- Antognini, J.F.; Wang, X.W.; Carstens, E. Isoflurane action in the spinal cord blunts electroencephalographic and thalamic–reticular formation responses to noxious stimulation in goats. Anesthesiol. J. Am. Soc. Anesthesiol. 2000, 92, 559. [Google Scholar] [CrossRef]
- Steffey, E.P. Concepts of general anesthesia and assessment of adequacy of anesthesia for animal surgery. In Animal Pain; Kitchell, R.L., Erickson, H.H., Eds.; Springer: New York, NY, USA, 1983; pp. 133–150. [Google Scholar]
- Steriade, M.; Amzica, F.; Contreras, D. Cortical and thalamic cellular correlates of electroencephalographic burst-suppression. Electroenceph. Clin. Neurophysiol. 1994, 90, 1–16. [Google Scholar] [CrossRef]
- Eger, E.; Saidman, L.; Brandstater, B. Minimum alveolar anesthetic concentration: A standard of anesthetic potency. Anesthesiology 1965, 26, 756–763. [Google Scholar] [CrossRef] [PubMed]
- Otto, K.A.; Voigt, S.; Piepenbrock, S. Differences in quantitated electroencephalographic variables during surgical stimulation of horses anesthetized with isoflurane. Vet. Surg. 1996, 25, 249–255. [Google Scholar] [CrossRef]
- Bovill, J.G.; Antognini, J.F.; Atherley, R.; Carstens, E. Isoflurane action in spinal cord indirectly depresses cortical activity associated with electrical stimulation of the reticular formation. Anesth. Analg. 2003, 96, 999–1003. [Google Scholar] [CrossRef] [PubMed]
- Dunigan, C.E.; Oglesbee, M.J.; Podell, M. Seizure activity associated with equine protozoal myeloencephalitis. Progr. Vet. Neurol. 1995, 6, 50–54. [Google Scholar]
- Bimar, J.; Bellville, J.W. Arousal reactions during anesthesia in man. Anesthesiology 1977, 47, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Long, C.W.; Shah, N.K.; Loughlin, C. A comparison of EEG determinants of near-awakening from iso£urane and fentanyl anesthesia. Anesth. Analg. 1989, 69, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Rampil, I.J.; Matteo, R.S. Changes in EEG spectral edge frequency correlate with the haemodynamic response to laryngoscopy and intubation. Anaesthesiology 1987, 67, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Schwender, D.; Daunderer, M.; Mulzer, S. Spectral edge frequency of the electroencephalogram to monitor ‘depth’ of anaesthesia with iso£urane or propofol. Br. J. Anaesth. 1996, 77, 179–184. [Google Scholar] [CrossRef]
- Huang, H.H.; Lee, Y.H.; Chan, H.L.; Wang, Y.P.; Huang, C.H. Using a short-term parameter of heart rate variability to distinguish awake from isoflurane anesthetic states. Med. Biol. Eng. Comput. 2008, 46, 977–984. [Google Scholar] [CrossRef]
- Akeju, O.; Westover, M.B.; Pavone, K.J.; Sampson, A.L.; Hartnack, K.E.; Brown, E.N.; Purdon, P.L. Effects of sevoflurane and propofol on frontal electroencephalogram power and coherence. Anesthesiology 2014, 121, 990–998. [Google Scholar] [CrossRef]
- Giovagnoli, G.; de Feo, M.R.; Frascarelli, M. The use of EEG and ECG ambulatory technique in horses: Preliminary observations. Pferdeheilkunde 1996, 12, 446–449. [Google Scholar]
- Cousillas, H.; Oger, M.; Rochais, C.; Pettoello, C.; Ménoret, M.; Henry, S.; Hausberger, M. An Ambulatory Electroencephalography System for Freely Moving Horses: An Innovating Approach. Front. Vet. Sci. 2017, 4, 57. [Google Scholar] [CrossRef] [PubMed]
- Mysinger, P.W.; Redding, R.W.; Vaughan, J.T.; Purohit, R.C.; Holladay, J.A. Electroencephalographic patterns of clinically normal, sedated and tranquilized newborn foals and adult horses. Am. J. Vet. Res. 1985, 46, 36–41. [Google Scholar] [PubMed]
- Ekstrom, P.M.; Short, C.E.; Geimer, T.R. Electroencephalography of detomidine-ketamine-halothane and detomidine-ketamine-isoflurane anesthetized horses during surgery: A comparison. Vet. Surg. 1993, 22, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.M.; Short, C.E.; Ekstrom, P.M. Quantitative electroencephalographic evaluation to determine the quality of analgesia during anesthesia of horses for arthroscopic surgery. Am. J. Vet. Res. 1995, 56, 374–379. [Google Scholar] [PubMed]
- Murrell, J.C.; Johnson, C.B.; White, K.L. Changes in the EEG during castration in horses and ponies anaesthetized with halothane. Vet. Anaesth. Analg. 2003, 30, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Tokushige, H.; Kakizaki, M.; Ode, H.; Okano, A.; Okada, J.; Kuroda, T.; Wakuno, A.; Ohta, M. Validation of the bispectral index as an indicator of anesthetic depth in Thoroughbred horses anesthetized with sevoflurane. J. Equine Sci. 2016, 27, 169–173. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yamashita, K.; Akashi, N.; Katayama, Y.; Uchida, Y.; Umar, M.A.; Itami, T.; Inoue, H.; Sams, R.A.; MUIR, W.W., III. Evaluation of bispectral index (BIS) as an indicator of central nervous system depression in horses anesthetized with propofol. J. Vet. Med Sci. 2009, 71, 1465–1471. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tünsmeyer, J.; Hopster, K.; Kästner, S.B. Clinical Use of a Multivariate electroencephalogram (narcotrend) for assessment of anesthetic Depth in horses during isoflurane–Xylazine anesthesia. Front. Vet. Sci. 2016, 3, 25. [Google Scholar] [CrossRef]
- Short, C.E.; Ekstrom, P.M. Compressed spectral analysis of the EEG as an indicator of anesthetic quality during anesthesia for orthopedic surgery in the horses. In Proceedings of the Annual Convention of the American Association of Equine Practitioners, San Antonio, TX, USA, 5–8 December 1993. [Google Scholar]
- Auer, J.A.; Amend, J.F.; Garner, H.E. Electroencephalographic responses during volatile anesthesia in domestic ponies: A comparative study of isoflurane, enflurane, methoxyflurane, and halothane. J. Equine Med. Surg. 1979, 3, 130–134. [Google Scholar]
- Kongara, K.; Chambers, J.P.; Johnson, C.B. Electroencephalographic responses of tramadol, parecoxib and morphine to acute noxious electrical stimulation in anaesthetised dogs. Res. Vet. Sci. 2010, 88, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Murrell, J.C.; White, K.L.; Johnson, C.B.; Taylor, P.M.; Doherty, T.J.; Waterman-Pearson, A.E. Investigation of the EEG effects of intravenous lidocaine during halothane anaesthesia in ponies. Vet. Anaesth. Analg. 2005, 32, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Otto, K.A.; Voigt, S.; Piepenbrock, S.; Deegen, E. Effects of low dose ketamine on haemodynamic and electroencephalographic variables during surgery in isoflurane anaesthetised horses. J. Vet. Anaesth 1998, 25, 8–12. [Google Scholar] [CrossRef]
- Johnson, C.B.; Bloomfield, M.; Taylor, P.M. Effects of ketamine on the equine electroencephalogram during anesthesia with halothane in oxygen. Vet. Surg. 1999, 28, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.B.; Bloomfield, M.; Taylor, P.M. Effects of guaiphenesin on the equine electroencephalogram during anaesthesia with halothane in oxygen. Vet. Anaesth. Analg. 2000, 27, 6–12. [Google Scholar] [CrossRef]
- Johnson, C.B.; Bloomfield, M.; Taylor, P.M. Effects of thiopentone on the equine electroencephalogram during anaesthesia with halothane in oxygen. Vet. Anaesth. Analg. 2000, 27, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Rochai, C.; Henry, S.; Fureix, C.; Hausberger, M. Investigating attentional processes in depressive-like domestic horses (Equus caballus). Behav. Process. 2016, 124, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Lacombe, V.A.; Podell, M.; Furr, M. Diagnostic validity of electroencephalography in equine intracranial disorders. J. Vet. Intern. Med. 2001, 15, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.B.; Taylor, P.M. Comparison of the effects of halothane, isoflurane and methoxyflurane on the electroencephalogram of the horse. Br. J. Anaesth. 1998, 81, 748–753. [Google Scholar] [CrossRef]
- Fuchs, C. Narkolepsie oder REM-Schlafmangel? Ph.D. Thesis, LMU München, Tierärztliche Fakultät, Munich, Germany, 2017. [Google Scholar]
- van der Ree, M.; Wijnberg, I. A review on epilepsy in the horse and the potential of Ambulatory EEG as a diagnostic tool. Vet. Q. 2012, 32, 159–167. [Google Scholar] [CrossRef]
- Wijnberg, I.D.; van Der Ree, M.; van Someren, P. The applicability of ambulatory electroencephalography (AEEG) in healthy horses and horses with abnormal behaviour or clinical signs of epilepsy. Vet. Q. 2013, 33, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Johnston, G.M.; Taylor, P.M.; Holmes, M.A. The confidential enquiry of perioperative equine fatalities (CEPEF-1): Preliminary results. Equine Vet. J. 1998, 27, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Haga, H.A.; Dolvik, N.I. Electroencephalographic and cardiovascular variables as nociceptive indicators in isoflurane-anaesthetized horses. Vet. Anaesth. Analg. 2005, 32, 128–135. [Google Scholar] [CrossRef]
- Williams, D.C.; Aleman, M.R.; Brosnan, R.J.; Fletcher, D.J.; Holliday, T.A.; Tharp, B.; Kass, P.H.; Steffey, E.P.; Lecouteur, R.A. Electroencephalogram of healthy horses during inhaled anesthesia. J. Vet. Intern. Med. 2016, 30, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Grint, N.J.; Johnson, C.B.; Lorena, S.D.S.; Luna, S.; Hussni, C.A.; Whay, H.R.; Murrell, J.C. Electroencephalographic responses to a noxious surgical stimulus in mules, horses, and ponies. J. Equine Vet. Sci. 2014, 34, 955–962. [Google Scholar] [CrossRef]
- Otto, K.A.; Mally, P. Noxious stimulation during orthopaedic surgery results in EEG ‘arousal’ and ‘paradoxical arousal’ reaction in isoflurane-anaesthetised sheep. Res. Vet. Sci. 2003, 75, 103–112. [Google Scholar] [CrossRef]
- Diesch, T.J.; Mellor, D.J.; Johnson, C.B.; Lentle, R.G. Electroencephalographic responses to tail clamping in anaesthetized rat pups. Lab. Anim. 2009, 43, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Haskins, S.C. Monitoring the anesthetized patient. In Lumb and Jones Veterinary Anesthesia, 3rd ed.; Thurmon, J.C., Tranquilli, W.J., Benson, G.J., Eds.; Williams and Wilkins: Baltimore, MD, USA, 1996; pp. 409–424. [Google Scholar]
- Steffey, E.P. Inhalation anesthetics. In Lumb and Jones Veterinary Anesthesia, 3rd ed.; Thurmon, J.C., Tranquilli, W.J., Benson, G.J., Eds.; Williams and Wilkins: Baltimore, MD, USA, 1996; pp. 297–329. [Google Scholar]
- Bickford, R.G.; Fleming, N.; Billinger, T. Compression of EEG data. Trans. Am. Neurol. Assoc. 1971, 96, 118–122. [Google Scholar] [PubMed]
- Short, C.E.; Kallfelz, F.A.; Otto, K.; Otto, B.; Wallace, R. The effects of alpha 2-adrenocepter agonist analgesia on the central nervous system in an equine model. In Animal Pain; Short, C.E., Van Poznak, A., Eds.; Churchill Livingstone: New York, NY, USA, 1992. [Google Scholar]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drewnowska, O.; Lisowska, B.; Turek, B. What Do We Know about the Use of EEG Monitoring during Equine Anesthesia: A Review. Appl. Sci. 2019, 9, 3678. https://doi.org/10.3390/app9183678
Drewnowska O, Lisowska B, Turek B. What Do We Know about the Use of EEG Monitoring during Equine Anesthesia: A Review. Applied Sciences. 2019; 9(18):3678. https://doi.org/10.3390/app9183678
Chicago/Turabian StyleDrewnowska, Olga, Barbara Lisowska, and Bernard Turek. 2019. "What Do We Know about the Use of EEG Monitoring during Equine Anesthesia: A Review" Applied Sciences 9, no. 18: 3678. https://doi.org/10.3390/app9183678
APA StyleDrewnowska, O., Lisowska, B., & Turek, B. (2019). What Do We Know about the Use of EEG Monitoring during Equine Anesthesia: A Review. Applied Sciences, 9(18), 3678. https://doi.org/10.3390/app9183678





