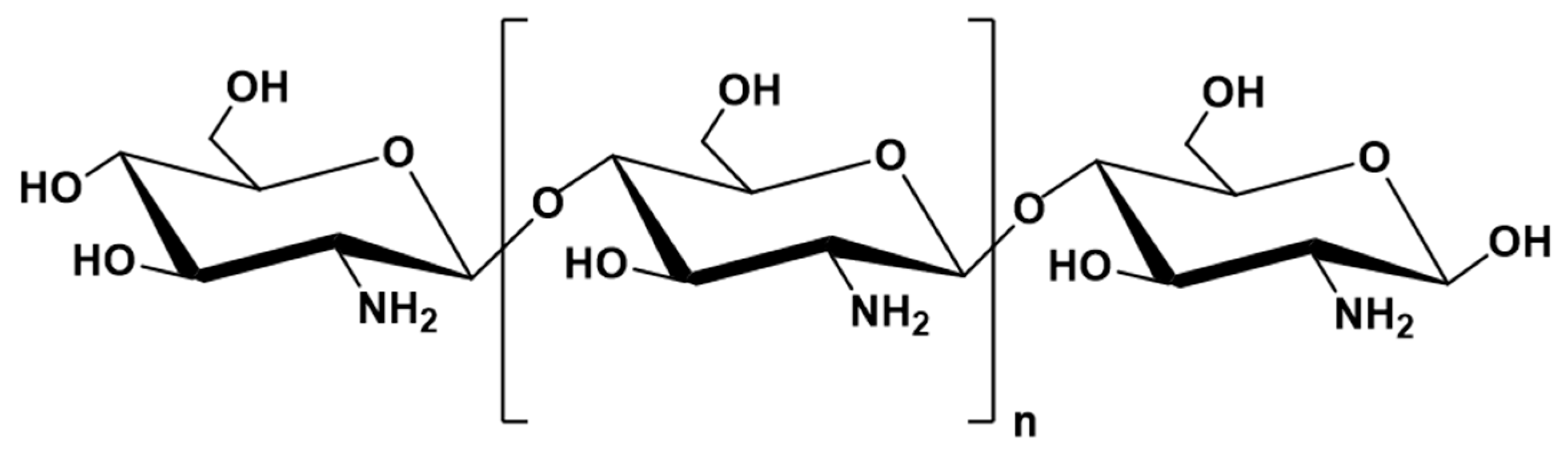
Chitosan as a Natural Copolymer with Unique Properties for the Development of Hydrogels
Abstract
1. Introduction
2. Determination of De-Acetylation of Chitosan
3. The Limitations of Chitosan
4. Chitosan in Nanoscience
5. Nanochitosan Synthesis Approaches
5.1. Ionotropic Gelation
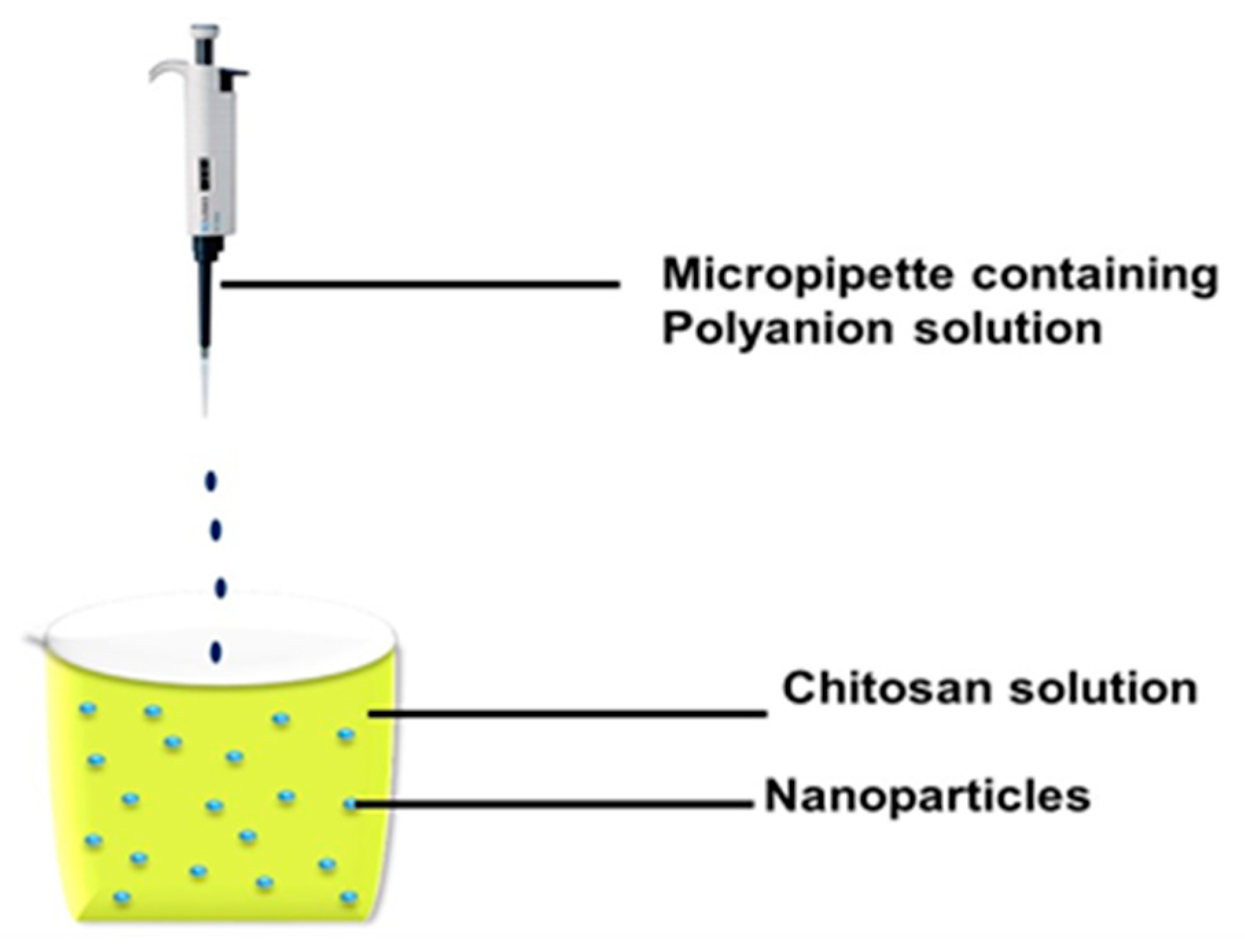
5.2. Ionic Gelation Method
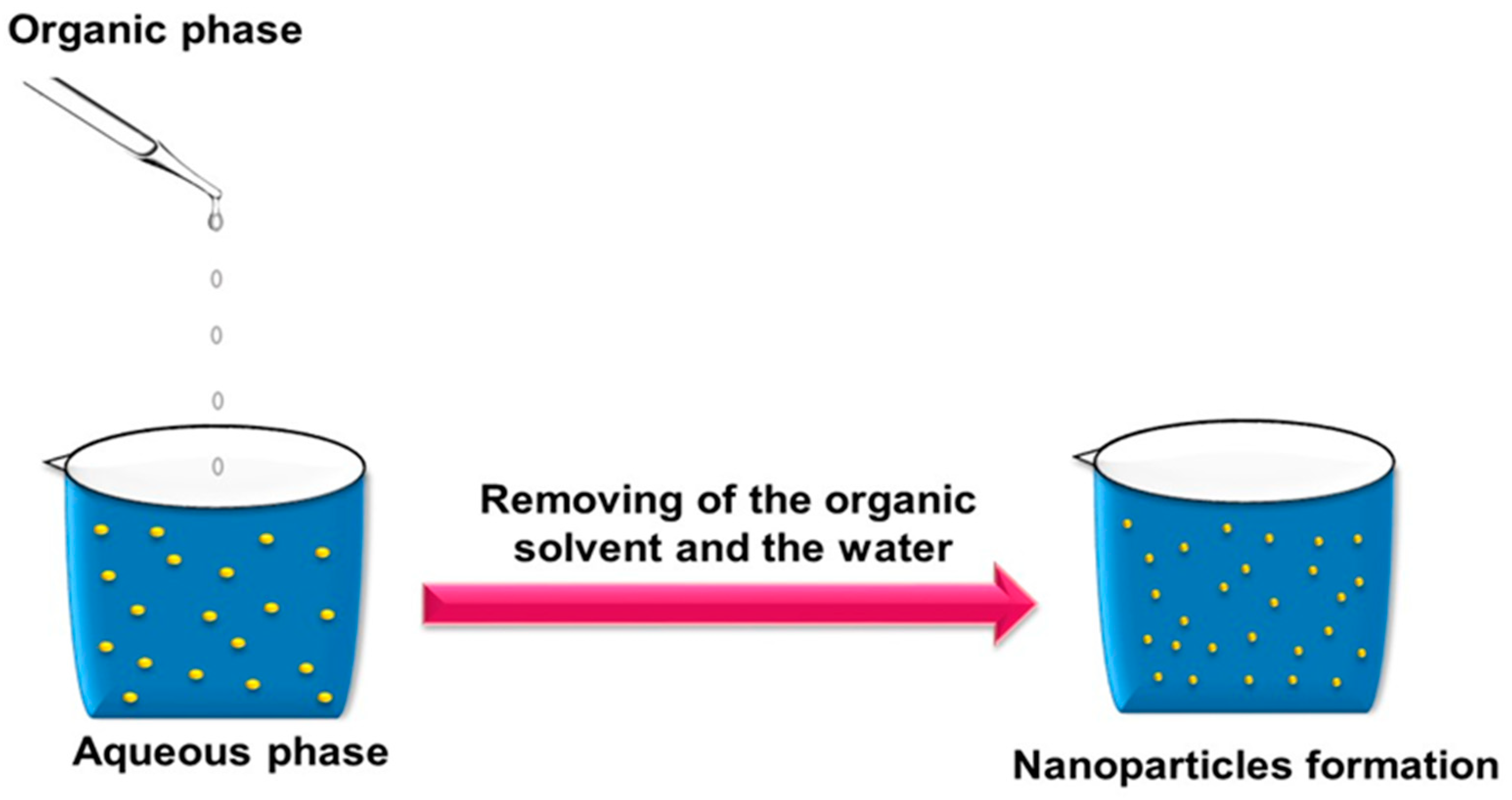
5.3. Emulsification Solvent Diffusion Method
5.4. Spray-Drying
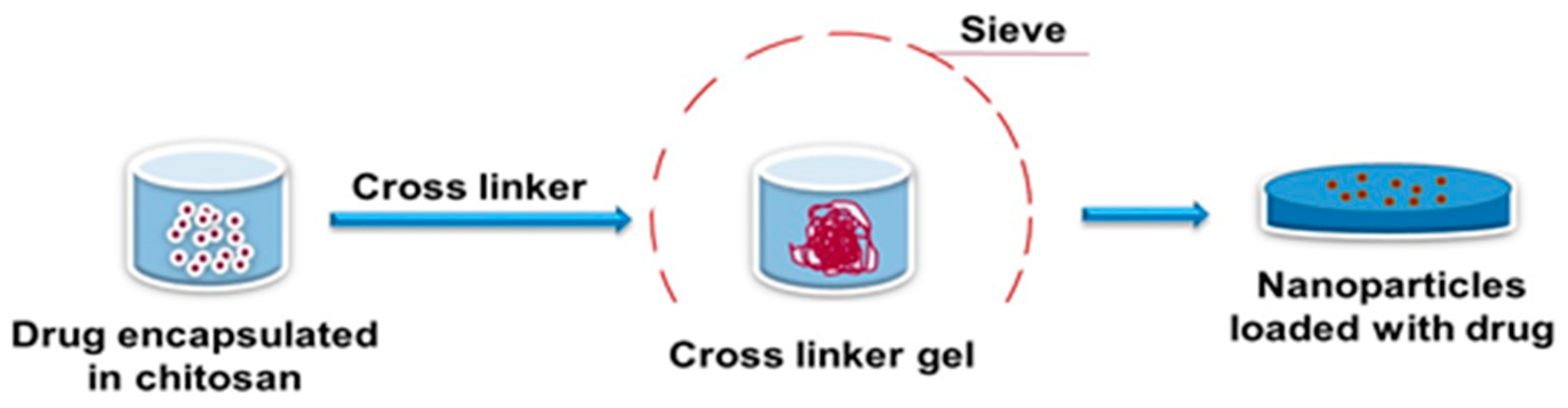
5.5. Sieving Method
5.6. Reverse Micellar Method
5.7. Self-Assembly
6. Hydrogels
6.1. Synthesis of the Hydrogel
6.2. Cross-Linking in Nanoparticles’ Preparation
7. Classification of Cross-Linking Agents
7.1. Physical Cross-Linking
7.2. Chemical Cross-Linking
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Chen, M.C.; Mi, F.L.; Liao, Z.X.; Hsiao, C.W.; Sonaje, K.; Chung, M.F.; Hsu, L.W.; Sung, H.W. Recent advances in chitosan-based nanoparticles for oral delivery of macromolecules. Adv. Drug Deliv. Rev. 2013, 65, 865–879. [Google Scholar] [CrossRef]
- Engkagul, V.; Klaharn, I.Y.; Sereemaspun, A.; Chirachanchai, S. Chitosan whisker grafted with oligo (lactic acid) nanoparticles via a green synthesis pathway: Potential as a transdermal drug delivery system. Nanomedicine 2017, 13, 2523–2531. [Google Scholar] [CrossRef]
- Motiei, M.; Kashanian, S.; Lucia, L.A.; Khazaei, M. Intrinsic parameters for the synthesis and tuned properties of amphiphilic chitosan drug delivery nanocarriers. J. Control. Release 2017, 260, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Shoueir, K.; El-Sheshtawy, H.; Misbah, M.; El-Hosainy, H.; El-Mehasseb, I.; El-Kemary, M. Fenton-like nanocatalyst for photodegradation of methylene blue under visible light activated by hybrid green DNSA@ Chitosan@ MnFe2O4. Carbohydr. Polym. 2018, 197, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Nimesh, S.; Thibault, M.; Lavertu, M.; Buschmann, M. Enhanced Gene Delivery Mediated by Low Molecular Weight Chitosan/DNA Complexes: Effect of pH and Serum. Mol. Biotechnol. 2010, 46, 182–196. [Google Scholar] [CrossRef]
- Rajitha, P.; Gopinath, D.; Biswas, R.; Sabitha, M.; Jayakumar, R. Chitosan nanoparticles in drug therapy of infectious and inflammatory diseases. Expert Opin. Drug Deliv. 2016, 13, 1177–1194. [Google Scholar] [CrossRef]
- Xiao, B.; Chen, Q.; Zhang, Z.; Wang, L.; Denning, T.; Kang, Y.; Merlin, D. TNFalpha gene silencing mediated by orally targeted nanoparticles combined with interleukin-22 for synergistic combination therapy of ulcerative colitis. J. Control. Release 2018, 287, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, M.A.; Syeda, J.T.M.; Wasan, K.M.; Wasan, E.K. An Overview of Chitosan Nanoparticles and Its Application in Non-Parenteral Drug Delivery. Pharmaceutics 2017, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Saravanakumar, G.; Kim, K.; Kwon, I.C. Targeted delivery of low molecular drugs using chitosan and its derivatives. Adv. Drug Deliv. Rev. 2010, 62, 28–41. [Google Scholar] [CrossRef]
- Li, J.; Cai, C.; Li, J.; Li, J.; Li, J.; Sun, T.; Wang, L.; Wu, H.; Yu, G. Chitosan-Based Nanomaterials for Drug Delivery. Molecules 2018, 23, 2661. [Google Scholar] [CrossRef]
- Croisier, F.; Jérôme, C. Chitosan-based biomaterials for tissue engineering. Eur. Polym. J. 2013, 49, 780–792. [Google Scholar] [CrossRef]
- Gonçalves, I.C.; Henriques, P.C.; Seabra, C.L.; Martins, M.C.L. The potential utility of chitosan micro/nanoparticles in the treatment of gastric infection. Expert Rev. Anti. Infect. 2014, 12, 981–992. [Google Scholar] [CrossRef]
- Martins, A.F.; de Oliveira, D.M.; Pereira, A.G.; Rubira, A.F.; Muniz, E.C. Chitosan/TPP microparticles obtained by microemulsion method applied in controlled release of heparin. Int. J. Biol. Macromol. 2012, 51, 1127–1133. [Google Scholar] [CrossRef]
- Hanafy, N.A.; De Giorgi, M.L.; Nobile, C.; Cascione, M.; Rinaldi, R.; Leporatti, S. CaCO3 rods as chitosan polygalacturonic acid carriers for brompyruvic acid delivery. Sci. Adv. Mater. 2016, 8, 514–523. [Google Scholar] [CrossRef]
- Ahsan, S.M.; Thomas, M.; Reddy, K.K.; Sooraparaju, S.G.; Asthana, A.; Bhatnagar, I. Chitosan as biomaterial in drug delivery and tissue engineering. Int. J. Biol. Macromol. 2018, 110, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Dube, A.; Nicolazzo, J.A.; Larson, I. Chitosan nanoparticles enhance the intestinal absorption of the green tea catechins (+)-catechin and (−)-epigallocatechingallate. Eur. J. Pharm. Sci. 2010, 41, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, S.; Buttini, F.; Rossi, A.; Bettini, R.; Colombo, P.; Ponchel, G.; Sonvico, F. Ex vivo permeation of tamoxifen and its 4-OH metabolite through rat intestine from lecithin/chitosan nanoparticles. Int. J. Pharm. 2015, 491, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Miladi, K.; Sfar, S.; Fessi, H.; Elaissari, A. Enhancement of alendronate encapsulation in chitosan nanoparticles. J. Drug Deliv. Sci. Technol. 2015, 30, 391–396. [Google Scholar] [CrossRef]
- Caramella, C.M.; Rossi, S.; Ferrari, F.; Bonferoni, M.C.; Sandri, G. Mucoadhesive and thermogelling systems for vaginal drug delivery. Adv. Drug Deliv. Rev. 2015, 92, 39–52. [Google Scholar] [CrossRef]
- Yang, Y.; Zhu, H.; Wang, J.; Fang, Q.; Peng, Z. Enzymatically Disulfide Crosslinked Chitosan/Hyaluronic Acid Layer-by-Layer Self-Assembled Microcapsules for Redox-Responsive Controlled Release of Protein. ACS Appl. Mater. Interfaces 2018, 10, 33493–33506. [Google Scholar] [CrossRef]
- Chen, W.L.; Li, F.; Tang, Y.; Yang, S.D.; Li, J.Z.; Yuan, Z.Q.; Liu, Y.; Zhou, X.F.; Liu, C.; Zhang, X.N. Stepwise pH-responsive nanoparticles for enhanced cellular uptake and on-demand intracellular release of doxorubicin. Int. J. Nanomed. 2017, 12, 4241–4256. [Google Scholar] [CrossRef]
- De la Fuente, M.; Ravina, M.; Paolicelli, P.; Sanchez, A.; Seijo, B.; Alonso, M.J. Chitosan-based nanostructures: A delivery platform for ocular therapeutics. Adv. Drug Deliv. Rev. 2010, 62, 100–117. [Google Scholar] [CrossRef]
- Woraphatphadung, T.; Sajomsang, W.; Rojanarata, T.; Ngawhirunpat, T.; Tonglairoum, P.; Opanasopit, P. Development of Chitosan-Based pH-Sensitive Polymeric Micelles Containing Curcumin for Colon-Targeted Drug Delivery. AAPS PharmSciTech 2018, 19, 991–1000. [Google Scholar] [CrossRef]
- Wu, J.; Tang, C.; Yin, C. Co-delivery of doxorubicin and interleukin-2 via chitosanbased nanoparticles for enhanced antitumor efficacy. Acta Biomater. 2017, 47, 81–90. [Google Scholar] [CrossRef]
- Shen, J.W.; Li, J.; Zhao, Z.; Zhang, L.; Peng, G.; Liang, L. Molecular dynamics study on the mechanism of polynucleotide encapsulation by chitosan. Sci. Rep. 2017, 7, 5050–5058. [Google Scholar] [CrossRef]
- Calvo, P.; Remunan-Lopez, C. Chitosan and chitosan ethylene oxide propylene oxide block copolymer nanoparticles as novel carriers for proteins and vaccines. Pharm. Res. 2003, 14, 1431–1436. [Google Scholar] [CrossRef]
- Ravi, H.; Baskaran, V. Chitosan Nanoparticles—An Emerging Trend in Nanotechnology. Food Hydrocoll. 2015, 43, 717–725. [Google Scholar] [CrossRef]
- Shen, S.; Li, Y.; Xiao, Y.; Zhao, Z.; Zhang, C.; Wang, J.; Li, H.; Liu, F.; He, N.; Yuan, Y.; et al. Folate-conjugated nanobubbles selectively target and kill cancer cells via ultrasound-triggered intracellular explosion. Biomaterials 2018, 181, 293–306. [Google Scholar] [CrossRef]
- Huang, Y.; Yeh, M.; Chiang, C. Formulation factors in preparing BTM-chitosan microspheres by spray drying method. Int. J. Pharm. 2002, 242, 239–242. [Google Scholar] [CrossRef]
- Agnihotri, S.A.; Aminabhavi, T.M. Controlled release of clozapine through chitosan microparticles prepared by a novel method. J. Control. Release 2004, 96, 245–259. [Google Scholar] [CrossRef]
- Mitra, S.; Gaur, U.; Ghosh, P.C.; Maitra, A.N. Tumour targeted delivery of encapsulated dextran-doxorubicin conjugate using chitosan nanoparticles as carrier. J. Control. Release 2001, 74, 317–323. [Google Scholar] [CrossRef]
- Oh, N.M.; Oh, K.T.; Baik, H.J.; Lee, B.R.; Lee, A.H.; Youn, Y.S.; Lee, E.S. A self-organized 3-diethylaminopropyl-bearing glycol chitosan nanogel for tumor acidic pH targeting: In vitro evaluation. Colloids Surf. B 2010, 78, 120–126. [Google Scholar] [CrossRef]
- Hanafy, N.A.; Dini, L.; Citti, C.; Cannazza, G.; Leporatti, S. Inhibition of Glycolysis by Using a Micro/Nano-Lipid Bromopyruvic Chitosan Carrier as a Promising Tool to Improve Treatment of Hepatocellular Carcinoma. Nanomaterials 2018, 8, 34. [Google Scholar] [CrossRef]
- Pereira, P.; Correia, A.; Gama, F.M. In Vivo Imaging of Glycol Chitosan-Based Nanogel Biodistribution. Macromol. Biosci. 2016, 16, 432–440. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, S.; Xiong, W.; Pei, Y.; Li, B.; Chen, Y. Nanogels fabricated from bovine serum albumin and chitosan via self-assembly for delivery of anticancer drug. Colloids Surf. B 2016, 146, 107–113. [Google Scholar] [CrossRef]
- Hoffman, A.S. Hydrogels for biomedical applications. Adv. Drug Deliv. Rev. 2002, 54, 3–12. [Google Scholar] [CrossRef]
- Hamidi, M.; Azadi, A.; Rafiei, P. Hydrogel nanoparticles in drug delivery, Hydrogel nanoparticles in drug delivery. Adv. Drug Deliv. Rev. 2008, 60, 1638–1649. [Google Scholar] [CrossRef] [PubMed]
- Peppas, N.A.; Hilt, J.Z.; Khademhosseini, A.; Langer, R. Hydrogels in biology and medicine: From molecular principles to bionanotechnology. Adv. Mater. 2006, 18, 1345–1360. [Google Scholar] [CrossRef]
- Peppas, N.A.; Bures, P.; Leobandung, W.; Ichikawa, H. Hydrogels in pharmaceutical formulations. Eur. J. Pharm. Biopharm. 2000, 50, 27–46. [Google Scholar] [CrossRef]
- Khan, F.; Tare, R.S.; Oreffo, R.O.; Bradley, M. Versatile biocompatible polymer hydrogels: Scaffolds for cell growth. Angew. Chem. Int. Ed. Engl. 2009, 48, 978–982. [Google Scholar] [CrossRef]
- Tessmar, J.K.; Gopferich, A.M. Matrices and scaffolds for protein delivery in tissue engineering. Adv. Drug Deliv. Rev. 2007, 59, 274–291. [Google Scholar] [CrossRef]
- Risbud, M.V.; Hardikar, A.A.; Bhat, S.V.; Bhonde, R.R. pH-sensitive freeze-dried chitosan–polyvinyl pyrrolidone hydrogels as controlled release system for antibiotic delivery. J. Control. Release 2000, 68, 23–30. [Google Scholar] [CrossRef]
- Flory, P.J. Principles of Polymer Chemistry; Cornell University Press: New York, NY, USA, 1953. [Google Scholar]
- Lou, X.; Dalton, P.D.; Chirila, T.V. Hydrophilic sponges based on 2-hydroxyethyl methacrylate: Part VII: Modulation of sponge characteristics by changes in reactivity and hydrophilicity of crosslinking agents. J. Mater. Sci. Mater. Med. 2000, 11, 319–325. [Google Scholar] [CrossRef]
- Lin, C.C.; Metters, A.T. Hydrogels in controlled release formulations: Network design and mathematical modeling. Adv. Drug Deliv. Rev. 2006, 58, 1379–1408. [Google Scholar] [CrossRef]
- Denkbas, E.B.; Ottenbrite, R.M. Perspectives on: Chitosan drug delivery systems based on their geometries. J. Bioact. Compat. Polym. 2006, 21, 351–368. [Google Scholar] [CrossRef]
- Muzzarelli, R.A.A.; Muzzarelli, C. Chitosan chemistry: Relevance to the biomedical sciences. In Polysaccharides 1: Structure, Characterization and Use; Springer: Berlin/Heidelberg, Germany, 2005; pp. 151–209. [Google Scholar]
- Crini, G. Recent developments in polysaccharide-based materials used as absorbents in waste water treatment. Prog. Polym. Sci. 2005, 30, 38–70. [Google Scholar] [CrossRef]
- Peniche, H.; Peniche, C. Chitosannanoparticles: A contribution to nanomedicine. Polym. Int. 2011, 60, 883–889. [Google Scholar] [CrossRef]
- Bumgardner, J.D.; Ong, J.L.; Yang, Y. The effect of cross-linking of chitosan microspheres with genipin on protein release. Carbohydr. Poly. 2007, 68, 561–567. [Google Scholar]
- Hanafy, N.A.; Leporatti, S.; El-Kemary, M. Mucoadhesive Hydrogel Nanoparticles as Smart Biomedical Drug Delivery System. Appl. Sci. 2019, 9, 825. [Google Scholar] [CrossRef]
- Shoueir, K.; Kandil, S.; El-hosainy, H.; El-Kemary, M. Tailoring the surface reactivity of plasmonic Au@ TiO2 photocatalyst bio-based chitosan fiber towards cleaner of harmful water pollutants under visible-light irradiation. J. Clean. 2019, 230, 383–393. [Google Scholar] [CrossRef]
- Laroui, H.; Dalmasso, G.; Nguyen, H.T.; Yan, Y.; Sitaraman, S.V.; Merlin, D. Drug-loaded nanoparticles targeted to the colon with polysaccharide hydrogel reduce colitis in a mouse model. Gastroenterology 2010, 138, 843–853. [Google Scholar] [CrossRef]

| Morphology | The Role Chitosan Played | Preparation Method | Application |
|---|---|---|---|
| Nanogels | Chitosan-carbon dot hybrid nanogels | Covalent cross-linking | Photothermal−chemo therapy |
| pH responsive eucalyptus oil coated double walled biodegradable nanogels | Ion cross-linking | Controlled drug delivery | |
| PEGylated and fluorinated chitosan nanogel | Covalent modification | Targeted drug delivery | |
| Reversible swelling-shrinking nanogel | Covalent modification/cross-linking | Character of deep tumor penetration | |
| Micelles | Chitosan-based pH-sensitive polymeric micelles | Covalent modification/self-assembly | Colon-targeted drug delivery |
| pH-responsive aerobic micelles | Ion cross-linking | Photodynamic therapy | |
| Chitosan-pluronic micelles | Covalent modification/self-assembly | Drug delivery for glioblastoma cancer | |
| Multifunctional nanoparticles | Covalent modification/self-assembly | Targeted photothermal therapy | |
| Chitosan grafted methoxy poly(ethylene glycol)-poly(ε-caprolactone) | Covalent modification/self-assembly | Ocular delivery of hydrophobic drug | |
| Nanofibers | Biomimetic mineralization of carboxymethyl chitosan nanofibers | Electrospinning process | Improve osteogenic activity |
| Liposomes | Arginine-modified nanostructured lipid carriers | Covalent modification/self-assembly | Anticancer drug delivery |
| Glycosaminoglycan modified chitosan liposome | Covalent modification | Antimalarial drug delivery | |
| Aptamer-modified liposomal complexes | Covalent modification/other processing | Reverse drug resistance in lung cancer | |
| Gold nanoshell-coated liposomes | Covalent modification/electrostatic adsorption | Photothermal and chemotherapy | |
| Glycol chitosan-coated liposomes | Covalent modification/self-assembly | pH-responsive drug-delivery | |
| Nanosphere | Magnetic nanoparticle-loaded chitosan-deoxycholic acid nanodroplets | Covalent modification, self-assembly | siRNA Delivery |
| Smart pH-responsive nanocarrier | Covalent modification/electrostatic adsorption | Targeted delivery of ursolic acid | |
| Thermoresponsivenanospheres | Covalent modification/emulsification/solvent evaporation method | Release drug for the treatment of osteoarthritis | |
| Nano-particles | Uniform core-shell nanoparticles | Ion crosslinking | Enhance oral delivery of insulin |
| N-trimethyl chitosan nanoparticles | Covalent modification/self-assembly | Oral delivery to treat breast cancer | |
| Chitosan-modified PLGA nanoparticles | Ion crosslinking | Tumor-targeted drug delivery | |
| EGFR-targeted chitosan nanoparticles | Covalent modification/self-assembly | SiRNA delivery | |
| Indomethacin-conjugated chitosan oligosaccharide nanoparticle | Covalent modification/self-assembly | Prodrug and tumor-targeted drug delivery | |
| Inorganic nano-materials | Viable smart targeted nanoenvelope delivery system | Covalent modification/self-assembly | Dox encapsulated and targeted therapy |
| Multifunctional magnetic nanoparticles | Covalent modification/ sonication treatment | Thermo-Chemotherapy Intracellular Imaging | |
| Combinatorial nanocarrier | Covalent modification/ion crosslinking | Drug delivery for breast cancer | |
| Magnetic thymine-imprinted chitosan nanoparticles | Physical adsorption | Gene therapy | |
| Functional hollow microspheres constructed from MOF shells | Covalent modification/Physical adsorption | Drug delivery and targeted transport |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sami El-banna, F.; Mahfouz, M.E.; Leporatti, S.; El-Kemary, M.; A. N. Hanafy, N. Chitosan as a Natural Copolymer with Unique Properties for the Development of Hydrogels. Appl. Sci. 2019, 9, 2193. https://doi.org/10.3390/app9112193
Sami El-banna F, Mahfouz ME, Leporatti S, El-Kemary M, A. N. Hanafy N. Chitosan as a Natural Copolymer with Unique Properties for the Development of Hydrogels. Applied Sciences. 2019; 9(11):2193. https://doi.org/10.3390/app9112193
Chicago/Turabian StyleSami El-banna, Fatma, Magdy Elsayed Mahfouz, Stefano Leporatti, Maged El-Kemary, and Nemany A. N. Hanafy. 2019. "Chitosan as a Natural Copolymer with Unique Properties for the Development of Hydrogels" Applied Sciences 9, no. 11: 2193. https://doi.org/10.3390/app9112193
APA StyleSami El-banna, F., Mahfouz, M. E., Leporatti, S., El-Kemary, M., & A. N. Hanafy, N. (2019). Chitosan as a Natural Copolymer with Unique Properties for the Development of Hydrogels. Applied Sciences, 9(11), 2193. https://doi.org/10.3390/app9112193







