Mechanical Resistance of Implant-Supported Crowns with Abutments Exhibiting Different Margin Designs
Abstract
1. Introduction
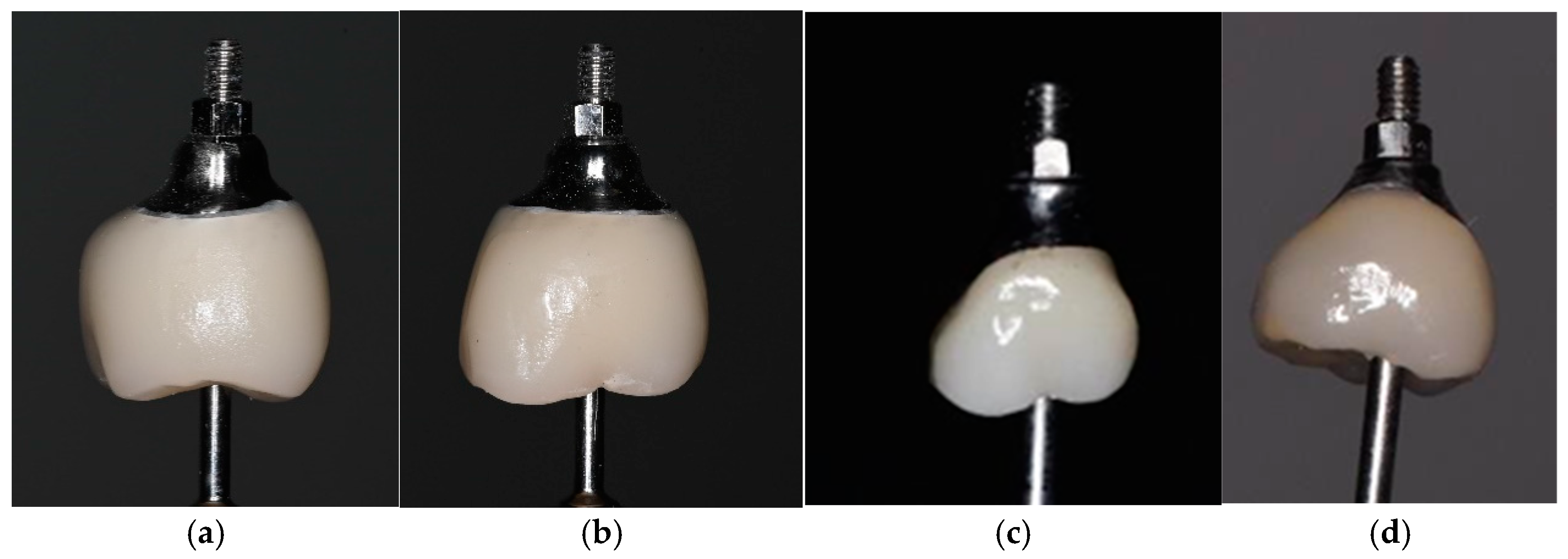
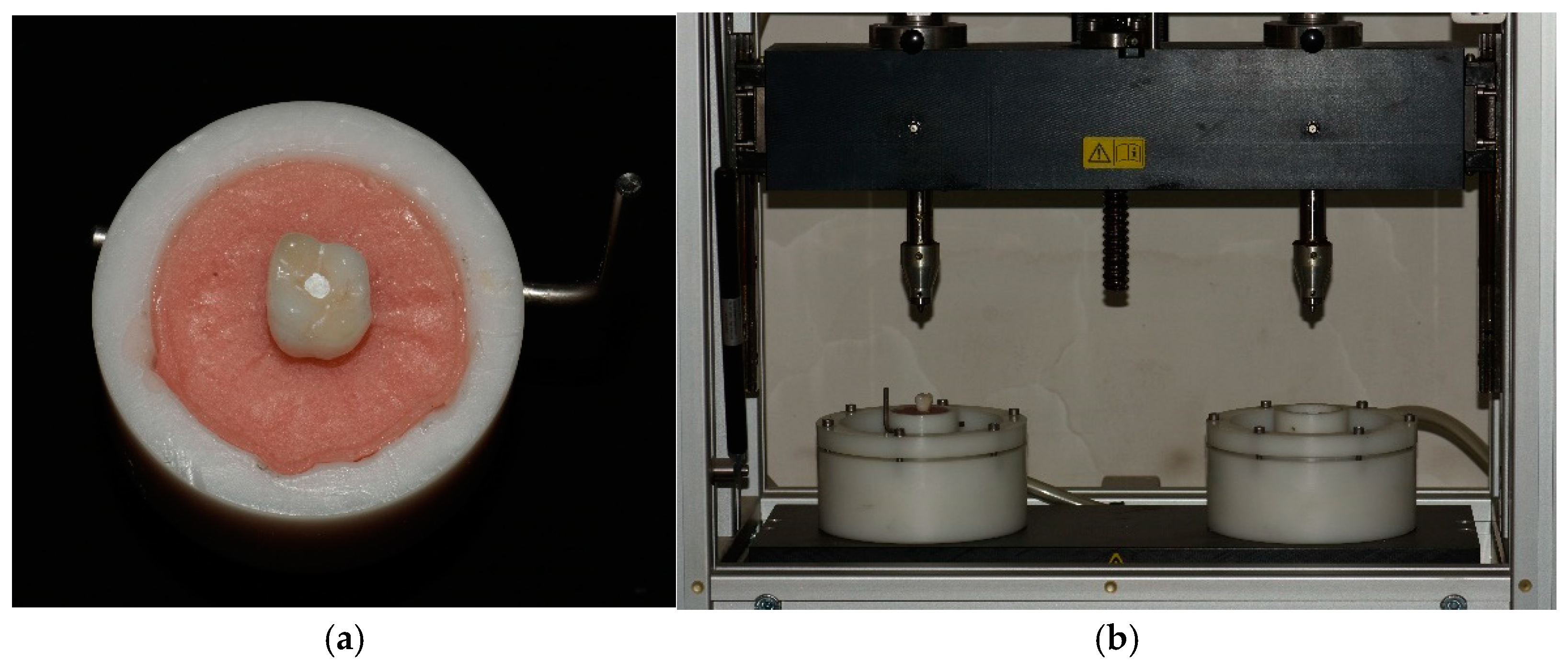
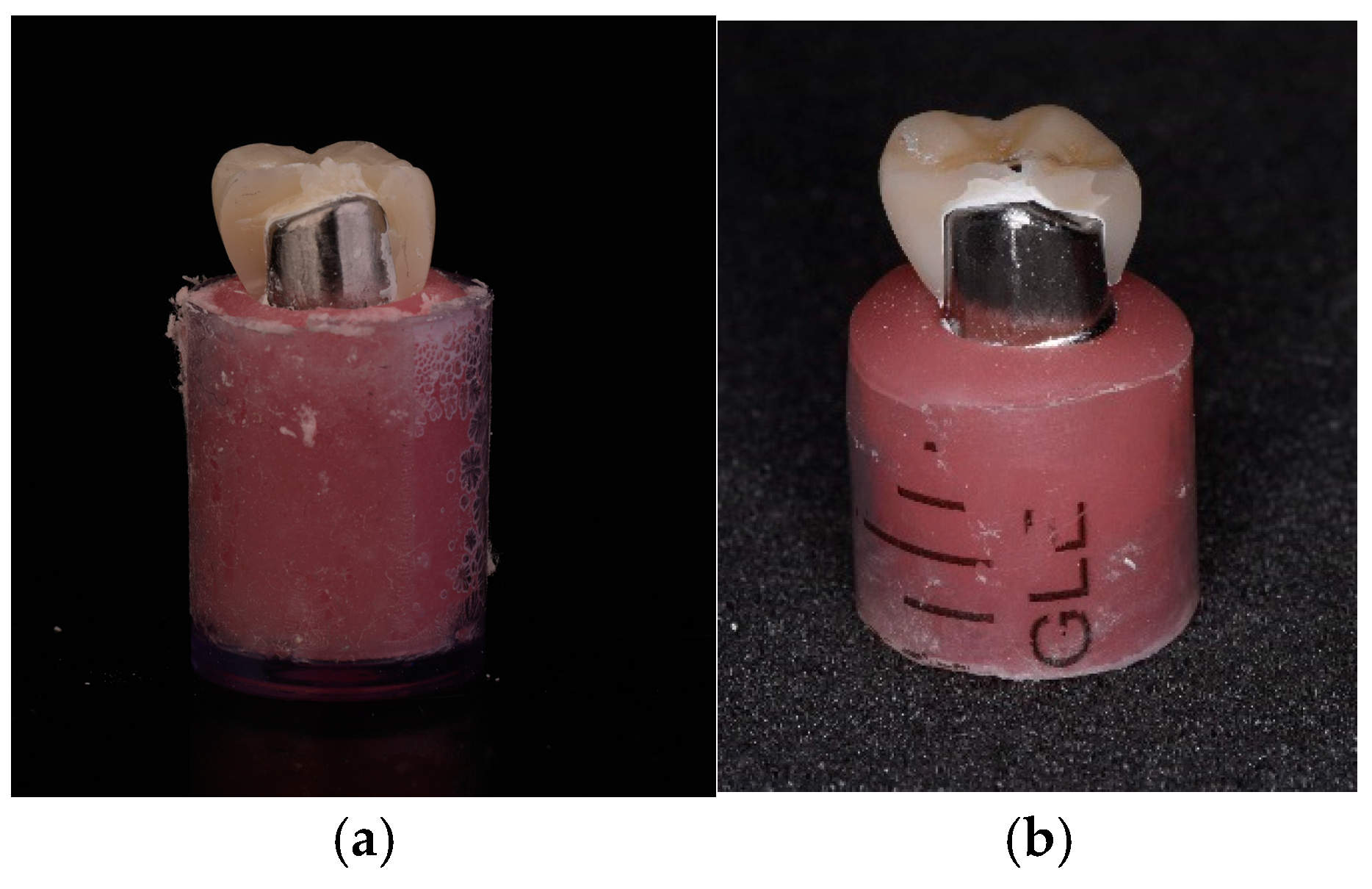
2. Materials and Methods
- Deformation of the connecting screw;
- Deformation of the abutment;
- Presence of a fracture line or crack in the monolithic crown;
- Observable failure of the adhesive bond between the monolithic crown and the abutment;
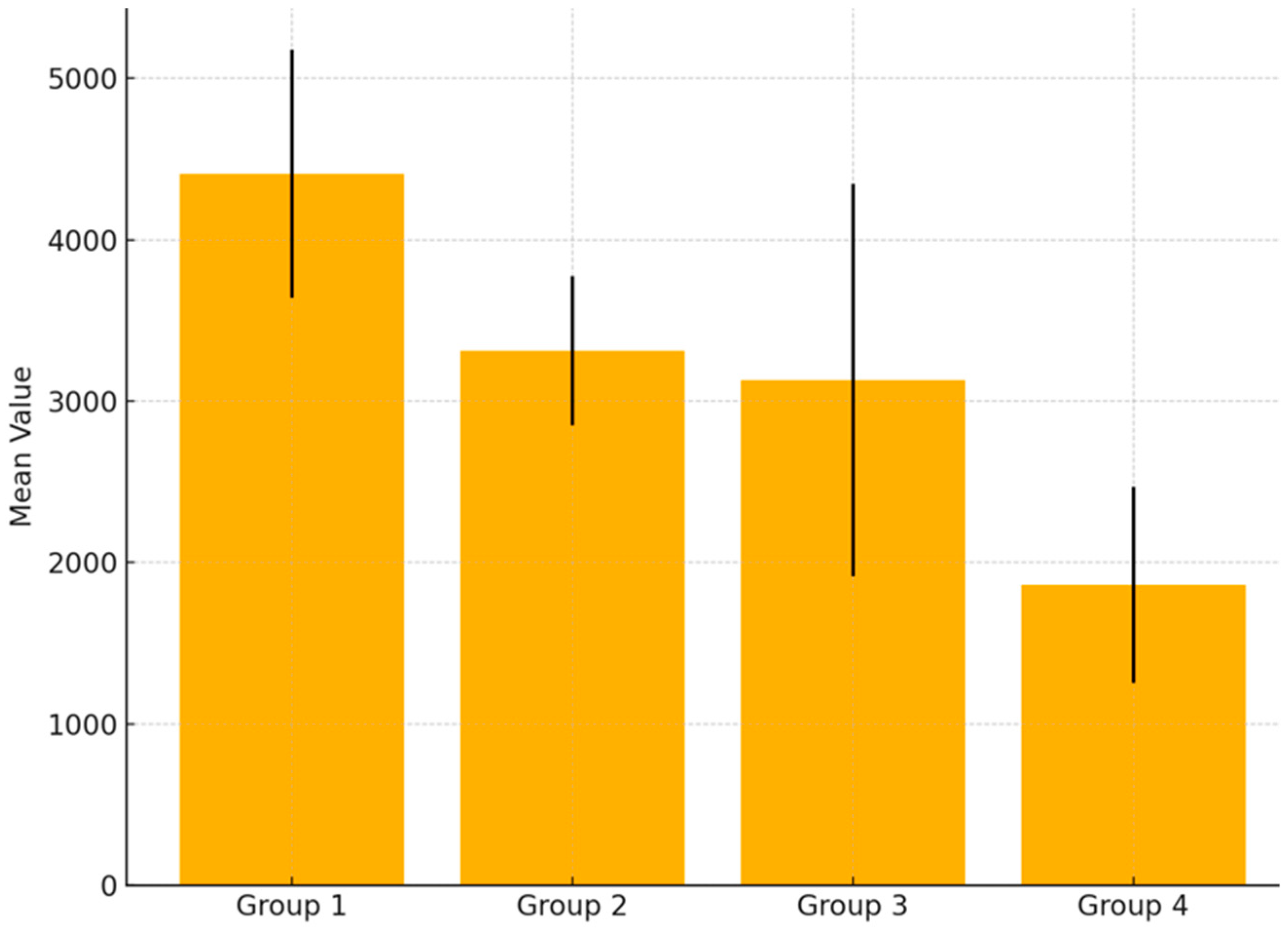
- Destruction of either the monolithic crown or the titanium abutment. Any fragmentation observed in the sample was considered as destruction.Mode of failure was defined due to Burke‘s classification [28]. Type I: minimal fracture or crack in the crown. Type II: less than half of the crown lost. Type III: crown fracture through midline or half of the crown displaced or lost. Type IV: more than half of the crown lost. Type V: severe fracture of the crown and/or tooth. In addition, cracks, chipping, delamination, and catastrophic total failures were noted.Statistical analysis was performed with the assistance of Microsoft Excel software (v.2019–2021). Descriptive statistics were used to show the mean values and variations in results. Moreover, analysis of variance (ANOVA) test was applied to compare the mean values of the four groups and measure the existence of statistical significance. More precise results regarding the existence of statistical significance across the specific groups of materials were obtained by using Games-Howell post hoc test. The use of a post hoc test was important to avoid Type I error and false positive differences—a common problem when running multiple ANOVA tests. It is also worth noting that the conventional confidence threshold of 0.05 was applied to confirm the existence of statistical significance.
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Carossa, M.; Alovisi, M.; Crupi, A.; Ambrogio, G.; Pera, F. Full-Arch Rehabilitation Using Trans-Mucosal Tissue-Level Implants with and without Implant-Abutment Units: A Case Report. Dent. J. 2022, 10, 116. [Google Scholar] [CrossRef] [PubMed]
- Belser, U.C.; Schmid, B.; Higginbottom, F.; Buser, D. Outcome analysis of implant restorations located in the anterior maxilla: A review of the recent literature. Int. J. Oral Maxillofac. Implant. 2004, 19 (Suppl. 30–42). [Google Scholar] [PubMed]
- Fenner, N.; Hämmerle, C.H.; Sailer, I.; Jung, R.E. Long-term clinical, technical, and esthetic outcomes of all-ceramic vs. titanium abutments on implant supporting single-tooth reconstructions after at least 5 years. Clin. Oral Implant. Res. 2016, 27, 716–723. [Google Scholar] [CrossRef]
- de Vasconcelos, J.E.L.; de Matos, J.D.M.; Queiroz, D.A.; Lopes, G.d.R.S.; de Lacerda, B.C.G.V.; Bottino, M.A.; Turssi, C.P.; Basting, R.T.; do Amaral, F.L.B.; França, F.M.G. Implant—Abutment Misfit after Cyclic Loading: An In Vitro Experimental Study. Materials 2022, 15, 5341. [Google Scholar] [CrossRef]
- Luthy, H. Strength and toughness of dental ceramics. In CAD/CIM in Aesthetic Dentistry: CEREC 10 Year Anniversary Symposium (1994; Zurich); Mormann, W.H., Ed.; Quintessence: Chicago, IL, USA, 1996; pp. 229–240. [Google Scholar]
- Glauser, R.; Sailer, I.; Wohlwend, A.; Studer, S.; Schibli, M.; Schärer, P. Experimental zirconia abutments for implant-supported single-tooth restorations in esthetically demanding regions: 4-year results of a prospective clinical study. Int. J. Prosthodont. 2004, 17, 285–290. [Google Scholar] [PubMed]
- Canullo, L. Clinical outcome study of customized zirconia abutments for single-implant restorations. Int. J. Prosthodont. 2007, 20, 489–493. [Google Scholar] [PubMed]
- Lops, D.; Meneghello, R.; Sbricoli, L.; Savio, G.; Bressan, E.; Stellini, E. Precision of the Connection between Implant and Standard or Computer-Aided Design/Computer-Aided Manufacturing Abutments: A Novel Evaluation Method. Int. J. Oral Maxillofac. Implant. 2018, 33, 23–30. [Google Scholar] [CrossRef]
- Marchack, C.B. A custom titanium abutment for the anterior single-tooth implant. J. Prosthet. Dent. 1996, 76, 288–291. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Serra-Pastor, B.; Roig-Vanaclocha, A.; Román-Rodriguez, J.L.; Fons-Font, A. Mechanical Behavior of Provisional Implant Prosthetic Abutments. Med. Oral Patol. Oral Cir. Buccal 2015, 20, e94–e102. [Google Scholar] [CrossRef]
- Azer, S.S. A Simplified Technique for Creating a Customized Gingival Emergence Profile for Implant-Supported Crowns. J. Prosthodont. 2010, 19, 497–501. [Google Scholar] [CrossRef]
- Andersson, B.; Taylor, Å.; Lang, B.R.; Scheller, H.; Schärer, P.; Sorensen, J.A.; Tarnow, D. Alumina ceramic implant abutments used for single-tooth replacement: A prospective 1- to 3-year multicenter study. Int. J. Prosthodont. 2001, 14, 432. [Google Scholar] [PubMed]
- Iliev, G.; Filtchev, D.; Trifković, B.; Jevremović, D.; Pavlova, Z.; Slavkov, S.; Stoeva, D. Mechanical Resistance of Different Implant Suprastructures: A Laboratory Study. Appl. Sci. 2023, 13, 6100. [Google Scholar] [CrossRef]
- Stoeva, D.; Filtchev, D.; Nikolova, N.; Pavlova, Z.; Slavkov, S.; Iliev, G. Clinical Evaluation of Implant Suprastructures Depending on the Biomechanical Characteristics of the Materials Used. Appl. Sci. 2022, 12, 8659. [Google Scholar] [CrossRef]
- Khamis, M.M. Prosthetic Role in Peri-Implant Soft Tissue Management: Treatment Planning Phase. In Peri-Implant Soft Tissue Management: A Clinical Guide; Springer International Publishing: Cham, Switzerland, 2024. [Google Scholar] [CrossRef]
- Elsayed, A.; Wille, S.; Al-Akhali, M.; Kern, M. Comparison of fracture strength and failure mode of different ceramic implant abutments. J. Prosthet. Dent. 2017, 117, 499–506. [Google Scholar] [CrossRef]
- Albakry, M.; Guazzato, M.; Swain, M.V. Biaxial flexural strength, elastic moduli, and x-ray diffraction characterization of three pressable allceramic materials. J. Prosthet. Dent 2003, 89, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Holst, S.; Blatz, M.B.; Hegenbarth, E.; Wichmann, M.; Eitner, S. Prosthodontic considerations for predictable single-implant esthetics in the anterior maxilla. J. Oral Maxillofac. Surg. 2005, 63, 89–96. [Google Scholar] [CrossRef]
- Lee, S.J.; Betensky, R.A.; Gianneschi, G.E.; Gallucci, G.O. Accuracy of digital versus conventional implant impressions. Clin. Oral Implant. Res. 2015, 26, 715–719. [Google Scholar] [CrossRef]
- De Kok, P.; Kleverlaan, C.J.; de Jager, N.; Kuijs, R.; Feilzer, A.J. Mechanical performance of implant-supported posterior crowns. J. Prosthet. Dent. 2015, 114, 59–66. [Google Scholar] [CrossRef]
- Sadowsky, S.J. Occlusal overload with dental implants: A review. Int. J. Implant. Dent. 2019, 5, 29. [Google Scholar] [CrossRef]
- Loi, I.; Di Felice, A. Biologically oriented preparation technique (BOPT): A new approach for prosthetic restoration of periodontically healthy teeth. Eur. J. Esthet. Dent. 2013, 8, 10–23. [Google Scholar]
- Elsayed, A.; Wille, S.; Al-Akhali, M.; Kern, M. Effect of fatigue loading on the fracture strength and failure mode of lithium disilicate and zirconia implant abutments. Clin. Oral Implant. Res. 2018, 29, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Verdugo, C.L.; Núñez, G.J.; Avila, A.A.; Martín, C.L.S. Microleakage of the prosthetic abutment/implant interface with internal and external connection: In vitro study. Clin. Oral Implant. Res. 2014, 25, 1078–1083. [Google Scholar] [CrossRef]
- Schultheis, S.; Strub, J.R.; Gerds, T.A.; Guess, P.C. Monolithic and bi-layer CAD/CAM lithium–disilicate versus metal–ceramic fixed dental prostheses: Comparison of fracture loads and failure modes after fatigue. Clin. Oral Investig. 2013, 17, 1407–1413. [Google Scholar] [CrossRef] [PubMed]
- Dogan, D.O.; Gorler, O.; Mutaf, B.; Ozcan, M.; Eyuboglu, G.B.; Ulgey, M. Fracture Resistance of Molar Crowns Fabricated with Monolithic All-Ceramic CAD/CAM Materials Cemented on Titanium Abutments: An In Vitro Study. J. Prosthodont. 2015, 26, 309–314. [Google Scholar] [CrossRef] [PubMed]
- SD Mechatronik. A Guide Through the SD Mechatronik Chewing Simulator; SD Mechatronik: Feldkirchen-Westerham, Germany, 2017. [Google Scholar]
- Burke, F.J. Fracture resistance of teeth restored with dentin-bonded crowns: The effect of increased tooth preparation. Quintessence Int. 1996, 27, 115–121. [Google Scholar]
- García-González, M.; González-González, I.; García-García, I.; Blasón-González, S.; Lamela-Rey, M.J.; Fernández-Canteli, A.; Álvarez-Arenal, Á. Effect of abutment finish lines on the mechanical behavior and marginal fit of screw-retained implant crowns: An in vitro study. J. Prosthet. Dent. 2022, 127, 318.e1–318.e10. [Google Scholar] [CrossRef]
- Nouh, I.; Kern, M.; Sabet, A.E.; AboelFadl, A.K.; Hamdy, A.M.; Chaar, M.S. Mechanical behavior of posterior all-ceramic hybrid abutment-crowns versus hybrid-abutments with separate crowns-A laboratory study. Clin. Oral Implant. Res. 2019, 30, 90–98. [Google Scholar] [CrossRef]
- Alessandretti, R.; Borba, M.; Della Bona, A. Cyclic contact fatigue resistance of ceramics for monolithic and multilayer dental restorations. Dent. Mater. 2020, 36, 535–541. [Google Scholar] [CrossRef]
- Elshiyab, S.H.; Nawafleh, N.; Öchsner, A.; George, R. Fracture resistance of implant- supported monolithic crowns cemented to zirconia hybrid-abutments: Zirconia-based crowns vs. lithium disilicate crowns. J. Adv. Prosthodont. 2018, 10, 65–72. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Bonfante, E.A.; Vollmer, F.; Gierthmuehlen, P.C. Failure Load of Monolithic Lithium Disilicate Implant-Supported Single Crowns Bonded to Ti-base Abutments versus to Customized Ceramic Abutments after Fatigue. J. Prosthodont. 2022, 31, 136–146. [Google Scholar] [CrossRef]
- Preis, V.; Behr, M.; Rosentritt, M. In Vitro Fatigue and Fracture Testing of Implant-Supported Anterior Ceramic Crowns. Int. J. Prosthodont. 2018, 31, 264–266. [Google Scholar] [CrossRef] [PubMed]
- Cocchetto, R.; Canullo, L. The “hybrid abutment”: A new design for implant cemented restorations in the esthetic zones. Int. J. Esthet. Dent. 2015, 10, 186–208. [Google Scholar] [PubMed]
- Kasem, A.T.; Sakrana, A.A.; Ellayeh, M.; Özcan, M. Evaluation of zirconia and zirconia-reinforced glass ceramic systems fabricated for minimal invasive preparations using a novel standardization method. J. Esthet. Restor. Dent. 2020, 32, 560–568. [Google Scholar] [CrossRef] [PubMed]

| Materials | Study Groups |
|---|---|
| Titanium Alloy Blanks GenTek™ Pre-Milled Abutment Blank (Zimmer Biomet, Warsaw, IN, USA), grade 5 titanium | A, B, C, D |
| Zirconium Dioxide Katana (Kuraray Noritake, Tokyo, Japan) | A, C |
| Lithium Disilicate IPS e.max CAD (IvoclarVivadent, Schaan, Liechtenstein) | B, D |
| Observed Criteria | |||||
|---|---|---|---|---|---|
| Groups | Deformation of the Connecting Screw | Deformation of the Abutment | Presence of a Fracture Line or Crack in the Monolithic Crown | Failure of the Adhesive Bond Between the Monolithic Crown and the Abutment | Destruction of Either the Monolithic Crown or the Titanium Abutment |
| A | 0 | 0 | 15 | 15 | 15 |
| B | 0 | 0 | 15 | 15 | 15 |
| C | 0 | 0 | 15 | 15 | 15 |
| D | 0 | 0 | 15 | 15 | 15 |
| Source of Variation | SS | df | MS | F | p-Value | F Crit |
|---|---|---|---|---|---|---|
| Between groups | 49,008,821 | 3 | 16,336,274 | 24.597 | 0.000 | 2.769 |
| Within groups | 37,192,186 | 56 | 664,146 | |||
| Total | 86,201,007 | 59 |
| Differences Between | Mean Difference | p-Value | 95% CI Lower | 95% CI Upper | |
|---|---|---|---|---|---|
| Group A | Group B | 1096.40 | 0.00 | 616.68 | 1576.12 |
| Group A | Group C | 1280.47 | 0.00 | 512.46 | 2048.47 |
| Group A | Group D | 2546.80 | 0.00 | 2026.79 | 3066.81 |
| Group B | Group C | 184.07 | 0.59 | −522.21 | 890.34 |
| Group B | Group D | 1450.40 | 0.00 | 1045.37 | 1855.43 |
| Group D | Group D | 1266.33 | 0.00 | 535.02 | 1997.64 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stoeva, D.; Mateeva, G.; Jevremovic, D.; Jevremović, A.; Trifkovic, B.; Filtchev, D. Mechanical Resistance of Implant-Supported Crowns with Abutments Exhibiting Different Margin Designs. Appl. Sci. 2025, 15, 5193. https://doi.org/10.3390/app15095193
Stoeva D, Mateeva G, Jevremovic D, Jevremović A, Trifkovic B, Filtchev D. Mechanical Resistance of Implant-Supported Crowns with Abutments Exhibiting Different Margin Designs. Applied Sciences. 2025; 15(9):5193. https://doi.org/10.3390/app15095193
Chicago/Turabian StyleStoeva, Daniela, Galena Mateeva, Danimir Jevremovic, Ana Jevremović, Branka Trifkovic, and Dimitar Filtchev. 2025. "Mechanical Resistance of Implant-Supported Crowns with Abutments Exhibiting Different Margin Designs" Applied Sciences 15, no. 9: 5193. https://doi.org/10.3390/app15095193
APA StyleStoeva, D., Mateeva, G., Jevremovic, D., Jevremović, A., Trifkovic, B., & Filtchev, D. (2025). Mechanical Resistance of Implant-Supported Crowns with Abutments Exhibiting Different Margin Designs. Applied Sciences, 15(9), 5193. https://doi.org/10.3390/app15095193







