Chronic Obstructive Pulmonary Disease Warning in the Approximate Ward Environment
Abstract
1. Introduction
2. Fundamentals of Breathing
2.1. WCI System Dynamics
2.2. WCI System with Breathing
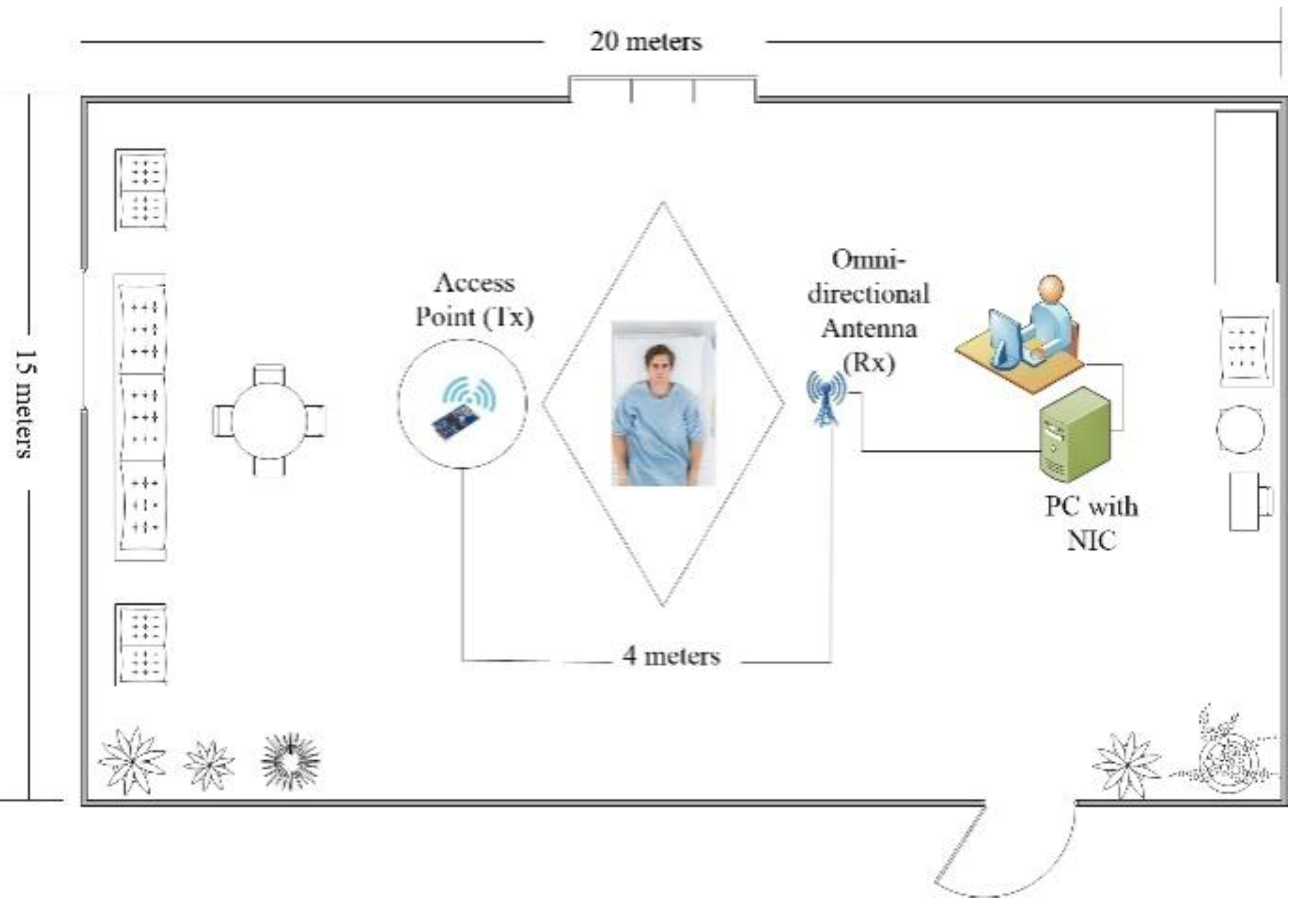
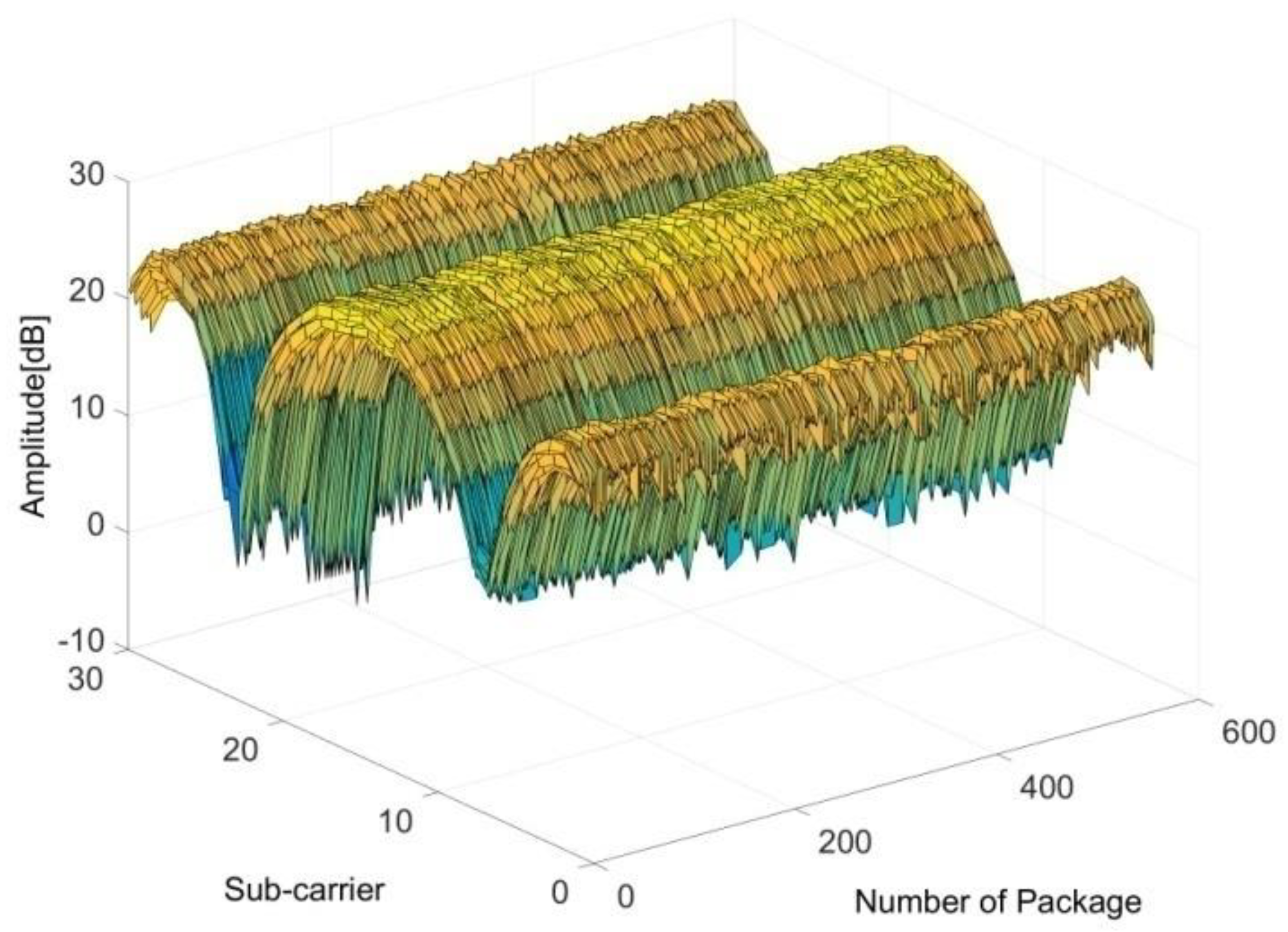
3. Design Implementation and C-Band Sensing
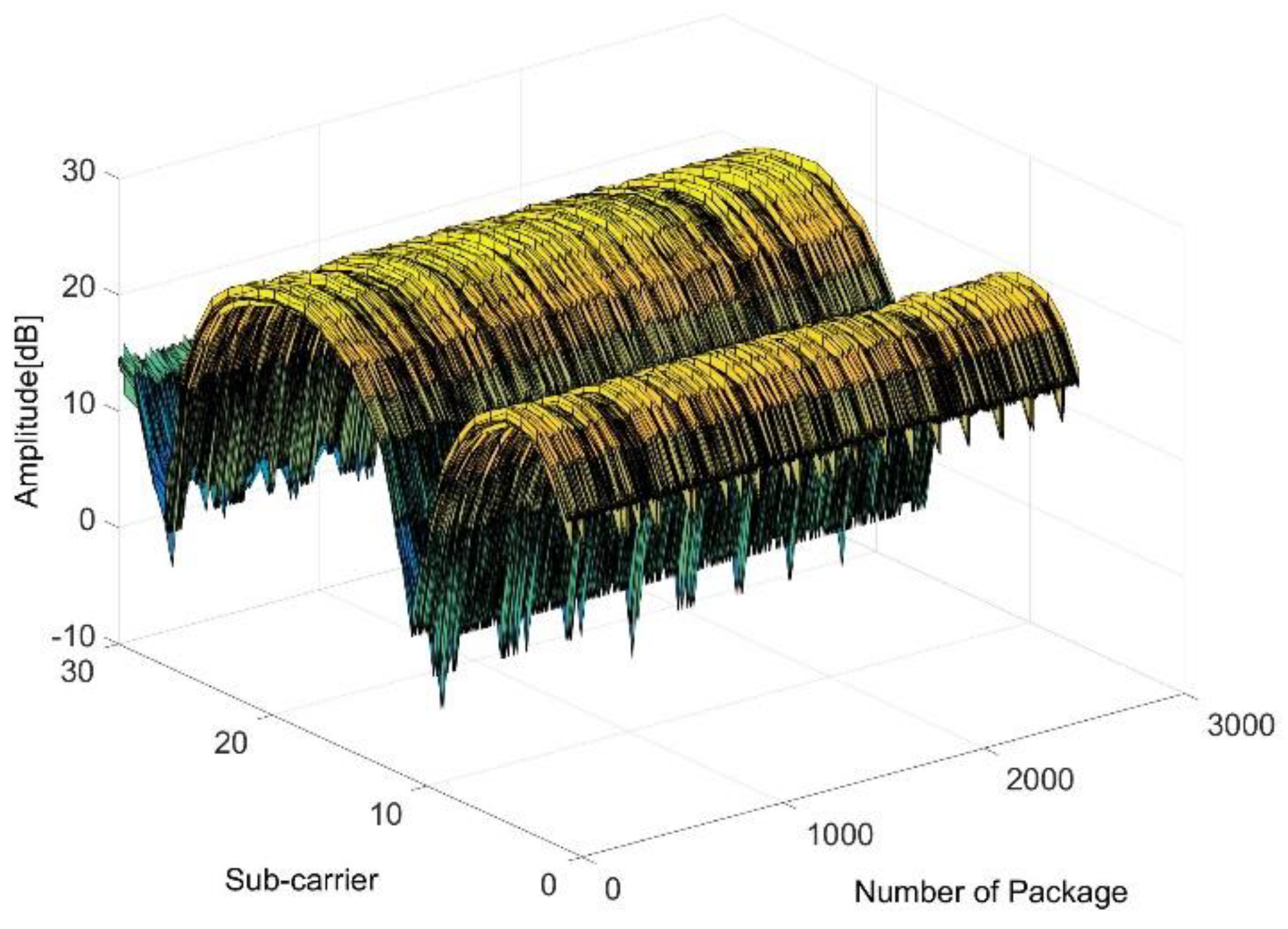
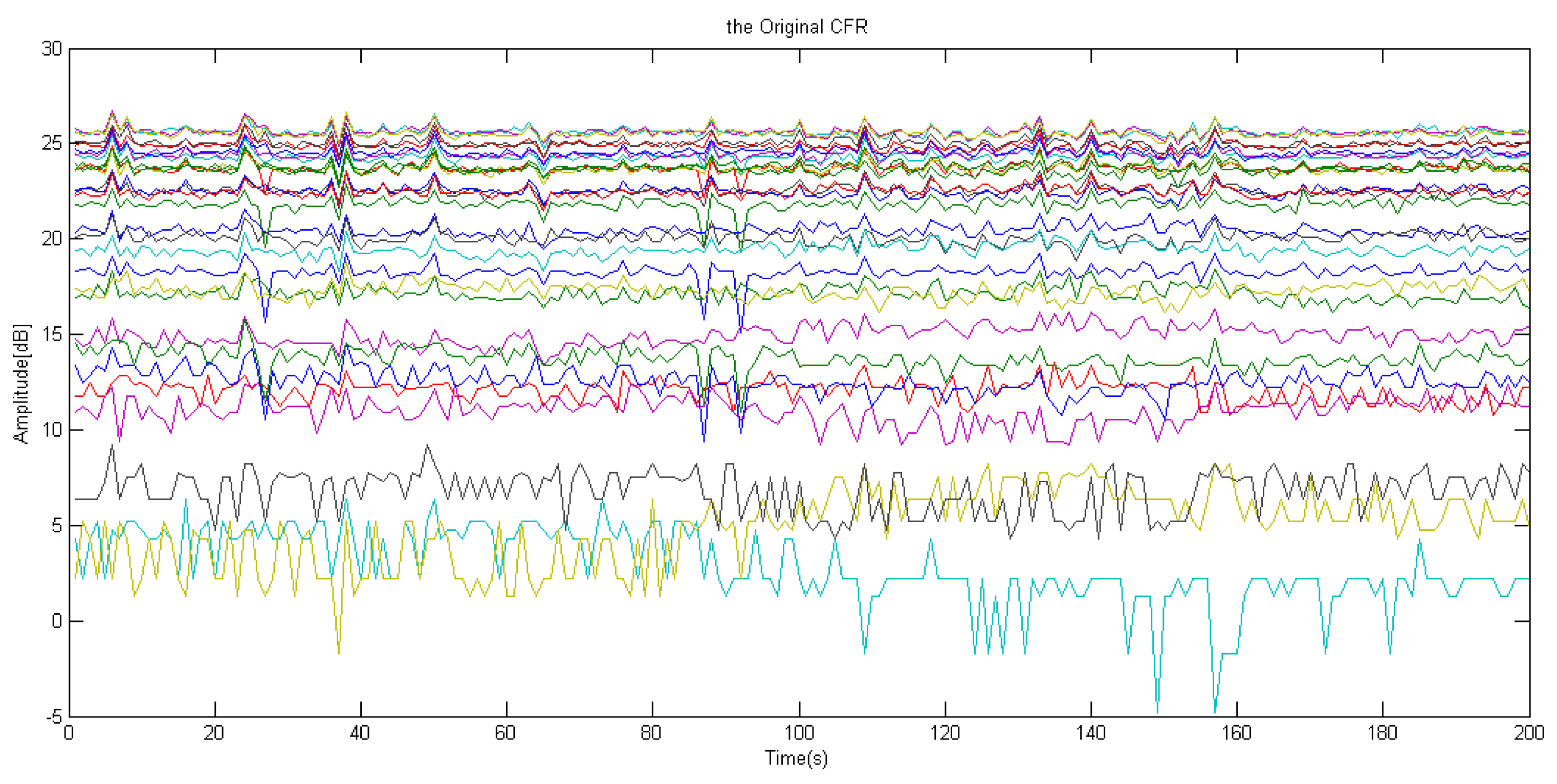
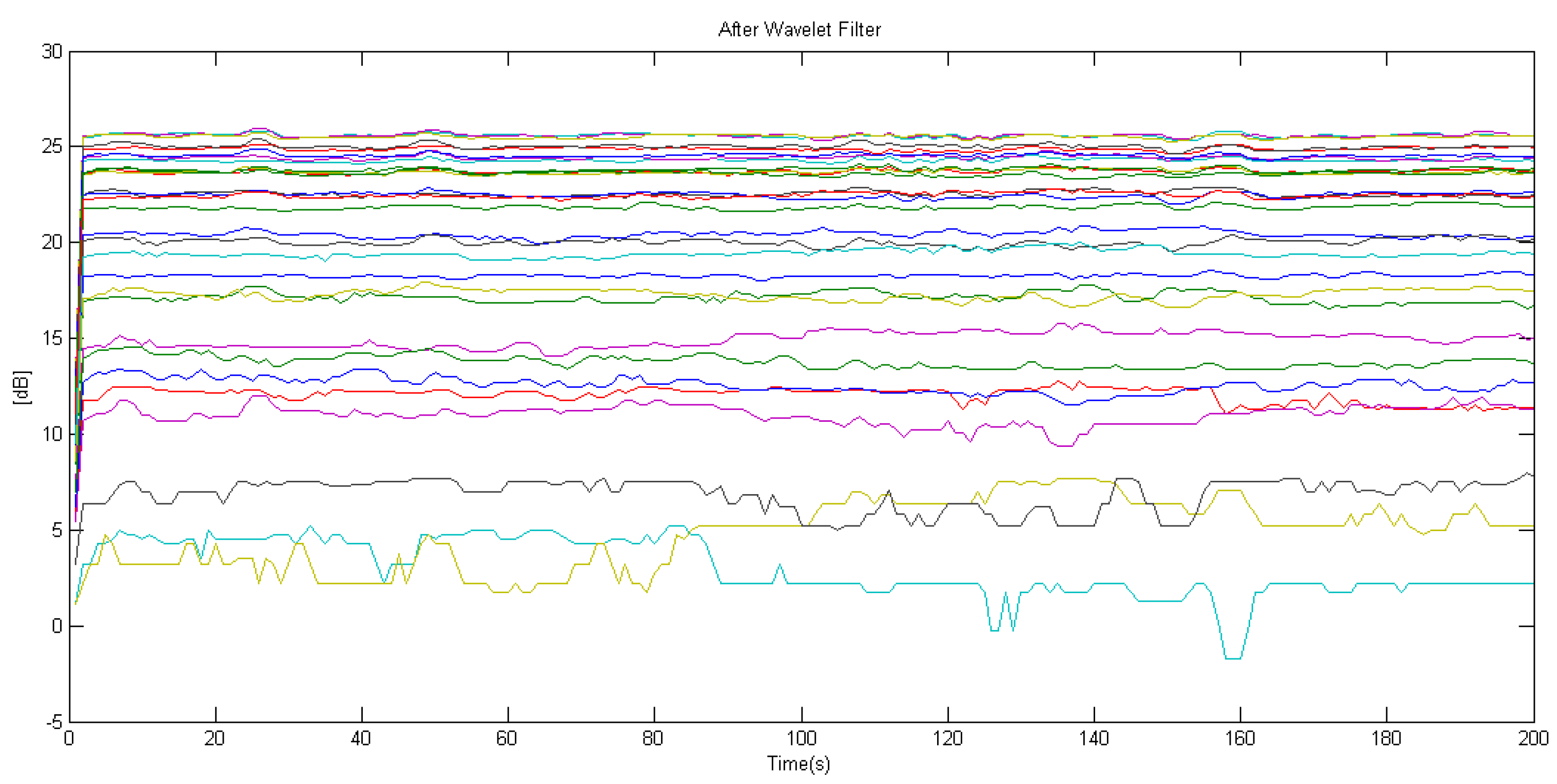
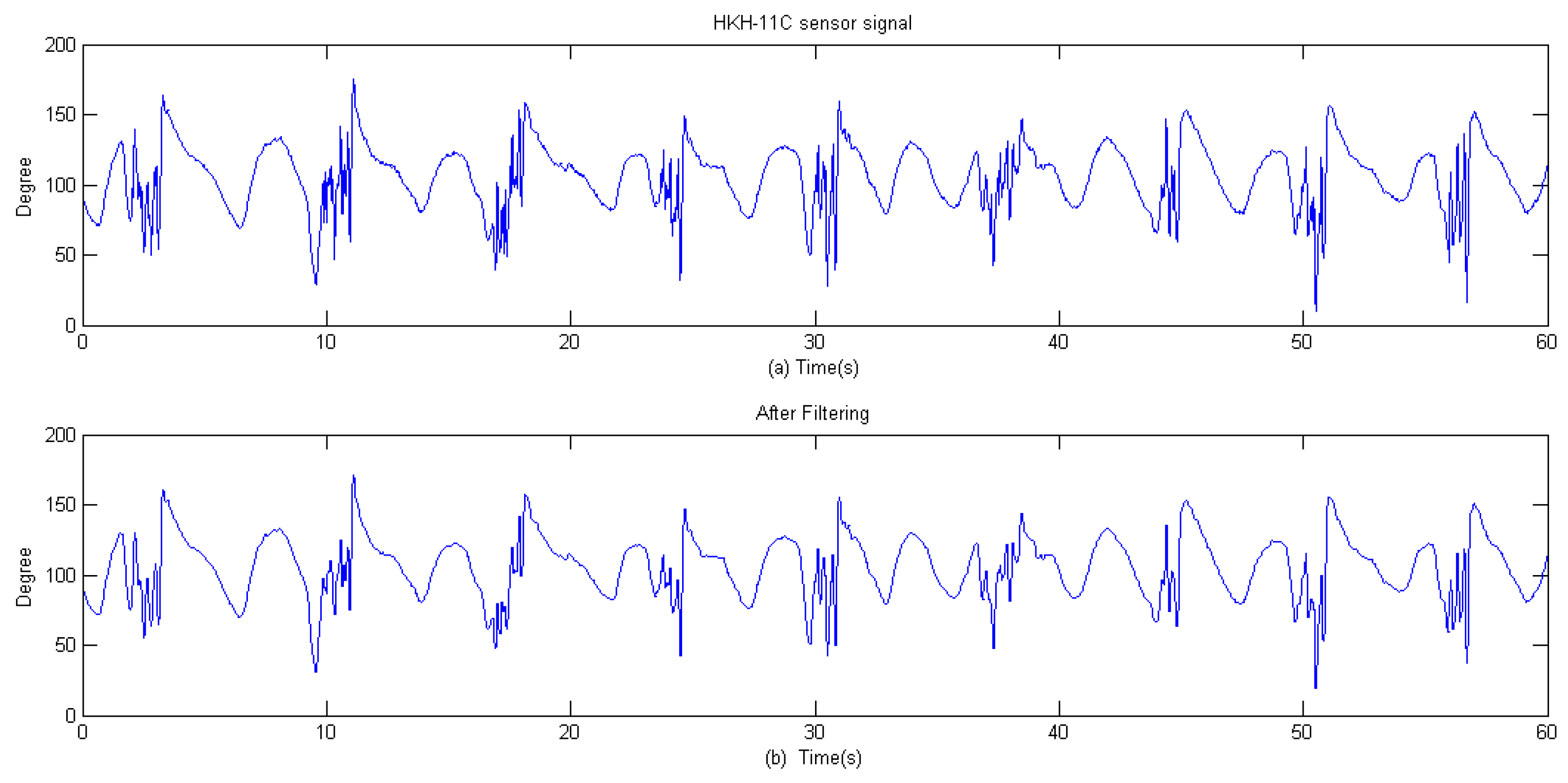
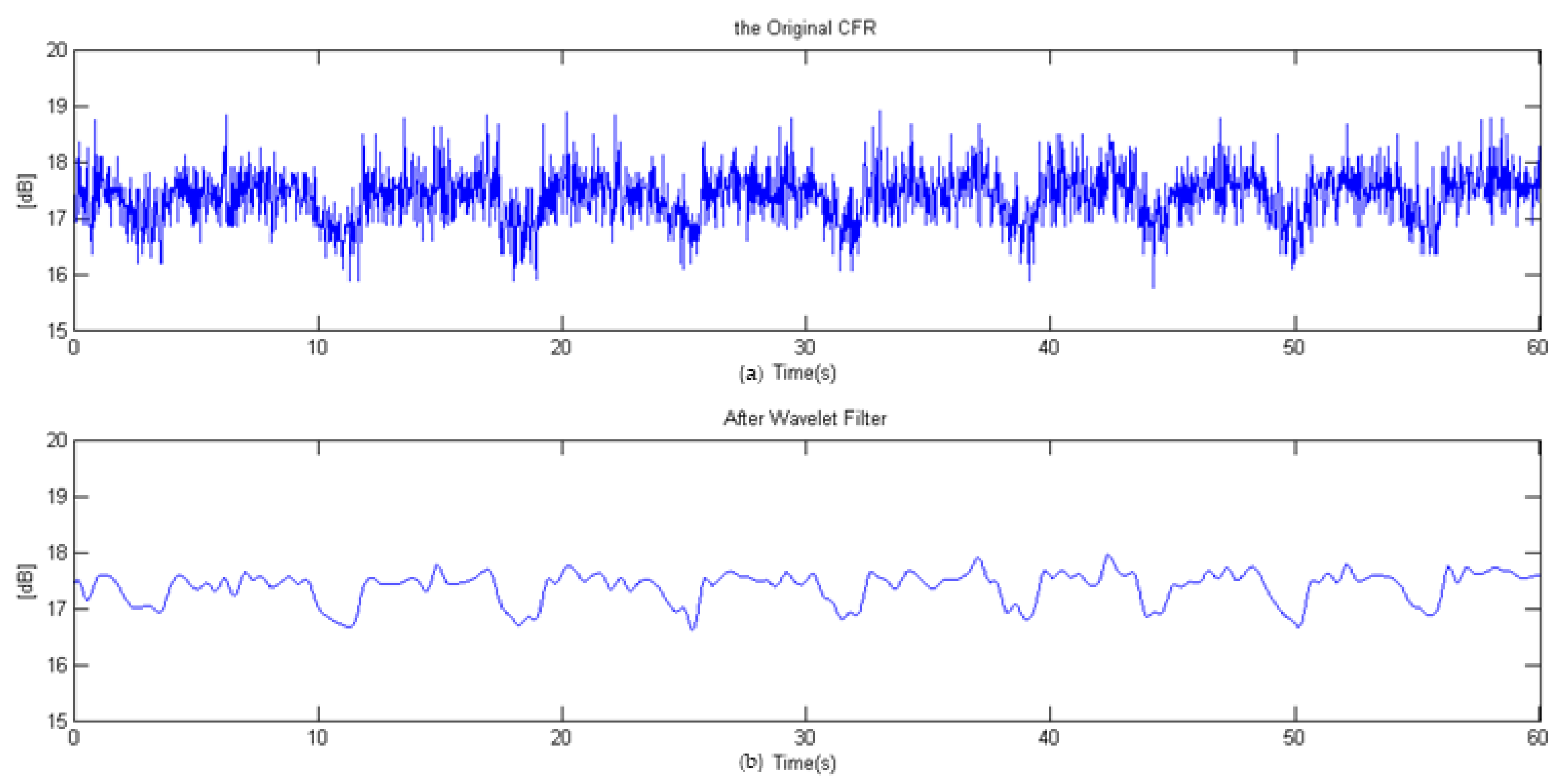
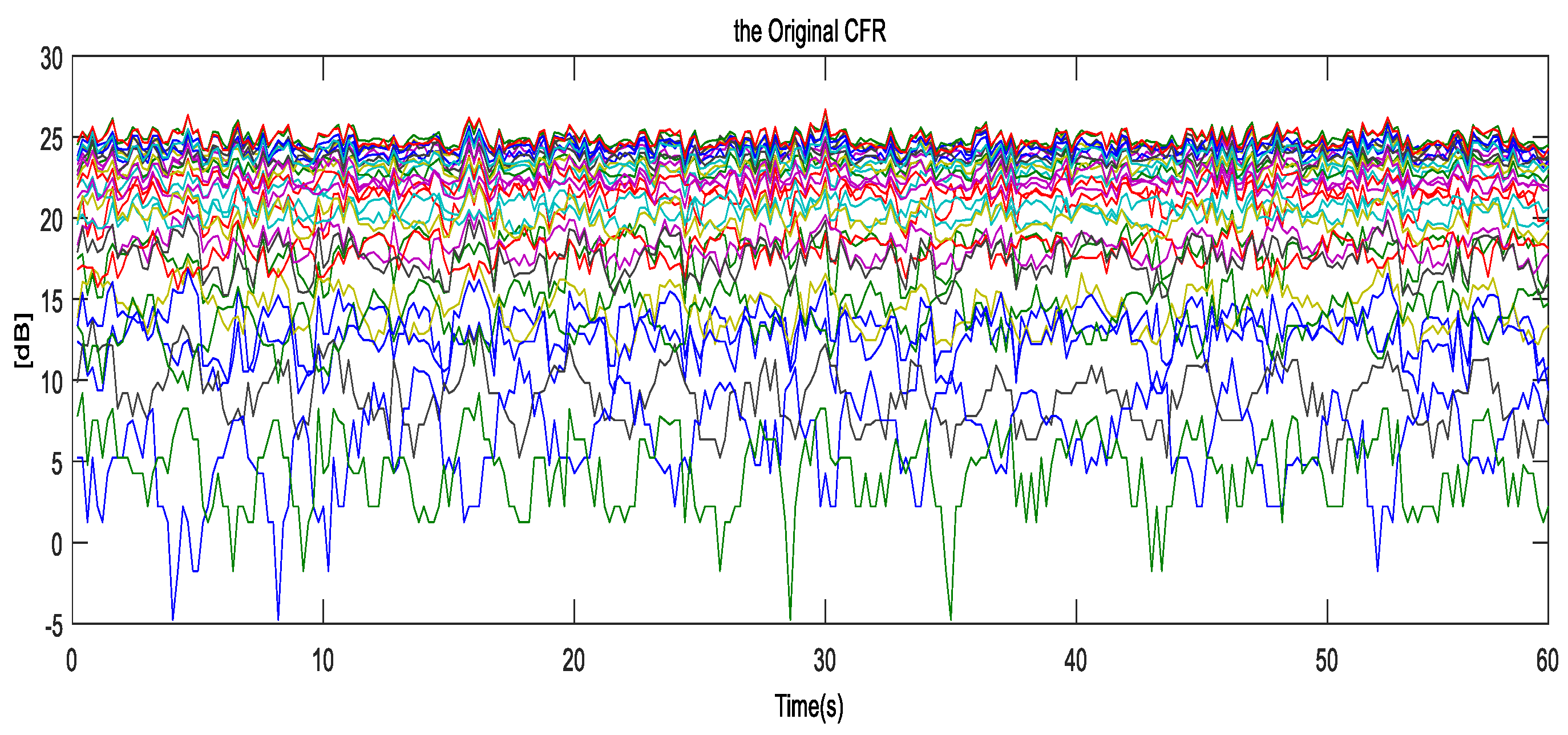
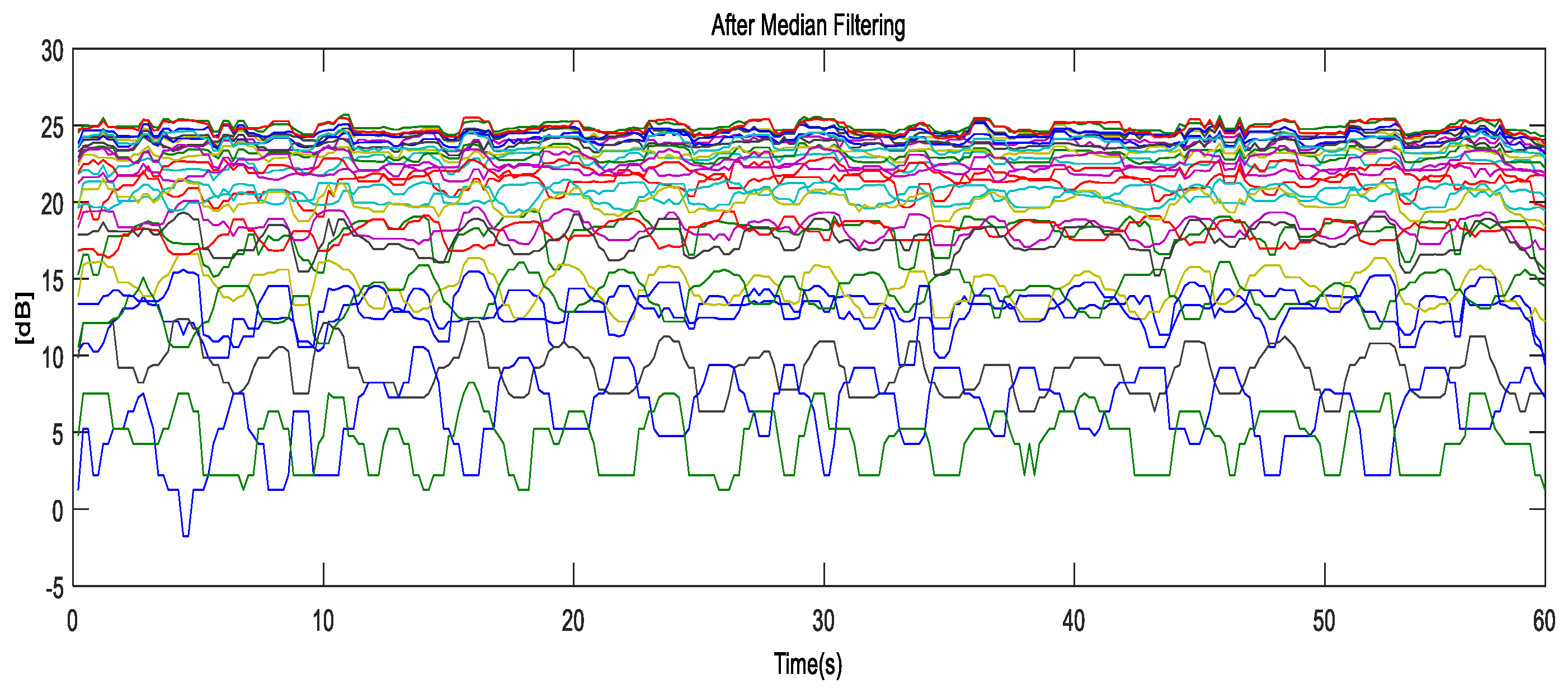
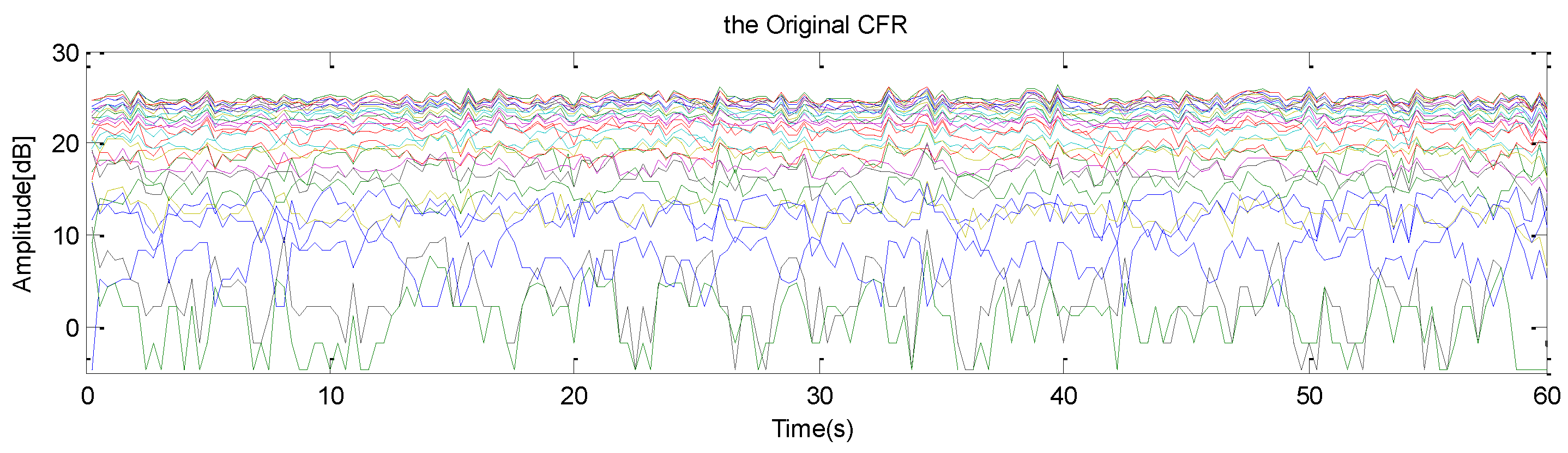
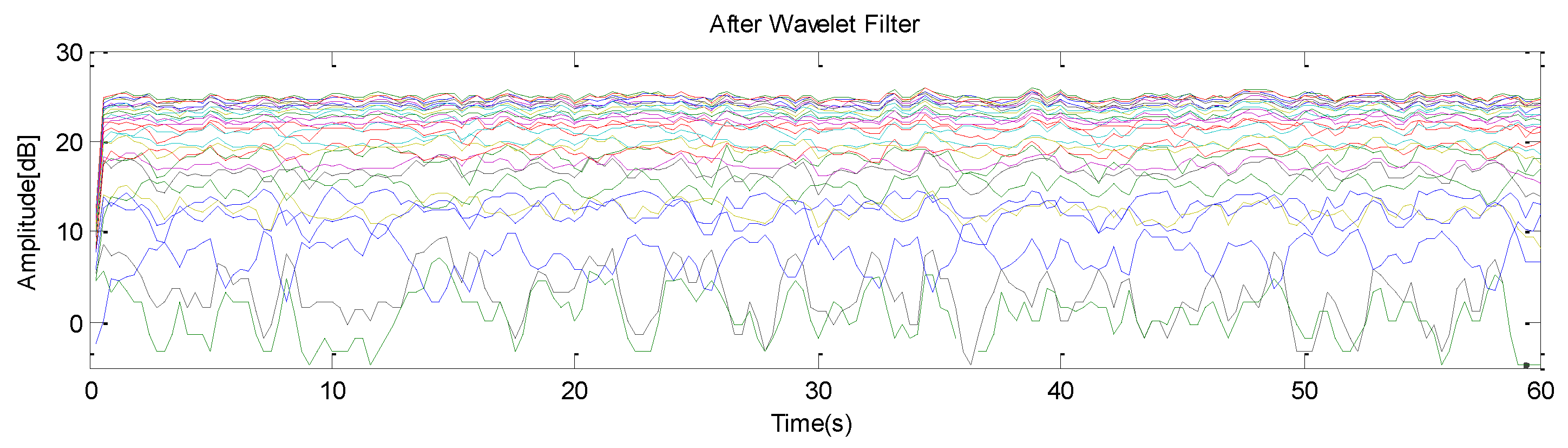
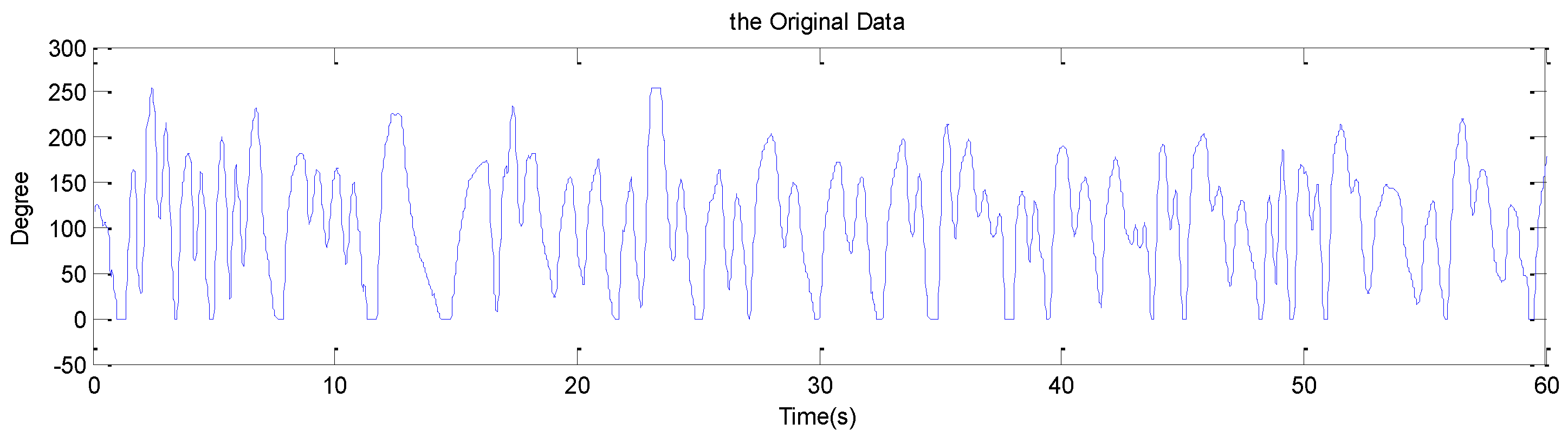
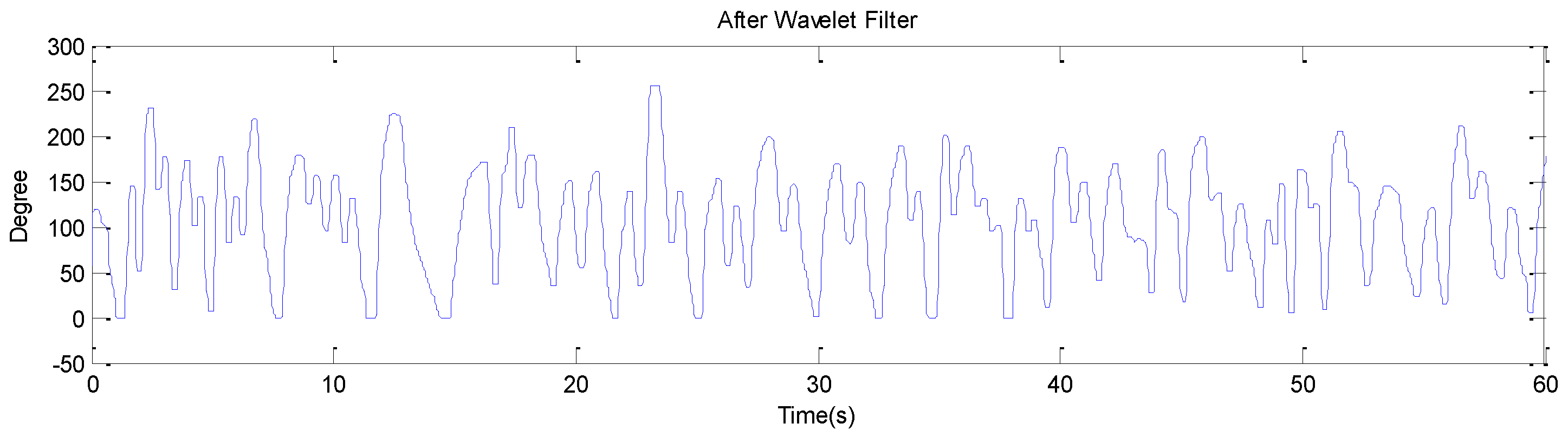
4. Monitoring Breathing and Its Analysis
4.1. Monitoring Coughing Pattern
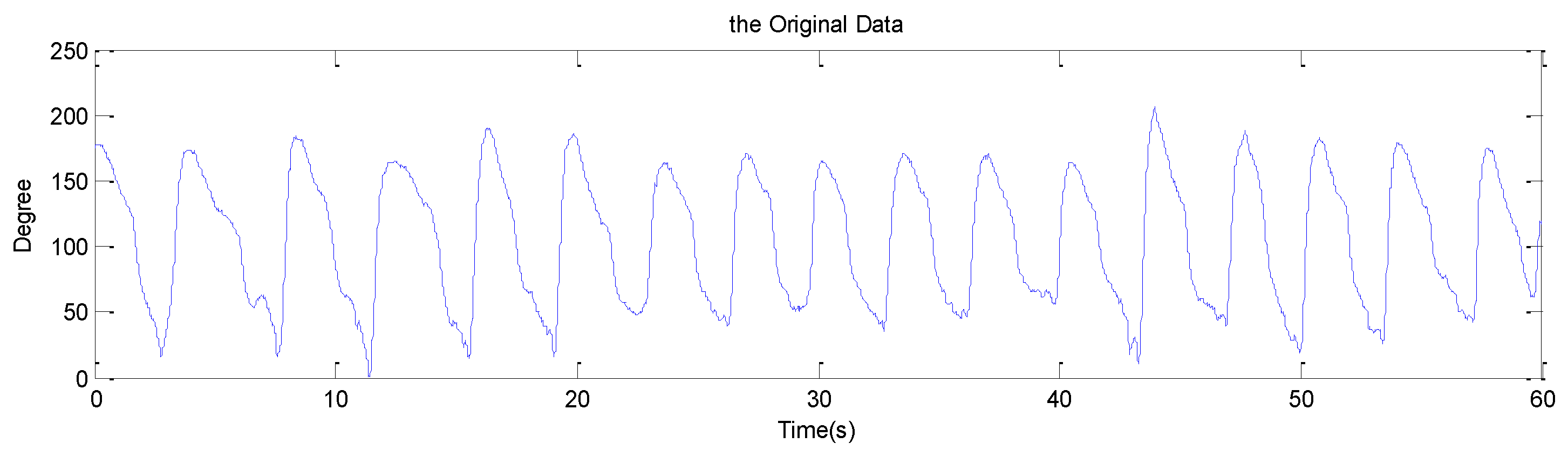
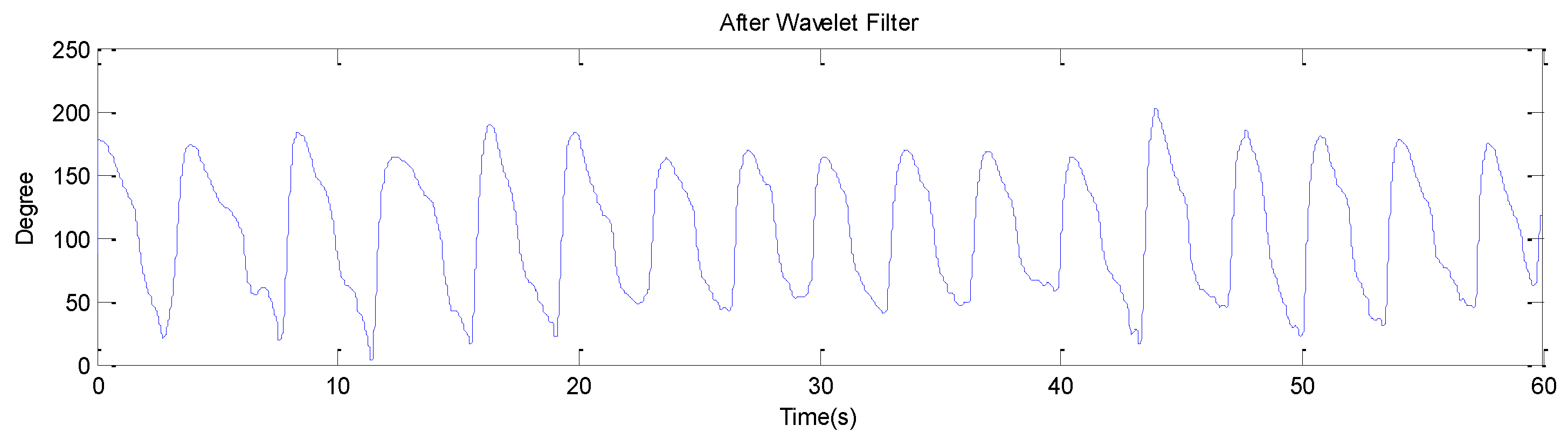
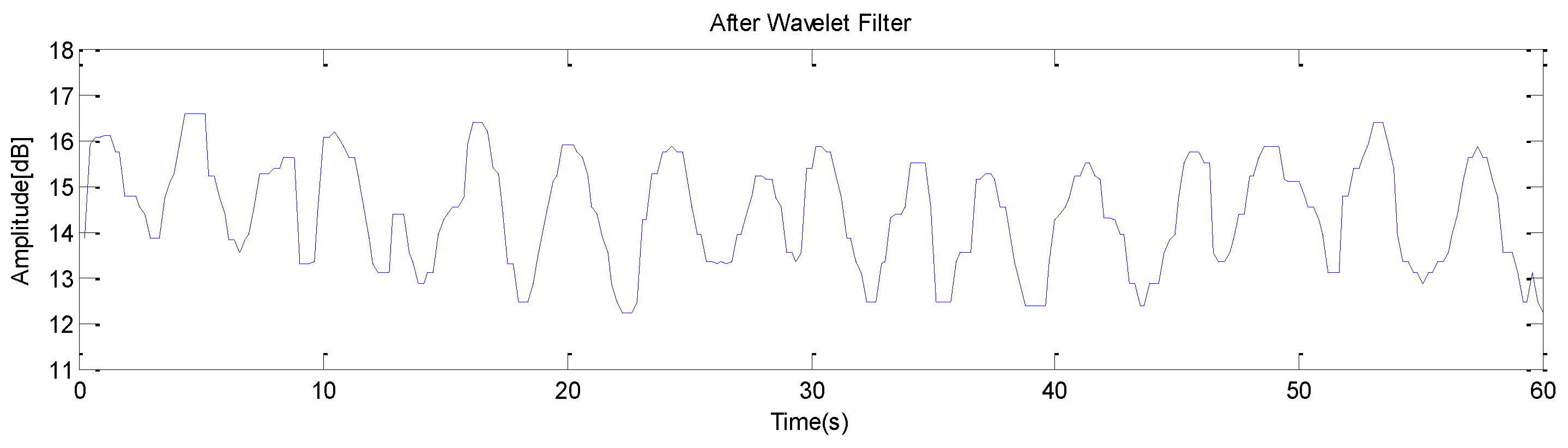
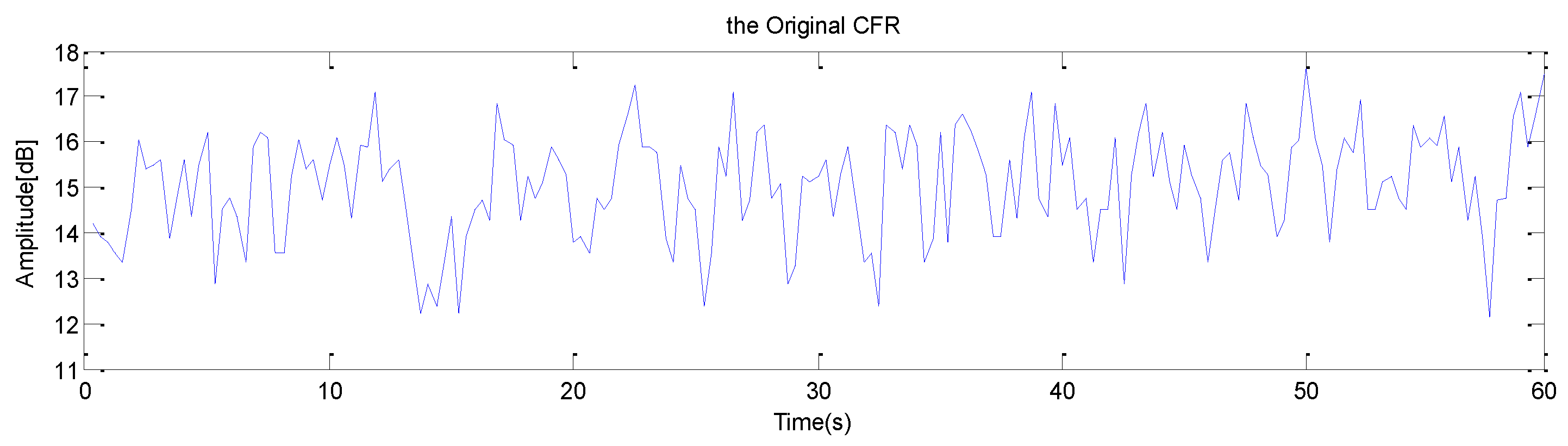
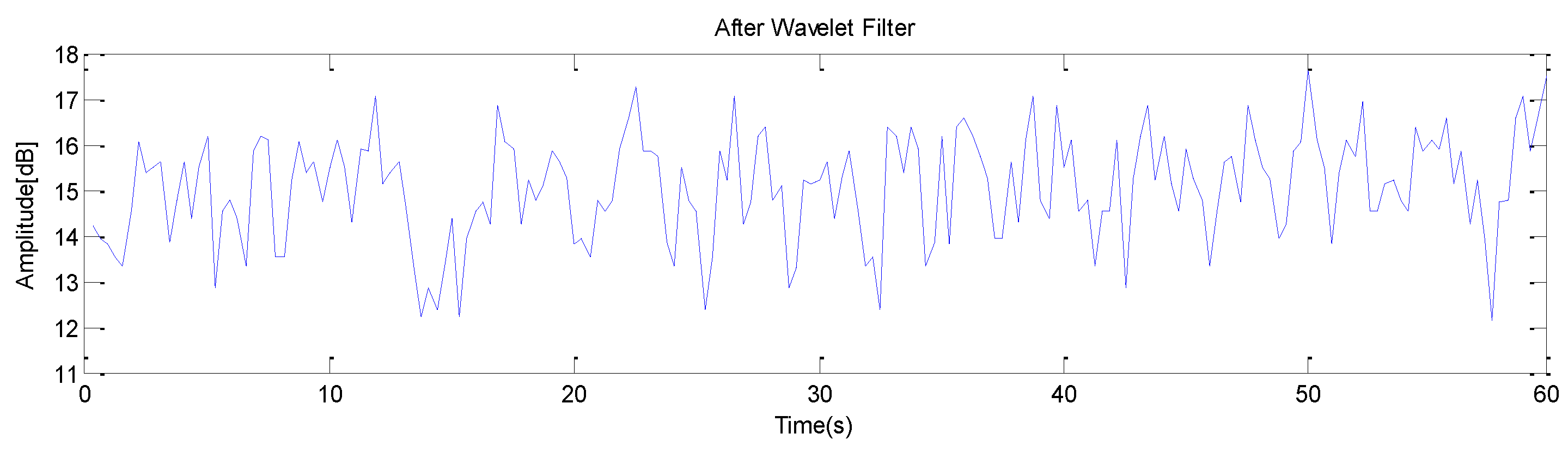
4.2. Monitoring Normal Breathing
4.3. Monitoring Abnormal Breathing
5. Spearman’s Rank Correlation
- = Rank correlation coefficient.
- N = Total number of pair observation.
- D = Rank difference.
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Xu, Y. Emerging Radio Communication Technology and Applications. Article by State Radio Monitoring Center of China Radio Monitoring Department. Available online: https://www.fiercewireless.com/wireless/china-reserves-spectrum-for-5g-says-more-low-band-frequencies-coming-report (accessed on 15 November 2017).
- Wang, T.; Li, G.; Ding, J.; Miao, Q.; Li, J.; Wang, Y. 5G spectrum: Is China Ready? IEEE Commun. Mag. 2015, 53, 58–65. [Google Scholar] [CrossRef]
- Van Putten, A.F.; Hitchings, D.J.; Quanjer, P.H. Portable electronic peak flowmeter for improved diagnosis of chest diseases in COPD patients. In Proceedings of the IEEE Instrumentation Technology Conference, Irvine, CA, USA, 18–20 May 1993. [Google Scholar]
- Garcia-Aymerich, J.; Farrero, E.; Felez, M.A.; Izquierdo, J.; Marrades, R.M.; Anto, J.M. Risk factors of readmission to hospital for a COPD exacerbation: A prospective study. Thorax 2003, 58, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Troosters, T.; Sciurba, F.; Battaglia, S.; Langer, D.; Valluri, S.R.; Martino, L.; Benzo, R.; Andre, D.; Weisman, I.; Decramer, M. Physical inactivity in patients with COPD, a controlled multi-center pilot-study. Respir. Med. 2010, 104, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Erden, F.; Cetin, A.E. Breathing Detection Based on the Topological Features of IR Sensor and Accelerometer Signals. In Proceedings of the IEEE 50th Asilomar Conference on Signal and Systems and Computer, Pacific Grove, CA, USA, 6–9 November 2016. [Google Scholar]
- Park, B.K.; Yamada, S.; Boric-Lubecke, O.; Lubecke, V. Single channel receiver limitations in Doppler radar measurements of periodic motion. In Proceedings of the 2006 IEEE Radio and Wireless Symposium, San Diego, CA, USA, 17–19 October 2006; pp. 99–102. [Google Scholar]
- Li, W.; Tan, B.; Piechocki, R.J. Non-Contact Breathing Detection Using Passive Radar. In Proceedings of the IEEE International Conference on Communication (ICC), Kuala Lumpur, Malaysia, 22–27 May 2016. [Google Scholar]
- Abdelnasser, H.; Harras, K.A.; Youssef, M. Ubibreathe: A ubiquitous non-invasive WiFi-based breathing estimator. In Proceedings of the 16th ACM International Symposium on Mobile Ad Hoc Networking and Computing, New York, NY, USA, 22–25 June 2015; pp. 277–286. [Google Scholar]
- Liu, J.; Wang, Y.; Chen, Y.; Yang, J.; Chen, X.; Cheng, J. Tracking vital signs during sleep leveraging off-the-shelf WiFi. In Proceedings of the 16th ACM International Symposium on Mobile Ad Hoc Networking and Computing, New York, NY, USA, 22–25 June 2015; pp. 267–276. [Google Scholar]
- Alemaryeen, A.; Noghanian, S.; Fazel-Rezai, R. Antenna Effects on Respiratory Rate Measurement Using a UWB Radar System. IEEE J. Electromagn. RF Microw. Med. Biol. 2018, 2, 87–93. [Google Scholar] [CrossRef]
- Andre, N.; Druart, S.; Gerard, P.; Pampin, R.; Moreno-Hagelsieb, L.; Kezai, T.; Francis, L.A.; Flandre, D.; Raskin, J.P. Miniaturized Wireless Sensing System for Real-Time Breath Activity Recording. IEEE Sens. J. 2010, 10, 178–184. [Google Scholar] [CrossRef]
- Patwari, N.; Wilson, J.; Ananthanarayanan, S.; Kasera, S.K.; Westenskow, D.R. Monitoring Breathing via Signal Strength in Wireless Networks. IEEE Trans. Mob. Comput. 2014, 13, 1774–1786. [Google Scholar] [CrossRef]
- Wang, C.W.; Hunter, A.; Gravill, N.; Matusiewicz, S. Unconstrained Video Monitoring of Breathing Behavior and Application to Diagnosis of Sleep Apnea. IEEE Trans. Biomed. Eng. 2014, 61, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Poreva, A.; Karplyuk, Y.; Makarenkova, A.; Makarenkov, A. Detection of COPD’s Diagnostic Signs Based on Polyspectral Lung Sounds Analysis of Respiratory Phases. In Proceedings of the 2015 IEEE 35th International Conference on Electronics and Nanotechnology (ELNANO), Kiev, Ukraine, 21–24 April 2015. [Google Scholar]
- Ritz, C.P.; Powers, E.J.; Bengtson, R.D. Experimental measurement of three wave coupling and energy cascading. Phys. Fluids 1989, 1, 153–163. [Google Scholar] [CrossRef]
- Chen, C.; Chen, Y.; Han, Y.; Lai, H.Q.; Zhang, F.; Wang, B.; Liu, K.J.R. TR-BREATH: Time-Reversal Breathing Rate Estimation and Detection. IEEE Trans. Biomed. Eng. 2018. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.A.; Zhang, Z.; Ren, A.; Zhao, N.; Yang, X.; Zhao, W.; Yang, J.; Zhao, J.; Sun, W.; Hao, Y. Buried Object Sensing Considering Curved Pipeline. IEEE Antennas Wirel. Propag. Lett. 2017, 16, 2771–2775. [Google Scholar] [CrossRef]
- Abramowitz, M. Handbook of Mathematical Functions, With Formulas, Graphs, and Mathematical Tables; Dover Publications, Incorporated: Mineola, NY, USA, 1974. [Google Scholar]
- Shah, S.A.; Ren, A.; Fan, D.; Zhang, Z.; Zhao, N.; Yang, X.; Luo, M.; Wang, W.; Hu, F.; Rehman, M.U.; et al. Internet of Things for Sensing: A Case Study in the Healthcare System. Appl. Sci. 2018, 8, 508. [Google Scholar] [CrossRef]
- Fan, D.; Ren, A.; Zhao, N.; Yang, X.; Zhang, Z.; Shah, S.A.; Hu, F.; Abbasi, Q.H. Breathing Rhythm Analysis in Body Centric Networks. IEEE Access 2018, 6, 32507–32513. [Google Scholar] [CrossRef]
- Yang, X.; Shah, S.A.; Ren, A.; Zhao, N.; Fan, D.; Hu, F.; Ur-Rehman, M.; von Deneen, K.M.; Tian, J. Wandering Pattern Sensing at S-Band. IEEE J. Biomed. Health Inform. 2017. [Google Scholar] [CrossRef] [PubMed]
- Kaltiokallio, O.J.; Yigitler, H.; Jäntti, R.; Patwari, N. Non-Invasive Respiration Rate Monitoring Using a Single COTS TX-RX Pair. In Proceedings of the 13th International Symposium on Information Processing in Sensor Networks, Berlin, Germany, 15–17 April 2014; pp. 59–70. [Google Scholar]


| S/No. | Techniques for Monitoring Breathing | Explanation | Advantages | Limitations |
|---|---|---|---|---|
| 1 | UWB Radar System | Ala Alemaryeen et al. [11] proposed ultra-wide band (UWB) radar based respiratory monitoring system. | Shows less error, more robust to noise. | Complex, Costly. |
| 2 | Non-invasive capacitive micro Sensor | Nicolas Andre et al. [12] proposed the concept of using capacitive micro sensors and negative temperature coefficient thermistor integrated on a silicon chip to monitor breathing with the help of wireless sensor system. | Useful for larger space, monitoring is easy. | More hardware, time consuming. |
| 3 | RSS system | Neal Patwari et al. [13], proposed the concept of monitoring breathing with the help of received signal strength in wireless sensors network. | Reliable detection, less RMS error. | RSS behaves less efficiently in the presence of fading and scattering, performance may decrease due to multipath propagation. |
| 4 | Video Monitoring | Ching We Wang et al. [14], proposed the idea of real-time automated infrared video monitoring technique for detection of respiratory activities. | High accuracy rate, robust to many body movements. | Less cost effective, excessive hardware, complex architecture. |
| Subjects | Age | Height (cm) | Weight (Kg) |
|---|---|---|---|
| 1 | 29 | 171 | 75 |
| 2 | 30 | 169 | 78 |
| 3 | 35 | 161 | 71 |
| 4 | 31 | 174 | 85 |
| 5 | 26 | 173 | 87 |
| 6 | 39 | 176 | 90 |
| 7 | 40 | 170 | 78 |
| 8 | 22 | 169 | 73 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Q.; Haider, D.; Wang, W.; Shah, S.A.; Yang, X.; Abbasi, Q.H. Chronic Obstructive Pulmonary Disease Warning in the Approximate Ward Environment. Appl. Sci. 2018, 8, 1915. https://doi.org/10.3390/app8101915
Zhang Q, Haider D, Wang W, Shah SA, Yang X, Abbasi QH. Chronic Obstructive Pulmonary Disease Warning in the Approximate Ward Environment. Applied Sciences. 2018; 8(10):1915. https://doi.org/10.3390/app8101915
Chicago/Turabian StyleZhang, Qing, Daniyal Haider, Weigang Wang, Syed Aziz Shah, Xiaodong Yang, and Qammer H. Abbasi. 2018. "Chronic Obstructive Pulmonary Disease Warning in the Approximate Ward Environment" Applied Sciences 8, no. 10: 1915. https://doi.org/10.3390/app8101915
APA StyleZhang, Q., Haider, D., Wang, W., Shah, S. A., Yang, X., & Abbasi, Q. H. (2018). Chronic Obstructive Pulmonary Disease Warning in the Approximate Ward Environment. Applied Sciences, 8(10), 1915. https://doi.org/10.3390/app8101915







