Featured Application
Prostheses and Orthoses application.
Abstract
Diabetic foot ulcer patients are usually unaware of excessive pressure on their feet due to lost pressure sensitivity. Offloading insoles are used to alleviate foot pain. This study investigated the effect of infill pattern and infill density on plantar pressure reduction for 3D-printed insoles while walking. The study involves five infill patterns: grid, honeycomb, triangle, cubic, and gyroid, along with several infill densities ranging from 14% to 20%. The test 3D-printed thermoplastic polyurethane specimens were assessed for mechanical properties to identify suitable infill patterns for creating prototypes of insoles. The results indicated that the honeycomb infill pattern exhibited the highest maximum compression load at 50% compressive strain and has a significant area under the loading-unloading curve, signifying high energy absorption. Conversely, the gyroid infill pattern exhibited the lowest maximum compression load at 50% compressive strain and minimal energy absorption. Both infill patterns with 20% infill density were applied in 3D-printed insoles and tested on the foot plantar pressure of healthy male volunteers during walking. No statistically significant differences in plantar pressure were observed between the two infill patterns compared to walking without insoles. A reduction in plantar pressure at hindfoot was observed when using the insoles, although this change was not statistically significant.
1. Introduction
Diabetes mellitus (DM) is a non-communicable disease which affects the daily life of patients and is associated with poor health outcomes. A common complication of diabetic patients is diabetic foot syndrome which can be developed to a severe complication such as diabetic foot ulcer (DFU). It was reported that the global prevalence of DFU was 6.3%, which was higher in males than in females and higher in patients with type 2 DM than those with type 1 DM [1]. The management of DFU becomes a challenge in the healthcare service and it also leads to a socioeconomic burden [2,3]. Many strategies have been implemented to manage foot DFU such as glycemic control, pharmacological therapy, topical oxygen therapy, wound dressing and debridement [3,4]. One effective strategy of preventive management for DFU is the off-loading strategy, which aims to reduce and redistribute weight-bearing load over an area of the foot. Several off-loading devices have been applied to diabetic patients including total contact cast, removable cast walkers, orthotic devices and custom-made shoes and insoles [2,3,5]. The effective off-loading of diabetic foot is mandatory for ulcer healing and ulcer recurrence prevention.
Additive manufacturing technology has been introduced for prototype fabrication and final product fabrication. It is the process of making an object by building material, layer-by-layer, such as 3D-printing technology. Recently, 3D-printing technology has become popular and is easily available as desktop equipment, especially fused deposition modeling (FDM). Making a diabetic custom-made insole using the FDM method can reduce the fabrication process by many steps compared to conventional insole manufacturing, which is laborious work [6]. Furthermore, conventional insole manufacturing creates harmful particles that can affect the respiratory system and environment [7]. Several studies have fabricated 3D-printed insoles for diabetic feet using the FDM method [6,8,9,10]. Various thermoplastic materials can be printed with the FDM method, e.g., acrylonitrile butadiene styrene (ABS), polylactic acid (PLA), polycarbonate (PC), thermoplastic elastomer (TPE) and thermoplastic polyurethane (TPU), etc. When making a 3D-printed insole for diabetic feet, the frequently used material is TPU due to homogeneous, isotropic and soft elastic material [9]. Furthermore, aside from materials, important printing factors include infill pattern and infill density. These two factors can affect printing time, material usage and the mechanical properties and off-loading characteristic of insoles.
Several computational and experimental studies have been conducted with different infill structures such as porous structural unit and lattice structures [11,12,13,14,15]. Kumar et al. proposed a 3D-printed insole using a Kelvin lattice structure, which can reduce plantar pressure and promotes more balanced weight distribution [13]. Ali et al. performed a simulation using three lattice meshes of midsole designs including hexagonal, elliptical and circular lattice structures [14]. They showed the highest maximum stress occurring in the midsole with the elliptical lattice structure. Their work concluded that using combination of lattice structure to increase the energy absorption capacity could provide more local comfort to user’s requirements. Jonnala and colleagues reported that the gyroid structure has a high specific energy absorption capability when compared to the solid structure. This characteristic is beneficial to the orthotic insole [11]. They suggested that the infill density parameter should be considered for the selection of the structure for 3D-printed insoles. Chatzistergos and colleagues varied the stiffness of 3D-printed footbeds by changing the infill density [16]. They showed that stiffer footbeds were suitable for participants who have a high body mass index. It was also reported that 3D-printed insoles show better comfort improvement compared to prefabricated insole in patients with symptomatic flatfoot [17]. However, there are still limited studies that consider the effects of infill pattern and infill density of 3D printing on the mechanical properties based on experimental studies and consequently tests in human subjects to observe the plantar pressure distribution during gait. This study investigated this gap by using five different infill patterns (honeycomb, grid, triangular, cubic and gyroid patterns) and four different infill densities (14%, 16%, 18%, 20%) for mechanical property testing. Furthermore, we investigated the effects of selected infill pattern and density using a 3D-printed insole on the plantar pressure distribution during walking in healthy subjects, which is valuable information for an insole design for diabetic patients.
2. Materials and Methods
2.1. Specimen Preparation
The standard test specimens were 28.6 ± 0.1 mm in diameter and 12.5 ± 0.5 mm in thickness, as suggested in ASTM D575-91 [18]. The test specimens were printed using Pro 2 Plus 3D printer (Raise 3D Technologies, Inc., Lake Forest, CA, USA). The material was TPU filament (PolyFlexTM TPU95, Polymaker, Changshu, China). ideaMaker® slicing software version 4.4.1 (Raise 3D Technologies, Inc., Lake Forest, CA, USA) was used to assign infill pattern and density. Honeycomb, grid, triangular, cubic and gyroid patterns were printed with four different infill densities (14%, 16%, 18%, 20%), as shown in Figure 1. For each infill density, three test specimens were prepared.
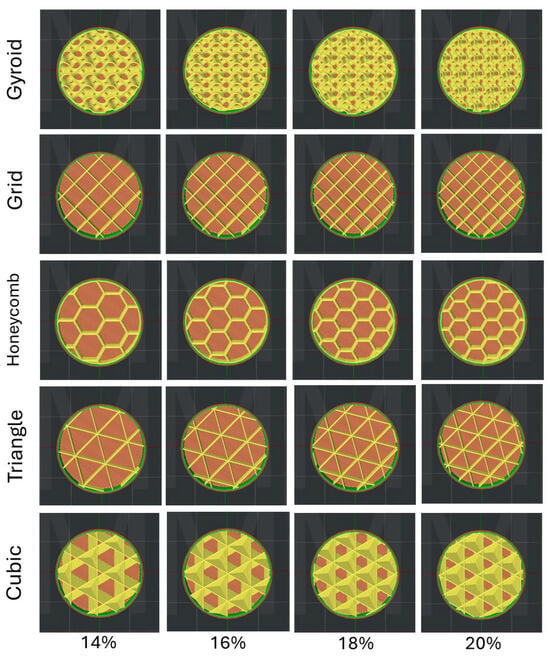
Figure 1.
Five infill patterns and four infill densities created for test specimens.
2.2. Mechanical Properties Test
The test specimens were performed a compression test at 50% strain using the Instron 8872 series of servohydraulic testing systems (Instron, Norwood, MA, USA). Loading and unloading conditions were performed during the test according to ASTM D575-91. Each test specimen was tested 4 times, and maximum compressive load and area under the loading–unloading curves were determined. The area under the loading–unloading curves was determined to quantify the energy dissipation.
2.3. Insole Fabrication
The 3D-printed insoles were designed as simple flat insoles with a length of 26.5 mm and a thickness of 3 mm, like a cushion insole, using a computer-aided design software ANSYS SpaceClaim 2022R1, a 3D modeling software (ANSYS, Inc., Canonsburg, PA, USA). The insoles were fabricated using Pro 2 Plus 3D printer (Raise 3D Technologies, Inc., Lake Forest, CA, USA) and PolyFlexTM TPU95 (Polymaker, Changshu, China). Figure 2 shows the 3D-printed flat insole.
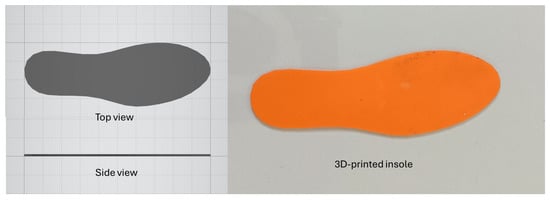
Figure 2.
Flat insole drawing for 3D printer.
2.4. Plantar Pressure Measurement
Ten healthy male participants without any foot deformity were recruited to measure the plantar pressure wearing with and without 3D-printed insoles. The study protocol was approved by the ethical committee of Faculty of Medicine, Prince of Songkla University with the approval number REC.66-188-38-2. Plantar pressure was measured using Pedar® system (Novel gmbh, Munich, Germany) and in-shoe plantar pressure sensors during 3 rounds of 10 m walking at self-selected speed. The test was conducted at the Southern Medical Rehabilitation Centre of Songklanagarind Hospital.
2.5. Gait Data Analysis
For each participant, five consecutive gait cycles were analyzed, and the plantar pressure data were processed to segment the cycles into the stance and swing phases. Then, the mean plantar pressure of each side in three regions of the foot (hindfoot, midfoot and forefoot) and area under the curve of force–time during stance phase of the gait cycle were determined. One-way ANOVA was performed to determine the significance of mean plantar pressure and area under the force–time curve. Statistical significance was defined as p < 0.05.
3. Results
3.1. Mechanical Property Testing
Figure 3 shows maximum compression load of test specimens with different infill patterns and infill densities. Increasing infill density potentially provides a higher compression load for every infill pattern. At 50% strain test, honeycomb infill pattern presents the highest maximum compression load that can be applied on specimens during the loading–unloading test, whereas gyroid infill pattern is the lowest. The loading–unloading test showed that TPU has viscoelastic material properties (Figure 4). In the first trial of the loading–unloading test, the specimen was in a pre-condition. Therefore, trial 2 to trail 4 were taken into consideration. The patterns of the loading–unloading plot looked similar for each infill pattern. When we calculated the area under the loading–unloading curves, which represented energy absorption, we found that the honeycomb infill pattern mostly had maximum area, whereas the gyroid infill pattern had minimum area, as shown in Figure 5. The loading–unloading area increased when the infill density increased. Therefore, we selected these two infill patterns, honeycomb and gyroid, to investigate the plantar pressure during walking.
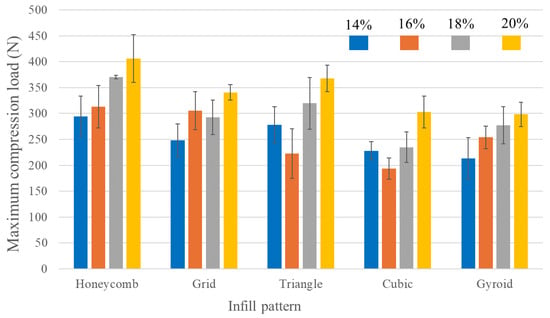
Figure 3.
Maximum compression load of test specimens with five infill patterns (honeycomb, grid, triangle, cubic and gyroid) and four infill densities (14%, 16%, 18%, 20%).
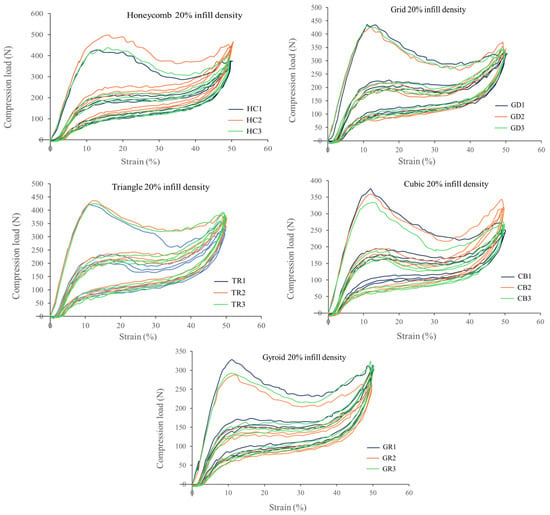
Figure 4.
The loading-unloading test at 50% strain on test specimens with 20% infill density of five infill patterns (HC: honeycomb, GD: grid, TR: triangle, CB: cubic and GR: gyroid).
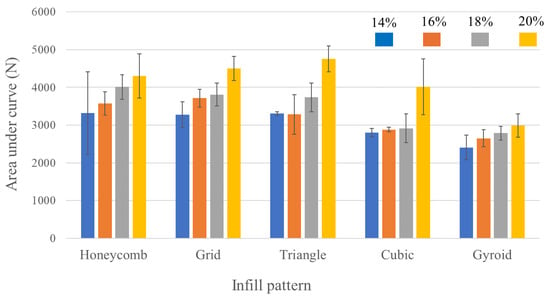
Figure 5.
The area under the loading-unloading curves of test specimens with five infill patterns (honeycomb, grid, triangle, cubic and gyroid) and four infill densities (14%, 16%, 18%, 20%).
3.2. Plantar Pressure in Gait
In this study, ten healthy male participants were recruited, and their demographic data are presented in Table 1. All participants were adults with a dominant right-hand side. Table 2 shows the mean plantar pressure during gait in three-foot regions when walking with and without 3D-printed insoles. It is noticed that the right foot has slightly lower mean plantar pressure compared to the left foot. Hindfoot and forefoot regions are higher mean plantar pressure areas when walking with or without 3D-printed insoles than a midfoot region. Using 3D-printed insoles, there is no significant difference in mean plantar pressure in each foot region when compared to walking without insole (p > 0.05).

Table 1.
The demographic data of 10 healthy male participants.

Table 2.
The mean plantar pressure during gait in three regions of the foot when walking with 3D-printed insoles and without insoles.
Center of pressure (COP) trajectories, green lines, during walking with and without 3D-printed insoles are displayed in Figure 6. The trajectories start from heel to forefoot regions, and they look different for each participant. In common, these trajectories line in the middle and move to medial side in the midfoot region more than lateral side. Table 3 presents the area under the force–time curve during gait. It shows that walking without insoles has the lowest force–time integral (FTI) compared to walking with 3D-printed insoles. Wearing 3D-printed insoles with honeycomb infill pattern provides the highest FTI. However, our investigations show no statistically significant difference in FTI between wearing 3D-printed insoles and not wearing them (p > 0.05).
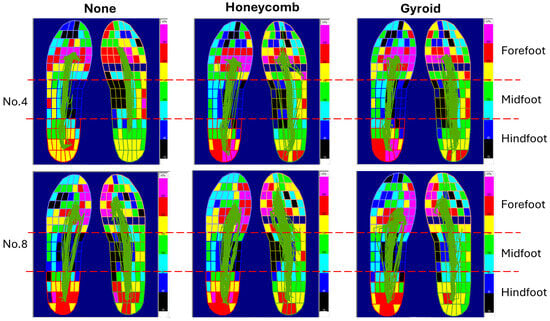
Figure 6.
Center of pressure (COP) trajectories during walking with and without 3D-printed insoles in two participants. The trajectory begins at heel contact and progresses through to the midfoot to the forefoot and toes during walking. A smooth, forward-moving COP trajectory indicates a stable and coordinated gait.

Table 3.
The area under the force–time curve during gait with and without 3D-printed insoles.
4. Discussion
This study demonstrated that infill patterns and density influence the mechanical properties of 3D-printed objects in terms of maximum compressive load and energy absorption. The findings of this study suggest that stiffness of 3D-printed object depends on infill pattern and infill density. Walking with insoles, the selected infill pattern (honeycomb and gyroid) with 20% infill density could reduce the plantar pressure at the heel around 10% when compared to walking without insole. However, there was increased plantar pressure in midfoot and forefoot regions when using insoles. This addresses the insole design and printing parameters that need to be considered when making 3D-printed insoles for diabetic patients.
There are several materials that are commonly used for insoles such as gel, foam, cork and leather. These materials have properties ranging from good flexibility to good firmness to add an extra cushion, support and control. It has been reported that low- to moderate-stiffness materials are suitable to provide a cushioning function [19,20]. Softer materials provide comfortable accommodation, whereas stiffer materials are more durable [21]. Chatzistergos et al. pointed out that the correct selection of cushioning stiffness can significantly reduce plantar pressure: stiffer cushioning materials were necessary for those with a higher BMI, and softer cushioning materials were suitable to reduce peak plantar pressure more at the midfoot than other foot regions [16,22]. They also showed increased infill densities from 10% to 20% provided higher relative stiffness for 3D-printed TPU footbeds. Their finding was, like in our study, that increased infill densities obtained a higher maximum compression load, especially for honeycomb and gyroid patterns. Orsu and Shaik looked at the compression strength of customized shoe insole with different infill patterns and infill densities using 3D printing [23]. Four infill patterns were investigated with 25%, 40% and 60% infill densities: they were triangle, rectilinear, cubic and gyroid. Compressive strength was higher when the infill density increased for all infill patterns. Gyroid and cubic infill patterns had lower compressive strength compared to the other two patterns. Their research has similar results to our study, showing that gyroid and cubic infill patterns had lower maximum compression load compared to the other three patterns. However, in our study, the honeycomb infill pattern provides the highest maximum compression load among five infill patterns, not the triangle infill pattern. Peker and colleagues performed mechanical tests on the 3D-printed specimens using elastic filament and found that hardness, Young’s modulus and tensile stress were increased when infill density was increased [6]. Some computational studies looked at the most effective insole infill for plantar pressure and weight distribution. Koteswari and Yeole used finite element analysis to demonstrate that lattice structures affected maximum stress and deformation [12]. Similarly, Kumar et al. numerically showed that increasing the number of unit cells enhances the stiffness of the insole model, and the unit cell architecture plays a role in stiffness [13].
Cushioning, shock absorption and durability are important features of diabetic insoles, which help to distribute pressure across the foot, reduce the impact of walking or standing and provide long-lasting support, respectively. Our study showed that TPU showed viscoelastic behavior when under the loading–unloading compression test. The energy absorbed during a loading–unloading cycle is different in each infill pattern and infill density. The honeycomb infill pattern possibly has good shock absorption characteristics due to its high energy absorption, while the gyroid infill pattern has low energy absorption. Furthermore, our study revealed that increased infill density provided higher energy absorption. Our findings are supported by Jonnala et al., who reported that gyroid structure showed lower elastic absorbed energy per unit volume than solid structure [11], and Xiao et al., who concluded that density is a major factor that influences cushioning energy absorption performance [24]. Materials with high energy absorption and elastic modulus indicate its potential application in dampers, shock absorbers and cushioning [25]. It was found that the specimens taken from the single material insole had larger relative energy dissipation compared to that taken from the dual-material insole, providing higher stress response [26,27]. However, good energy absorption materials relate to high stiffness, which should be considered when using them as materials for diabetic insoles.
Three-dimensional-printed insoles have been proposed in many studies for diabetic foot management in the aspect of off-loading function and plantar pressure reduction. Stiffness optimization of 3D-printed footbeds was conducted in fifteen diabetic patients by Chatzistergos et al. They found that the optimum stiffness resulted in a maximum percentage of plantar pressure reduction [16]. In our study, subjects who walked with 3D-printed insoles had lower mean plantar pressure in the hindfoot region on both left and right sides than without insoles, whereas they had elevated mean plantar pressure in other regions of the foot. The area under the force–time curve during gait represented the vertical impulse showed similar values between insoles with honeycomb and gyroid infill patterns. However, the test specimen with honeycomb infill pattern showed higher energy dissipation than that with gyroid infill pattern. Kumar and Sarangi used 3D-printed insoles made of kelvin lattice infill to look at the plantar pressure distribution during standing and showed that the insole-clad foot condition had lower average pressure compared to the barefoot condition, similar in both feet [13]. Another study by Zuniga et al. found that 3D-printed insoles using thermoplastic polyurethane polyester-based polymer with hexagonal infill pattern and 40% infill density had lower average peak pressure than the standard insole [28]. Zuniga et al. also reported that another filament that they used for 3D-printed insoles showed slightly higher average peak pressure than the standard insoles. This suggests that wearing insoles is beneficial in plantar pressure reduction. This benefit is also supported by Muir and colleagues, who confirmed that 3D-printed personalized metamaterial insoles could reduce plantar pressure in offloading regions [29].
A total contact insole (TCI) with graded stiffness showed a reduction in peak plantar pressure better than a normal TCI, a flat insole with graded stiffness and a normal flat insole during walking, especially during upward acceleration [9]. Our study used 3D-printed flat insoles that might not fit the foot shape of each participant, but they were able to reduce plantar pressure at the heel. In clinical practice, contoured insoles are provided to diabetic patients due to their offloading performance [27,30]. The material selection for insoles is also important for offloading performance, and soft insole materials usually have better performance than rigid insole materials. Furthermore, the thickness of an insole can influence offloading performance as well as energy absorption. In our study, 3D-printed insoles with 3 mm thickness were tested. This might be a reason why there is no significant difference in plantar pressure reduction and area under the curve of force–time plot when compared to walking without insole. Several studies performed a finite element analysis and addressed several factors in reducing peak plantar pressure including arch-conforming, insole stiffness and insole thickness [31,32]. Tang et al. proposed a new design method to optimize the stress distribution of the contact surfaces between the foot and the insole using functional gradient structure via porous structural units (cube) to the 3D-printed insole, leading to a reduction in the peak plantar pressure [33]. Furthermore, we could not clearly distinguish the difference of center of pressure (COP) trajectory between with 3D-printed insoles and without insoles. There are various paths of COP, which are different for each participant. However, there was a study that showed the effect of types of material, stiffness, thickness and shape of insole on COP trajectory [27,34].
This study has several limitations that should be further mitigated and investigated. First, the design and thickness of the insole should be modified. As previously mentioned, contoured and optimized stiffness insoles should be designed, printed and tested. A flexural fatigue, durability and comfort ability test should be performed with 3D-printed insoles to look at the effects of infill pattern and density on these characteristics [16,35]. As this study involved only healthy subjects and was conducted over a short period, it is better to perform a long-term durability assessment and determine the effectiveness of 3D-printed insoles on plantar pressure reduction and distribution in diabetic patients who have an early stage of foot ulceration to obtain more insights from users.
5. Conclusions
The effects of infill pattern and density were investigated on the mechanical properties of 3D-printed specimens and on plantar pressure reduction of 3D-printed insoles. The findings of this study showed that both infill pattern and density notably influence stiffness and energy absorption. Increased infill densities provided higher stiffness and energy absorption. Among five infill patterns, based on test specimens, the honeycomb infill pattern gave the highest stiffness, whereas the gyroid infill pattern showed the lowest stiffness. When applying a honeycomb infill pattern and gyroid infill pattern at 20% infill density, the 3D-printed insoles showed no significant reduction in plantar pressure compared to not wearing insoles. The 3D-printed insoles slightly reduced plantar pressure on the heel during walking, whereas other foot regions had elevated plantar pressure. We suggest that optimized stiffness should be considered when offloading is focused on diabetic feet. In addition, a long-term durability assessment and the effectiveness of 3D-printed insoles on plantar pressure reduction should be conducted in diabetic patients.
Author Contributions
Conceptualization, S.C., T.D. and A.K.; methodology, S.C., A.K. and S.S.; formal analysis, S.C. and M.N.; investigation, S.C.; resources, A.K.; data curation, S.C.; writing—original draft preparation, S.C.; writing—review and editing, M.N., S.S. and D.M.; visualization, S.C.; supervision, T.D. and D.M.; funding acquisition, S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by National Science, Research and Innovation Fund (NSRF) and Prince of Songkla University (Grant No. MED6601240S) and Horizon Europe Framework Programme (Grant No. 101086348).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Faculty of Medicine, Prince of Songkla University (REC.66-188-38-2, 25 June 2023).
Informed Consent Statement
Informed consent was obtained from a subject involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding authors.
Acknowledgments
We acknowledge the participants who volunteered for this study. We thank Kitthida Riabroi for assisting in the mechanical testing of specimens and Nusreena Hohsoh for the participant recruitment and data recording.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Zhang, P.; Lu, J.; Jing, Y.; Tang, S.; Zhu, D.; Bi, Y. Global Epidemiology of Diabetic Foot Ulceration: A Systematic Review and Meta-Analysis. Ann. Med. 2017, 49, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Backhouse, M.R.; Bruce, J. Rehabilitation for People Wearing Offloading Devices for Diabetes-Related Foot Ulcers: A Systematic Review and Meta-Analyses. J. Foot Ankle Res. 2023, 16, 16. [Google Scholar] [PubMed]
- Lim, J.Z.M.; Ng, N.S.L.; Thomas, C. Prevention and Treatment of Diabetic Foot Ulcers. J. R. Soc. Med. 2017, 110, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, V.; Mohanasundaram, T.; Karunakaran, D.; Gunasekaran, M.; Tiwari, R. Physiological and Pathophysiological Aspects of Diabetic Foot Ulcer and Its Treatment Strategies. Curr. Diabetes Rev. 2023, 19, e031122210617. [Google Scholar] [CrossRef]
- Cavanagh, P.R.; Bus, S.A. Off-Loading the Diabetic Foot for Ulcer Prevention and Healing. J. Vasc. Surg. 2010, 52, 37S–43S. [Google Scholar] [CrossRef]
- Peker, A.; Aydin, L.; Kucuk, S.; Ozkoc, G.; Cetinarslan, B.; Canturk, Z.; Selek, A. Additive Manufacturing and Biomechanical Validation of a Patient-Specific Diabetic Insole. Polym. Adv. Technol. 2020, 31, 988–996. [Google Scholar] [CrossRef]
- Cheng, J.; Wang, J.-C. Exploring the Feasibility of Advanced Manufacturing for Mass Customization of Insoles in the Context of ESG. Int. J. Precis. Eng. Manuf.-Green Technol. 2024, 11, 815–832. [Google Scholar] [CrossRef]
- Mancuso, M.; Bulzomì, R.; Mannisi, M.; Martelli, F.; Giacomozzi, C. 3D-Printed Insoles for People with Type 2 Diabetes: An Italian, Ambulatory Case Report on the Innovative Care Model. Diabetology 2023, 4, 339–355. [Google Scholar] [CrossRef]
- Zhang, X.; Chu, P.; Ma, X.; Chen, W.M. 3D-Printed Insole Designs for Enhanced Pressure-Relief in Diabetic Foot Based on Functionally-Graded Stiffness Properties. In IFMBE Proceedings, Proceedings of the 12th Asian-Pacific Conference on Medical and Biological Engineering, Suzhou, China, 18–21 May 2023; Springer: Cham, Switzerland, 2024; Volume 104. [Google Scholar]
- Kumar, K.R.; Vinothkumar, P.; Soms, N. Investigation on the Development of Custom Foot Insole Using Soft Polylactic Acid by Fused Deposition Modelling Technique. J. Mater. Eng. Perform. 2023, 32, 1790–1796. [Google Scholar] [CrossRef]
- Jonnala, U.K.; Sankineni, R.; Ravi Kumar, Y. Design and Development of Fused Deposition Modeling (FDM) 3D-Printed Orthotic Insole by Using Gyroid Structure. J. Mech. Behav. Biomed. Mater. 2023, 145, 106005. [Google Scholar] [CrossRef]
- Koteswari, S.; Yeole, S.N. Development of 3D Printed Orthotic Device for Flat Foot Problem. Mater. Today Proc. 2021, 44, 2435–2441. [Google Scholar] [CrossRef]
- Kumar, R.; Sarangi, S.K. 3D Printed Customized Diabetic Foot Insoles with Architecture Designed Lattice Structures—A Case Study. Biomed. Phys. Eng. Express 2024, 10, 015019. [Google Scholar] [CrossRef]
- Zolfagharian, A.; Lakhi, M.; Ranjbar, S.; Bodaghi, M. Custom Shoe Sole Design and Modeling Toward 3D Printing. Int. J. Bioprint 2021, 7, 169–178. [Google Scholar] [CrossRef]
- Hudak, Y.F.; Li, J.S.; Cullum, S.; Strzelecki, B.M.; Richburg, C.; Kaufman, G.E.; Abrahamson, D.; Heckman, J.T.; Ripley, B.; Telfer, S.; et al. A Novel Workflow to a Fabricate Patient-Specific 3D Printed Accommodative Foot Orthosis with Personalized Latticed Metamaterial. Med. Eng. Phys. 2022, 104, 103802. [Google Scholar] [CrossRef]
- Chatzistergos, P.E.; Gatt, A.; Formosa, C.; Farrugia, K.; Chockalingam, N. Optimised Cushioning in Diabetic Footwear Can Significantly Enhance Their Capacity to Reduce Plantar Pressure. Gait Posture 2020, 79, 244–250. [Google Scholar] [CrossRef]
- Xu, R.; Wang, Z.; Ren, Z.; Ma, T.; Jia, Z.; Fang, S.; Jin, H. Comparative Study of the Effects of Customized 3D Printed Insole and Prefabricated Insole on Plantar Pressure and Comfort in Patients with Symptomatic Flatfoot. Med. Sci. Monit. 2019, 25, 3510–3519. [Google Scholar] [CrossRef]
- ASTM D575-91(2024); Standard Test Methods for Rubber Properties in Compression. ASTM International: West Conshohocken, PA, USA, 2024. Available online: https://store.astm.org/d0575-91r24.html (accessed on 6 March 2025).
- Faulí, A.C.; Andrés, C.L.; Rosas, N.P.; Fernández, M.J.; Parreño, E.M.; Barceló, C.O. Physical Evaluation of Insole Materials Used to Treat the Diabetic Foot. J. Am. Podiatr. Med. Assoc. 2008, 98, 229–238. [Google Scholar] [CrossRef]
- Nilsen, F.; Molund, M.; Lium, E.M.; Hvaal, K.H. Material Selection for Diabetic Custom Insoles: A Systematic Review of Insole Materials and Their Properties. JPO J. Prosthet. Orthot. 2022, 34, e131–e143. [Google Scholar] [CrossRef]
- Hellstrand Tang, U.; Zügner, R.; Lisovskaja, V.; Karlsson, J.; Hagberg, K.; Tranberg, R. Comparison of Plantar Pressure in Three Types of Insole given to Patients with Diabetes at Risk of Developing Foot Ulcers—A Two-Year, Randomized Trial. J. Clin. Transl. Endocrinol. 2014, 1, 121–132. [Google Scholar] [CrossRef]
- Chatzistergos, P.E.; Gatt, A.; Formosa, C.; Sinclair, J.K.; Chockalingam, N. Effective and Clinically Relevant Optimisation of Cushioning Stiffness to Maximise the Offloading Capacity of Diabetic Footwear. Diabetes Res. Clin. Pract. 2023, 204, 110914. [Google Scholar] [CrossRef]
- Orsu, B.; Shaik, Y.P. Compression Strength Analysis of Customized Shoe Insole with Different Infill Patterns Using 3D Printing. Open Access J. Sci. 2022, 9, 1–13. [Google Scholar] [CrossRef]
- Xiao, Y.; Yin, J.; Zhang, X.; An, X.; Xiong, Y.; Sun, Y. Mechanical Performance and Cushioning Energy Absorption Characteristics of Rigid Polyurethane Foam at Low and High Strain Rates. Polym. Test. 2022, 109, 107531. [Google Scholar] [CrossRef]
- Reddy, S.K.; Ferry, D.B.; Misra, A. Highly Compressible Behavior of Polymer Mediated Three-Dimensional Network of Graphene Foam. RSC Adv. 2014, 4, 50074–50080. [Google Scholar] [CrossRef]
- Melia, G.; Siegkas, P.; Levick, J.; Apps, C. Insoles of Uniform Softer Material Reduced Plantar Pressure Compared to Dual-Material Insoles during Regular and Loaded Gait. Appl. Ergon. 2021, 91, 103298. [Google Scholar] [CrossRef]
- Nouman, M.; Dissaneewate, T.; Leelasamran, W.; Chatpun, S. The Insole Materials Influence the Plantar Pressure Distributions in Diabetic Foot with Neuropathy during Different Walking Activities. Gait Posture 2019, 74, 154–161. [Google Scholar] [CrossRef]
- Zuñiga, J.; Moscoso, M.; Padilla-Huamantinco, P.G.; Lazo-Porras, M.; Tenorio-Mucha, J.; Padilla-Huamantinco, W.; Tincopa, J.P. Development of 3D-Printed Orthopedic Insoles for Patients with Diabetes and Evaluation with Electronic Pressure Sensors. Designs 2022, 6, 95. [Google Scholar] [CrossRef]
- Muir, B.C.; Li, J.-S.; Hudak, Y.F.; Kaufman, G.E.; Cullum, S.; Aubin, P.M. Evaluation of Novel Plantar Pressure-Based 3-Dimensional Printed Accommodative Insoles—A Feasibility Study. Clin. Biomech. 2022, 98, 105739. [Google Scholar] [CrossRef]
- Shi, Q.Q.; Li, P.L.; Yick, K.L.; Li, N.W.; Jiao, J. Effects of Contoured Insoles with Different Materials on Plantar Pressure Offloading in Diabetic Elderly during Gait. Sci. Rep. 2022, 12, 15395. [Google Scholar] [CrossRef]
- Cheung, J.T.M.; Zhang, M. Parametric Design of Pressure-Relieving Foot Orthosis Using Statistics-Based Finite Element Method. Med. Eng. Phys. 2008, 30, 269–277. [Google Scholar] [CrossRef]
- Peng, Y.; Wong, D.W.-C.; Chen, T.L.-W.; Wang, Y.; Zhang, G.; Yan, F.; Zhang, M. Influence of Arch Support Heights on the Internal Foot Mechanics of Flatfoot during Walking: A Muscle-Driven Finite Element Analysis. Comput. Biol. Med. 2021, 132, 104355. [Google Scholar] [CrossRef]
- Tang, L.; Wang, L.; Bao, W.; Zhu, S.; Li, D.; Zhao, N.; Liu, C. Functional Gradient Structural Design of Customized Diabetic Insoles. J. Mech. Behav. Biomed. Mater. 2019, 94, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Jin, L. The Influence of Different Footwear Insole Stiffness on Center of Pressure and Ankle Kinematics during Walking: A Case Report. Biomechanics 2022, 2, 205–212. [Google Scholar] [CrossRef]
- Iacob, M.C.; Popescu, D.; Petcu, D.; Marinescu, R. Assessment of the Flexural Fatigue Performance of 3D-Printed Foot Orthoses Made from Different Thermoplastic Polyurethanes. Appl. Sci. 2023, 13, 12149. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).