Examination of the Bond Strength of Retrograde Filling in Teeth with Failed Apical Resection After Retreatment
Abstract
1. Introduction
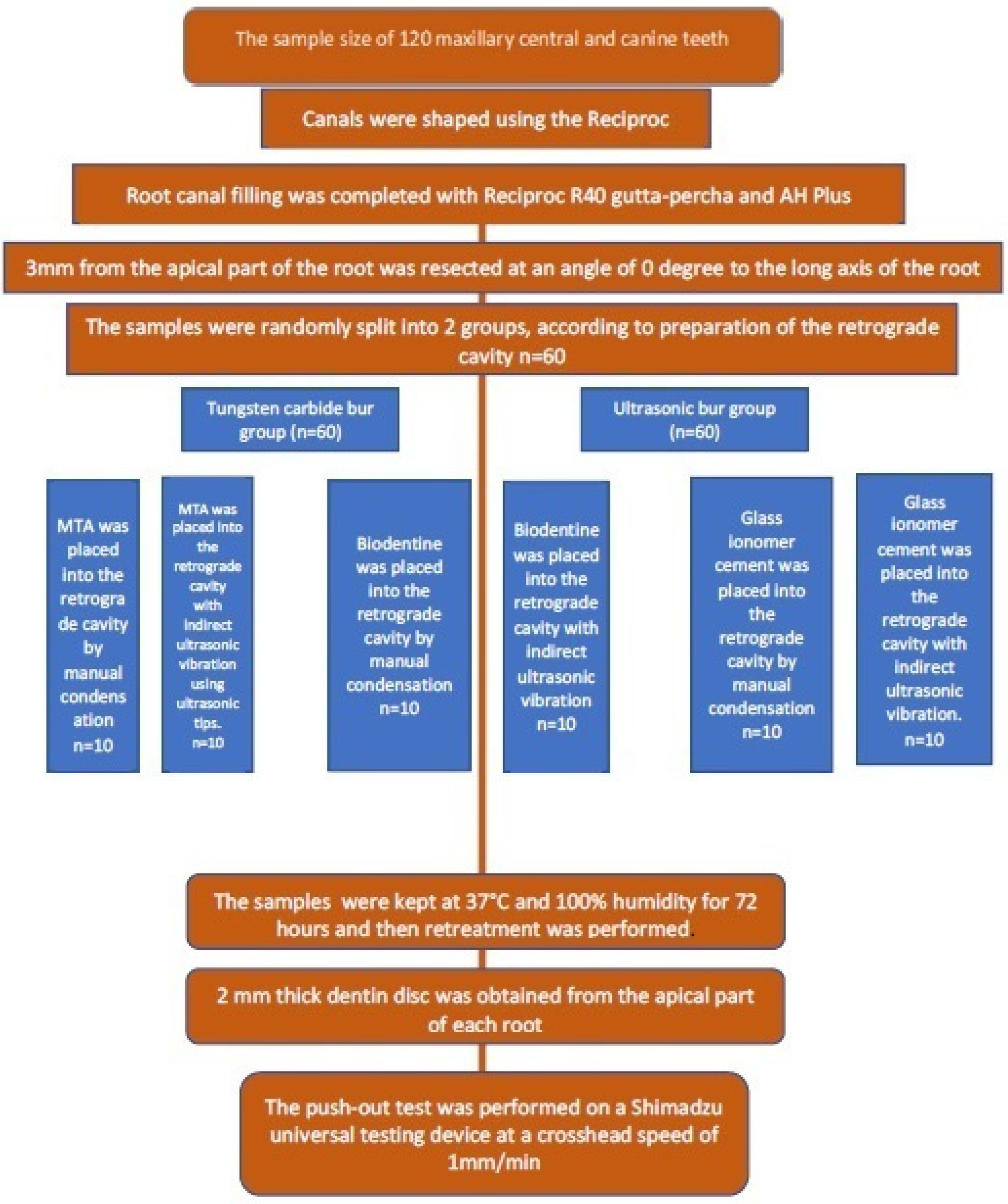
2. Materials and Methods
2.1. Ethics Committee Approval
2.2. Preparation of Experimental Teeth
- -
- Root tip development must be completed,
- -
- There should be no defects or signs of resorption at the root,
- -
- The root should not be too long, too short, too wide or too narrow,
- -
- Should not have more than 10 degrees of curvature,
- -
- Must be single-rooted and single-canal,
- -
- Root canal anatomy should not show variation,
- -
- Root canal treatment must not have been applied before,
- -
- No visible cracks or fractures on the root.
2.3. Preparation and Obturation of Root Canals
2.4. Apical Resection Procedure
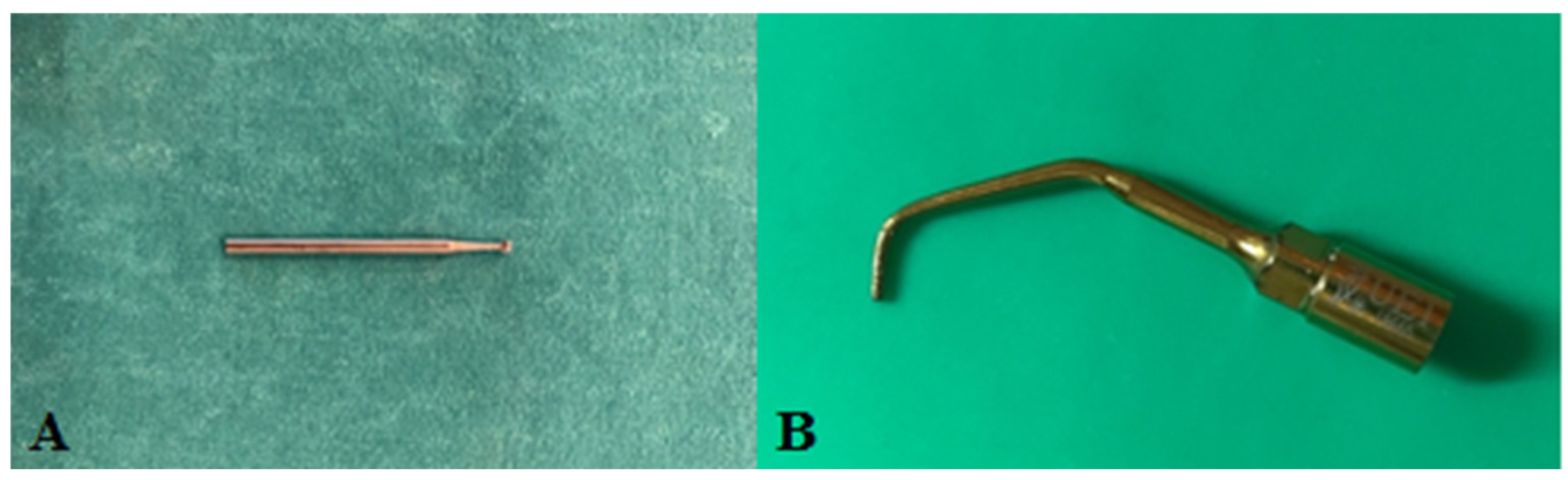
2.5. Retrograde Cavity Preparation
2.6. Retreatment Procedures
2.7. Sample Preparation and Push-Out Test
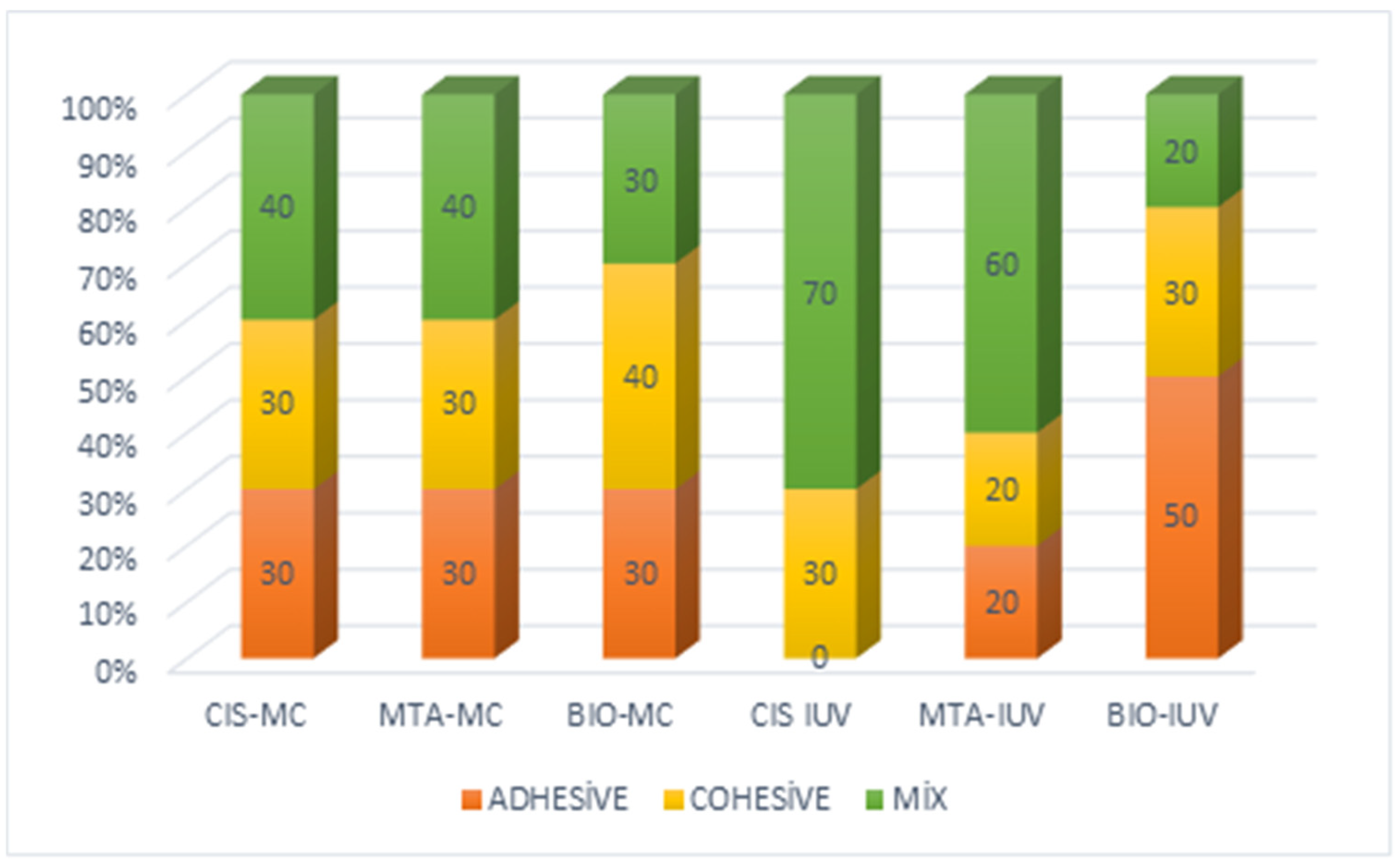
2.8. Analysis of Fracture Types
2.9. Statistical Analysis
3. Results
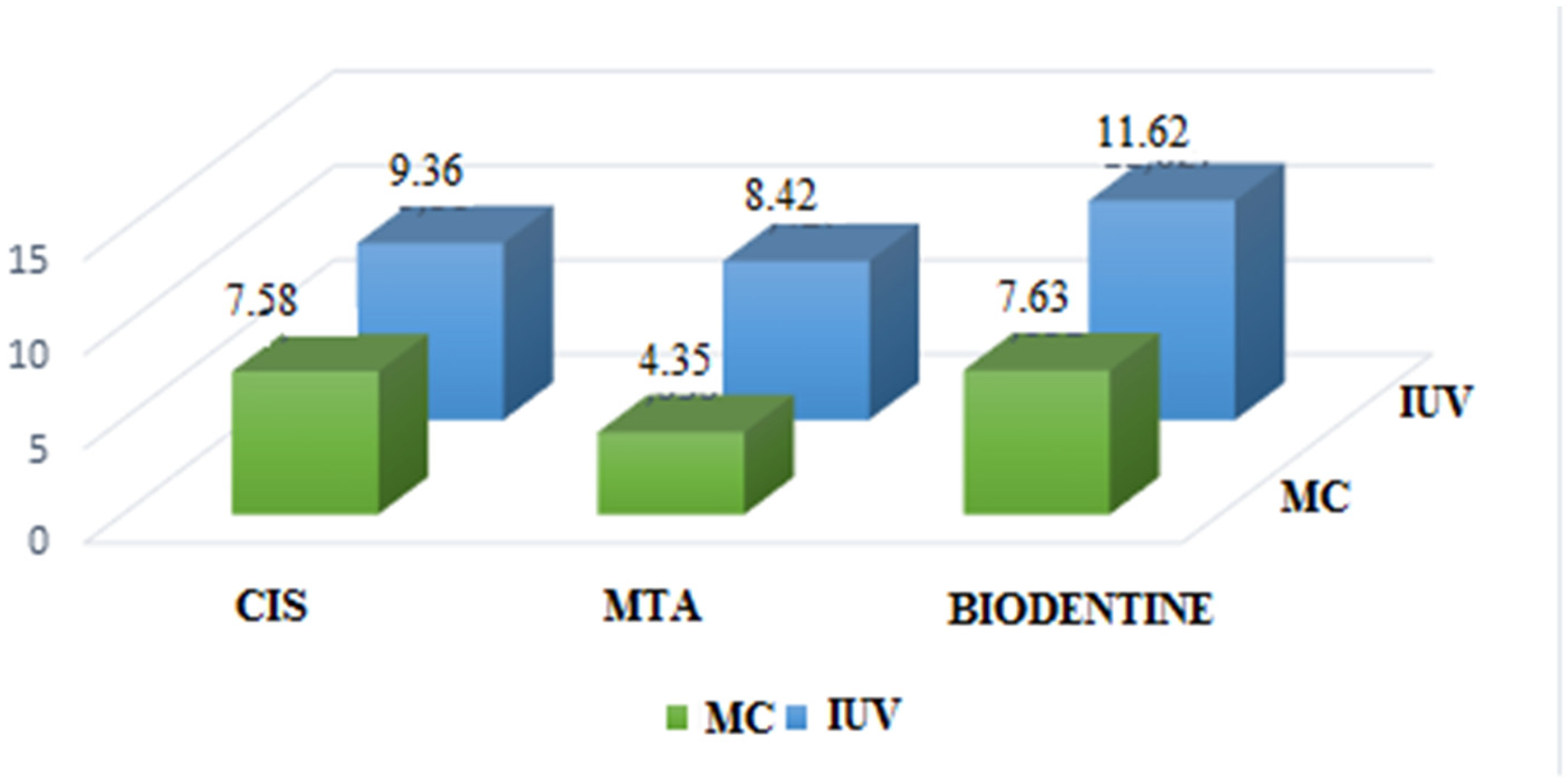
3.1. Bond Strength
3.2. Apical Reach
3.3. Stereomicroscope Analysis
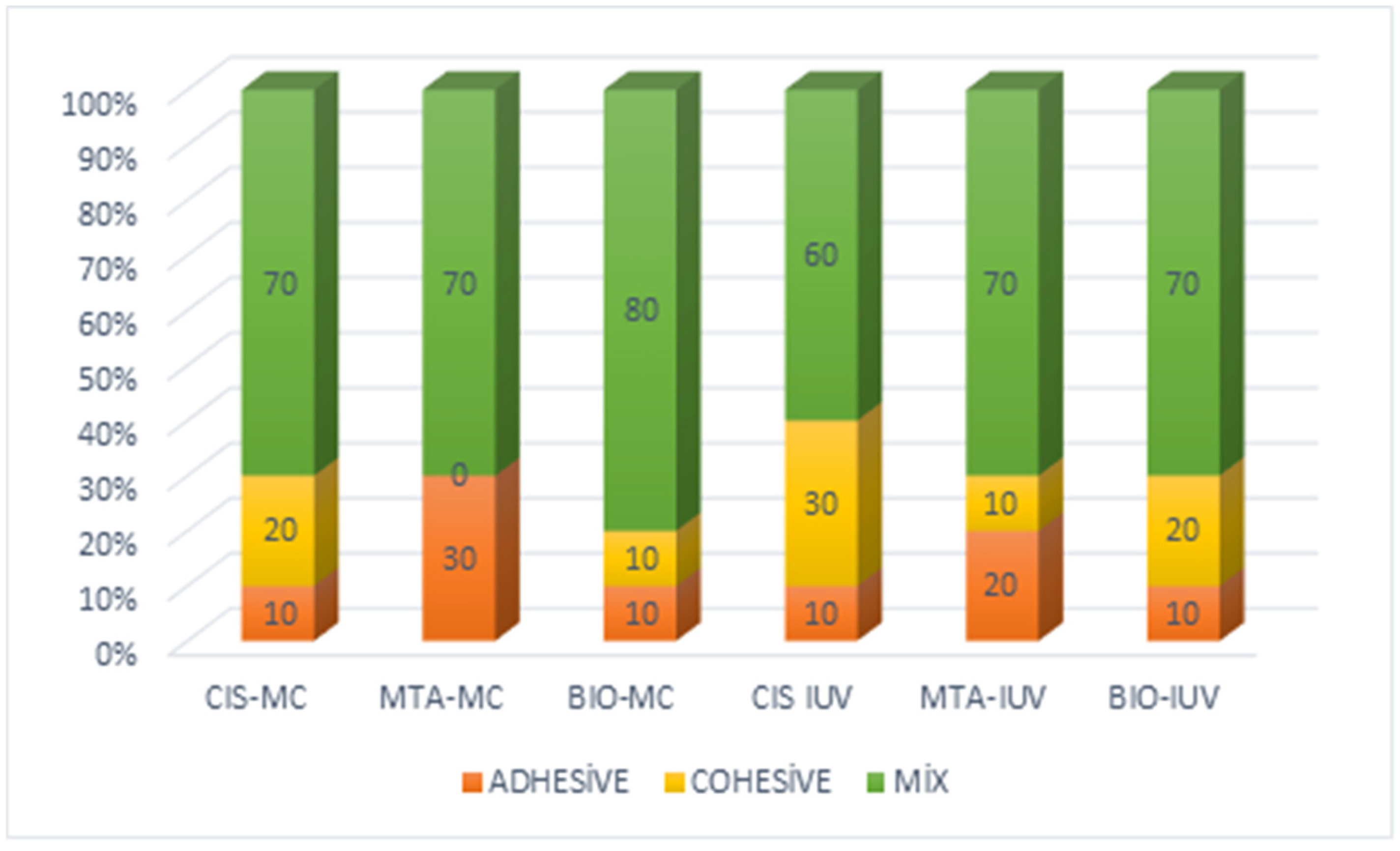
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kruse, C.; Spin-Neto, R.; Reibel, J.; Wenzel, A.; Kirkevang, L.L. Diagnostic validity of periapical radiography and CBCT for assessing periapical lesions that persist after endodontic surgery. Dentomaxillofac. Radiol. 2017, 46, 20170210. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Kratchman, S. Modern endodontic surgery concepts and practice: A review. J. Endod. 2006, 32, 601–623. [Google Scholar] [CrossRef]
- Chong, B.S.; Ford, T.R.; Kariyawasam, S.P. Tissue response to potential root-end filling materials in infected root canals. Int. Endod. J. 1997, 30, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Premjith; Shetty, D.; Kailar, A.; Pare, S.; Kumar, P.; Ragher, M. The Effect of Root End Cavity Preparation Using Er,Cr:YSGG Laser, Ultrasonic Retrotip, and Bur on the Apical Microleakage of Retrograde Cavity Filled with MTA Plus. J. Pharm. Bioallied Sci. 2020, 12, S299–S303. [Google Scholar] [CrossRef] [PubMed]
- Karlovic, Z.; Pezelj-Ribaric, S.; Miletic, I.; Jukic, S.; Grgurevic, J.; Anic, I. Erbium:YAG laser versus ultrasonic in preparation of root-end cavities. J. Endod. 2005, 31, 821–823. [Google Scholar] [CrossRef]
- Rubinstein, R.A.; Kim, S. Long-term follow-up of cases considered healed one year after apical microsurgery. J. Endod. 2002, 28, 378–383. [Google Scholar] [CrossRef]
- Torabinejad, M.; Watson, T.F.; Pitt Ford, T.R. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J. Endod. 1993, 19, 591–595. [Google Scholar] [CrossRef]
- Alsubait, S.A.; Hashem, Q.; AlHargan, N.; AlMohimeed, K.; Alkahtani, A. Comparative evaluation of push-out bond strength of ProRoot MTA, bioaggregate and biodentine. J. Contemp. Dent. Pract. 2014, 15, 336–340. [Google Scholar] [CrossRef]
- Prati, C.; Gandolfi, M.G. Calcium silicate bioactive cements: Biological perspectives and clinical applications. Dent. Mater. 2015, 31, 351–370. [Google Scholar] [CrossRef]
- Chong, B.S.; Pitt Ford, T.R.; Watson, T.F. Light-cured glass ionomer cement as a retrograde root seal. Int. Endod. J. 1993, 26, 218–224. [Google Scholar] [CrossRef]
- Friedman, S. The prognosis and expected outcome of apical surgery. Endod. Top. 2005, 11, 219–262. [Google Scholar] [CrossRef]
- de Chevigny, C.; Dao, T.T.; Basrani, B.R.; Marquis, V.; Farzaneh, M.; Abitbol, S.; Friedman, S. Treatment outcome in endodontics: The Toronto study—phases 3 and 4: Orthograde retreatment. J. Endod. 2008, 34, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.L.; Mann, V.; Gulabivala, K. Outcome of secondary root canal treatment: A systematic review of the literature. Int. Endod. J. 2008, 41, 1026–1046. [Google Scholar] [CrossRef]
- Dioguardi, M.; Stellacci, C.; La Femina, L.; Spirito, F.; Sovereto, D.; Laneve, E.; Manfredonia, M.F.; D’Alessandro, A.; Ballini, A.; Cantore, S.; et al. Comparison of Endodontic Failures between Nonsurgical Retreatment and Endodontic Surgery: Systematic Review and Meta-Analysis with Trial Sequential Analysis. Medicina 2022, 58, 894. [Google Scholar] [CrossRef]
- Mente, J.; Leo, M.; Michel, A.; Gehrig, H.; Saure, D.; Pfefferle, T. Outcome of orthograde retreatment after failed apicoectomy: Use of a mineral trioxide aggregate apical plug. J. Endod. 2015, 41, 613–620. [Google Scholar] [CrossRef]
- Stefopoulos, S.; Tzanetakis, G.N.; Kontakiotis, E.G. Non-surgical retreatment of a failed apicoectomy without retrofilling using white mineral trioxide aggregate as an apical barrier. Braz. Dent. J. 2012, 23, 167–171. [Google Scholar] [CrossRef]
- Vivan, R.R.; Guerreiro-Tanomaru, J.M.; Bosso-Martelo, R.; Costa, B.C.; Duarte, M.A.H.; Tanomaru-Filho, M. Push-out Bond Strength of Root-end Filling Materials. Braz. Dent. J. 2016, 27, 332–335. [Google Scholar] [CrossRef]
- Angerame, D.; De Biasi, M.; Lenhardt, M.; Porrelli, D.; Bevilacqua, L.; Generali, L.; La Rosa, G.R.M.; Pedulla, E. Root-end resection with or without retrograde obturation after orthograde filling with two techniques: A micro-CT study. Aust. Endod. J. 2022, 48, 423–430. [Google Scholar] [CrossRef]
- Chaudhari, P.S.; Chandak, M.G.; Jaiswal, A.A.; Ikhar, A. Comparative evaluation of push-out bond strength of three retrograde filling materials in teeth with root apices resected at 90 degrees: Mineral trioxide aggregate Angelus, Zirconomer, and Bioactive bone cement. J. Conserv. Dent. 2022, 25, 605–609. [Google Scholar] [CrossRef]
- Parashos, P.; Phoon, A.; Sathorn, C. Effect of ultrasonication on physical properties of mineral trioxide aggregate. Biomed. Res. Int. 2014, 2014, 191984. [Google Scholar] [CrossRef]
- Skidmore, L.J.; Berzins, D.W.; Bahcall, J.K. An in vitro comparison of the intraradicular dentin bond strength of Resilon and gutta-percha. J. Endod. 2006, 32, 963–966. [Google Scholar] [CrossRef] [PubMed]
- Kadic, S.; Baraba, A.; Miletic, I.; Ionescu, A.; Brambilla, E.; Ivanisevic Malcic, A.; Gabric, D. Push-out bond strength of three different calcium silicate-based root-end filling materials after ultrasonic retrograde cavity preparation. Clin. Oral. Investig. 2018, 22, 1559–1565. [Google Scholar] [CrossRef] [PubMed]
- Gilheany, P.A.; Figdor, D.; Tyas, M.J. Apical dentin permeability and microleakage associated with root end resection and retrograde filling. J. Endod. 1994, 20, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.J.; Lynch, E. Marginal adaptation. J. Dent. 1993, 21, 265–273. [Google Scholar] [CrossRef]
- Ishikawa, H.; Sawada, N.; Kobayashi, C.; Suda, H. Evaluation of root-end cavity preparation using ultrasonic retrotips. Int. Endod. J. 2003, 36, 586–590. [Google Scholar] [CrossRef]
- O’Connor, R.P.; Hutter, J.W.; Roahen, J.O. Leakage of amalgam and Super-EBA root-end fillings using two preparation techniques and surgical microscopy. J. Endod. 1995, 21, 74–78. [Google Scholar] [CrossRef]
- Taschieri, S.; Bettach, R.; Lolato, A.; Moneghini, L.; Fabbro, M.D. Endodontic surgery failure: SEM analysis of root-end filling. J. Oral. Sci. 2011, 53, 393–396. [Google Scholar] [CrossRef]
- Bernardes, R.A.; de Moraes, I.G.; Garcia, R.B.; Bernardineli, N.; Baldi, J.V.; Victorino, F.R.; Vasconcelos, B.C.; Duarte, M.A.; Bramante, C.M. Evaluation of apical cavity preparation with a new type of ultrasonic diamond tip. J. Endod. 2007, 33, 484–487. [Google Scholar] [CrossRef]
- Jung, J.; Kim, S.; Kim, E.; Shin, S.J. Volume of Voids in Retrograde Filling: Comparison between Calcium Silicate Cement Alone and Combined with a Calcium Silicate-based Sealer. J. Endod. 2020, 46, 97–102. [Google Scholar] [CrossRef]
- Bueno, C.R.E.; Vasques, A.M.V.; Cury, M.T.S.; Sivieri-Araujo, G.; Jacinto, R.C.; Gomes-Filho, J.E.; Cintra, L.T.A.; Dezan-Junior, E. Biocompatibility and biomineralization assessment of mineral trioxide aggregate flow. Clin. Oral. Investig. 2019, 23, 169–177. [Google Scholar] [CrossRef]
- Formosa, L.M.; Mallia, B.; Camilleri, J. Push-out bond strength of MTA with antiwashout gel or resins. Int. Endod. J. 2014, 47, 454–462. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, V.; Singla, M.; Miglani, S.; Kohli, S. Comparative evaluation of push-out bond strength of ProRoot MTA, Biodentine, and MTA Plus in furcation perforation repair. J. Conserv. Dent. 2013, 16, 462–465. [Google Scholar] [CrossRef] [PubMed]
- Ertas, H.; Kucukyilmaz, E.; Ok, E.; Uysal, B. Push-out bond strength of different mineral trioxide aggregates. Eur. J. Dent. 2014, 8, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Vivan, R.R.; Guerreiro-Tanomaru, J.M.; Bernardes, R.A.; Reis, J.M.; Hungaro Duarte, M.A.; Tanomaru-Filho, M. Effect of ultrasonic tip and root-end filling material on bond strength. Clin. Oral. Investig. 2016, 20, 2007–2011. [Google Scholar] [CrossRef] [PubMed]
- Stefaneli Marques, J.H.; Silva-Sousa, Y.T.C.; Rached-Junior, F.J.A.; Macedo, L.M.D.; Mazzi-Chaves, J.F.; Camilleri, J.; Sousa-Neto, M.D. Push-out bond strength of different tricalcium silicate-based filling materials to root dentin. Braz. Oral. Res. 2018, 32, e18. [Google Scholar] [CrossRef]
- Shokouhinejad, N.; Razmi, H.; Fekrazad, R.; Asgary, S.; Neshati, A.; Assadian, H.; Kheirieh, S. Push-out bond strength of two root-end filling materials in root-end cavities prepared by Er,Cr:YSGG laser or ultrasonic technique. Aust. Endod. J. 2012, 38, 113–117. [Google Scholar] [CrossRef]
- Akbulut, M.B.; Bozkurt, D.A.; Terlemez, A.; Akman, M. The push-out bond strength of BIOfactor mineral trioxide aggregate, a novel root repair material. Restor. Dent. Endod. 2019, 44, e5. [Google Scholar] [CrossRef]
- Camilleri, J.; Sorrentino, F.; Damidot, D. Investigation of the hydration and bioactivity of radiopacified tricalcium silicate cement, Biodentine and MTA Angelus. Dent. Mater. 2013, 29, 580–593. [Google Scholar] [CrossRef]
- Roda, R.S.; Gettleman, B.H.; Jhonson, S.C. Nonsurgical retreatment. In Cohen’s Pathways of the Pulp, 12th ed.; Berman, L.H., Ed.; Elsevier: Philadelphia, PA, USA, 2021; pp. 343–410. [Google Scholar]
- Goncalves Galoza, M.O.; Fagundes Jordao-Basso, K.C.; Escalante-Otarola, W.G.; Victorino, K.R.; Rached Dantas, A.A.; Kuga, M.C. Effect of cleaning protocols on bond strength of etch-and-rinse adhesive system to dentin. J. Conserv. Dent. 2018, 21, 602–606. [Google Scholar] [CrossRef]
- Cacciafesta, V.; Sfondrini, M.F.; Scribante, A.; De Angelis, M.; Klersy, C. Effects of blood contamination on the shear bond strengths of conventional and hydrophilic primers. Am. J. Orthod. Dentofacial Orthop. 2004, 126, 207–212. [Google Scholar] [CrossRef]
- Appel, D.; Schafer, E.; Appel, C. Success rate of orthograde endodontic retreatment after failed apicectomy—A retrospective study. Int. Endod. J. 2023, 56, 819–826. [Google Scholar] [CrossRef] [PubMed]

| Material | Method | Cavities | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TC | U | Total | ||||||||||
| n | Mean | SD | n | Mean | SD | n | Mean | SD | ||||
| CIS | MC | 10 | 7.58 | 4.64 | 10 | 21.90 | 5.47 | 40 | 14.12 | 9.23 | ||
| IUV | 10 | 9.36 | 5.99 | 10 | 17.63 | 11.34 | ||||||
| MTA | MC | 8 | 4.35 | 3.68 | 8 | 23.86 | 8.04 | 35 | 15.40 | 11.08 | ||
| IUV | 9 | 8.42 | 7.06 | 10 | 23.75 | 7.79 | ||||||
| BIO | MC | 9 | 7.63 | 4.77 | 10 | 25.34 | 11.68 | 38 | 17.95 | 11.34 | ||
| IUV | 9 | 11.62 | 4.81 | 10 | 25.56 | 8.96 | ||||||
| Total | MC | 55 | 15.32 | 11.00 | ||||||||
| IUV | 58 | 16.26 | 10.26 | |||||||||
| Total | 55 | 8.24 | 5.48 | 58 | 22.98 | 9.18 | ||||||
| Variances | Sum of Squares | SD | Mean Square | F-Value | p-Value |
|---|---|---|---|---|---|
| Cavity | 6183.874 | 1 | 6183.874 | 108.474 | 0.000 * |
| Material | 238.885 | 2 | 119.442 | 2.095 | 0.128 |
| Placement | 25.130 | 1 | 25.130 | 0.441 | 0.508 |
| Cavity × Material | 191.669 | 2 | 95.834 | 1.681 | 0.191 |
| Cavity × Placement | 153.107 | 1 | 153.107 | 2.686 | 0.104 |
| Material × Placement | 70.094 | 2 | 35.047 | 0.615 | 0.543 |
| Cavity × Material × Placement | 7.182 | 2 | 3.591 | 0.063 | 0.939 |
| Material | Placement | Cavity | The Apical Access | p | |||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| n | % | n | % | ||||
| CIS | MC | TC | 5 | 50.0 | 5 | 50.0 | 0.350 |
| U | 2 | 20.0 | 8 | 80.0 | |||
| IUV | TC | 5 | 50.0 | 5 | 50.0 | 0.350 | |
| U | 2 | 20.0 | 8 | 80.0 | |||
| MTA | MC | TC | 10 | 100.0 | 0 | 0.0 | 0.087 |
| U | 6 | 60.0 | 4 | 40.0 | |||
| IUV | TC | 10 | 100.0 | 0 | 0.0 | 0.011 * | |
| U | 4 | 40.0 | 6 | 60.0 | |||
| BIO | MC | TC | 10 | 100.0 | 0 | 0.0 | 0.000 * |
| U | 0 | 0.0 | 10 | 100.0 | |||
| IUV | TC | 7 | 70.0 | 3 | 30.0 | 0.003 * | |
| U | 0 | 0.0 | 10 | 100.0 | |||
| Material | Cavity | Placement | The Apical Access | p | |||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| n | % | n | % | ||||
| CIS | TC | MC | 5 | 50.0 | 5 | 50.0 | 1.000 |
| IUV | 5 | 50.0 | 5 | 50.0 | |||
| U | MC | 2 | 20.0 | 8 | 80.0 | 1.000 | |
| IUV | 2 | 20.0 | 8 | 80.0 | |||
| MTA | TC | MC | 10 | 100.0 | 0 | 0.0 | - |
| IUV | 10 | 100.0 | 0 | 0.0 | |||
| U | MC | 6 | 60.0 | 4 | 40.0 | 0.656 | |
| IUV | 4 | 40.0 | 6 | 60.0 | |||
| BIO | TC | MC | 10 | 100.0 | 0 | 0.0 | 0.211 |
| IUV | 7 | 70.0 | 3 | 30.0 | |||
| U | MC | 0 | 0.0 | 10 | 100.0 | - | |
| IUV | 0 | 0.0 | 10 | 100.0 | |||
| Placement | Method | Material | Apical Access | p | |||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| n | % | n | % | ||||
| MC | TC | CIS | 5 | 50.0 | 5 | 50.0 | 0.001 * |
| MTA | 10 | 100.0 | 0 | 0.0 | |||
| BIO | 10 | 100.0 | 0 | 0.0 | |||
| U | CIS | 2 | 20.0 | 8 | 80.0 | 0.003 * | |
| MTA | 6 | 60.0 | 4 | 40.0 | |||
| BIO | 0 | 0.0 | 10 | 100.0 | |||
| IUV | TC | CIS | 5 | 50.0 | 5 | 50.0 | 0.013 * |
| MTA | 10 | 100.0 | 0 | 0.0 | |||
| BIO | 7 | 70.0 | 3 | 30.0 | |||
| U | CIS | 2 | 20.0 | 8 | 80.0 | 0.038 * | |
| MTA | 4 | 40.0 | 6 | 60.0 | |||
| BIO | 0 | 0.0 | 10 | 100.0 | |||
| Cavity Methods | Apical Access | n | Mean | SD | p | |
|---|---|---|---|---|---|---|
| TC | MPa | Yes | 47 | 6.37 | 5.61 | 0.002 * |
| No | 13 | 11.82 | 3.92 | |||
| U | MPa | Yes | 14 | 16.52 | 11.07 | 0.013 * |
| No | 46 | 23.94 | 9.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tok, S.; Ayranci, L.B. Examination of the Bond Strength of Retrograde Filling in Teeth with Failed Apical Resection After Retreatment. Appl. Sci. 2025, 15, 3441. https://doi.org/10.3390/app15073441
Tok S, Ayranci LB. Examination of the Bond Strength of Retrograde Filling in Teeth with Failed Apical Resection After Retreatment. Applied Sciences. 2025; 15(7):3441. https://doi.org/10.3390/app15073441
Chicago/Turabian StyleTok, Sevda, and Leyla Benan Ayranci. 2025. "Examination of the Bond Strength of Retrograde Filling in Teeth with Failed Apical Resection After Retreatment" Applied Sciences 15, no. 7: 3441. https://doi.org/10.3390/app15073441
APA StyleTok, S., & Ayranci, L. B. (2025). Examination of the Bond Strength of Retrograde Filling in Teeth with Failed Apical Resection After Retreatment. Applied Sciences, 15(7), 3441. https://doi.org/10.3390/app15073441







