Abstract
Endermologie is a non-invasive mechanical massage technique that combines suction, mechanized rollers and/or flaps, and mechanotransduction principles to stimulate the skin and subcutaneous tissues. This review assessed endermologie’s therapeutic indications and physiological effects. A comprehensive literature search was conducted using EDS DB (Med Univ) and PubMed to identify relevant studies published between 2000 and February 2025. Two authors independently screened studies, resulting in 24 articles included in the qualitative synthesis. Key applications identified included for burns, scars, muscle regeneration, lymphedema, cellulite, panniculitis/lipoatrophy, skin elasticity improvement, fat reduction, morphea, fibromyalgia, pre- and post-liposuction care, peri-oncology rehabilitation, orthopedics, and postoperative recovery. Research highlights the importance of treatment frequency, duration, and mechanostimulation parameters in determining therapeutic outcomes. Studies indicate that endermologie induces extracellular matrix remodeling, fibroblast activation, adipocyte fat release sensitivity, and enhanced venolymphatic circulation. Documented effects include improved microcirculation, anti-fibrotic properties, enhanced skin elasticity, fluid drainage, and pain relief, contributing to scar management, tissue softening, and post-surgical rehabilitation. Despite its potential, methodological heterogeneity across studies limits direct comparability, emphasizing the need for future research on standardization and long-term efficacy validation.
1. Introduction
In the 1970s, Louis-Paul Guitay (LPG) survived a motor vehicle accident that resulted in significant skin and muscle damage. The resulting scarring was treated with manual therapeutic massage; however, Guitay found this approach labor-intensive, time-consuming, and highly dependent on the therapist’s skill. In response, he developed a unique mechanostimulation device, the CelluM6, which delivers endermologie technology (LPG Systems, Valence, France). This device replicates the effects of manual massage, including compression, pinching, slurring, grazing, and rotation, with the goal of standardizing physical therapy. Initially, it was designed for the treatment of post-traumatic and burn scars.
The term endermologie (or endermotherapy) originates from two words: “ende”, meaning “under”, and “derm”, meaning “skin”. The primary objective of this innovation was to create a massage technique that was consistent, controlled, and repeatable, while also reducing the physical effort required from the practitioner. During its application in scar therapy, improvements in the aesthetic quality of the skin were observed. As a result, the method was later introduced for cosmetic purposes, primarily for cellulite reduction. Over time, its indications have expanded significantly, paralleling technological advancements such as additional settings (sequential modes, rhythmic frequency from 0.2 Hz to 30 Hz, minimum and maximum intensity control) and specialized treatment heads with rollers, flaps, or a combination of both [1,2,3], allowing infinity modes of tissue stimulation to adapt continuously to tissue state.
In English, this technique is described using various terms, including depressomassage, mechanical massage, mécano-stimulation, vacuum massage, endermotherapy, endermology, and suction massage. However, the term endermologie is exclusively associated with CelluM6 devices, which pioneered this technology.
Endermologie is believed to exert both local and systemic therapeutic effects, contributing to the metabolic recovery of tissues following trauma, surgery, or implantation. This natural method of skin mobilization is employed by professionals across multiple disciplines, including physiotherapists, osteopaths, phlebologists, aesthetic medicine doctors, cosmetologists, beauticians, dermatologists, and surgeons. It is particularly valued in pre- and post-liposuction care, as well as in the management of swelling and scar tissue [2].
The effects of mechanical forces on tissues trigger cellular responses, making endermologie a non-invasive and painless method for addressing conditions related to circulation, connective tissue, fat metabolism, and muscle tone. While the treatment is widely recognized for its aesthetic benefits, including cellulite reduction, adipose tissue remodeling, and anti-aging effects, its therapeutic applications are also gaining attention.
The purpose of this paper is to provide a narrative review of the available literature on endermologie, summarizing its medical, aesthetic, and rehabilitation applications. This review aims to synthesize current knowledge, highlight key findings from relevant studies, and discuss the potential mechanisms of action underlying endermologie’s effects. Additionally, it seeks to identify gaps in the existing research and propose directions for future studies in this field.
1.1. Mechanism of Action
Endermologie is a treatment technique based on mechanical stimulation of the skin and subcutaneous tissues using vacuum-assisted mobilization. The device used in this procedure generates negative pressure, which lifts a skin fold and subjects it to controlled mechanical stimulation through motorized rollers and/or flaps. This process, known as mechano-stimulation, triggers physiological responses within the connective tissue, influencing circulation, lymphatic drainage, and adipocyte and fibroblast activity. The treatment heads used in endermologie are designed to adjust to different treatment areas and therapeutic goals. The device allows for a large panel of treatment heads and the modulation of various parameters, including suction intensity, frequency, and movement direction, enabling customized treatments tailored to individual skin conditions and therapeutic needs. By altering these settings, practitioners can influence tissue mobilization depth; optimize treatment for conditions such as cellulite, skin laxity, fibrosis, post-surgical swelling, pain, and scar remodeling; and enhance both aesthetic and medical outcomes. Depending on the treatment mode, endermologie can be applied using continuous or sequential vacuum stimulation. The continuous vacuum is typically used for deep mobilization, supporting fat metabolism and fibrotic tissue remodeling [4,5].
The intermittent or sequential vacuum operates by rhythmically lifting and releasing the skin, which enhances microcirculation, lymphatic flow, and tissue oxygenation, making it particularly effective for reducing swelling, improving skin elasticity, and addressing cellulite. The versatility of endermologie lies in its ability to precisely control the depth and intensity of tissue mobilization, ensuring that treatments are adapted to specific indications, such as body contouring, post-operative rehabilitation, or skin rejuvenation. The parameters can be adjusted manually by the practitioner or set according to pre-programmed treatment protocols, optimizing both safety and efficacy [5,6].
1.2. Influence on the Skin
The treatment head used in endermologie initiates this process by stimulating the skin surface while simultaneously sending signals to dermal and subcutaneous cells. Cell activation relies on signal transduction, a fundamental biological process that converts external stimuli into intracellular responses. This mechanism is essential for intercellular communication and the regulation of cellular functions. When the external stimuli are mechanical forces, this process is referred to as mechanotransduction (Figure 1). In the context of endermologie, mechanical stimulation applied to the skin is transmitted through the epidermis, dermis, and subcutaneous tissues, influencing both cell–cell and cell–extracellular matrix (ECM) interactions. This mechanotransduction plays a crucial role in tissue remodeling, as connective tissue cells adapt their ECM composition in response to mechanical stress. Cells exposed to such forces modulate protein expression, leading to functional and structural changes that help the tissue meet new mechanical demands [7].
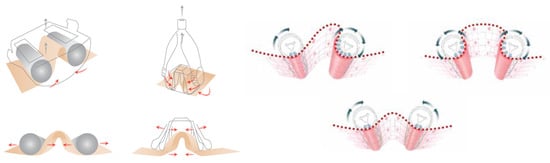
Figure 1.
Comparison of different mechanical tissue mobilization techniques used in aesthetic and therapeutic procedures. The illustrations depict variations in mechanical stimulation of the skin and subcutaneous tissues, highlighting different approaches to vacuum- and roller-based manipulation [8].
The receptors of various types of cells are stimulated and, as a result, their kinetic and functional activity is increased (Figure 2). When keratinocytes, fibroblasts, endothelial cells, and other skin cells are mechanically stimulated, they release growth factors or cytokines, which, in turn, influence all structural and morphological modifications of the skin [9].
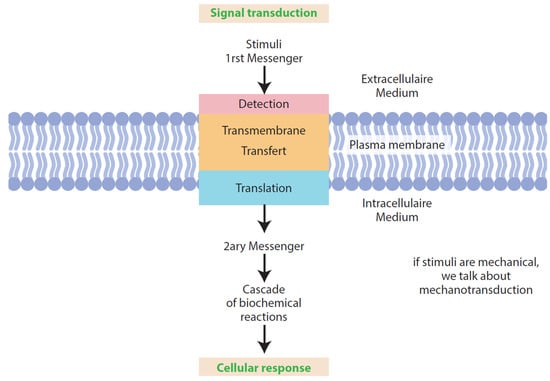
Figure 2.
Mechanotransduction pathway in cellular activation. External mechanical stimuli (first messengers) are detected at the cell membrane, initiating transmembrane signal transfer and intracellular translation. This leads to the generation of secondary messengers, which trigger a cascade of biochemical reactions, ultimately resulting in a specific cellular response. This process is fundamental to mechanotransduction, the mechanism by which mechanical forces influence cell behavior and extracellular matrix remodeling.
Under the influence of mechanical stimuli, i.e., mechanotransduction (Figure 3), numerous skin processes are activated, processes by which cells perceive mechanical stimuli and respond to them by converting them into biochemical signals. Studies prove that the mechanical stress of epithelial cells activates the transcription factors YAP1 and β-catenin and causes cell cycle triggering. Moreover, transcriptional activity is important for cell cycle rebirth and progression [4]. YAP1 regulates gene expression in response to mechanical tension through the Hippo pathway. β-catenin modulates cellular responses via the Wnt pathway, cooperating with YAP1. Both pathways influence tissue regeneration, fibroblast proliferation, and ECM remodeling, which are crucial in mechanical therapies such as endermologie [10].
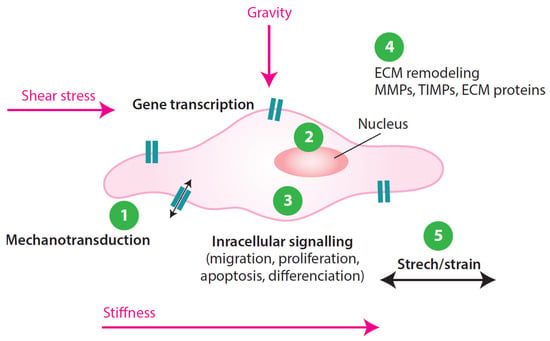
Figure 3.
Mechanotransduction and cellular response to mechanical stimuli. External mechanical forces (shear stress, gravity, stiffness, stretch/strain) activate mechanoreceptors on the cell surface, triggering intracellular signaling pathways. This leads to gene transcription, affecting cellular behaviors such as proliferation, migration, apoptosis, and differentiation. Additionally, mechanotransduction influences extracellular matrix (ECM) remodeling, contributing to tissue restructuring and adaptation to mechanical stress. 1. Mechanotransduction; 2. Gene transcription; 3. Intracellular signalling; 4. ECM remodelling; 5. Strech/strain.
The mechanotransduction activates the specific receptors for free substances such as histamine, bradykinin, serotonin, and catecholamines, which act on beta-adrenergic receptors and activate adenyl cyclase and AMP. Then, protein kinase activates intra-adipocyte lipase to lipolysis. The mechanical simulations act on the mechanoreceptors such as the corpuscles of Meissner (touch corpuscles are tactile receptors responsible for feeling light, superficial, vibrational sensations), corpuscles of Water–Pacini (sensitive to deep pressure, localized in the deep dermis and subcutaneous tissue), corpuscles of the Golgi (sensitive to the pressures, provoke revascularization and the restructuring of connective tissue), and the corpuscles of Merkel (situated in the epidermis, sensitive to pressure and vibration; they act on cellular metabolic activity). Most of these mechanoreceptors stimulate the activity of the fibroblasts and the regeneration of collagen and connective tissue [2].
Research shows changes in the number and surface of fibroblasts, blood vessels, the thickness of the epidermis (basal to granular layer), and the area of the dermal–epidermal junction. At the level of the epidermis, mechanical stretching causes DNA synthesis and keratinocyte proliferation [9,11].
The reconstruction of connective tissue (increasing the number of fibroblasts) and a decrease in the interstitial space of the skin result from the remodeling of collagen and its reorientation [11]. After mechanostimulation, fibroblasts proliferate by increasing DNA synthesis and changing their phenotype (Figure 4). The release of growth factors induced by mechanical forces is associated with the remodeling of the extracellular matrix, in particular, type I, III, IV, and XII collagen and fibronectin [9].
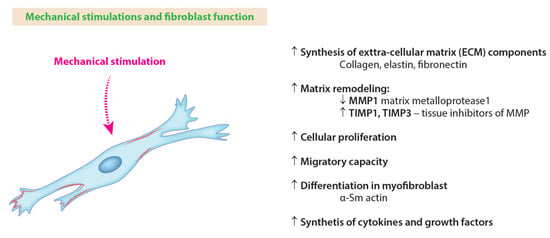
Figure 4.
The impact of mechanical stimulation on fibroblast function.
Mechanical stimulation (MS) influences fibroblast activity, leading to the increased synthesis of extracellular matrix (ECM) components such as collagen, elastin, and fibronectin, which contribute to tissue integrity and elasticity. MS also plays a crucial role in matrix remodeling, regulating the activity of matrix metalloproteases (MMPs) and their inhibitors (TIMPs) to maintain ECM homeostasis. Additionally, mechanical cues stimulate cellular proliferation, migration, and differentiation into myofibroblasts, which are essential for tissue repair and wound healing. These processes are accompanied by the enhanced synthesis of cytokines and growth factors, further supporting fibroblast-mediated tissue remodeling and regeneration.
The main purpose of the procedure is to stimulate blood and lymph circulation, which accelerates metabolism and facilitates the removal of unnecessary metabolic byproducts. This, in turn, promotes further processes such as lipolysis stimulation, swelling resorption, and collagen and elastin production in the skin and subcutaneous tissue. Vacuum kneading makes it easier to replace the fluid between the cell and extracellular space and their discharge. This also promotes the removal of proteins that cause water retention. Additionally, the negative pressure from suction and the positive pressure from rolling cause an improvement in the distribution of subcutaneous fat [11]. As described by Shoham, the dynamic mechanical forces applied by Endermologie could lead to the inhibition of adipogenesis (Figure 5) and the subsequent reduction in adipose tissue.
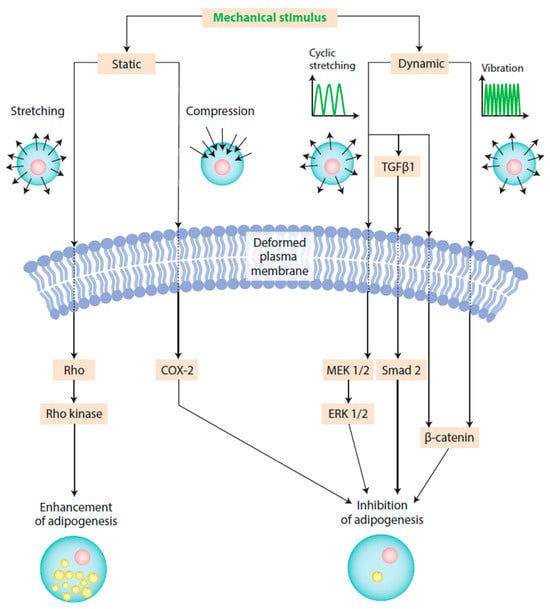
Figure 5.
Effects of mechanical stimulation on adipocytes and adipogenesis. Source: [12].
Mechanical stimulation can influence adipogenesis—the transformation of pre-adipocytes into mature adipocytes—either by promoting or inhibiting the process, depending on the type of mechanical force applied. Static stimuli, such as stretching and compression, activate signaling pathways involving Rho kinase and COX-2, which are associated with the enhancement of adipogenesis. In contrast, dynamic mechanical forces, including cyclic stretching and vibration, stimulate pathways mediated by TGF-β1, MEK 1/2, ERK 1/2, Smad 2, and β-catenin, leading to the inhibition of adipogenesis. These mechanical signals deform the plasma membrane and trigger intracellular responses that regulate fat cell differentiation, metabolism, and tissue remodeling.
Moreover, endermologie has been recognized for its beneficial effects on lymphedema management. Moseley et al. compared endermologie with manual lymphatic drainage and showed that both MLD and endermologie plus compression bandaging applied over a minimum of two weeks (but preferably four weeks) were beneficial for the treatment of secondary arm lymphoedemam with endermologie having a 33% shorter treatment time than MLD [13,14]. Malloizel-Delaunay et al. validated a reproductive endermologie protocol dedicated to upper limb lymphedema secondary to breast cancer. It could be proposed as a maintenance treatment for lymphedema, but only for patients who do not have fragile skin. It can be used by all physiotherapists, thus reducing variations between manual lymphatic drainage practitioners [15]. This effect is likely due to the enhanced lymphatic flow facilitated by mechanical stimulation. Supporting this, a study by Ahmed indicated that endermologie not only decreases limb volume but also improves range of motion (including flexion and abduction) while reducing pain levels [16]. Consequently, endermologie contributes not only to the reduction of lymphedema-related limb size but also to an overall improvement in patients’ quality of life. Additionally, a study by Moortgat et al. analyzed the physiological impact of vacuum therapy on various skin layers, including the epidermis and dermis. The findings revealed that vacuum therapy increases tissue strength and skin elasticity by stimulating fibroblast proliferation and collagen synthesis. These effects not only enhance skin quality but also contribute to better lymphatic drainage, which may explain its effectiveness in lymphedema treatment [3].
In research on scars, it was found that the apoptosis of myofibroblasts may occur, which reduces the cohesion of scars. A beneficial effect on the layers of the epidermis was also demonstrated, i.e., the thickening of the epidermis (expansion of the layers of the live epidermis) and an increase in the adhesion of the dermis to the epidermis under the influence of an increase in the surface of the skin’s native limit (increase in the number of warts (dermal papilla) and epidermal ridge). The exfoliating effects of the epidermis and the effect on the sebaceous glands, resulting in the adjustment of the lubrication and hydration of the skin, were also mentioned [2,17].
Mechanical stimulation affects the vascular bearing of the skin and also increases microcirculation parameters. The action of rollers and flaps, combined with suction, favors effective tissue and lymphatic drainage. Treatment has an effect on the activation of neovascularization and angiogenic processes. This occurs as a result of arterial tension, which affects the walls of the vascular endothelium, determining the release of vascular endothelial growth factors (VEGFs) and the proliferation and migration of cells responsible for angiogenesis. This is evidenced primarily by the greater number of vascular structures in the superficial vascular plexus. Data from videocapillaroscopic measurements indicate increased capillary blood flow rate values and an increase in capillary density. Mechanical stimulation increases microcirculation, vascularity, skin oxygenation, and, hence, skin oxygenation, cellular exchange, and nutrition [9,18].
The superficial fascia is responsible for numerous aesthetic alterations of the skin surface. It is a kind of net that is formed from horizontal septa of collagen and elastic fibers separated by fat lobules crossed vertically by fibers that organize the superficial adipose tissue. The superficial fascia is considered a systemic bandage. The elevations and depressions of the contour of the body are connected with the fascia and its relationships with muscles, fat, and skin. Endermologie is essentially the traction and stretching (activation) of the superficial band and the superficial muscular fascia [2].
It can be stated that endermologie works on the following levels: activation of the arteriolar microcirculation, metabolic activation, lymph drainage, traction and mobilization of the connective tissue, and neurotic regulation [2]. Regular, high-frequency skin pinching can be understood as so-called skin and muscle gymnastics. This affects the stimulation of blood and lymph flow [6,9], the reconstruction of the dermis (the stimulation of fibroblasts) [5,9,11], and the relaxation of incorrectly tight muscles [5,6]. To sum up, endermologie acts on the connective tissue, subcutaneous tissue, muscles, and venous and lymphatic circulation [5,6,9,17].
2. Methods
A comprehensive literature search was conducted across two major electronic databases, EDS DB (Med. Univ.) and PubMed, to identify relevant studies on the effects of endermologie. The search covered publications up to February 2025, ensuring the inclusion of the most recent research. The search strategy incorporated a combination of MeSH terms and free-text keywords, including “endermologie”, “endermology”, “mechanical massage”, and “mechanotherapy”.
To ensure the selection of high-quality and relevant studies, predefined inclusion and exclusion criteria were applied.
2.1. Inclusion Criteria
Original research articles, clinical trials, and systematic reviews that investigated endermologie’s effects in medical, aesthetic, or rehabilitation contexts. Studies published in English or French between 2000 and 2025. Research with a clear methodology, describing the mechanisms of action, efficacy, or physiological effects of endermologie. Studies published in academic journals and peer-reviewed review articles.
2.2. Exclusion Criteria
Non-peer-reviewed articles, editorials, conference abstracts, or case reports lacking rigorous methodology. Studies focusing solely on general massage techniques without specific reference to endermologie or related vacuum-based mechanostimulation. Research without clear outcome measures or with significant methodological limitations. Publications categorized as eBooks, news articles, trade publications, books, and conference materials, as these do not meet the standards of peer-reviewed scientific literature.
2.3. Screening Process
The literature search and study selection process were carefully conducted to ensure a systematic and objective approach. After removing duplicates, an initial screening was performed based on titles and abstracts to eliminate studies that did not meet the inclusion criteria. The full texts of potentially eligible articles were then retrieved and reviewed for final inclusion.
A total of 463 studies were initially identified. After applying the selection criteria and removing duplicates, 42 articles were assessed for eligibility. Finally, 24 studies were included in the qualitative synthesis (Table 1).

Table 1.
Endermology research analysis.
2.4. Data Extraction and Quality Assessment
Key information extracted from each study included sample size, methodology, study design, intervention details, outcome measures, and main findings. Although PRISMA guidelines were not followed, the included studies were chosen based on their relevance and methodological clarity. The selected studies were categorized based on their findings related to specific medical, aesthetic, or rehabilitation applications of endermologie.
3. Results
Endermologie was initially developed to standardize and enhance the effectiveness of treatment for burns, scars, and muscle regeneration. The mobilization of tissues was found to improve fibrosis reduction, edema resorption, adhesion breakdown, tissue elasticity, oxygenation, and trophism. Studies have also highlighted its role in the treatment of hypertrophic burn scars [19].
Endermologie has applications in peripheral lymphedema and secondary arm lymphedema, as well as cancer-related lymphedema treatment, edema management, and lymphatic drainage [13,15,22,28,38]. Findings suggest that endermologie not only reduces edema but also improves quality of life in individuals with lymphatic dysfunction.
Authors conducted studies assessing the effects of endermologie on radiation-induced skin fibrosis. The results indicated that mechanical stimulation through this technique improves skin elasticity and reduces fibrotic changes, providing a promising, non-invasive approach for managing post-radiotherapy complications. Moreover, the therapy has been applied for mastectomy scars and skin trophicity improvement during breast reconstruction with lipofilling [1,20,21,31], further demonstrating its benefits in post-cancer recovery and tissue regeneration. Authors emphasized its role as a non-invasive approach for tissue rehabilitation by influencing post-traumatic, postoperative, and post-implantation recovery.
Endermologie is widely recognized as a non-invasive method for body contouring and cellulite reduction. Vacuum massage has been shown to alter the structural and physiological properties of the skin, leading to improved skin firmness and elasticity. Additionally, it has demonstrated benefits in lipid mobilization, body fat reduction, and cellulite management [24,26,29,30,35,37]. The technique has also been explored for its effectiveness in lipodystrophy [9] and panniculitis/lipoatrophy [23,25,27], broadening its range of applications in metabolic and adipose tissue disorders.
Preoperative and postoperative applications of endermologie have been reported to be beneficial in liposuction procedures. Additionally, its role in postoperative ileus following colectomy has been explored, indicating potential benefits in the treatment of pain and accelerating gastrointestinal recovery [36].
Endermologie has demonstrated therapeutic potential in fibromyalgia management [32], where it aids in pain reduction and tissue relaxation. It has also been investigated as a treatment for Mondor’s disease [33], morphea [34], and other conditions affecting connective tissue health.
4. Discussion
Endermologie is a versatile treatment that is utilized in the medical and aesthetic treatment of numerous skin disorders. It is often used to strengthen, complement, prepare, and support surgical or other medical or aesthetic procedures. Endermologie stimulates microcirculation, drains fluid flow, and accelerates revascularization. This reduces edema, cellulite, and other dysfunctional changes in subcutaneous tissue [3,14,24,29,39,40]. Treatments favor dermal remodeling, enhance skin elasticity, and reduce fibrosis and scarring [5,6,21,31]. Moreover, the treatment affects muscle recovery [22].
Many studies have been conducted on endermologie and reveal extracellular matrix remodeling that can be interpreted as a cell activation process: fibroblasts acquire a “secretory” phenotype, adipocytes become more sensitive to fat release, and venolymphatic circulation improves [5,26,30]. Endermologie has documented circulatory, trophic, and anti-fibrosis properties and can be used to improve the integrity of the integumentary system, treat most types of scars, stimulate circulation, drain fluids, soften tissue, improve fibrosis and adhesions, relieve pain, and improve range of motion [3,6,14,31,32,39].
Despite the heterogeneous population and the wide diversity of designs used in studies, global results showed that endermologie has beneficial effects on the integumentary system and can be used in medical therapy, surgery, and aesthetic procedures as a holistic integrative treatment to help optimize the scarring process and final aesthetic and functional outcome [6,28,34]; prevent, reduce, or manage complications after surgery [15,19,21,31]; and improve therapeutic care, satisfaction, and quality of life [3,32,39]. The role of therapists is of paramount importance.
4.1. Cellulite
Cellulite is a nodular, edematous, and fibrotic degeneration of adipose tissue (female-type lipodystrophy). This degeneration is closely related to blood and lymph microcirculation dysfunctions, as well as adipose tissue metabolism. There is dystrophy and hypertrophy of the adipocyte structure and enlargement and thickening of the vascular endothelium leading to microangiopathy and increased fibrosis of the interdigitating septae. Noticeably, there may be a blurring of the border between the underlying tissue and the skin. Since there are several types of cellulite (adipose, fibrous, interstitial, edematous, and pseudo-cellulite), endermologie treatments can be tailored individually depending on the coexisting skin problems. Endermologie is a US FDA-approved treatment for the treatment of cellulite [40] and the improvement of lymphatic circulation.
The treatment works on all the most important dysfunctions associated with cellulite. Mechanical massage activates lipolysis; decompartmentalizes fatty tissues; acts on the septa; stimulates adipocytes through the action on ß receptors, provoking the release of fat cells; and stimulates fibroblasts and drainage [26,40]. The examination of tissues (porcine skin) revealed changes in architecture and showed the accumulation of new, dense, thick, and longitudinal collagen bands in the subdermal tissue layer. There was also some distortion and disruption of the adipocyte cell membrane. The redistribution of the vertical tethering force vector via collagen bands running parallel to the skin surface, coupled with the tearing of vertical bands, may account for the skin smoothing effect and the appearance of decreased cellulite after endermologie treatments. These changes were proportional to the number of treatments performed [2,24,29]. The studies also point to effects depending on the duration of therapy, the number of treatments, and the maintenance treatments performed after the main series of treatments. The continuation of anti-cellulite treatments in the amount of two treatments per month gives the best results. Simple quantitative effects were also demonstrated, such as reductions in body circumference, skin fold thickness, the length of the dermis-hypodermis interface (ultrasound analysis at 20 MHz), and the area of cellulite depressions (skin imprints) [35].
4.2. Fat Reduction
Subcutaneous gluteofemoral adipose tissue (GAT) adipocytes are less metabolically reactive than visceral adipose tissue adipocytes. Moreover, in GAT, fat cell hypertrophy, less blood flow, and reactiveness to hormones are observed. Mechanical massage exerts circulatory and dermotrophic effects and has been shown to reduce skin fold measurements and body circumferences. Mechanical massage shows a number of impacts on the expression of genes involved in metabolic pathways. It promotes improvements in adipose tissue biology, including enhanced lipolytic responsiveness and adipose tissue blood flow. A higher lipolytic efficiency occurs in adipose tissue if treatment is associated with physical activity training because training enhances both non-esterified fatty acid mobilization from adipose tissue and their oxidation by the skeletal muscle [26]. The microdialysis technique was used to assess the lipolytic responsiveness of femoral adipose tissue after mechanical massage. The treatment sessions improved the lipid mobilizing effects [30].
4.3. Panniculitis/Lipoatrophy
Lipoatrophy is a localized loss of subcutaneous adipose tissue without significant inflammation. It is a common reaction at injection sites. Endermologie treats panniculitis/lipoatrophy associated with the long-term administration of glatiramer acetate in patients with multiple sclerosis RRMS. Endermologie sessions achieved complete recovery from indurations and improved skin conditions [23]. Mechanical massage was also reported to enhance tolerance to glatiramer acetate administration in patients with decreased cutaneous reactions [25]. Endermologie can help patients resolve injection-site reactions to GA (erythema, inflammation, pain, and pruritus) and continue immunomodulatory treatment. Treatment sessions were well tolerated without pain [27,41].
4.4. Scars
Manual massage therapy is commonly used to improve scar pliability, reduce adhesions, and enhance tissue mobility. However, its effectiveness is inconsistent due to variations in therapist technique, applied force, and individual patient response. Additionally, manual application can lead to therapist fatigue, limiting the intensity and duration of treatment. Mechanized vacuum massage offers a standardized alternative by delivering controlled, reproducible mechanical force through motorized rollers/flaps and suction. This ensures consistent tissue mobilization, lymphatic drainage, and collagen remodeling, addressing the limitations of manual therapy. By reducing therapist-dependent variability, mechanized massage may provide more uniform scar treatment outcomes while minimizing operator strain. Further research is needed to fully establish its role in optimizing scar remodeling (Figure 6) and functional recovery. Preclinical studies indicate that mechanized massage may aid in collagen realignment, fibroblast activity modulation, and the enhancement of skin elasticity; however, its specific impact on hypertrophic scar remodeling, especially for post-burn injuries, remains insufficiently investigated [42].
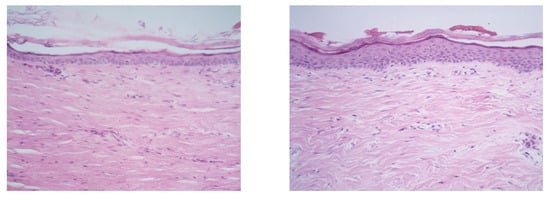
Figure 6.
The histological images represent cicatricial tissue modifications in the xypho-pubic area before and after 10 sessions of endermologie treatment. The study conducted by Petricig et al. (2000) [43] demonstrated significant changes in skin structure following mechanical stimulation. Before treatment (left image): The epidermis appeared thinner, with a lower density of the papillary dermis and less organized collagen fibers in the dermal layer. After 10 sessions (right image): A notable increase in epidermal thickness was observed, along with a higher density of the papillary dermis, suggesting improved skin regeneration and restructuring. The dermal layer exhibited better collagen organization, indicating enhanced skin elasticity and strength. Source: [43].
Scarred tissue mechanostimulation techniques have been used in rehabilitation medicine, physiotherapy, cosmetology, reconstructive and aesthetic plastic surgery, and aesthetic medicine. Studies showed the validity of endermologie to treat scars (post-traumatic scars, surgical scars) and burns, an improvement in subjective symptoms like paresthesia and pain, and an improvement in scar appearance. The new generation of hand pieces (pulsed stimulation and flap) depend less on the operator, allow for early treatment, and enable faster and more predictable results than those that are obtained from previous-generation equipment [6].
De la Cruz M. explored the use of endermologie (LPG® Cellu M6) as a novel approach in delayed breast reconstruction following mastectomy. The study demonstrated that external skin expansion using endermologie effectively increases skin elasticity, reduces scar tissue stiffness, and enhances the pliability of irradiated and non-irradiated mastectomy sites. This technique, based on mechanical stimulation, facilitates the reconstruction process by eliminating inextensible scar tissue between the pectoralis major fascia and subcutaneous tissue, ultimately allowing for breast augmentation with anatomical implants without the need for additional donor site morbidity [1].
Leung A. et al. showed that adding mechanical stimulation to conventional physiotherapy for women who have undergone mastectomy for breast cancer was safe and produced additional benefits in the form of improvements in scar vascularity and pliability, arm function, and functional well-being compared with conventional scar treatment. The benefits persisted for at least three months after completing the treatment. No significant impact was observed on pain, range of motion, or grip strength. Mechanical therapy is safe and can serve as a complementary approach to conventional rehabilitation. Further research is needed to optimize stimulation parameters and assess long-term effects [20].
Post-mastectomy irradiation (radiation therapy) severely impairs skin trophicity, decreases epithelial tissue thickness, inhibits the regenerative ability of the skin, and worsens blood circulation in dermal tissue, resulting in a poor outcome with a prosthetic implant. The procedure of autologous fat grafting, commonly known as lipofilling, enhances the skin’s quality, enabling a minimally invasive approach to prosthetic reconstruction. The thoracic wall skin of the receiving site was prepared 15 days before the second and consecutive fat transfers using endermologie [44]. The results of preoperative and postoperative skin mechanotherapy (endermologie) demonstrated a rise in skin compliance for lipofilling, which was correlated with a lower prosthesis volume and a higher volume of fat injection. The control group of patients without endermologie treatment displayed signs of low skin trophicity, such as thin skin, vessel dilatation, and capsular retraction. As confirmed by a prospective study, mechanotherapy has the potential to become a standard in patients’ preparation for lipofilling-based reconstruction [21,44,45].
4.5. Skin Fibrosis
Cutaneous, superficial radiation-induced fibrosis induces more or less important functional discomfort, clinically seen as changes in skin texture and skin retraction. The skin is dry, scaly, stiff, and less supple with telangiectasia, pain, and itching. Endermologie allows skin mobilization by unfolding/folding. Studies showed improvement in the clinical signs associated with skin dysfunctions after radiotherapy. Clinically, the LPG treatment induced a decrease in the feeling of induration of the skin, a skin-softening sensation, and a decrease in erythema, pain, and pruritus. There was an increase in the average roughness of the skin, which corresponded to a softening of the skin and an increase in the skin’s ability to retract and stretch. The treated skin had more uniform contours and less difference between the visible wrinkles in terms of “altitude”. The LPG technique seems to improve suppleness and skin microrelief but also reduces the induration of irradiated breasts. The treatment protocol for radiation-induced fibrosis should include an “attack” phase (phase one) with about three sessions per week (15 treatments) and a maintenance phase of at least one session per month. Moreover, mechanical massage was effective on irradiated skin in a qualitative study (clinical), leading to better comfort for patients [31].
4.6. Lymphedema, Drainage, and Phebolymphology
As a result of endermologie treatments, specific tissue drainage occurs. This may be the result of metabolic stimulation and the activation of the autonomous nervous system. This treatment works on the principle of physical decongestion while improving extracellular fluid and lymphatic drainage. Endermologie in combination with intensive decongestive treatment improves upper limb volume reduction compared with the standard of care for breast cancer lymphedema. After treatments, there was a reduction in excess fluid volume in the upper limb. The effect also improved patient psychological and social well-being [15]. The LPG technique combined with compression bandaging improved the subjective symptoms of lymphedema. Treatments resulted in a reduction in arm volume and arm and truncated fluid and a softening in lymphatic territories [13]. Studies using endermologie have shown that it improves lymphatic transport capacity and superficial lymphatic drainage and decreases fibrotic tightness, induration, heaviness, and functional discomfort [38].
Malloizel-Delaunay J et al., in their ELOCS Phase II, randomized, controlled trial, investigated a new approach to breast cancer-related lymphedema (BCRL) treatment by incorporating endermologie alongside standard intensive decongestive therapy (IDT). The study compared three groups: IDT alone, IDT with manual lymphatic drainage (MLD) and endermologie, and IDT with endermologie only over a 5-day period. Although the predefined success threshold (≥30% volume reduction in at least 21/31 patients) was not met, endermologie showed comparable effectiveness to conventional therapy, with mean limb volume reductions of 38% (IDT), 33% (IDT + MLD + endermologie), and 34% (IDT + endermologie). The success rate was highest in the IDT + endermologie group (64.5%), suggesting that mechanical stimulation can be a valuable adjunct in BCRL management. However, 16% of patients reported pain and 15% found the treatment unpleasant, highlighting the need for further optimization. Despite these limitations, the study validated a standardized and reproducible endermologie protocol, supporting its potential role in lymphedema care [15].
Findings supporting the use of endermologie suggest that this therapy may enhance lymphatic flow, leading to a reduction in limb volume. Moortgat et al. analyzed the physiological effects of vacuum therapy on the skin, demonstrating an increase in fibroblast and collagen production as well as improved tissue elasticity, which promotes lymphatic drainage [3]. Ahmed’s study showed that endermologie can improve range of motion (e.g., flexion, abduction), reduce pain, and decrease limb volume, ultimately enhancing patients’ quality of life. Ahmed et al. evaluated the efficacy of endermologie vs. decongestive lymphatic therapy (DLT) in reducing post-mastectomy lymphedema and pain and improving shoulder mobility. Forty women (30–50 years) with unilateral post-mastectomy lymphedema were randomized into an endermologie group (n = 20), DLT group (n = 20), and endermologie group with 4 sessions/week for 4 weeks. There was a greater reduction in limb volume and pain and improved ROM in the endermologie group (p < 0.001). A comparison of endermologie with low-level laser therapy in Ahmed’s study revealed no significant differences in lymphedema reduction at the start of therapy. However, by the end of treatment, endermologie resulted in more substantial changes in arm volume and circumference compared to laser therapy. This discrepancy in findings highlights the need for further research to understand the mechanisms and long-term efficacy of this method [16].
4.7. Skin Elasticity and Aging
Studies have shown the influence of mechanical forces on fibroblasts through the conversion of mechanical signals into biochemical responses (mechanotransduction). The results of in vitro studies indicated increases in type I collagen, elastin, hyaluronic acid, and MMP9 content along with an improvement of the migratory capacity of the fibroblasts after a series of mécano-stimulation (24 sessions). Evaluation using electron microscopy showed a dermal remodeling in relation to the activation of fibroblast activity. The results of the skin biopsy correlated with the clinical evaluation of the therapy’s effects. Superficial mechanical stimulation sends a signal to the fibroblasts, keratinocytes, and adipocytes, which then results in the production of collagen, elastin, and hyaluronic acid and the activation of lipolysis. Myofibroblasts that cause smooth muscle (SM)-actin protein expression have a main role in cell migration and motility within the connective tissue [5]. The network of elastic fibers is better structured. The network of collagen fibers in both the papillary and reticular layers of the dermis is denser and more compact. The interstitial space (the space between blood and lymph vessels) is also reduced, which is a draining effect. Studies (stereophotogrammetry method) also showed a reduction in the volume of the face in fatty and gravitational areas such as low cheeks, the face oval, or the chin. Mécano-stimulation makes it possible to enhance the effect of hyaluronic acid injections. This stimulation enables increased water uptake by the HA and the stimulation of natural HA, collagen, and elastin [45]. As clinical effects, the improvement of the following criteria is indicated: surface irregularity, fine lines, wrinkles, blemishes, skin texture, under-eye dark circles, relief score, skin complexion heterogeneity, redness/rosacea, and color score [5].
4.8. Liposuction and Lipoplasty
Studies have proven that endermologie treatments are the right method to prepare the treatment area before liposuction. They also reduce the risk of complications, postoperative effects, and postoperative recovery time. Endermologie can increase lymphatic and venous flow, leading to a faster resolution of swelling and faster recovery after liposuction. Patient satisfaction is also increased [28]. It is indicated that the use of a combined technique, endermologie and external ultrasound-assisted lipoplasty (EUAL), can improve both body contouring and cellulite. Moreover, a program of postoperative endermologie can redistribute malpositioned, weakly adherent subcutaneous fat accumulations in the postlipoplasty patient. While the combination of endermologie and external ultrasound-assisted lipoplasty (EUAL) has been suggested to enhance both body contouring and cellulite reduction, clinical evidence presents a more nuanced perspective. A study by LaTrenta and Mick (2001) [37] compared postoperative outcomes between patients undergoing EUAL alone and those receiving EUAL followed by a 20-week course of endermologie. The findings indicated no statistically significant difference in body contour improvement between the two groups; however, a notable reduction in the appearance of cellulite was observed in the group receiving the combined treatment. These results suggest that while endermologie may not significantly enhance body contouring outcomes when combined with EUAL, it does offer benefits in reducing cellulite appearance and decreasing the likelihood of revision surgeries. This highlights the importance of tailoring postoperative care to individual patient goals, particularly when addressing concerns related to cellulite [37].
4.9. Morphea
Endermologie can be considered a method of treatment for morphea symptoms, and it should also be tried in other types of scleroderma because this treatment can soften the skin, relieve pain, and, therefore, improve the quality of life for these patients. Studies showed overall improvement in the lesions, as well as pain and induration reduction (an increase in elasticity). The tolerance to the treatment was good. Although the disease cannot be cured, the patients were satisfied with the therapy; they wanted to continue LPG treatments and their quality of life improved [34].
4.10. Fibromyalgia
Fibromyalgia (fibromyalgia syndrome, FMS) is a pain syndrome characterized by chronic, generalized muscle and joint pain and the occurrence of the so-called tender points, i.e., places of the body with excessive sensitivity to pressure. Multidisciplinary treatments combining different approaches (drug therapy, acupuncture), including connective tissue massage, may have the best overall effectiveness. The massage technique (LPG technique) was used because of its effects, such as an increase in blood flow, relaxation of muscle spasms, and the relief of delayed-onset muscle soreness. Massage is thought to affect outcomes through both psychologic and physiologic mechanisms. The results of Gordon et al.’s pilot study showed an improvement in the number of tender points, physical function, and pain intensity [32].
4.11. Orthopedics and Postoperative Rehabilitation
Endermologie treatment after total knee arthroplasty showed significant improvement in active knee flexion and a reduction in edema and pain at the end of treatment. Endermologie could be an alternative method used in early postoperative recovery [22].
4.12. After Colectomy
The results of Le Blanc-Louvry et al. suggest that mechanical massage of the abdominal wall may reduce the duration of ileus and decrease pain after a colectomy. The study compared 25 patients treated with active mechanical massage of the abdominal wall (endermologie) with 25 patients treated with sham non-active mechanical massage (endermologie without aspiration; placebo group). The researchers hypothesized that parietal abdominal stimulation could counteract postoperative ileus and induce pain through common spinal sensitive pathways with nociceptive visceral messages [36].
5. Limitations and Future Research Directions
Despite the growing body of evidence supporting the efficacy of endermologie, several limitations must be acknowledged, particularly regarding the heterogeneity of existing studies. The studies analyzed in this review varied considerably in terms of methodology, patient selection, treatment parameters, and outcome measures, which may impact the generalizability of the findings. One key source of heterogeneity was the patient selection criteria. Additionally, variations in the treatment protocols applied—such as differences in vacuum intensity, duration, frequency, and the number of sessions—introduced inconsistencies in the reported outcomes. While some studies demonstrated significant improvements in post-surgical recovery, others reported skin elasticity and cellulite reduction, raising questions about the standardization of treatment parameters. Moreover, the lack of large-scale, long-term clinical trials limits our ability to assess the durability of endermologie’s effects. Additionally, there is an absence of comparative studies evaluating endermologie against other physical therapy modalities.
From a practical perspective, several factors may influence the accessibility and applicability of endermologie. The cost of treatment remains a potential barrier, as sessions may not be covered by health insurance, limiting their availability to a wider patient population. Additionally, the procedure requires specialized equipment and trained personnel, which may affect its integration into standard medical and physiotherapy settings. Furthermore, certain contraindications, such as active skin infections, severe circulatory disorders, or deep vein thrombosis, must be considered when determining patient eligibility for the therapy.
Given these limitations, future research should aim to address several critical gaps. First, long-term efficacy validation is needed through well-designed, randomized controlled trials (RCTs) with larger sample sizes and extended follow-up periods. Second, mechanistic exploration at the cellular and molecular levels should be prioritized to better understand how endermologie influences fibroblast activity, extracellular matrix remodeling, and adipose tissue metabolism. Finally, comparative studies evaluating endermologie alongside other therapeutic interventions will help clarify its unique benefits and relative efficacy in different clinical and aesthetic applications.
Addressing these research gaps will not only enhance our understanding of endermologie’s mechanisms and effectiveness but also support its broader adoption as a scientifically validated therapeutic tool in both medical and aesthetic practice.
6. Conclusions
Endermologie is a versatile treatment with proven benefits in both medical and aesthetic applications. It enhances microcirculation, reduces edema, improves skin trophicity, and supports tissue remodeling. Scientific studies highlight its role in extracellular matrix modulation, fibroblast activation, fat metabolism, and venolymphatic circulation. Despite variations in study designs, evidence suggests that endermologie can be an effective adjunct therapy for optimizing scar healing, preventing post-surgical complications, and improving overall therapeutic outcomes. Its integrative approach makes it a valuable tool in enhancing patient care, satisfaction, and quality of life.
Author Contributions
Conceptualization—A.K.; Methodology—A.K.; Software—A.K.; Validation—A.K.; Formal analysis—J.A.; Investigation—A.K. and J.A.; Data curation—A.K. and J.A.; Funding acquisition—H.R.; Project administration—H.R.; Resources—A.K.; Supervision—A.K.; Writing—original draft—A.K. and J.A.; Visualization—A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by statutory research activity Department of Cosmetology and Aesthetic Dermatology, Faculty of Pharmacy, Medical University of Lodz No.: 503/3-066-01/503-31-001-19-00.
Acknowledgments
We would like to thank Felice Picariello for their valuable insights and feedback on this research, particularly for providing resources and materials. We also appreciate the assistance of RuthAnn Fanston, especially with the analysis of the results.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- De la Cruz, M. Expansión cutánea externa con endermología. Un método alternativo complementario en reconstrucción mamaria diferida. Cirugía Plástica Ibero-Latinoam. 2015, 41, 359–372. [Google Scholar] [CrossRef]
- Bacci, P.A. Endermologie–LPG Systems® after 15 Years. In Cellulite, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2010; pp. 91–98. [Google Scholar]
- Moortgat, P.; Anthonissen, M.; Meirte, J.; Van Daele, U.; Maertens, K. The physical and physiological effects of vacuum massage on the different skin layers: A current status of the literature. Burn. Trauma 2016, 4, 34. [Google Scholar] [CrossRef]
- Mezencevová, V.; Torok, J.; Czánová, T.; Zajac, J. Endermologie new aproach in the medicine Treatment. Technol. Eng. 2017, 1, 27–30. [Google Scholar] [CrossRef][Green Version]
- Humbert, P.; Fanian, F.; Lihoreau, T.; Jeudy, A.; Elkhyat, A.; Robin, S.; Courderot-Masuyer, C.; Tauzin, H.; Lafforgue, C.; Haftek, M. Mécano-Stimulation™ of the skin improves sagging score and induces beneficial functional modification of the fibroblasts: Clinical, biological, and histological evaluations. Clin. Interv. Aging 2015, 10, 387–403. [Google Scholar]
- Majani, U.; Majani, A. Tissue mechanostimulation in the treatment of scars. Acta Medica 2013, 29, 191–192. [Google Scholar]
- Silver, F.H.; Siperko, L.M.; Seehra, G.P. Mechanobiology of force transduction in dermal tissue. Ski. Res. Technol. 2003, 9, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Kolodziejczak, A. Mechanized vacuum massage (endermology-type treatments). In Cosmetology; PZWL Wydawnictwo Lekarskie: Warszawa, UK, 2019; Volume 1, Chapter 53; p. 503. [Google Scholar]
- Innocenzi, D.; Balzani, A.; Montesi, G.; La Torre, G.; Tenna, S.; Scuderi, N.; Calvieri, S. Evidenza delle modificazioni cutanee indotte dalla tecnica LPG mediante analise d’immagini. In DermoCosmetologia; CIC International Editions: Brooklyn, NY, USA, 2003; pp. 9–15. [Google Scholar]
- Xia, M.; Chen, Y.; He, Y.; Li, H.; Li, W. Activation of the RhoA-YAP-β-catenin signaling axis promotes the expansion of inner ear progenitor cells in 3D culture. Stem Cells 2020, 38, 860–874. [Google Scholar] [CrossRef] [PubMed]
- Adcock, D.; Paulsen, S.; Jabour, K.; Davis, S.; Nanney, L.B.; Shack, R.B. Analysis of the effects of deep mechanical massage in the porcine model. Plast. Reconstr. Surg. 2001, 108, 233–240. [Google Scholar] [CrossRef]
- Shoham, N.; Gefen, A. Mechanotransduction in adipocytes. J. Biomech. 2012, 45, 1–8. [Google Scholar] [CrossRef]
- Moseley, A.; Piller, N.; Douglass, J.; Esplin, M. Comparison of the effectiveness of MLD and LPG technique. J. Lymphoedema 2007, 2, 30–36. [Google Scholar]
- Moseley, A.L.; Esplin, M.; Piller, N.B.; Douglass, J. Endermologie (with and without compression bandaging) a new treatment option for secondary arm lymphedema. Lymphology 2007, 40, 129–137. [Google Scholar] [PubMed]
- Malloizel-Delaunay, J.; Weyl, A.; Brusq, C.; Chaput, B.; Garmy-Susini, B.; Bongard, V.; Vaysse, C. New Strategy for Breast Cancer Related Lymphedema Treatment by Endermology: ELOCS Phase II Randomized Controlled Trial. Clin. Breast Cancer 2024, 24, 533–540. [Google Scholar] [CrossRef]
- Ahmed Ziethar, E.T. Endermologie Technique versus Decongestive Lymphatic Therapy on Post-mastectomy Related Lymphedema. J. Nov. Physiother. 2013, 3, 155. [Google Scholar]
- Revuz, J.; Adhoute, H.; Cesarini, J.; Poli, F.; Lacarrière, C.; Emiliozzi, C. Clinical and histological effects of the Lift 6 device used on facial skin aging. Nouv. Dermatol. 2002, 21, 335–342. [Google Scholar]
- Lattarulo, P.; Bacci, P.; Mangini, S. Physiological tissue changes after administration of micronized Diosmin/Hesperidin, individually or in association with Endermologiae. Int. J. Aesthetic Cosmet Beauty Surg. 2001, 1, 25–28. [Google Scholar]
- Nedelec, B.; Edger-Lacoursière, Z.; Gauthier, N.; Marois-Pagé, E.; Jean, S. Randomized, controlled, within-patient, single-blinded pilot study to evaluate the efficacy of 12-weeks of endermotherapy with adult burn survivors. Burns 2024, 50, 107269. [Google Scholar] [CrossRef]
- Leung, A.K.P.; Ouyang, H.; Pang, M.Y.C. Effects of mechanical stimulation on mastectomy scars within 2 months of surgery: A single-center, single-blinded, randomized controlled trial. Ann. Phys. Rehabil. Med. 2023, 66, 101724. [Google Scholar] [CrossRef] [PubMed]
- Razzouk, K.; Humbert, P.; Borens, B.; Gozzi, M.; Al Khori, N.; Pasquier, J.; Rafii Tabrizi, A. Skin trophicity improvement by mechanotherapy for lipofilling-based breast reconstruction postradiation therapy. Breast J. 2020, 26, 725–728. [Google Scholar] [CrossRef]
- Kim, S.M.; Kim, S.R.; Lee, Y.K.; Kim, B.R.; Han, E.Y. The effect of mechanical massage on early outcome after total knee arthroplasty: A pilot study. J. Phys. Ther. Sci. 2015, 27, 3413–3416. [Google Scholar] [CrossRef]
- Márquez-Rebollo, C.; Vergara-Carrasco, L.; Díaz-Navarro, R.; Rubio-Fernández, D.; Francoli-Martínez, P.; Sánchez-De la Rosa, R. Benefit of endermology on indurations and panniculitis/lipoatrophy during relapsing-remitting multiple sclerosis long-term treatment with glatiramer acetate. Adv. Ther. 2014, 31, 904–914. [Google Scholar] [CrossRef]
- Kutlubay, Z.; Songur, A.; Engin, B.; Khatib, R.; Calay, Ö.; Serdaroğlu, S. An alternative treatment modality for cellulite: LPG endermologie. J. Cosmet. Laser Ther. 2013, 15, 266–270. [Google Scholar] [CrossRef]
- Rubio Fernández, D.; Rodríguez Del Canto, C.; Marcos Galán, V.; Falcón, N.; Edreira, H.; Sevane Fernández, L.; Francoli Martínez, P.; Sánchez-De la Rosa, R. Contribution of endermology to improving indurations and panniculitis/lipoatrophy at glatiramer acetate injection site. Adv. Ther. 2012, 29, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Marques, M.A.; Combes, M.; Roussel, B.; Vidal-Dupont, L.; Thalamas, C.; Lafontan, M.; Viguerie, N. Impact of a mechanical massage on gene expression profile and lipid mobilization in female gluteofemoral adipose tissue. Obes. Facts 2011, 4, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Lebrun, C.; Mondot, L.; Bertagna, M.; Calleja, A.; Cohen, M. Endermology: A treatment for injection-induced lipoatrophy in multiple sclerosis patients treated with sub cutaneous glatiramer acetate. Clin. Neurol. Neurosurg. 2011, 113, 721–724. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Cha, S.M.; Naidu, S.; Hwang, W.J. Analysis of postoperative complications for superficial liposuction: A review of 2398 cases. Plast. Reconstr. Surg. 2011, 127, 863–871. [Google Scholar] [CrossRef]
- Güleç, A.T. Treatment of cellulite with LPG endermologie. Int. J. Dermatol. 2009, 48, 265–270. [Google Scholar] [CrossRef]
- Monteux, C.; Lafontan, M. Use of the microdialysis technique to assess lipolytic responsiveness of femoral adipose tissue after 12 sessions of mechanical massage technique. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 1465–1470. [Google Scholar] [CrossRef]
- Bourgeois, J.F.; Gourgou, S.; Kramar, A.; Lagarde, J.M.; Guillot, B. A randomized, prospective study using the LPG technique in treating radiation-induced skin fibrosis: Clinical and profilometric analysis. Ski. Res. Technol. 2008, 14, 71–76. [Google Scholar] [CrossRef]
- Gordon, C.; Emiliozzi, C.; Zartarian, M. Use of a mechanical massage technique in the treatment of fibromyalgia: A preliminary study. Arch. Phys. Med. Rehabil. 2006, 87, 145–147. [Google Scholar] [CrossRef]
- Lhoest, F.; Grandjean, F.X.; Heymans, O. La maladie de Mondor: Une complication de la chirurgie mammaire [Mondor’s disease: A complication after breast surgery]. Ann. Chir. Plast Esthet. 2005, 50, 197–201. [Google Scholar] [CrossRef]
- Worret, W.I.; Jessberger, B. Effectiveness of LPG treatment in morphea. J. Eur. Acad. Dermatol. Venereol. 2004, 18, 527–530. [Google Scholar] [CrossRef]
- Ortonne, J.P.; Queille-Roussel, C.; Duteil, L.; Emiliozzi, C.; Zartarian, M. Treatment of cellulite: Effectiveness and sustained effect at 6 months with Endermologiefi demonstrated by several quantitative evaluation methods. Nouv. Dermatol. 2004, 23, 261–269. [Google Scholar]
- Le Blanc-Louvry, I.; Costaglioli, B.; Boulon, C.; Leroi, A.M.; Ducrotte, P. Does mechanical massage of the abdominal wall after colectomy reduce postoperative pain and shorten the duration of ileus? Results of a randomized study. J. Gastrointest. Surg. 2002, 6, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Latrenta, G.S.; Mick, S.L. Endermologie after external ultrasound-assisted lipoplasty (EUAL) versus EUAL alone. Aesthet. Surg. J. 2001, 21, 128–135. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Moortgat, P.; Meirte, J.; Van Daele, U.; Anthonissen, M.; Vanhullebusch, T.; Maertens, K. Chapter 54 Vacuum Massage in the Treatment of Scars. In Textbook on Scar Management: State of the Art Management and Emerging Technologies; Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G., Eds.; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar] [PubMed]
- Campisi, C.; Boccardo, F.; Azevedo, W.F., Jr. LPG systems in the treatment of peripheral lymphedema. Lymphology 2002, 35, 364–367. [Google Scholar]
- Arora, G.; Patil, A.; Hooshanginezhad, Z.; Fritz, K.; Salavastru, C.; Kassir, M.; Goldman, M.P.; Gold, M.H.; Adatto, M.; Grabbe, S.; et al. Cellulite: Presentation and management. J. Cosmet. Dermatol. 2022, 21, 1393–1401. [Google Scholar] [CrossRef]
- Lebrun, C.; Bertagna, M.; Cohen, M. Cutaneous Side-effects of Immunomodulators in MS. Int. MS J. 2011, 17, 88–94. [Google Scholar]
- Wahid, D.I.; Wahyono, R.A.; Setiaji, K.; Hardiyanto, H.; Suwardjo, S.; Anwar, S.L.; Aryandono, T. The Effication of Low-Level Laser Therapy, Kinesio Taping, and Endermology on Post-Mastectomy Lymphedema: A Systematic Review and Meta-Analysis. Asian Pac. J. Cancer Prev. 2024, 25, 3771–3779. [Google Scholar] [CrossRef]
- Petricig, P.; Becchetti, E.; Barile, A.; Becchetti, A.; Dominici, C. Studio istologico del tessuto cutaneo e sottocutaneo dopo trattamento con tecnica LPG (Endermologie). In Proceedings of the XXI Italian Congress of Aesthetic Medicine, Rome, Italy, 31 March–2 April 2000. [Google Scholar]
- Fitoussi, A.; Razzouk, K.; Ahsan, M.D.; Andrews, G.; Rafii, A. Autologous Fat Grafting as a Stand-alone Method for Immediate Breast Reconstruction After Radical Mastectomy in a Series of 15 Patients. Ann. Plast. Surg. 2022, 88, 25–31. [Google Scholar] [CrossRef]
- Breton-Torres, I.; Lefebvre, C.; Jammet, P. Post-injection facial massage/kinesiotherapy in aesthetic medicine. Kinesither Sci. 2014, 554, 15–21. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).