Abstract
This study evaluates the biomechanical efficacy of clear aligners in closing anterior maxillary diastemas using enhanced force systems. While clear aligners offer esthetic and functional benefits, their predictability in controlling bodily movement and torque remains limited. This research investigates the effects of structural modifications, such as the addition of flowable resin to interdental embrasures and intrusive force application, on the force and moment characteristics during mesial bodily movement of maxillary central incisors. Experiments were conducted using 3D-printed maxillary models with a 6-axis force/torque sensor under controlled conditions. Four experimental groups were tested: Group 1 (0.3 mm mesial bodily shift), Group 2 (0.3 mm mesial shift + 0.1 mm intrusion), Group 3 (0.3 mm mesial shift with resin reinforcement), and Group 4 (0.3 mm mesial shift + 0.1 mm intrusion with resin reinforcement). The results showed that Groups 1 and 3 exhibited extrusive forces, while Groups 2 and 4 exhibited intrusive movement with minimized extrusion. Resin reinforcement significantly increased mesiodistal force application and reduced unwanted tipping and rotational moments, improving bodily movement efficiency. The addition of intrusive movement minimized extrusive forces but introduced a minor lingual inclination. The combination of both modifications provided the most controlled and efficient tooth movement. These results suggest that modifying clear aligners with localized structural enhancements can improve treatment predictability and efficiency. Clinically, the application of flowable resin enhancements offers a simple and effective approach to optimizing clear aligner therapy.
1. Introduction
The clinical use of clear aligners (CAs) is increasing as an alternative to traditional fixed orthodontic appliances due to their esthetics, convenience, and ease of oral hygiene [1,2,3]. In particular, advances in materials science and the incorporation of digital technologies, such as CAD-CAM technology, intraoral scanning, and 3D printing, have simplified the fabrication of CAs and expanded their clinical applications [4,5]. However, while CAs have demonstrated effective results in the treatment of intrusion, distal bodily shift in molars, and retraction of incisors, they still have limited predictability in the treatment of incisor bodily shift and torque control, and the mechanics of the forces and moments that cause tooth movement remain insufficiently understood [6].
Diastema is the presence of space between two adjacent teeth and has both esthetic and functional significance clinically. In esthetic terms, diastema can negatively affect a patient’s facial appearance and self-esteem, and in functional terms, it can increase the risk of periodontal disease by promoting the deposition of food residue and calculus formation [7]. Recently, the use of CAs has been increasing as a treatment modality for diastema, but previous studies have shown that space closure involving incisor and canine movement with CAs can result in unwanted extrusive and rotational forces in addition to mesiodistal forces upon initial force application, which can further complicate treatment by causing tooth tipping and occlusal interference [8,9].
Despite these findings, there is still a lack of quantitative understanding regarding force distribution and movement control during diastema closure with CAs. While previous research has identified issues such as uncontrolled tipping and rotational moments, the precise biomechanical mechanisms governing these movements remain unclear. Additionally, it is not well understood how structural modifications, such as localized reinforcements or the incorporation of intrusive forces, can improve bodily movement control and reduce unwanted forces [10].
While additional appliances such as attachments, power arms, and mini-implants can be used for effective tooth movement, they have limitations that increase the complexity of the treatment process and prolong the treatment time. In particular, attachments have limited application to the prosthetic surface, power arms can cause a foreign body sensation and poor esthetics, and mini-implants are at risk of inflammation and dislodgment. Structural design variations in CAs have been proposed as an alternative to overcome these limitations. Structural design modifications include the utilization of existing attachments, subgingival extension of the margins of CAs, adjustment of the device thickness, and creation of an enhanced structure by adding flowable resin directly to the interdental embrasure. A recent study by Jin X et al. reported that adding flowable resin locally to the molar region increased the stiffness of the appliance, altered the distribution of forces applied to the molar region, and enabled force transfer closer to the center of resistance [11].
However, although adjusting the overall thickness of the CAs affects the characteristics of the forces transmitted to the entire dentition, increasing the localized thickness of the aligners can improve the stiffness of the desired area, allowing for the precise control of the targeted tooth movement [12,13]. Despite these advancements, there is still limited experimental data on how such modifications specifically affect the force and moment system during diastema closure. Furthermore, the potential benefits of combining structural reinforcements with intrusive forces for optimizing space closure efficiency have not been fully explored.
In orthodontic treatment, force/moment measurement is essential for accurate prediction of tooth movement patterns and effective application of biomechanical principles. Force/moment measurement systems utilize sensors to measure the forces and moments applied to teeth in three dimensions under various conditions in real time, allowing for precise biomechanical analysis [14,15]. This can aid in understanding orthodontic forces, achieving targeted tooth movement, and minimizing collateral side effects.
To address these gaps, this study aims to analyze how structural modifications, specifically the addition of flowable resin and intrusive forces, influence force transmission and movement control in maxillary central incisor diastema closure. This study hypothesized that structural modifications to CAs, specifically the addition of flowable resin to the interdental area and the incorporation of intrusive forces, would improve the mesial movement of incisors during maxillary central incisor diastema closure, minimize unwanted tilting and rotational moments, and improve the predictability of body movement. To test this hypothesis, a 3D-printed maxillary model equipped with 6-axis force/torque sensors was used to compare closure protocols for maxillary central incisor mesial bodily movement (0.3 mm mesial bodily movement with or without 0.1 mm intrusive movement) and the reinforcing structure (flowable resin addition) on the forces (Fx, Fy, Fz) and moments (Mx, My, Mz) generated during tooth movement after placement of CAs for maxillary central incisor diastema closure. The results of this study should provide biomechanical insights that may improve the clinical effectiveness of CA treatment.
2. Materials and Methods
2.1. Forces/Moments Measurement Apparatus Design and Fabrication
The maxillary dentition models were obtained by scanning a Nissin dental model (NISSIN B3-305, Nissin Dental Product, Kyoto, Japan) with a high-resolution TRIOS 4 intraoral scanner (3Shape TRIOS A/S, Copenhagen, Denmark) for precise digital impressions. The resulting STL files were processed using Meshmixer (Autodesk Inc., San Francisco, CA, USA) for standardization, including artifact removal and alignment correction. The final models were 3D printed using G10-Br (Gruck, Seoul, Republic of Korea). To increase reproducibility, the same digital workflow and printing parameters were applied to each experimental setup to create identical models under all test conditions.
A 6-axis miniature force/torque sensor (Aidin Robotics, Seoul, Republic of Korea) was connected to measure the forces and moments exerted by the CA on the maxillary left central incisor dentition model, and calibration followed the manufacturer’s recommended protocol and repeated calibration tests were performed to minimize system error (Figure 1).
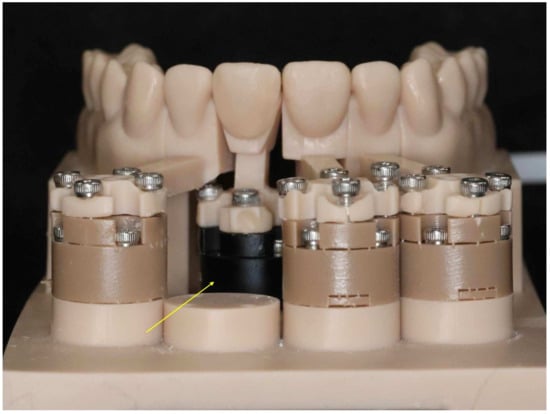
Figure 1.
Experimental apparatus design. The maxillary dentition model was set with spaces between the central incisors, and the maxillary left central incisor was connected to a six-axis miniature force/torque sensor (yellow arrow).
To comprehensively evaluate the biomechanical effects of diastema closure, all six force and moment components (Fx, Fy, Fz, Mx, My, and Mz) were measured. Although Fy represents the primary intended movement, actual tooth displacement occurs in a three-dimensional pattern due to continuous contact changes between the aligner and tooth surfaces. Measuring Fx and Fz enabled the quantification of unintended forces that may influence treatment outcomes. Similarly, Mx, My, and Mz moments were analyzed to assess rotational effects, distinguishing between bodily movement and tipping. This selection was based on a previous finite element analysis study [9], which demonstrated that even with planned unidirectional movement, CAs induce complex force distributions across multiple planes (Table 1).

Table 1.
Sign convention of force and moments system.
To ensure measurement consistency, we standardized the sensor mounting, calibration, and data acquisition procedures. The sensor was calibrated before each session following the manufacturer’s protocol, and the same mounting procedure was applied across all test specimens. All measurements were conducted at a controlled temperature (37 °C) to minimize variability and ensure reliable data across groups.
Forces and moments were measured by mounting a CA made from thermoforming material (polyethylene terephthalate glycol, PETG) (Flexera, GwangMyeong Co., Seoul, Republic of Korea) on the experimental device and maintaining it at 37 °C, the temperature of the oral cavity, for 10 min using a Forced Convection Incubator (C-INDF, Changshin Science, Seoul, Republic of Korea), and then recording the average value of the measured forces and moments for the next 1 min for analysis.
2.2. Design Modification and Fabrication of the Experimental CA for Mesial Bodily Shift in Maxillary Left Central Incisor
In this study, in order to close the diastema closure between the maxillary central incisors, the CA was designed into 4 groups to measure the force and moment exerted on the maxillary central incisor by the CA (experimental group) according to whether the maxillary central incisor was intruded or not and the enhanced structure added to the buccal interdental embrasure of the CA (Figure 2). Since the maxillary model is left/right symmetrical, the experiment was conducted on the left central incisor.
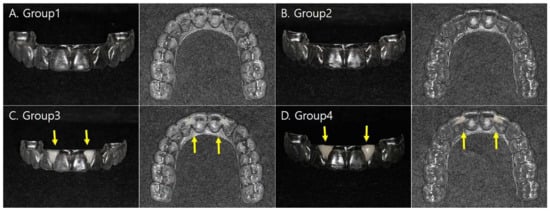
Figure 2.
Designs of three-dimensional maxillary dental models for the fabrication of the clear aligners. (A) Group 1: 0.3 mm mesial bodily movement of maxillary left central incisor; (B) Group 2: 0.3 mm mesial bodily movement of maxillary left central incisor + 0.1 mm intrusive movement; (C) Group 3: 0.3 mm mesial bodily movement of maxillary left central incisor with enhanced structure (direct flowable resin adding, yellow arrows); (D) Group 4: 0.3 mm mesial bodily movement + 0.1 mm intrusive movement of maxillary left central incisor with enhanced structure (direct flowable resin adding, yellow arrows).
Group 1: 0.3 mm mesial bodily movement of maxillary left central incisor.
Group 2: 0.3 mm mesial bodily movement of maxillary left central incisor + 0.1 mm intrusive movement.
Group 3: 0.3 mm mesial bodily movement of maxillary left central incisor with enhanced structure (direct flowable resin adding).
Group 4: 0.3 mm mesial bodily movement + 0.1 mm intrusive movement of maxillary left central incisor with enhanced structure (direct flowable resin adding).
The experimental CAs were fabricated via thermoforming using 0.75 mm thick PETG, with 20 pieces made for each experimental group (80 pieces in total). The sample size for this study was determined using a four-group one-way ANOVA with a significance level (α) of 0.05, explanatory power (1-β) of 0.80, and a medium effect size (f = 0.25), referencing a previous study by Choi et al. [16]. It was determined that a minimum of 18 samples per group was required. To account for potential attrition and to ensure statistical robustness, 20 CAs were selected per experimental group, for a total of 80 CAs.
The enhanced structure was added using a flowable resin (Charmfil, Denkist, Gunpo-si, Republic of Korea) by filling the buccal embrasure areas of the maxillary central incisors and lateral incisors on the outer surface of the CAs. The addition procedure consisted of sandblasting for 10 s, pretreatment with adhesive (3MTM AdperTM ScotchbondTM Multi-purpose adhesive, 3M, Saint Paul, MN, USA), photopolymerization for 20 s, application of flowable resin, and followed by photopolymerization.
2.3. Statistical Analysis
All measured force and moment values did not follow a normal distribution; data were described as median and interquartile range (IQR). Comparisons between groups were performed using the Kruskal–Wallis test with Bonferroni post hoc tests. All statistical analyses were performed using the R language (R Foundation for Statistical Computing, Vienna, Austria), and statistical significance was assessed at the p < 0.05 level.
3. Results
The results of this study evaluated the forces and moments exerted on the maxillary central incisors during the mesial movement of the maxillary central incisors, depending on the tooth movement settings and the structurally reinforced CAs, and compared the differences between the four experimental groups. The directions of the experimental variables (forces and moments) obtained from multiple axes were separated by +/− signs. (Table 1).
Statistical analysis confirmed significant differences between groups in all experimental variables (Fx, Fy, Fz and Mx, My, and Mz) (p < 0.001) (Table 2).

Table 2.
Comparative analysis of the forces and moments generated by different clear aligner groups.
3.1. Forces
3.1.1. Fx (Labiolingual Force, (+): Labial Force, (−): Lingual Force)
Group 2 showed the least lingual force at −1.74 N. This suggests that the 0.3 mm mesial bodily shift and 0.1 mm intrusive shift during space closure contributed to the decrease in lingual force. Groups 1, 3, and 4 had statistically similar levels of lingual forces (p < 0.001), with Group 3 having the largest lingual force of −3.01 N with an enhanced structure without intrusive forces.
3.1.2. Fy (Mesiodistal Force, (+): Mesial Force, (−): Distal Force)
Group 2, which only applied the intrusive force, showed a significantly lower mesial force of 0.16 N than the other groups (p < 0.001), while Group 3, which only applied the structural enhancement, had the highest proximal force value of 0.31 N. Group 1 (0.26 N) and Group 4 (0.27 N) had relatively similar values, and these results show that the combination of structural strengthening and intrusive movement conditions had a significant effect on Fy, respectively. In other words, when 0.1 mm of intrusive force was applied, the mesial force decreased, while the structural enhancement with resin addition increased the mesial force.
3.1.3. Fz (Vertical Force, (+): Extrusion Force, (−): Intrusion Force)
In the vertical force, Groups 1 and 3, where no intrusive force was applied to the CAs, showed an extrusion force, and Group 3, where the reinforced structure was applied, showed a greater force, although not significant. On the other hand, Groups 2 and 4 with 0.1 mm intrusion showed intrusive forces, with greater intrusive forces observed in Group 4 with the enhanced structure. The amount of change in the vertical direction was smaller in Groups 2 and 4 with 0.1 mm intrusive force than in Groups 1 and 3 and was close to zero, which means that if only the bodily movement in the mesial direction is planned for diastema closure, the extrusive force will be generated, so additional movement in the intrusive direction can reduce the extrusive force.
3.2. Moments
3.2.1. Mx (Mesiodistal Angulation Moment, (+): Distal Tipping Moment, (−): Mesial Tipping Moment)
Mx represents the mesiodistal rotational force along the long axis of the tooth. Groups 3 and 4 with enhanced structures had significantly smaller mesial tipping moments than Groups 1 and 2. Group 2, which only added an intrusive force, had the largest mesial tipping moment of −12.43 Nmm, followed by Group 1 with −10.70 Nmm. Therefore, the application of enhanced structures can reduce mesiodistal tipping.
3.2.2. My (Labiolingual Inclination Moment, (+): Labial Inclination Moment, (−): Lingual Inclination Moment)
Group 2, which was given only the intrusive movement, had the only lingual inclination moment value of −2.273 Nmm, which was significantly different (p < 0.001). In other words, when the intrusive movement was added, a lingual inclination moment occurred. However, in Group 4, which was given structural enhancement even with the intrusive movement, a labial inclination moment occurred. Group 3, which only applied structural reinforcement, had the largest labial inclination moment of 2.97 Nmm, indicating that the structural enhancement contributed to increasing the net labial rotation force.
3.2.3. Mz (Rotational Moment, (+): Mesial (Mesial-In) Rotational Moment, (−): Distal (Mesial-Out) Rotational Moment)
Mz represents the rotation moment in the occlusal plane of the tooth. Group 4, with both the enhanced structure and 0.1 mm of intrusive movement, recorded the smallest rotational moment, significantly at −12.50 Nmm, indicating a decrease in mesial-out rotational force. Groups 3 and 4 with enhanced structures observed relatively smaller rotation moments compared to Groups 1 and 2.
4. Discussion
In this study, we analyzed the tooth movement forces and moments during CA treatment for maxillary midline diastema closure with and without enhanced structure and intrusive movement. Although CAs are widely used due to their esthetics and convenience, it is known that the accuracy and predictability of tooth movement are limited due to the low stiffness of the appliance [12,13,15]. In particular, the thermoplastic material of CAs exhibits viscoelastic behavior, which has elastic and plastic properties [15], which can lead to difficulties in achieving the intended tooth movement. However, implementing structural modifications that increase the thickness of certain areas of the CAs, as in this study, may help to achieve the planned tooth movement. Baik et al. reported that the forces and moments generated during tooth movement can be controlled by changing the design of CAs using 3D printing [17]. Although this study used CAs fabricated by thermoforming, the addition of enhanced structures changed the distribution of forces and moments during tooth movement.
Recently, the materials for CAs have diversified, and direct 3D-printed CAs made from materials such as TC-85 (Graphy Inc., Seoul, Republic of Korea) have been commercialized. However, the most commonly used CAs in clinical practice are still thermoplastic materials, typically 0.75 mm thick. Although different manufacturers use slightly different materials, common compositions include polyurethane, polymethyl methacrylate (PMMA), and polyethylene terephthalate glycol (PETG). In this study, we used PETG, a thermoplastic material with a thickness of 0.75 mm, which is representative of the most commonly used clinical CAs. Thus, the experimental setup used in this study is likely to reflect the physical properties of CAs commonly used in clinical practice, which has meaningful implications for clinical application. Future studies should consider evaluating different thicknesses and material properties to provide a more comprehensive comparison.
The increasing interest in CA treatment is evident in bibliometric analyses that highlight research trends in removable orthodontic appliances, biomechanics, and predictability of tooth movement [18]. These studies emphasize the importance of experimental validation, particularly in force and moment analysis, which is consistent with the focus of our study. Our findings contribute to this growing field of knowledge by providing experimental evidence for the biomechanical efficiency of structural modifications in diastema closure.
The results of the simulation of the mesial movement of maxillary central incisors with four groups of CAs showed that the largest mesiodistal force (Fy), which is most related to the direction of tooth movement for diastema closure, was generated in Group 3 with the enhanced structure. This is consistent with previous studies that have shown a strong correlation between the thickness of the CAs and the force transmitted [12,13]. In particular, the enhanced structure generated greater forces with increasing thickness of the interproximal area, which Cheng et al. reported [19], the thicker the CAs, the less deformation of the appliance, and the stronger the adjustment force for the same size of deformation, resulting in a more uniform distribution of forces on the PDL surface.
For the vertical force (Fz), Groups 1 and 3, which were not subjected to an intrusive force, generated an extrusive force, which is similar to what is commonly observed with conventional fixed appliances. Previous studies have reported that in treatment with fixed appliances, mesial tipping can result in inclination movement, which can result in a wedge effect in the occlusion due to the application of an occlusal force [20]. However, in the present study, intrusive forces were observed in Groups 2 and 4, which were given 0.1 mm of intrusive movement, and greater intrusive forces occurred in Group 4, where both enhanced structure and intrusive forces were applied. This shows that the increased stiffness of the appliance with the enhanced structure, along with the “bite block” effect of CA, contributes to a more effective achievement of the planned tooth movement [21,22].
Tooth movement in orthodontic treatment can exhibit various movement patterns depending on the center of resistance (CR) and the point, magnitude, and vector at which the force is applied [23]. In particular, uncontrolled tipping is the most common type of tooth movement due to the nature of orthodontic treatment, where forces are applied to the crown [24], and for bodily movement, a more significant force should be applied to the cervical region to provide an appropriate moment [25]. However, in thermoformed CAs, the cervical region is the most vulnerable part due to deformation and irregularities [26,27], so applying an appropriate force to the cervical region in CA treatment has been a challenge.
The mesiodistal angulation moment (Mx) results of this study showed that the mesial tipping moment was significantly reduced in Groups 3 and 4 with the enhanced structure. This finding is consistent with the results of Jin X et al. [11], who found that extending the margin of the CA or the enhanced structure prevented the tooth from tipping and distributed the stress more evenly across the PDL, reducing adverse effects such as the ’roller coast effect’. This showed that applying structural enhancement can reduce unwanted tipping and rotational moments, which can contribute to stable bodily movement to control tooth movement. Regarding the labiolingual inclination moment (My), the labial inclination moment increased in the groups with the enhanced structure.
Regarding the labiolingual inclination moment (My), the labial inclination moment increased in the groups with the enhanced structure. This is believed to be due to the increased stiffness of the CA, which reduces appliance deformation and allows for a more effective grasp of the interproximal undercuts, thus reducing the constant change in contact point between the appliance and the tooth [28,29,30], which is expected to prevent unwanted lingual inclination. However, the minor lingual inclination observed in Group 4 warrants careful clinical consideration. Our results indicate that integrating an intrusive force component reduced lingual tipping during diastema closure, as seen in the reduced lingual force in Groups 2 and 4 compared to their respective controls (Groups 1 and 3). This suggests that intrusion may help counteract unwanted lingual inclination, leading to improved control of bodily movement. Clinically, this effect can enhance functional occlusion, maintain a natural smile arc, and contribute to long-term stability by reducing the risk of relapse. These findings highlight the importance of incorporating intrusion into treatment planning, particularly for patients with deep bites or strong perioral muscle forces, where excessive lingual inclination may be undesirable.
This is believed to be due to the increased stiffness of the CA, which reduces appliance deformation and allows for a more effective grasp of the interproximal undercuts, thus decreasing the constant change in contact point between the appliance and the tooth [28,29,30], which is expected to prevent unwanted lingual inclination.
However, Rossini et al. reported [31] that CAs have limitations associated with the control of extrusion and rotation, as well as low prediction accuracy for tooth movement in certain directions where pulling forces such as space closure are applied. The results of the Fz analysis in this study also showed that if an additional 0.1 mm of intrusive movement was not designed, the angulation tipping of the tooth caused unexpected extrusion forces, which may appear as limitations, such as premature occlusal contact and limited tooth movement during the treatment process. To compensate for this, consideration should be given to the tooth movement plan, and the addition of intrusive movement in Groups 2 and 4 resulted in a significant intrusive movement. The enhanced structure method with flowable resin used in this study has the advantage of easy clinical application. The conventional CA fabrication method, thermoforming, may not be uniform in thickness during the fabrication process [32,33], and when modifications to the treatment are required, it is cumbersome to remake the appliance, and direct 3D printing requires additional design work. On the other hand, the flowable resin approach has the advantage that it can be applied immediately in the clinic and can be modified as needed during treatment.
To better understand the impact of flowable resin reinforcement, it is important to consider its mechanical properties. Chamfil Flow (Denkist, Republic of Korea) is a nano-based, light-cured composite with radiopaque properties and low polymerization shrinkage, enhancing stability and reducing deformation. However, it has lower microhardness and shear bond strength (1.9 MPa) compared to Filtek XTE (16.8 MPa), leading to weaker adhesion and reduced rigidity. Resin reinforcement increased mesiodistal force application and reduced unwanted tipping and rotation, improving force distribution. Future studies should explore resins with higher mechanical strength and adhesion for optimal aligner modifications.
This study has several limitations. First, as an in vitro study, it does not fully replicate clinical conditions, where factors like bone density, periodontal ligament compliance, occlusal forces, and intraoral temperature changes can affect aligner performance [18]. Future studies should incorporate dynamic models or clinical trials. Second, CAs may degrade over time, altering force transmission and treatment predictability [11]. Long-term intraoral studies are needed to assess their biomechanical stability. Third, the flowable resin used in this study has lower microhardness and shear bond strength compared to other dental composites. While it enhances force application, its relatively low stiffness and adhesion may limit its reinforcement effect. Variability in resin thickness during application may also introduce minor inconsistencies in force distribution. Standardizing enhancement methods and testing alternative resins with higher rigidity could improve reproducibility and effectiveness. Fourth, attachments were not considered despite their role in bodily movement [9]. Future studies should evaluate the combined effects of enhanced structures and attachments. Finally, this study focused on a single tooth, while real treatments involve multiple teeth and occlusal interactions. Clinical trials incorporating these factors are necessary to validate the findings.
Based on these limitations, future research should explore several key areas. First, in vivo clinical trials should be conducted to validate the findings in real treatment conditions, considering physiological factors such as bone density, occlusal forces, and saliva exposure. Second, long-term studies on the mechanical stability of structurally modified aligners will help determine their durability and effectiveness over extended treatment periods. Third, integrating finite element analysis with experimental models can provide deeper insights into force distribution and aligner performance. Lastly, optimizing the combination of attachments and structural modifications may further improve control over bodily movement and minimize unwanted tipping and rotation.
5. Conclusions
This study experimentally demonstrated that the precision of tooth movement during diastema closure can be improved by adjusting the design of the CA. In particular, as a strategy to compensate for the limitations of CAs reported in previous studies, we found that the application of enhanced structure can reduce unwanted forces or unnecessary tipping that may occur during mesial bodily movement. Clinically, this has implications in that structural enhancement can be applied to specific areas of the CA to increase the efficiency of bodily movement and induce more precise tooth movement. The results of this study also enable a more accurate prediction of the changes in forces and moments that occur during diastema closure and the fabrication of CAs that take this into account, which could play an important role in optimizing orthodontic treatment outcomes.
Author Contributions
Conceptualization, Y.-K.C. and Y.-I.K.; methodology, M.-J.J., Y.-K.C., S.-H.K. and S.-S.K.; formal analysis, Y.-K.C., S.-H.K., S.-S.K. and Y.-I.K.; writing—original draft preparation, M.-J.J., S.-S.K., Y.-K.C. and Y.-I.K.; writing—review and editing, Y.-K.C., S.-H.K., S.-S.K., S.-B.P. and Y.-I.K.; funding acquisition, Y.-K.C. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Dental Research Institute (PNUDH DRI-2025-04), Pusan National University Dental Hospital.
Institutional Review Board Statement
Ethical approval was not required for this study as it did not involve human participants or animal subjects.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data supporting the findings of this study will be available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CA | Clear Aligners |
| CAD | Computer-Aided Design |
| CAM | Computer-Aided Manufacturing |
| PETG | Polyethylene terephthalate glycol |
References
- Gu, J.F.; Tang, J.S.Y.; Skulski, B.; Fields, H.W.; Beck, F.M.; Firestone, A.R.; Kim, D.G.; Deguchi, T. Evaluation of Invisalign treatment effectiveness and efficiency compared with conventional fixed appliances using the Peer Assessment Rating index. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 259–266. [Google Scholar]
- Gao, M.; Yan, X.; Zhao, R.; Shan, Y.; Chen, Y.; Jian, F.; Long, H.; Lai, W. Comparison of pain perception, anxiety, and impacts on oral health related quality of life between patients receiving clear aligners and fixed appliances during the initial stage of orthodontic treatment. Eur. J. Orthod. 2021, 43, 353–359. [Google Scholar] [PubMed]
- Zhao, R.; Huang, R.; Long, H.; Li, Y.; Gao, M.; Lai, W. The dynamic of the oral microbicome and oral health among patients receiving clear aligner orthodontic treatment. Oral Dis. 2020, 26, 473–483. [Google Scholar]
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores, M.C. Effectiveness of clear aligner therapy for orthodontic treatment: A systematic review. Orthod. Craniofac. Res. 2020, 23, 133. [Google Scholar]
- Papadimitriou, A.; Mousoulea, S.; Gkantidis, N.; Kloukos, D. Clinical effectiveness of Invisalign® orthodontic treatment: A systematic review. Prog. Orthod. 2018, 19, 37. [Google Scholar]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Forces and moments generated by removable thermoplastic aligners: Incisor torque, premolar derotation, and molar distalization. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 728–736. [Google Scholar]
- Kurth, J.R.; Kokich, V.G. Open gingival embrasures after orthodontic treatment in adults: Prevalence and etiology. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 116–123. [Google Scholar] [CrossRef]
- Fan, Y.; Lv, X.; Wang, B.; An, L. Initial forces acting on the maxillary teeth with aligner activation of canine distalization on the basis of different initial canine tips in vitro. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 867–873. [Google Scholar]
- Yokoi, Y.; Arai, A.; Kawamura, J.; Uozumi, T.; Usui, Y.; Okafuji, N. Effects of Attachment of Plastic Aligner in Closing of Diastema of Maxillary Dentition by Finite Element Method. J. Healthc. Eng. 2019, 3, 1075097. [Google Scholar] [CrossRef]
- An, S.S.; Choi, Y.J.; Kim, J.Y.; Chung, C.J.; Kim, K.H. Risk factors associated with open gingival embrasures after orthodontic treatment. Angle Orthod. 2018, 88, 267–274. [Google Scholar] [CrossRef]
- Jin, X.; Tian, X.; Lee Zhi Hui, V.; Zheng, Y.; Song, J.; Han, X. The effect of enhanced structure in the posterior segment of clear aligners during anterior retraction: A three-dimensional finite element and experimental model analysis. Prog. Orthod. 2024, 25, 3. [Google Scholar] [CrossRef] [PubMed]
- Kohda, N.; Iijima, M.; Muguruma, T.; Brantley, W.A.; Ahluwalia, K.S.; Mizoguchi, I. Effects of mechanical properties of thermoplastic materials on the initial force of thermoplastic appliances. Angle Orthod. 2013, 83, 476–483. [Google Scholar] [PubMed]
- Hahn, W.; Dathe, H.; Fialka-Fricke, J.; Fricke-Zech, S.; Zapf, A.; Kubein-Meesenburg, D.; Sadat-Khonsari, R. Influence of thermoplastic appliance thickness on the magnitude of force delivered to a maxillary central incisor during tipping. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 12.e1–12.e7. [Google Scholar]
- Badawi, H.M.; Toogood, R.W.; Carey, J.P.; Heo, G.; Major, P.W. Three-dimensional orthodontic force measurements. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 518–528. [Google Scholar]
- Bichu, Y.M.; Alwaf, A.; Liu, X.; Andrews, J.; Ludwig, B.; Bichu, A.Y.; Zou, B. Advances in orthodontic clear aligner materials. Bioact. Mater. 2023, 22, 384–403. [Google Scholar]
- Choi, Y.-K.; Kim, S.-H.; Park, H.R.; Kim, S.-S.; Kim, Y.-I. Analysis of the Forces and Moments in Canine Bodily Movement with Different Clear Aligners’ Extraction Space Designs. Appl. Sci. 2024, 14, 7619. [Google Scholar] [CrossRef]
- Baik, J.C.; Choi, Y.K.; Cho, Y.; Baek, Y.; Kim, S.H.; Kim, S.S.; Park, S.B.; Kim, K.B.; Kim, Y.I. Evaluation of different designs of 3D printed clear aligners on mandibular premolar extrusion using force/moment measurement devices and digital image correlation method. Korean J. Orthod. 2024, 54, 359–373. [Google Scholar] [CrossRef]
- Grassia, V.; Fiori, A.; Diodati, F.; Sayahpour, B.; Jamilian, A.; Armogida, N.G.; d’Apuzzo, F.; Nucci, L. Clear aligners: A network and bibliometric analysis of 50 pivotal articles. Dent. Med. Probl. 2025, 62, 161–171. [Google Scholar]
- Cheng, Y.; Liu, X.; Chen, X.; Li, X.; Fang, S.; Wang, W.; Ma, Y.; Jin, Z. The three-dimensional displacement tendency of teeth-depending on incisor torque compensation with clear aligners of different thicknesses in cases of extraction: A finite element study. BMC Oral Health 2022, 22, 499. [Google Scholar]
- Al-Thomali, Y.; Basha, S.; Mohamed, R.N. Pendulum and modified pendulum appliances for maxillary molar distalization in Class II malocclusion a systematic review. Acta Odontol. Scand. 2017, 75, 394–401. [Google Scholar]
- Ravera, S.; Castroflorio, T.; Garino, F.; Daher, S.; Cugliari, G.; Deregibus, A. Maxillary molar distalization with aligners in adult patients: A multicenter retrospective study. Prog. Orthod. 2016, 17, 12. [Google Scholar] [PubMed]
- Caruso, S.; Nota, A.; Ehsani, S.; Maddalone, E.; Ojima, K.; Tecco, S. Impact of molar teeth distalization with clear aligners on occlusal vertical dimension: A retrospective study. BMC Oral Health 2019, 19, 182. [Google Scholar]
- Nanda, R.S.; Tosun, Y.S. Biomechanics in Orthodontics; Princ Pract. Hanover Park Quintessence Publ. Co.: Hanover Park, IL, USA, 2010. [Google Scholar]
- Yassir, Y.A.; Nabbat, S.A.; McIntyre, G.T.; Bearn, D.R. Clinical effectiveness of clear aligner treatment compared to fixed appliance treatment: An overview of systematic reviews. Clin. Oral Investig. 2022, 26, 2353–2370. [Google Scholar] [PubMed]
- Elshazly, T.M.; Salvatori, D.; Elattar, H.; Bourauel, C.; Keilg, L. Effect of trimming line design and edge extension of orthodontic aligners on force transmission: A 3D finite element study. J. Mech. Behav. Biomed. Mater. 2023, 140, 105741. [Google Scholar]
- Cowley, D.P.; Mah, J.; O’Toole, B. The effect of gingival margin design on the retention of thermoformed aligners. J. Clin. Orthod. 2012, 46, 697. [Google Scholar]
- Elshazly, T.M.; Keilig, L.; Salvatori, D.; Chavanne, P.; Aldesoki, M.; Bourauel, C. Effect of trimming line design and edge extension of orthodontic aligners on force transmission: An in vitro study. J. Dent. 2022, 125, 104276. [Google Scholar] [CrossRef]
- Gomez, J.P.; Peña, F.M.; Martínez, V.; Giraldo, D.C.; Cardona, C.I. Initial force systems during bodily tooth movement with plastic aligners and composite attachments: A three-dimensional finite element analysis. Angle Orthod. 2015, 85, 454–460. [Google Scholar]
- Guo, R.; Lam, X.Y.; Zhang, L.; Li, W.; Lin, Y. Biomechanical analysis of miniscrew-assisted molar distalization with clear aligners: A three-dimensional finite element study. Eur. J. Orthod. 2024, 46, cjad077. [Google Scholar]
- Lu, T.Y.; Ahmad, M.A.; Hassan, W.N.W.; Hariri, F. The stress and deformation effect of novel rapid maxillary expanders by finite element analysis. J. Med. Biol. Eng. 2022, 42, e397–e403. [Google Scholar]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–999. [Google Scholar] [CrossRef]
- Palone, M.; Longo, M.; Arveda, N.; Nacucchi, M.; Pascalis, F.D.; Spedicato, G.A.; Siciliani, G.; Lombardo, L. Micro-computed tomography evaluation of general trends in aligner thickness and gap width after thermoforming procedures involving six commercial clear aligners: An in vitro study. Korean J. Orthod. 2021, 51, 135–141. [Google Scholar] [PubMed]
- Bucci, R.; Rongo, R.; Levate, C.; Michelotti, A.; Barone, S.; Razionale, A.V.; D’Anto, V. Thickness of orthodontic clear aligners after thermoforming and after 10 days of intraoral exposure: A prospective clinical study. Prog. Orthod. 2019, 20, 36–43. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).