Empirical Evidences for Urban Influences on Public Health in Hamburg
Abstract
1. Introduction
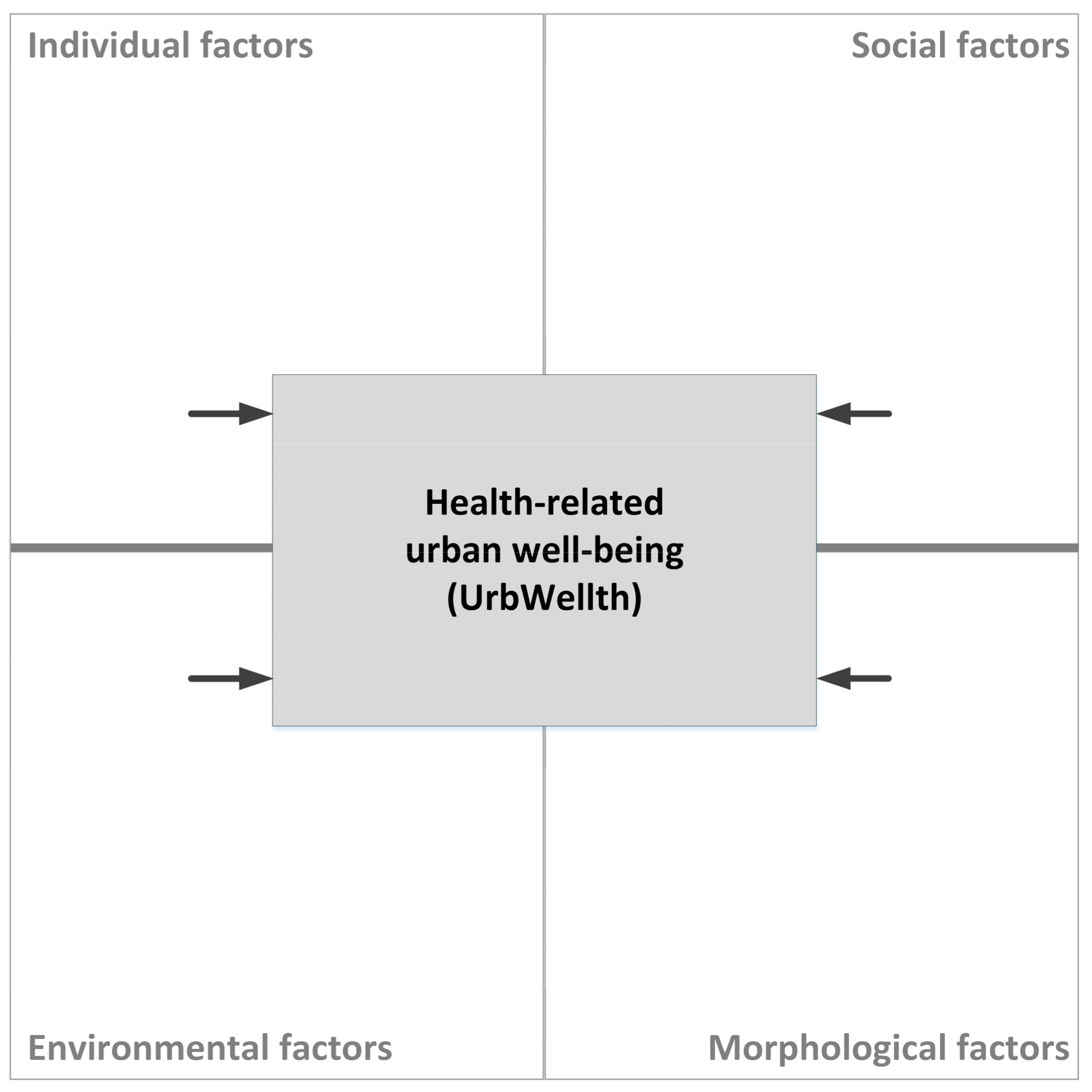
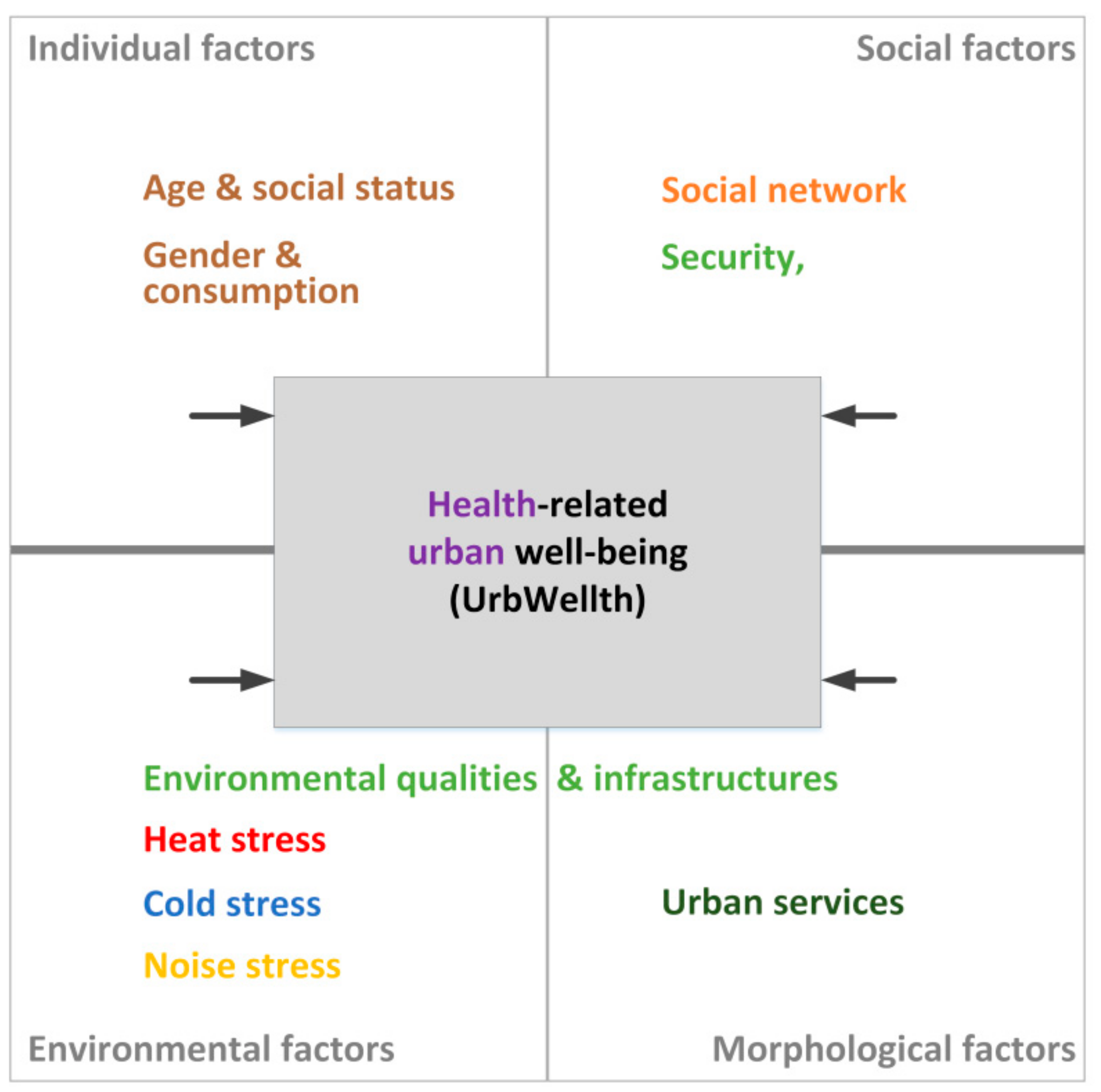
1.1. Conceptions of Urban Health and Research Design
1.2. Selected Empirical Results and Research Gaps
1.3. Research Questions
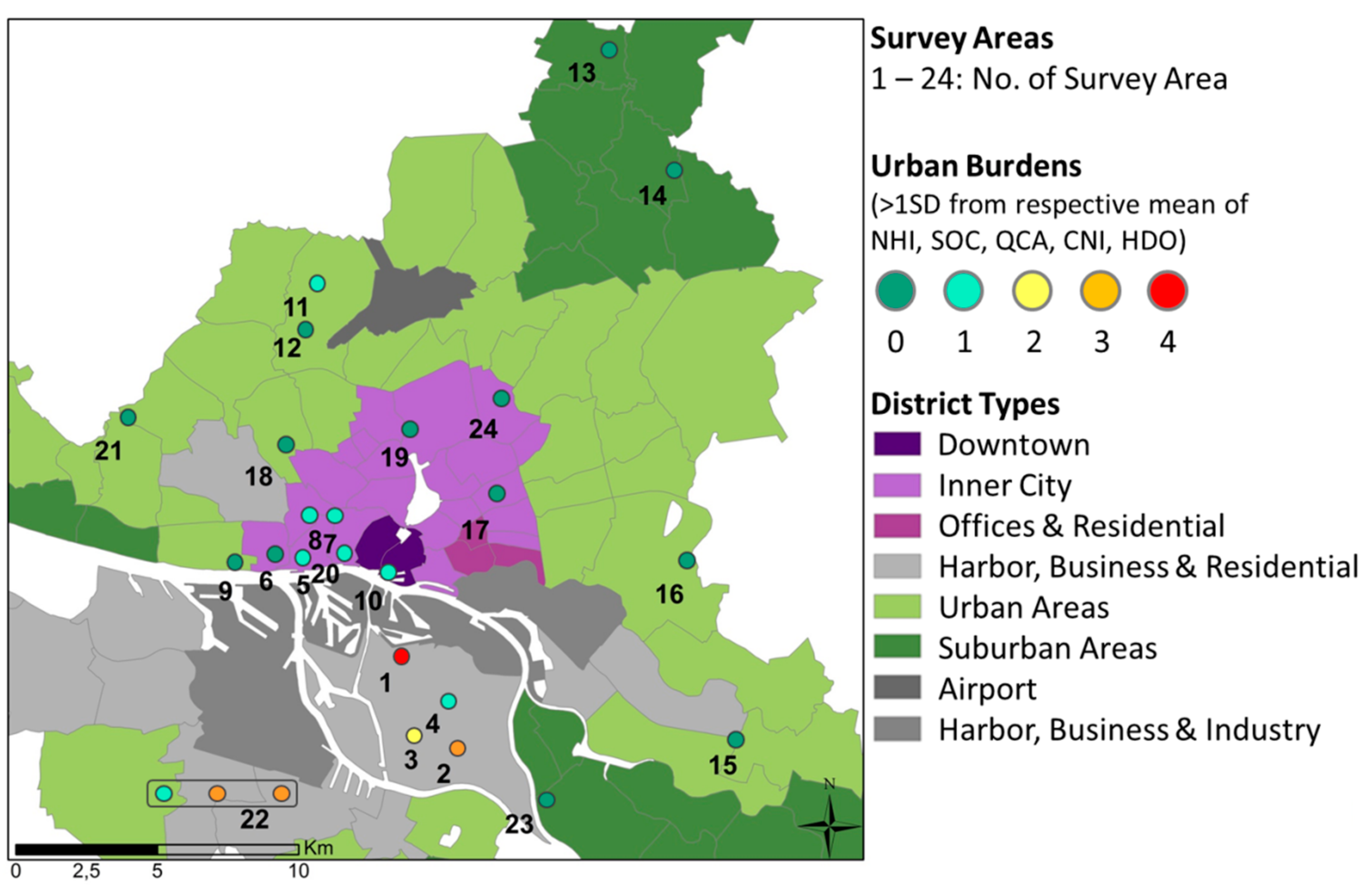
2. Materials and Methods
2.1. Data Collected
2.2. Methods and Statistical Tests
3. Results: Identifying Urban Influences on Health
3.1. Principal Component Analysis
3.2. Multiple Linear Regression Analyses
3.3. Answering the Research Question
4. Discussion
5. Conclusions and Outlook
5.1. Highlights of the Results in Reference to a Salutogenetic Perspective
5.2. Methodological Strengths and Limitations
5.3. Consequences for Research and Urban Planning
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Singh, G.K.; Siahpush, M. Widening rural-urban disparities in life expectancy, U.S., 1969–2009. Am. J. Prev. Med. 2014, 46, e19–e29. [Google Scholar] [CrossRef] [PubMed]
- Kyte, L.; Wells, C. Variations in life expectancy between rural and urban areas of England, 2001–2007. Health Stat. Q. 2010, 46, 25–50. [Google Scholar] [CrossRef] [PubMed]
- Vardoulakis, S.; Dear, K.; Wilkinson, P. Challenges and Opportunities for Urban Environmental Health and Sustainability: The HEALTHY-POLIS initiative. Environ. Health 2016, 15 Suppl 1, 30. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Nath, I.; Capon, A.; Hasan, N.; Jaron, D. Health and wellbeing in the changing urban environment: Complex challenges, scientific responses, and the way forward. Curr. Opin. Environ. Sustain. 2012, 4, 465–472. [Google Scholar] [CrossRef]
- Van Kamp, I.; Leidelmeijer, K.; Marsman, G.; de Hollander, A. Urban environmental quality and human well-being. Landsc. Urban Plan. 2003, 65, 5–18. [Google Scholar] [CrossRef]
- Hancock, T. Lalonde and beyond: Looking back at “A New Perspective on the Health of Canadians”. Health Promot. Int. 1986, 1, 93–100. [Google Scholar] [CrossRef]
- Coutts, C. Green Infrastructure and Public Health; Routledge: Abingdon/Oxon, UK; New York, NY, USA, 2016; ISBN 978-0415711364. [Google Scholar]
- Evans, R.G.; Stoddart, G.L. Producing health, consuming health care. Soc. Sci. Med. (1982) 1990, 31, 1347–1363. [Google Scholar] [CrossRef]
- Vlahov, D.; Freudenberg, N.; Proietti, F.; Ompad, D.; Quinn, A.; Nandi, V.; Galea, S. Urban as a determinant of health. J. Urban Health Bull. N. Y. Acad. Med. 2007, 84, 16–26. [Google Scholar] [CrossRef]
- Barton, H.; Grant, M. A health map for the local human habitat. J. R. Soc. Promot. Health 2006, 126, 252–253. [Google Scholar] [CrossRef]
- Galea, S.; Freudenberg, N.; Vlahov, D. Cities and population health. Soc. Sci. Med. (1982) 2005, 60, 1017–1033. [Google Scholar] [CrossRef]
- Coutts, C. Public health ecology. J. Environ. Health 2010, 72, 53–55. [Google Scholar] [PubMed]
- Cummins, S. Ecological Approaches to Public Health. In Health Geographies: A Critical Introduction; Brown, T., Andrews, G.J., Cummins, S., Greenhough, B., Lewis, D., Power, A., Eds.; Wiley Blackwell: Hoboken, NJ, USA; Chicester, UK, 2017; pp. 137–155. ISBN 9781118739013. [Google Scholar]
- Sallis, J.F.; Owen, N. Ecological models of Health Behavior. In Health Behavior: Theory, Research, and Practice, 5th ed.; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: San Francisco, CA, USA, 2015; pp. 43–64. ISBN 9781118629000. [Google Scholar]
- Lawrence, R.J. Human Ecology in the Context of Urbanisation. In Integrating Human Health into Urban and Transport Planning; Nieuwenhuijsen, M., Khreis, H., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 89–109. ISBN 978-3-319-74982-2. [Google Scholar]
- Cummins, S.; Curtis, S.; Diez-Roux, A.V.; Macintyre, S. Understanding and representing ‘place’ in health research: A relational approach. Soc. Sci. Med. (1982) 2007, 65, 1825–1838. [Google Scholar] [CrossRef] [PubMed]
- Rydin, Y.; Bleahu, A.; Davies, M.; Dávila, J.D.; Friel, S.; de Grandis, G.; Groce, N.; Hallal, P.C.; Hamilton, I.; Howden-Chapman, P.; et al. Shaping cities for health: Complexity and the planning of urban environments in the 21st century. Lancet 2012, 379, 2079–2108. [Google Scholar] [CrossRef]
- Shanahan, D.F.; Lin, B.B.; Bush, R.; Gaston, K.J.; Dean, J.H.; Barber, E.; Fuller, R.A. Toward improved public health outcomes from urban nature. Am. J. Public Health 2015, 105, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Radtke, M.A.; Augustin, J.; Blome, C.; Reich, K.; Rustenbach, S.J.; Schäfer, I.; Laass, A.; Augustin, M. How do regional factors influence psoriasis patient care in Germany? JDDG J. Der Dtsch. Dermatol. Ges. 2010, 8, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Augustin, J.; Mangiapane, S.; Kern, W.V. A regional analysis of outpatient antibiotic prescribing in Germany in 2010. Eur. J. Public Health 2015, 25, 397–399. [Google Scholar] [CrossRef] [PubMed]
- Pescosolido, B.A.; Kronenfeld, J.J. Health, Illness, and Healing in an Uncertain Era: Challenges from and for Medical Sociology. J. Health Soc. Behav. 1995, 35, 5. [Google Scholar] [CrossRef]
- Weltgesundheitsorganisation (WHO). Verfassung der Weltgesundheitsorganisation. Available online: https://www.admin.ch/opc/de/classified-compilation/19460131/index.html (accessed on 26 March 2019).
- Bundeszentrale für Gesundheitliche Aufklärung (BZgA). Was erhält Menschen gesund? Antonovskys Modell der Salutogenese-Diskussionsstand und Stellenwert. Available online: https://www.bzga.de/botmed_60606000.html (accessed on 26 March 2019).
- Gandek, B.; Sinclair, S.J.; Kosinski, M.; Ware, J.E. Psychometric Evaluation of the SF-36® Health Survey in Medicare Managed Care. Health Care Financ. Rev. 2004, 25, 5–25. [Google Scholar] [PubMed]
- McHorney, C.A. Health status assessment methods for adults: Past accomplishments and future challenges. Annu. Rev. Public Health 1999, 20, 309–335. [Google Scholar] [CrossRef]
- Selim, A.J.; Rogers, W.; Fleishman, J.A.; Qian, S.X.; Fincke, B.G.; Rothendler, J.A.; Kazis, L.E. Updated U.S. population standard for the Veterans RAND 12-item Health Survey (VR-12). Qual. Life Res. An Int. J. Qual. Life Asp. Treat. Care Rehabil. 2009, 18, 43–52. [Google Scholar] [CrossRef]
- DeSalvo, K.B.; Bloser, N.; Reynolds, K.; He, J.; Muntner, P. Mortality prediction with a single general self-rated health question. A meta-analysis. J. Gen. Intern. Med. 2006, 21, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Wang, R.; Zhao, Y.; Ma, X.; Wu, M.; Yan, X.; He, J. The relationship between self-rated health and objective health status: A population-based study. BMC Public Health 2013, 13, 320. [Google Scholar] [CrossRef] [PubMed]
- Van der Linde, R.M.; Mavaddat, N.; Luben, R.; Brayne, C.; Simmons, R.K.; Khaw, K.T.; Kinmonth, A.L. Self-rated health and cardiovascular disease incidence: Results from a longitudinal population-based cohort in Norfolk, UK. PLoS ONE 2013, 8, e65290. [Google Scholar] [CrossRef] [PubMed]
- Szombathely, M.v.; Albrecht, M.; Antanaskovic, D.; Augustin, J.; Augustin, M.; Bechtel, B.; Bürk, T.; Fischereit, J.; Grawe, D.; Hoffmann, P.; et al. A Conceptual Modeling Approach to Health-Related Urban Well-Being. Urban Sci. 2017, 1, 17. [Google Scholar] [CrossRef]
- Kickbusch, I. The move towards a new public health. Promot. Educ. 2007, 14, 9. [Google Scholar] [CrossRef]
- Balestroni, G.; Bertolotti, G. L’EuroQol-5D (EQ-5D): Uno strumento per la misura della qualità della vita. Monaldi Arch. Chest Dis. Card. Ser. 2012, 78, 155–159. [Google Scholar] [CrossRef]
- Hancock, T. The mandala of health: A model of the human ecosystem. Fam. Community Health 1985, 8, 1–10. [Google Scholar] [CrossRef]
- Babisch, W.; Swart, W.; Houthuijs, D.; Selander, J.; Bluhm, G.; Pershagen, G.; Dimakopoulou, K.; Haralabidis, A.S.; Katsouyanni, K.; Davou, E.; et al. Exposure modifiers of the relationships of transportation noise with high blood pressure and noise annoyance. J. Acoust. Soc. Am. 2012, 132, 3788–3808. [Google Scholar] [CrossRef] [PubMed]
- Bodin, T.; Albin, M.; Ardö, J.; Stroh, E.; Ostergren, P.-O.; Björk, J. Road traffic noise and hypertension: Results from a cross-sectional public health survey in southern Sweden. Environ. Health A Glob. Access Sci. Source 2009, 8, 38. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [CrossRef]
- Greenland, S.; Morgenstern, H. Confounding in health research. Annu. Rev. Public Health 2001, 22, 189–212. [Google Scholar] [CrossRef] [PubMed]
- Consonni, D.; Bertazzi, P.A.; Zocchetti, C. Why and how to control for age in occupational epidemiology. Occup. Environ. Med. 1997, 54, 772–776. [Google Scholar] [CrossRef] [PubMed]
- Oßenbrügge, J.; Pohl, T.; Vogelpohl, A. Entgrenzte Zeitregime und wirtschaftsräumliche Konzentrationen. Z. Für Wirtsch. 2009, 53. [Google Scholar] [CrossRef]
- Millennium Ecosystem Assessment. Ecosystems and Human Well-Being. Synthesis; Island Press: Washington, DC, USA, 2005; ISBN 1-59726-040-1. [Google Scholar]
- Jarup, L.; Babisch, W.; Houthuijs, D.; Pershagen, G.; Katsouyanni, K.; Cadum, E.; Dudley, M.-L.; Savigny, P.; Seiffert, I.; Swart, W.; et al. Hypertension and exposure to noise near airports: The HYENA study. Environ. Health Perspect. 2008, 116, 329–333. [Google Scholar] [CrossRef] [PubMed]
- Orru, K.; Orru, H.; Maasikmets, M.; Hendrikson, R.; Ainsaar, M. Well-being and environmental quality: Does pollution affect life satisfaction? Qual. Life Res. An Int. J. Qual. Life Asp. Treat. Care Rehabil. 2016, 25, 699–705. [Google Scholar] [CrossRef]
- Christine, K.; Andreas, M. Human-biometeorological assessment of heat stress reduction by replanning measures in Stuttgart, Germany. Landsc. Urban Plan. 2014, 122, 78–88. [Google Scholar] [CrossRef]
- Bryant, R.L. Political ecology: An emerging research agenda in Third-World studies. Polit. Geogr. 1992, 1, 12–36. [Google Scholar] [CrossRef]
- Thomson, H.; Thomas, S. Developing empirically supported theories of change for housing investment and health. Soc. Sci. Med. 2015, 124, 205–214. [Google Scholar] [CrossRef]
- Krieger, J.; Higgins, D.L. Housing and health: Time again for public health action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef]
- Krieger, N. Theories for social epidemiology in the 21st century: An ecosocial perspective. Int. J. Epidemiol. 2001, 30, 668–677. [Google Scholar] [CrossRef]
- Bourdieu, P. Die Feinen Unterschiede. Kritik Der Gesellschaftlichen Urteilskraft, 5th ed.; Suhrkamp: Frankfurt, Germany, 1992. [Google Scholar]
- Grusky, D.B. Theories of Stratification and Inequality. In The Concise Encyclopedia of Sociology; Ritzer, G., Ryan, J.M., Eds.; Wiley-Blackwell: Chichester, UK, 2011; pp. 622–624. [Google Scholar]
- Minton, J.W.; McCartney, G. Is there a north–south mortality divide in England or is London the outlier? Lancet Public Health 2018, 3, e556–e557. [Google Scholar] [CrossRef]
- Babisch, W.; Wolf, K.; Petz, M.; Heinrich, J.; Cyrys, J.; Peters, A. Associations between traffic noise, particulate air pollution, hypertension, and isolated systolic hypertension in adults: The KORA study. Environ. Health Perspect. 2014, 5, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Babisch, W.; Wölke, G.; Heinrich, J.; Straff, W. Road traffic noise and hypertension-accounting for the location of rooms. Environ. Res. 2014, 133, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Krefis, A.C.; Albrecht, M.; Kis, A.; Langenbruch, A.; Augustin, M.; Augustin, J.; Maniglio, R. Multivariate Analysis of Noise, Socioeconomic and Sociodemographic Factors and Their Association with Depression on Borough Level in the City State of Hamburg, Germany. JDT 2017, 1, 1–14. [Google Scholar] [CrossRef][Green Version]
- Duhme, H.; Weiland, S.K.; Keil, U.; Kraemer, B.; Schmid, M.; Stender, M.; Chambless, L. The association between self-reported symptoms of asthma and allergic rhinitis and self-reported traffic density on street of residence in adolescents. Epidemiology 1996, 6, 578–582. [Google Scholar] [CrossRef]
- Ising, H.; Lange-Asschenfeldt, H.; Lieber, G.F.; Weinhold, H.; Eilts, M. Respiratory and dermatological diseases in children with long-term exposure to road traffic immissions. Noise Health 2003, 19, 41–50. [Google Scholar]
- Hiramatsu, K.; Yamamoto, T.; Taira, K.; Ito, A.; Nakasone, T. A survey on health effects due to aircraft noise on residents living around kadena air base in the ryukyus. J. Sound Vib. 1997, 4, 451–460. [Google Scholar] [CrossRef]
- Yoshida, T.; Osada, Y.; Kawaguchi, T.; Hoshiyama, Y.; Yoshida, K.; Yamamoto, K. Effects of road traffic noise on inhabitants of tokyo. J. Sound Vib. 1997, 4, 517–522. [Google Scholar] [CrossRef]
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 9341, 1233–1242. [Google Scholar] [CrossRef]
- Gehring, U.; Heinrich, J.; Krämer, U.; Grote, V.; Hochadel, M.; Sugiri, D.; Kraft, M.; Rauchfuss, K.; Eberwein, H.G.; Wichmann, H.-E. Long-term exposure to ambient air pollution and cardiopulmonary mortality in women. Epidemiology 2006, 5, 545–551. [Google Scholar] [CrossRef]
- Naess, O.; Nafstad, P.; Aamodt, G.; Claussen, B.; Rosland, P. Relation between concentration of air pollution and cause-specific mortality: Four-year exposures to nitrogen dioxide and particulate matter pollutants in 470 neighborhoods in Oslo, Norway. Am. J. Epidemiol. 2007, 4, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A.; Burnett, R.T.; Thurston, G.D.; Thun, M.J.; Calle, E.E.; Krewski, D.; Godleski, J.J. Cardiovascular mortality and long-term exposure to particulate air pollution: Epidemiological evidence of general pathophysiological pathways of disease. Circulation 2004, 1, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.-H.; Kim, H.; Kim, J.H.; Bae, S.; Park, H.Y.; Hong, Y.-C. Air pollution and symptoms of depression in elderly adults. Environ. Health Perspect. 2012, 120, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Tzivian, L.; Winkler, A.; Dlugaj, M.; Schikowski, T.; Vossoughi, M.; Fuks, K.; Hoffmann, B. Effect of long-term outdoor air pollution and noise on cognitive and psychological functions in adults. Int. J. Hyg. Environ. Health 2015, 218, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Taylor, W.C.; Floyd, M.F.; Whitt-Glover, M.C.; Brooks, J. Environmental justice: A framework for collaboration between the public health and parks and recreation fields to study disparities in physical activity. J. Phys. Act. Health 2007, 4, S50–S63. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Leonhart, R.; Schaefert, R.; Zhao, X.; Zhang, L.; Wei, J.; Yang, J.; Wirsching, M.; Larisch, A.; Fritzsche, K. Sense of coherence contributes to physical and mental health in general hospital patients in China. Psychol. Health Med. 2015, 20, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Flensborg-Madsen, T.; Ventegodt, S.; Merrick, J. Sense of coherence and physical health. A review of previous findings. Sci. World J. 2005, 5, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Fischereit, J.; Schlünzen, K.H. Evaluation of thermal indices for their applicability in obstacle-resolving meteorology models. Int. J. Biometeorol. 2018, 62, 1887–1900. [Google Scholar] [CrossRef]
- Błażejczyk, K.; Epstein, Y.; Jendritzky, G.; Staiger, H.; Tinz, B. Comparison of UTCI to selected thermal indices. Int. J. Biometeorol. 2012, 3, 515–535. [Google Scholar] [CrossRef]
- De Freitas, C.R.; Grigorieva, E.A. A comprehensive catalogue and classification of human thermal climate indices. Int. J. Biometeorol. 2015, 1, 109–120. [Google Scholar] [CrossRef]
- McMichael, A.J.; Wilkinson, P.; Kovats, R.S.; Pattenden, S.; Hajat, S.; Armstrong, B.; Vajanapoom, N.; Niciu, E.M.; Mahomed, H.; Kingkeow, C.; et al. International study of temperature, heat and urban mortality: The ‘ISOTHURM’ project. Int. J. Epidemiol. 2008, 5, 1121–1131. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Xiao, Y.; Li, G.; Zeng, W.; Lin, H.; Rutherford, S.; Xu, Y.; Luo, Y.; Xu, X.; Chu, C.; et al. Temperature-mortality relationship in four subtropical Chinese cities: A time-series study using a distributed lag non-linear model. Sci. Total Environ. 2013, 449, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Wolff, R.; Yu, W.; Vaneckova, P.; Pan, X.; Tong, S. Ambient temperature and morbidity: A review of epidemiological evidence. Environ. Health Perspect. 2012, 1, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Foster, H.M.E.; Celis-Morales, C.A.; Nicholl, B.I.; Petermann-Rocha, F.; Pell, J.P.; Gill, J.M.R.; O’Donnell, C.A.; Mair, F.S. The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: A prospective analysis of the UK Biobank cohort. Lancet Public Health 2018, 3, e576–e585. [Google Scholar] [CrossRef]
- Gusmano, M.K.; Weisz, D.; Rodwin, V.G.; Lang, J.; Qian, M.; Bocquier, A.; Moysan, V.; Verger, P. Disparities in access to health care in three French regions. Health Policy 2014, 1, 31–40. [Google Scholar] [CrossRef]
- Sørgaard, K.W.; Sandlund, M.; Heikkilä, J.; Hansson, L.; Vinding, H.R.; Bjarnason, O.; Bengtsson-Tops, A.; Merinder, L.; Nilsson, L.-L.; Middelboe, T. Schizophrenia and contact with health and social services: A Nordic multi-centre study. Nord. J. Psychiatry 2003, 57, 253–261. [Google Scholar] [CrossRef]
- Kehler, D.S. Age-related disease burden as a measure of population ageing. Lancet Public Health 2019, 4, e123–e124. [Google Scholar] [CrossRef]
- Szombathely, M.v.; Albrecht, M.; Augustin, J.; Bechtel, B.; Dwinger, I.; Gaffron, P.; Krefis, A.; Oßenbrügge, J.; Strüver, A. Relation between Observed and Perceived Traffic Noise and Socio-Economic Status in Urban Blocks of Different Characteristics. Urban Sci. 2018, 2, 20. [Google Scholar] [CrossRef]
- League of American Bicyclists. Bicycle Account Guidelines; League of American Bicyclists: Newport, RI, USA, 2013; Available online: http://bikeleague.org/ (accessed on 26 March 2019).
- New South Wales Government. Adult Population Health Survey Forthcoming. Available online: http://www.health.nsw.gov.au/surveys/adult/Pages/default.aspx (accessed on 26 March 2019).
- Universitätsklinikum Hamburg-Eppendorf. Hamburg City Health Study. Available online: http://hchs.hamburg (accessed on 26 March 2019).
- Schuster, C.; Honold, J.; Lauf, S.; Lakes, T. Urban heat stress: Novel survey suggests health and fitness as future avenue for research and adaptation strategies. Environ. Res. Lett. 2017, 12, 44021. [Google Scholar] [CrossRef]
- Freie und Hansestadt Hamburg. Sozialmonitoring Integrierte Stadtentwicklung. Bericht 2018. Available online: https://www.hamburg.de/contentblob/11944782/7c72f0a6e51fe0159cdbc24cc3e58283/data/d-sozialmonitoring-bericht-2018.pdf (accessed on 26 March 2019).
- Freie und Hansestadt Hamburg. Strategische Lärmkarte Straßenverkehr Lden. Available online: http://www.hamburg.de/contentblob/3476512/data/lden-strasse-2012.pdf (accessed on 26 March 2019).
- Bechtel, B.; Schmidt, K. Floristic mapping data as a proxy for the mean Urban heat Island. Clim. Res. 2011, 49, 45–58. [Google Scholar] [CrossRef]
- Stewart, I.D.; Oke, T.R. Local Climate Zones for Urban Temperature Studies. Bull. Amer. Meteor. Soc. 2012, 93, 1879–1900. [Google Scholar] [CrossRef]
- Kaveckis, G. Modeling Future Populations Vulnerability to Heat Waves in Greater Hamburg. Ph.D. Thesis, Universität Hamburg, Hamburg, Germany, 2017. [Google Scholar]
- Feng, Y.; Parkin, D.; Devlin, N.J. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual. Life Res. An Int. J. Qual. Life Asp. Treat. Care Rehabil. 2014, 23, 977–989. [Google Scholar] [CrossRef] [PubMed]
- EuroQol Research Foundation. EUROQOL|About Us. Available online: https://euroqol.org/euroqol/ (accessed on 26 March 2019).
- EuroQol Research Foundation. EQ-5D-5L|About. Available online: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/ (accessed on 26 March 2019).
- MacCallum, R.C.; Widaman, K.F.; Zhang, S.; Hong, S. Sample size in factor analysis. Psychol. Methods 1999, 4, 84–99. [Google Scholar] [CrossRef]
- Little, T.D. The Oxford Handbook of Quantitative Methods in Psychology; Oxford University Press: Oxford, UK, 2013; ISBN 9780199934898. [Google Scholar]
- Huber, P.J. Robust Statistics; John Wiley & Sons: New York, NY, USA, 1981; ISBN 0-47141805-6. [Google Scholar]
- Velleman, P.F.; Welsch, R.E. Efficient Computing of Regression Diagnostics. Am. Stat. 1981, 35, 234. [Google Scholar] [CrossRef]
- Whynes, D.K. Correspondence between EQ-5D health state classifications and EQ VAS scores. Health Qual. Life Outcome 2008, 6, 94. [Google Scholar] [CrossRef] [PubMed]
- EuroQol Research Foundation. EQ-5D-5L|Valuation|Crosswalk Index Value Calculator. Available online: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/valuation/crosswalk-index-value-calculator/ (accessed on 18 July 2018).
- Lee, H.-L.; Huang, H.-C.; Lee, M.-D.; Chen, J.H.; Lin, K.-C. Factors affecting trajectory patterns of self-rated health (SRH) in an older population—A community-based longitudinal study. Arch. Gerontol. Geriatr. 2012, 54, e334–e341. [Google Scholar] [CrossRef] [PubMed]
- Maniecka-Bryła, I.; Gajewska, O.; Burzyńska, M.; Bryła, M. Factors associated with self-rated health (SRH) of a University of the Third Age (U3A) class participants. Arch. Gerontol. Geriatr. 2013, 57, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Hertzman, C.; Power, C.; Matthews, S.; Manor, O. Using an interactive framework of society and lifecourse to explain self-rated health in early adulthood. Soc. Sci. Med. 2001, 53, 1575–1585. [Google Scholar] [CrossRef]
- Ma, J.; Mitchell, G.; Dong, G.; Zhang, W. Inequality in Beijing: A Spatial Multilevel Analysis of Perceived Environmental Hazard and Self-Rated Health. Ann. Am. Assoc. Geogr. 2017, 107, 109–129. [Google Scholar] [CrossRef]
- Kardan, O.; Gozdyra, P.; Misic, B.; Moola, F.; Palmer, L.J.; Paus, T.; Berman, M.G. Neighborhood greenspace and health in a large urban center. Sci. Rep. 2015, 5, 11610. [Google Scholar] [CrossRef]
- Pietilä, M.; Neuvonen, M.; Borodulin, K.; Korpela, K.; Sievänen, T.; Tyrväinen, L. Relationships between exposure to urban green spaces, physical activity and self-rated health. J. Outdoor Recreat. Tour. 2015, 10, 44–54. [Google Scholar] [CrossRef]
- Braubach, M. Preventive Application. In Therapeutic Landscapes; Williams, A., Ed.; Ashgate: Aldershot, UK; Burlington, VT, USA, 2007; pp. 111–132. ISBN 9780754670995. [Google Scholar]
- Mayer, F.S.; Frantz, C.M. The connectedness to nature scale: A measure of individuals’ feeling in community with nature. J. Environ. Psychol. 2004, 24, 503–515. [Google Scholar] [CrossRef]
- Völzke, H.; Neuhauser, H.; Moebus, S.; Baumert, J.; Berger, K.; Stang, A.; Ellert, U.; Werner, A.; Döring, A. Rauchen: Regionale Unterschiede in Deutschland. Dtsch. Arztebl. 2006, 42, 2784–2790. [Google Scholar]
- Bundesinstitut Für Bau-, Stadt- und Raumforschung. Deutschland Altert Unterschiedlich. Available online: https://www.bbsr.bund.de/BBSR/DE/Home/Topthemen/alterung_bevoelkerung.html (accessed on 26 March 2019).
- Gatzweiler, H.-P.; Milbert, A. Regionale Einkommensunterschiede in Deutschland. Inf. Zur Raumentwickl. 2003, 4, 125–146. [Google Scholar]
- Grant, K.E.; O’koon, J.H.; Davis, T.H.; Roache, N.A.; Poindexter, L.M.; Armstrong, M.L.; Minden, J.A.; McIntosh, J.M. Protective Factors Affecting Low-Income Urban African American Youth Exposed to Stress. J. Early Adolesc. 2000, 20, 388–417. [Google Scholar] [CrossRef]
- Baum, F. ‘Opportunity structures’: Urban landscape, social capital and health promotion in Australia. Health Promot. Int. 2002, 17, 351–361. [Google Scholar] [CrossRef] [PubMed]
- House, J.; Landis, K.; Umberson, D. Social relationships and health. Science 1988, 241, 540–545. [Google Scholar] [CrossRef]
- Needham, D.M.; Foster, S.D.; Tomlinson, G.; Godfrey-Faussett, P. Socio-economic, gender and health services factors affecting diagnostic delay for tuberculosis patients in urban Zambia. Trop. Med. Int. Health 2001, 6, 256–259. [Google Scholar] [CrossRef]
- McGregor, G. Human biometeorology. Prog. Phys. Geogr. 2011, 36, 93–109. [Google Scholar] [CrossRef]
- Habibi, P.; Momeni, R.; Dehghan, H. The Effect of Body Weight on Heat Strain Indices in Hot and Dry Climatic Conditions. Jundishapur J. Health Sci. 2016, 8. [Google Scholar] [CrossRef]
- Tuomaala, P.; Holopainen, R.; Piira, K.; Airaksinen, M. Impact of individual characteristics such as age, gender, BMI and fitness on human thermal sensation. In Proceedings of the 13th International Building Performance Simulation Association Conference, Chambéry, France, 25–28 August 2013; pp. 2305–2311. [Google Scholar]
- Baker, E.L.; Potter, M.A.; Jones, D.L.; Mercer, S.L.; Cioffi, J.P.; Green, L.W.; Halverson, P.K.; Lichtveld, M.Y.; Fleming, D.W. The public health infrastructure and our nation’s health. Annu. Rev. Public Health 2005, 26, 303–318. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.E.; Hackett, R.A.; Steptoe, A. Associations between age discrimination and health and wellbeing: Cross-sectional and prospective analysis of the English Longitudinal Study of Ageing. Lancet Public Health 2019, 4, e200–e208. [Google Scholar] [CrossRef]
- Universitätsklinikum Hamburg-Eppendorf. Die HCHS—Hintergründe. Available online: http://hchs.hamburg/wp-content/uploads/2017/03/HCHS_Hintergrundinfo.pdf (accessed on 26 March 2019).
- Gehl, J. Cities for People; Island Press: Washington, DC, USA, 2010; ISBN 978-1597265737. [Google Scholar]
- Dapp, U.; Minder, C.E.; Anders, J.; Golgert, S.; von Renteln-Kruse, W. Long-term prediction of changes in health status, frailty, nursing care and mortality in community-dwelling senior citizens—Results from the longitudinal urban cohort ageing study (LUCAS). BMC Geriatr. 2014, 14, 141. [Google Scholar] [CrossRef] [PubMed]
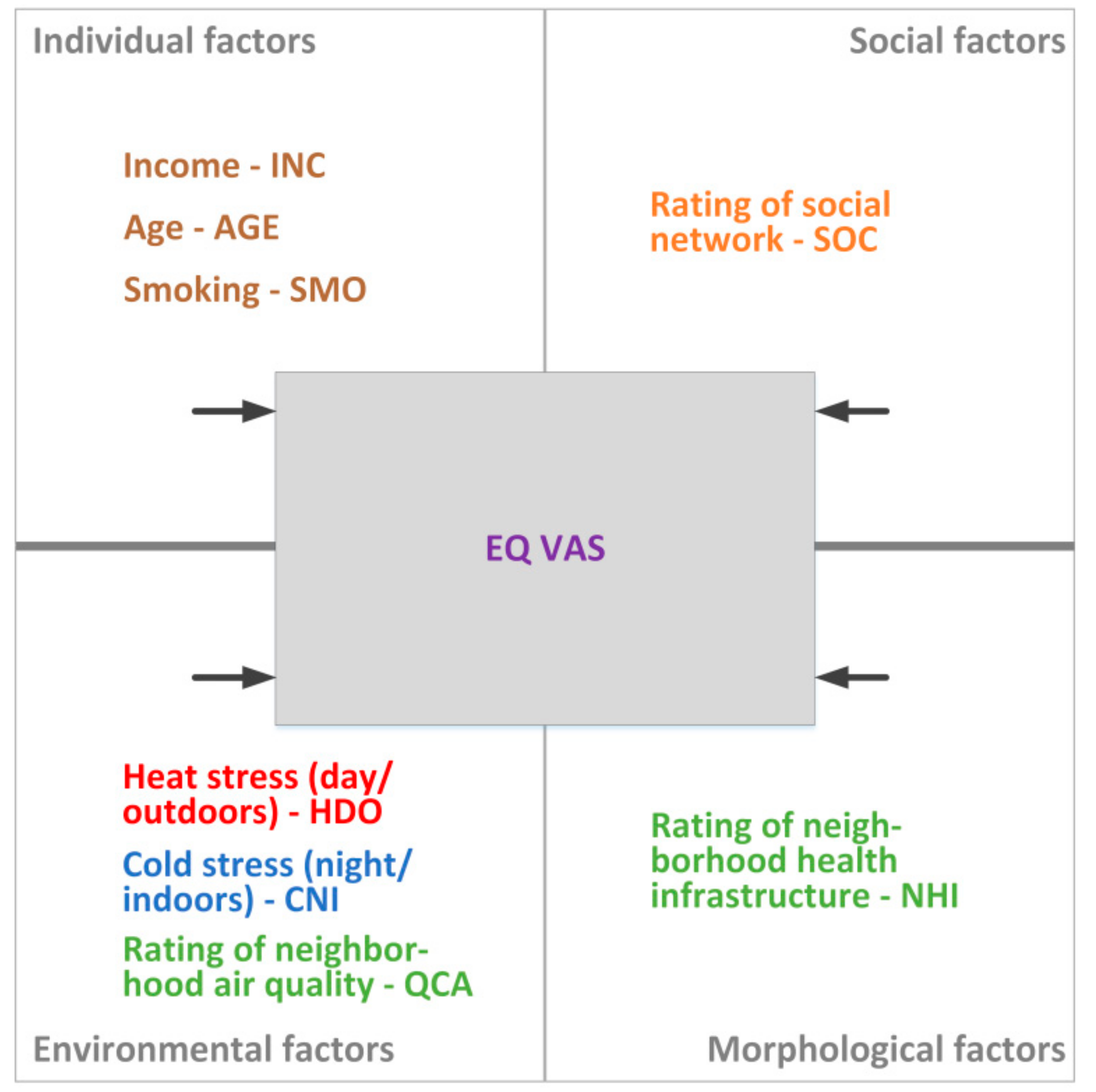
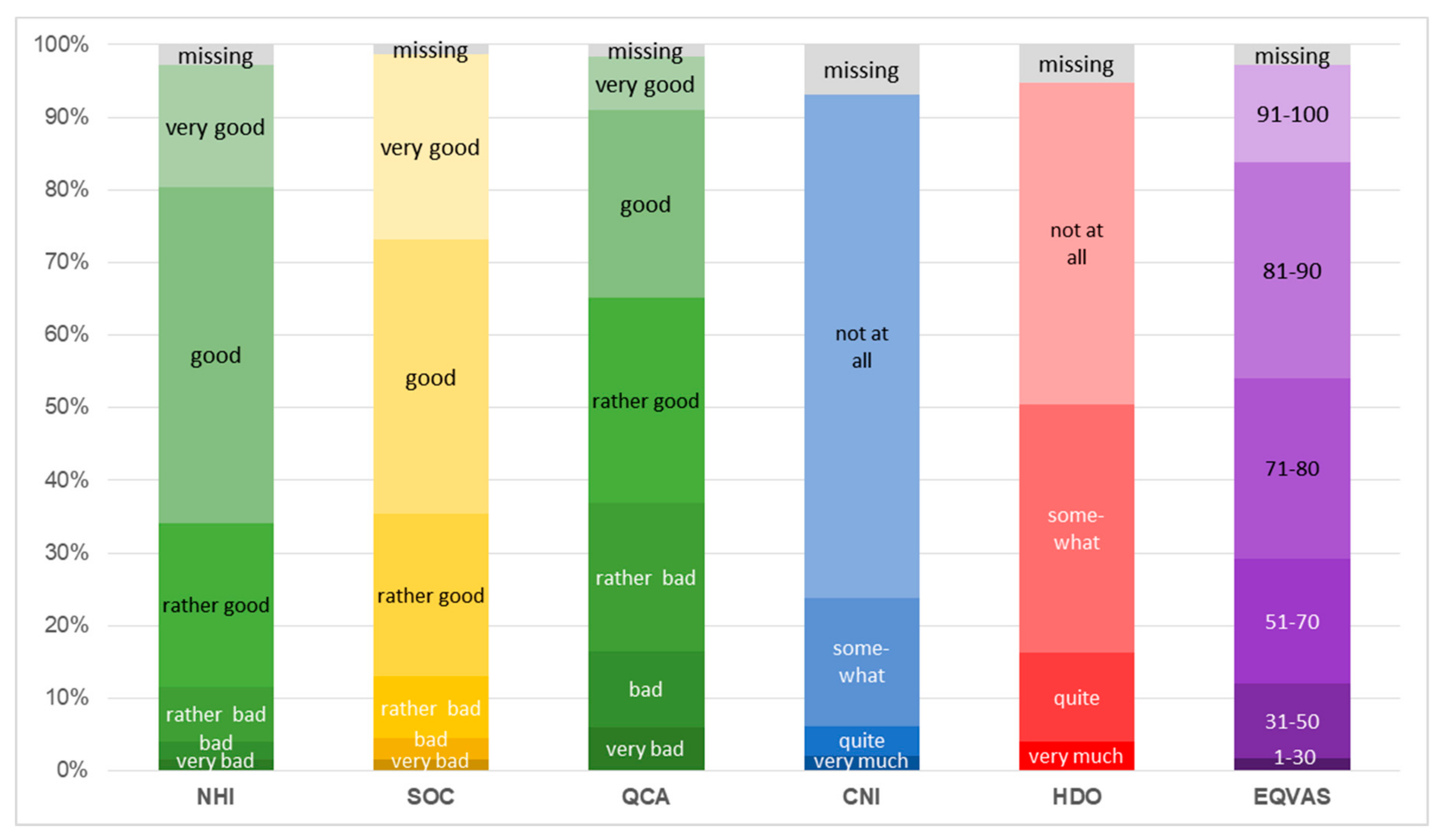
| No. | Question | Variable | n | Scale Type | Mean | Min | Max | SD |
|---|---|---|---|---|---|---|---|---|
| 1. | EQ: Pain, discomfort | EQPD | 1060 | 1 | 1.76 | 5 | 1 | 0.82 |
| 2. | Physical health in general | PHG | 1072 | 2 | 2.61 | 6 | 1 | 1.12 |
| 3. | EQ VAS: Health today | EQVAS | 1051 | 3 | 76.06 | 0 | 100 | 18.21 |
| 4. | EQ: Usual activities | EQDA | 1061 | 1 | 1.28 | 5 | 1 | 0.70 |
| 5. | EQ: Physical mobility | EQPM | 1063 | 1 | 1.35 | 5 | 1 | 0.77 |
| 6. | EQ: Anxiety, depression | EQAD | 1050 | 1 | 1.43 | 5 | 1 | 0.71 |
| 7. | EQ: Self-care | EQSC | 1059 | 1 | 1.08 | 5 | 1 | 0.42 |
| 8. | Green spaces neighborhood: Security | GNS | 1049 | 4 | 2.69 | 6 | 1 | 1.05 |
| 9. | Green spaces neighborhood: General amenity value | GNAV | 1053 | 4 | 2.49 | 6 | 1 | 1.04 |
| 10. | Green spaces neighborhood: Cleanliness | GNC | 1068 | 4 | 2.77 | 6 | 1 | 1.14 |
| 11. | Quality criterion: Cleanliness | QCCL | 1077 | 4 | 3.02 | 6 | 1 | 1.23 |
| 12. | Safety Neighborhood | SNE | 1069 | 4 | 2.42 | 6 | 1 | 1.05 |
| 13. | Neighborhood: General Assessment | NGA | 1053 | 4 | 2.23 | 6 | 1 | 0.95 |
| 14. | Quality criterion: Leisure areas and public places | QCL | 1065 | 4 | 2.65 | 6 | 1 | 1.15 |
| 15. | Quality criterion: Seating accommodation | QCSA | 1056 | 4 | 3.37 | 6 | 1 | 1.23 |
| 16. | Quality criterion: Rating of neighborhood air quality | QCA | 1063 | 4 | 3.19 | 6 | 1 | 1.31 |
| 17. | Green spaces neighborhood: Reachability | GNR | 1063 | 4 | 2.10 | 6 | 1 | 0.97 |
| 18. | Quality criterion: Pedestrian paths | QCP | 1067 | 4 | 2.63 | 6 | 1 | 1.15 |
| 19. | Rating of neighborhood health infrastructure | NHI | 1050 | 2 | 2.36 | 6 | 1 | 1.04 |
| 20. | Quality criterion: Cycle lanes | QCC | 1029 | 4 | 3.18 | 6 | 1 | 1.31 |
| 21. | Quality criterion: Public transport | QCPT | 1077 | 4 | 1.60 | 6 | 1 | 0.86 |
| 22. | Quality criterion: Shopping | QCS | 1078 | 4 | 1.95 | 6 | 1 | 1.13 |
| 23. | Do you feel disturbed by noise at home?…on weekdays | NWD | 1060 | 5 | 2.98 | 1 | 4 | 0.99 |
| 24. | …on weekends | NWE | 1043 | 5 | 3.07 | 1 | 4 | 0.92 |
| 25. | …during night | NNI | 1045 | 5 | 3.22 | 1 | 4 | 0.93 |
| 26. | To what extent do you feel disturbed in your apartment/house by road traffic noise? | NRT | 1024 | 5 | 2.72 | 1 | 4 | 1.09 |
| 27. | Heat stress (day/inside) | HDI | 1048 | 5 | 3.36 | 1 | 4 | 0.83 |
| 28. | Heat stress (night/indoors) | HNI | 1011 | 5 | 3.34 | 1 | 4 | 0.85 |
| 29. | Heat stress (day/outdoors) | HDO | 1025 | 5 | 3.24 | 1 | 4 | 0.85 |
| 30. | Cold stress (day/indoors) | CDI | 1043 | 5 | 3.54 | 1 | 4 | 0.74 |
| 31. | Cold stress (night/indoors) | CNI | 1006 | 5 | 3.66 | 1 | 4 | 0.67 |
| 32. | Cold stress (day/outdoors) | CDO | 1028 | 5 | 3.10 | 1 | 4 | 0.84 |
| 33. | Communication neighborhood | CON | 1068 | 6 | 2.36 | 6 | 1 | 1.41 |
| 34. | Rating of one’s social network | SOC | 1067 | 4 | 2.29 | 6 | 1 | 1.12 |
| 35. | Gender | GEN | 1073 | 7 | - | - | - | - |
| 36. | Daily fruit consumption | DFC | 1047 | 8 | 1.85 | 0 | 7.5 | 1.03 |
| 37. | Frequency of alcohol consumption | FAC | 1052 | 6 | 3.15 | 1 | 6 | 1.35 |
| 38. | Smoking | SMO | 1044 | 5 | 2.73 | 1 | 4 | 1.14 |
| 39. | Highest level of education reached | EDU | 1056 | 9 | 6.31 | 1 | 9 | 2.61 |
| 40. | Approximate monthly net income of household | INC | 953 | 10 | 5.74 | 1 | 11 | 2.73 |
| 41. | Age | AGE | 1048 | 8 | 51.86 | 18 | 95 | 18.69 |
| Factor | Name | No. | Code | Component | Communality | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||||
| 2 | Urban Health | 1. | EQPD | 0.091 | 0.761 | –0.033 | –0.032 | 0.009 | 0.014 | 0.023 | –0.015 | 0.051 | 0.593 |
| 2. | PHG | 0.150 | 0.759 | –0.064 | –0.126 | 0.038 | –0.022 | –0.021 | 0.062 | –0.173 | 0.655 | ||
| 3. | EQVAS | 0.099 | 0.755 | –0.035 | –0.082 | –0.025 | 0.–026 | –0.089 | 0.150 | 0.023 | 0.620 | ||
| 4. | EQDA | –0.008 | 0.689 | –0.033 | –0.093 | –0.169 | 0.141 | 0.067 | –0.063 | 0.207 | 0.584 | ||
| 5. | EQPM | 0.027 | 0.687 | 0.006 | 0.067 | –0.103 | 0.134 | –0.041 | –0.019 | 0.307 | 0.602 | ||
| 6. | EQAD | 0.083 | 0.493 | –0.071 | –0.177 | –0.142 | –0.091 | 0.214 | 0.120 | –0.297 | 0.463 | ||
| 7. | EQSC | –0.073 | 0.453 | –0.049 | –0.035 | –0.251 | 0.179 | –0.013 | –0.176 | 0.312 | 0.438 | ||
| 1 | Security, environmental qualities and infrastructure | 8. | GNS | 0.817 | 0.040 | 0.048 | –0.037 | –0.106 | –0.068 | –0.090 | 0.083 | 0.013 | 0.704 |
| 9. | GNAV | 0.809 | –0.026 | –0.041 | –0.009 | –0.106 | 0.086 | 0.038 | 0.178 | 0.007 | 0.708 | ||
| 10. | GNC | 0.761 | –0.028 | –0.039 | –0.063 | –0.028 | –0.094 | –0.056 | –0.105 | –0.098 | 0.619 | ||
| 11. | QCCL | 0.744 | 0.025 | –0.098 | –0.077 | 0.126 | –0.129 | –0.116 | –0.217 | –0.055 | 0.666 | ||
| 12. | SNE | 0.719 | 0.150 | 0.044 | 0.005 | –0.117 | –0.059 | –0.026 | 0.119 | 0.087 | 0.581 | ||
| 13. | NGA | 0.694 | 0.158 | –0.298 | –0.008 | –0.055 | 0.010 | 0.001 | 0.111 | –0.009 | 0.612 | ||
| 14. | QCL | 0.663 | –0.003 | –0.216 | –0.046 | 0.005 | 0.248 | 0.109 | 0.092 | 0.088 | 0.578 | ||
| 15. | QCSA | 0.615 | 0.027 | –0.132 | –0.076 | –0.006 | 0.281 | 0.155 | –0.085 | 0.104 | 0.523 | ||
| 16. | QCA | 0.602 | 0.092 | –0.474 | 0.029 | 0.057 | –0.061 | 0.057 | –0.125 | –0.119 | 0.637 | ||
| 17. | GNR | 0.596 | –0.030 | –0.047 | 0.036 | –0.135 | 0.277 | 0.106 | 0.211 | 0.106 | 0.521 | ||
| 18. | QCP | 0.514 | 0.016 | –0.167 | –0.042 | 0.191 | 0.280 | –0.144 | –0.279 | 0.210 | 0.552 | ||
| 19. | NHI | 0.420 | 0.337 | 0.047 | –0.072 | –0.037 | 0.348 | 0.079 | 0.169 | –0.237 | 0.510 | ||
| 20. | QCC | 0.370 | –0.026 | –0.248 | –0.075 | 0.228 | 0.302 | –0.011 | –0.346 | 0.052 | 0.470 | ||
| 6 | Urban Services | 21. | QCPT | 0.182 | 0.101 | 0.043 | 0.020 | –0.027 | 0.771 | –0.060 | 0.073 | –0.056 | 0.653 |
| 22. | QCS | 0.226 | 0.143 | 0.054 | –0.010 | 0.031 | 0.747 | –0.104 | 0.032 | –0.064 | 0.649 | ||
| 3 | Noise Stress | 23. | NWD | –0.206 | –0.077 | 0.836 | 0.020 | 0.144 | 0.010 | 0.011 | –0.014 | 0.052 | 0.772 |
| 24. | NWE | –0.236 | –0.075 | 0.810 | 0.086 | 0.158 | –0.012 | 0.015 | –0.069 | 0.024 | 0.755 | ||
| 25. | NNI | –0.249 | –0.033 | 0.756 | 0.056 | 0.155 | 0.015 | –0.002 | –0.022 | 0.100 | 0.672 | ||
| 26. | NRT | –0.173 | –0.004 | 0.809 | 0.069 | 0.031 | 0.040 | –0.094 | –0.023 | –0.031 | 0.702 | ||
| 4 | Heat Stress | 27. | HDI | –0.105 | –0.046 | 0.080 | 0.869 | 0.113 | –0.056 | –0.004 | –0.075 | –0.038 | 0.798 |
| 28. | HNI | –0.115 | –0.112 | 0.153 | 0.828 | 0.102 | 0.007 | –0.004 | –0.105 | –0.044 | 0.758 | ||
| 29. | HDO | –0.099 | –0.253 | –0.003 | 0.743 | 0.018 | 0.030 | 0.043 | 0.006 | 0.013 | 0.629 | ||
| 5 | Cold Stress | 30. | CDI | –0.105 | –0.086 | 0.148 | 0.082 | 0.818 | –0.031 | –0.037 | –0.029 | –0.047 | 0.721 |
| 31. | CNI | –0.158 | –0.095 | 0.174 | 0.014 | 0.809 | 0.014 | 0.017 | –0.044 | –0.007 | 0.721 | ||
| 32. | CDO | –0.042 | –0.190 | 0.111 | 0.129 | 0.601 | 0.029 | 0.015 | 0.118 | 0.034 | 0.445 | ||
| 8 | Social Network | 33. | CON | 0.095 | –0.025 | –0.032 | –0.103 | –0.051 | 0.063 | 0.028 | 0.717 | 0.113 | 0.555 |
| 34. | SOC | 0.123 | 0.190 | –0.098 | –0.080 | 0.172 | 0.074 | –0.102 | 0.656 | –0.042 | 0.544 | ||
| 7 | Gender and Consumption | 35. | GEN | –0.027 | –0.131 | –0.038 | –0.033 | 0.048 | 0.128 | –0.662 | 0.152 | 0.022 | 0.501 |
| 36. | DFC | 0.043 | 0.009 | –0.026 | 0.048 | 0.036 | –0.102 | 0.579 | –0.094 | –0.149 | 0.383 | ||
| 37. | FAC | 0.144 | 0.065 | –0.126 | 0.028 | 0.029 | –0.014 | 0.494 | 0.225 | 0.340 | 0.452 | ||
| 38. | SMO | –0.131 | –0.120 | –0.005 | –0.037 | 0.018 | 0.143 | 0.482 | 0.109 | 0.012 | 0.298 | ||
| 9 | Age and Social Status | 39. | EDU | –0.117 | –0.178 | –0.122 | 0.063 | 0.002 | 0.116 | 0.124 | –0.057 | –0.678 | 0.556 |
| 40. | INC | –0.241 | –0.202 | –0.075 | 0.175 | 0.141 | 0.190 | –0.214 | –0.098 | –0.415 | 0.418 | ||
| 41. | AGE | –0.072 | 0.315 | 0.150 | 0.157 | 0.191 | 0.095 | –0.390 | 0.003 | 0.411 | 0.518 | ||
| Model | Variable | Estimation | Std. Error | t-Stat | p-Value |
|---|---|---|---|---|---|
| 1 | SMO | 1.162 | 0.446 | 2.604 | 0.009 b |
| AGE | –0.237 | 0.028 | –8.505 | 0.000 b | |
| INC | 1.226 | 0.184 | 6.682 | 0.000 b | |
| 2 | SMO | 1.055 | 0.417 | 2.531 | 0.012 c |
| AGE | –0.241 | 0.026 | –9.108 | 0.000 b | |
| INC | 0.831 | 0.175 | 4.744 | 0.000 b | |
| QCA | –0.726 | 0.365 | –1.989 | 0.047 c | |
| SOC | –1.379 | 0.421 | –3.276 | 0.001 b | |
| NHI | –2.488 | 0.479 | –5.194 | 0.000 b | |
| CNI | 2.389 | 0.731 | 3.269 | 0.001 b | |
| HDO | 3.641 | 0.568 | 6.409 | 0.000 b |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
von Szombathely, M.; Bechtel, B.; Lemke, B.; Oßenbrügge, J.; Pohl, T.; Pott, M. Empirical Evidences for Urban Influences on Public Health in Hamburg. Appl. Sci. 2019, 9, 2303. https://doi.org/10.3390/app9112303
von Szombathely M, Bechtel B, Lemke B, Oßenbrügge J, Pohl T, Pott M. Empirical Evidences for Urban Influences on Public Health in Hamburg. Applied Sciences. 2019; 9(11):2303. https://doi.org/10.3390/app9112303
Chicago/Turabian Stylevon Szombathely, Malte, Benjamin Bechtel, Bernd Lemke, Jürgen Oßenbrügge, Thomas Pohl, and Maike Pott. 2019. "Empirical Evidences for Urban Influences on Public Health in Hamburg" Applied Sciences 9, no. 11: 2303. https://doi.org/10.3390/app9112303
APA Stylevon Szombathely, M., Bechtel, B., Lemke, B., Oßenbrügge, J., Pohl, T., & Pott, M. (2019). Empirical Evidences for Urban Influences on Public Health in Hamburg. Applied Sciences, 9(11), 2303. https://doi.org/10.3390/app9112303





