Sagittal Posture Measurement in Adolescent Athletes: Which Parameters Are Reliable over the Course of a Day?
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Examination Procedure
2.3. Posture Analysis
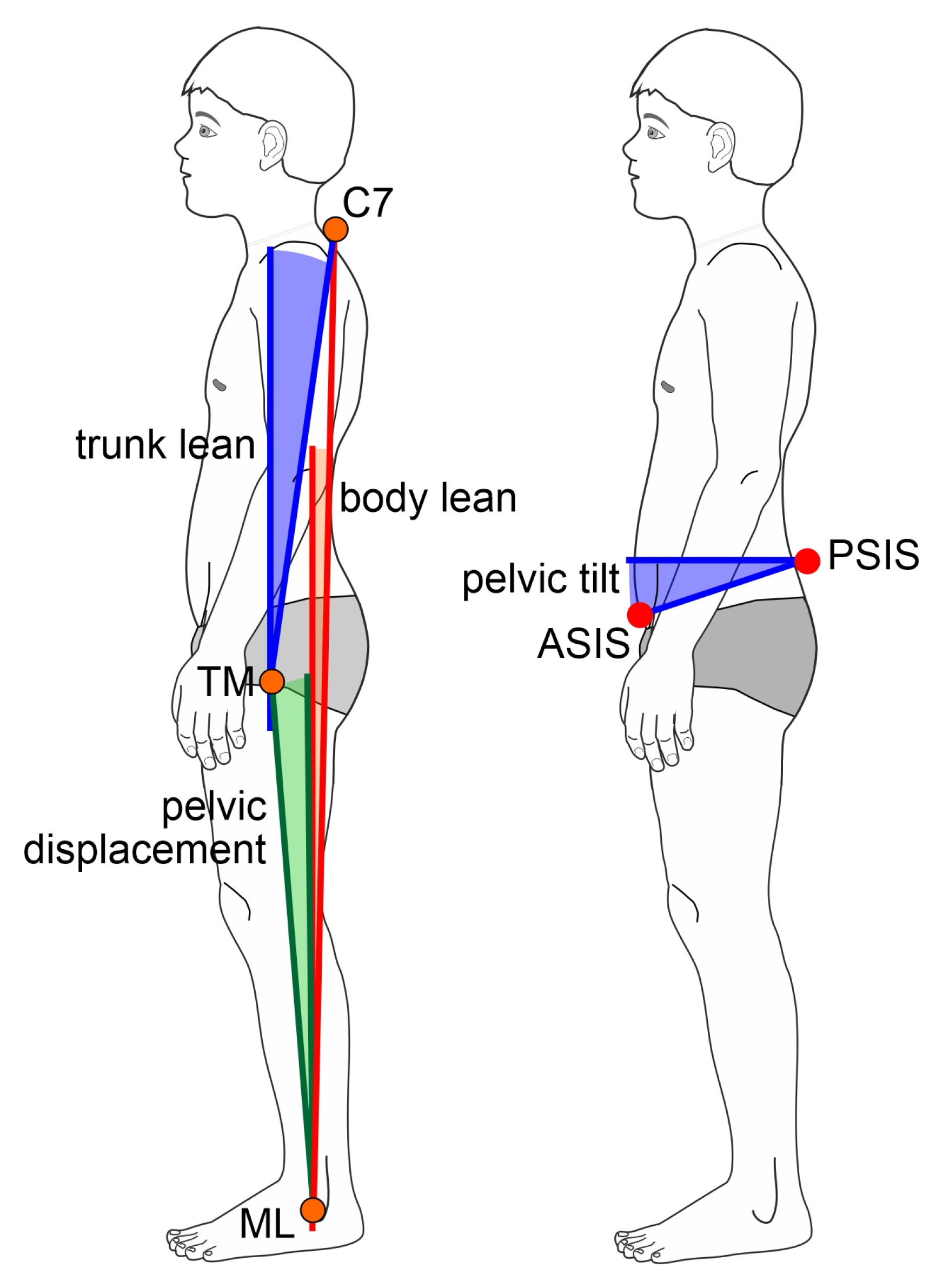
- Global alignment (global posture parameter):
- (1)
- Body lean: angle between the line connecting the lateral malleolus and C7 and the vertical.
- (2)
- Pelvic displacement: angle between the line connecting the lateral malleolus and the greater trochanter and the vertical.
- Local alignment (local/segmental posture parameters):
- (3)
- Pelvic tilt: angle between the line connecting the anterior superior iliac spines and the horizontal.
- (4)
- Trunk lean: angle between the line connecting the greater trochanter to C7 and the vertical.
2.4. Statistics
3. Results
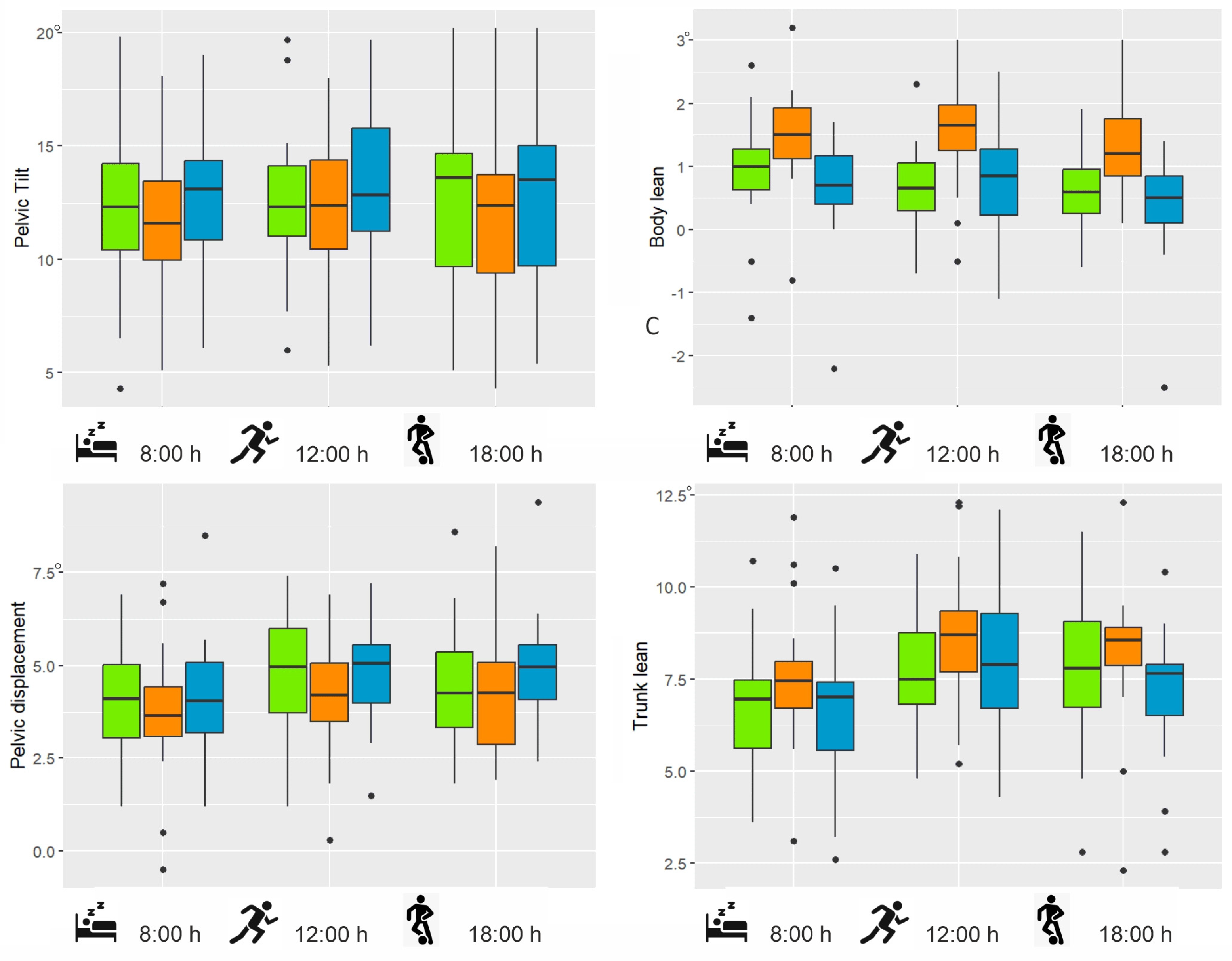
3.1. Pelvic Tilt
3.2. Body Lean
3.3. Trunk Lean
3.4. Pelvic Displacement
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barczyk-Pawelec, K.; Dziubek, W.; Piechura, J.R.; Rożek, K. Correlations between somatic features, anteroposterior spinal curvatures and trunk muscle strength in schoolchildren. Acta Bioeng. Biomech. 2017, 19, 133–139. [Google Scholar] [PubMed]
- Barczyk-Pawelec, K.; Piechura, J.R.; Dziubek, W.; Rozek, K. Evaluation of isokinetic trunk muscle strength in adolescents with normal and abnormal postures. J. Manip. Physiol. Ther. 2015, 38, 484–492. [Google Scholar] [CrossRef]
- Grabara, M. Analysis of Body Posture Between Young Football Players and their Untrained Peers. Hum. Mov. 2012, 13, 120. [Google Scholar] [CrossRef]
- Yoo, W.G. Effect of Individual Strengthening Exercises for Anterior Pelvic Tilt Muscles on Back Pain, Pelvic Angle, and Lumbar ROMs of a LBP Patient with Flat Back. J. Phys. Ther. Sci. 2013, 25, 1357–1358. [Google Scholar] [CrossRef]
- Ludwig, O.; Kelm, J.; Hammes, A.; Schmitt, E.; Fröhlich, M. Targeted athletic training improves the neuromuscular performance in terms of body posture from adolescence to adulthood–Long-term study over 6 years. Front. Physiol. 2018, 9, 1620. [Google Scholar] [CrossRef]
- Klee, A.; Jöllenbeck, T.; Wiemann, K. Correlation between muscular function and posture-lowering the degree of pelvic inclination with exercise. In Proceedings of the ISBS-Conference Proceedings Archive, Hong Kong, China, 25–30 June 2000. [Google Scholar]
- Preece, S.J.; Tan, Y.F.; Alghamdi, T.D.; Arnall, F.A. Comparison of pelvic tilt before and after hip flexor stretching in healthy adults. J. Manip. Physiol. Ther. 2021, 44, 289–294. [Google Scholar] [CrossRef]
- López-Miñarro, P.A.; Alacid, F.; Rodríguez-García, P.L. Comparison of sagittal spinal curvatures and hamstring muscle extensibility among young elite paddlers and non-athletes. Int. Sport. J. 2010, 11, 301–312. [Google Scholar]
- Myer, G.D.; Kushner, A.M.; Brent, J.L.; Schoenfeld, B.J.; Hugentobler, J.; Lloyd, R.S.; Vermeil, A.; Chu, D.A.; Harbin, J.; McGill, S.M. The back squat: A proposed assessment of functional deficits and technical factors that limit performance. Strength Cond. J. 2014, 36, 4–27. [Google Scholar] [CrossRef]
- Alizadeh, S.; Mattes, K. How anterior pelvic tilt affects the lower extremity kinematics during the late swing phase in soccer players while running: A time series analysis. Hum. Mov. Sci. 2019, 66, 459–466. [Google Scholar] [CrossRef]
- Patel, R.V.; Han, S.; Lenherr, C.; Harris, J.D.; Noble, P.C. Pelvic tilt and range of motion in hips with femoroacetabular impingement syndrome. JAAOS-J. Am. Acad. Orthop. Surg. 2020, 28, e427–e432. [Google Scholar] [CrossRef]
- Ludwig, O.; Schneider, G.; Kelm, J. Improvement of Groin Pain in a Football Player with Femoroacetabular Impingement via a Correction of the Pelvic Position—A Case Report. J. Clin. Med. 2023, 12, 7443. [Google Scholar] [CrossRef] [PubMed]
- Barczyk-Pawelec, K.; Rubajczyk, K.; Stefańska, M.; Pawik, Ł.; Dziubek, W. Characteristics of body posture in the sagittal plane in 8–13-year-old male athletes practicing soccer. Symmetry 2022, 14, 210. [Google Scholar] [CrossRef]
- Betsch, M.; Furian, T.; Quack, V.; Rath, B.; Wild, M.; Rapp, W. Effects of athletic training on the spinal curvature in child athletes. Res. Sports Med. 2015, 23, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Salsali, M.; Sheikhhoseini, R.; Sayyadi, P.; Hides, J.A.; Dadfar, M.; Piri, H. Association between physical activity and body posture: A systematic review and meta-analysis. BMC Public Health 2023, 23, 1670. [Google Scholar] [CrossRef]
- Wojtys, E.M.; Ashton-Miller, J.A.; Huston, L.J.; Moga, P.J. The association between athletic training time and the sagittal curvature of the immature spine. Am. J. Sports Med. 2000, 28, 490–498. [Google Scholar] [CrossRef]
- Dolphens, M.; Cagnie, B.; Coorevits, P.; Vleeming, A.; Palmans, T.; Danneels, L. Posture class prediction of pre-peak height velocity subjects according to gross body segment orientations using linear discriminant analysis. Eur. Spine J. 2014, 23, 530–535. [Google Scholar] [CrossRef]
- Dolphens, M.; Cagnie, B.; Coorevits, P.; Vleeming, A.; Danneels, L. Classification system of the normal variation in sagittal standing plane alignement. Spine 2013, 38, E1003–E1012. [Google Scholar] [CrossRef]
- Dolphens, M.; Cagnie, B.; Vleeming, A.; Vanderstraeten, G.; Coorevits, P.; Danneels, L. A clinical postural model of sagittal alignment in young adolescents before age at peak height velocity. Eur. Spine J. 2012, 21, 2188–2197. [Google Scholar] [CrossRef]
- Bayrak, A.; Patlar, S. Increased anterior pelvic tilt angle elevates the risk of hamstring injuries in soccer player. Res. Sports Med. 2024, 33, 129–145. [Google Scholar] [CrossRef]
- Romero, V.; Lahti, J.; Castaño Zambudio, A.; Mendiguchia, J.; Jiménez Reyes, P.; Morin, J.-B. Effects of Fatigue Induced by Repeated Sprints on Sprint Biomechanics in Football Players: Should We Look at the Group or the Individual? Int. J. Environ. Res. Public Health 2022, 19, 14643. [Google Scholar] [CrossRef]
- Mendiguchia, J.; Garrues, M.A.; Schilders, E.; Myer, G.D.; Dalmau-Pastor, M. Anterior pelvic tilt increases hamstring strain and is a key factor to target for injury prevention and rehabilitation. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Suits, W.H. Clinical measures of pelvic tilt in physical therapy. Int. J. Sports Phys. Ther. 2021, 16, 1366. [Google Scholar] [CrossRef]
- Alviso, D.J.; Dong, G.T.; Lentell, G.L. Intertester reliability for measuring pelvic tilt in standing. Phys. Ther. 1988, 68, 1347–1351. [Google Scholar] [CrossRef] [PubMed]
- Bullock-Saxton, J. Postural alignment in standing: A repeatability study. Aust. J. Physiother. 1993, 39, 25–29. [Google Scholar] [CrossRef]
- Dong, M.; Li, X.; Xie, J.; Zhang, L.; Wang, Y. Reliability of photogrammetry for evaluating pelvic posture in healthy individuals. Chin. J. Tissue Eng. Res. 2024, 28, 5846. [Google Scholar]
- Glaner, M.; Mota, Y.; Viana, A.; Santos, M. Photogrammetry: Reliability and lack of objectivity in posture evaluation. Motricidade 2012, 8, 78–85. [Google Scholar]
- Hazar, Z.; Karabicak, G.O.; Tiftikci, U. Reliability of photographic posture analysis of adolescents. J. Phys. Ther. Sci. 2015, 27, 3123–3126. [Google Scholar] [CrossRef]
- Pausic, J.; Pedisic, Z.; Dizdar, D. Reliability of a photographic method for assessing standing posture of elementary school students. J. Manip. Physiol. Ther. 2010, 33, 425–431. [Google Scholar] [CrossRef]
- Buchtelová, E.; Tichy, M.; Vaniková, K. Influence of muscular imbalances on pelvic position and lumbar lordosis: A theoretical basis. J. Nurs. Soc. Stud. Public Health Rehabil. 2013, 1–2, 25–36. [Google Scholar] [CrossRef]
- Araújo, F.; Lucas, R.; Alegrete, N.; Azevedo, A.; Barros, H. Sagittal standing posture, back pain, and quality of life among adults from the general population: A sex-specific association. Spine 2014, 39, E782–E794. [Google Scholar] [CrossRef]
- Król, A.; Polak, M.; Szczygieł, E.; Wójcik, P.; Gleb, K. Relationship between mechanical factors and pelvic tilt in adults with and without low back pain. J. Back Musculoskelet. Rehabil. 2017, 30, 699–705. [Google Scholar] [CrossRef]
- Kuo, Y.-L.; Tully, E.A.; Galea, M.P. Video Analysis of Sagittal Spinal Posture in Healthy Young and Older Adults. J. Manip. Physiol. Ther. 2009, 32, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, C.J.; Norton, B.J.; Callaghan, J.P.; Hwang, C.-T.; Van Dillen, L.R. Is lumbar lordosis related to low back pain development during prolonged standing? Man. Ther. 2015, 20, 553–557. [Google Scholar] [CrossRef]
- Alvim, F.C.; Peixoto, J.G.; Vicente, E.J.; Chagas, P.S.; Fonseca, D.S. Influences of the extensor portion of the gluteus maximus muscle on pelvic tilt before and after the performance of a fatigue protocol. Rev. Bras. de Fisioter. 2010, 14, 206–213. [Google Scholar] [CrossRef]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Sahrmann, S.A. Does postural assessment contribute to patient care? J. Orthop. Sports Phys. Ther. 2002, 32, 376–379. [Google Scholar] [CrossRef] [PubMed]
- Fourchet, F.; Materne, O.; Rajeb, A.; Horobeanu, C.; Farooq, A. Pelvic tilt: Reliability of measuring the standing position and range of motion in adolescent athletes. Br. J. Sports Med. 2014, 48, 594. [Google Scholar] [CrossRef]
- Dunk, N.M.; Chung, Y.Y.; Compton, D.S.; Callaghan, J.P. The reliability of quantifying upright standing postures as a baseline diagnostic clinical tool. J. Manip. Physiol. Ther. 2004, 27, 91–96. [Google Scholar] [CrossRef]
- Julious, S.A.; Patterson, S.D. Sample sizes for estimation in clinical research. Pharm. Stat. J. Appl. Stat. Pharm. Ind. 2004, 3, 213–215. [Google Scholar] [CrossRef]
- Ludwig, O.; Kelm, J.; Hopp, S. Impact of Quadriceps/Hamstrings Torque Ratio on Three-Dimensional Pelvic Posture and Clinical Pubic Symphysis Pain-Preliminary Results in Healthy Young Male Athletes. Appl. Sci. 2020, 10, 5215. [Google Scholar] [CrossRef]
- Ludwig, O.; Mazet, C.; Mazet, D.; Hammes, A.; Schmitt, E. Changes in Habitual and Active Sagittal Posture in Children and Adolescents with and without Visual Input—Implications for Diagnostic Analysis of Posture. J. Clin. Diagn. Res. 2016, 10, SC14–SC17. [Google Scholar] [CrossRef]
- Pivotto, L.R.; Navarro, I.J.R.L.; Candotti, C.T. Radiography and photogrammetry-based methods of assessing cervical spine posture in the sagittal plane: A systematic review with meta-analysis. Gait Posture 2021, 84, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Stolinski, L.; Kozinoga, M.; Czaprowski, D.; Tyrakowski, M.; Cerny, P.; Suzuki, N.; Kotwicki, T. Two-dimensional digital photography for child body posture evaluation: Standardized technique, reliable parameters and normative data for age 7–10 years. Scoliosis Spinal Disord. 2017, 12, 38. [Google Scholar] [CrossRef] [PubMed]
- Singla, D.; Veqar, Z.; Hussain, M.E. Photogrammetric Assessment of Upper Body Posture Using Postural Angles: A Literature Review. J. Chiropr. Med. 2017, 16, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. J. Appl. Stat. Pharm. Ind. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- R_Core_Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2021. [Google Scholar]
- Weir, J.P. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar]
- Michnik, R.; Zadoń, H.; Nowakowska-Lipiec, K.; Jochymczyk-Woźniak, K.; Myśliwiec, A.; Mitas, A.W. The effect of the pelvis position in the sagittal plane on loads in the human musculoskeletal system. Acta Bioeng. Biomech. 2020, 22, 33–42. [Google Scholar] [CrossRef]
- Kroll, P.G.; Arnofsky, S.; Leeds, S.; Peckham, D.; Rabinowitz, A. The relationship between lumbar lordosis and pelvic tilt angle. J. Back Musculoskelet. Rehabil. 2000, 14, 21–25. [Google Scholar] [CrossRef]
- Furlan, L.; Sterr, A. The applicability of standard error of measurement and minimal detectable change to motor learning research—A behavioral study. Front. Hum. Neurosci. 2018, 12, 95. [Google Scholar] [CrossRef] [PubMed]
- Dolphens, M.; Vansteelandt, S.; Cagnie, B.; Vleeming, A.; Nijs, J.; Vanderstraeten, G.; Danneels, L. Multivariable modeling of factors associated with spinal pain in young adolescence. Eur. Spine J. 2016, 25, 2809–2821. [Google Scholar] [CrossRef]
- Dolphens, M.; Cagnie, B.; Coorevits, P. Sagittal standing posture and its association with spinal pain: A school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine 2012, 37, 1657–1666. [Google Scholar] [CrossRef]
- Dolphens, M.; Vansteelandt, S.; Cagnie, B.; Nijs, J.; Danneels, L. Factors associated with low back and neck pain in young adolescence: A multivariable modeling study. Physiotherapy 2015, 101, e1090–e1091. [Google Scholar] [CrossRef]
- Krawczky, B.; Pacheco, A.G.; Mainenti, M.R. A systematic review of the angular values obtained by computerized photogrammetry in sagittal plane: A proposal for reference values. J. Manip. Physiol. Ther. 2014, 37, 269–275. [Google Scholar] [CrossRef]
- Sousa, A.S.; Silva, A.; Tavares, J.M. Biomechanical and neurophysiological mechanisms related to postural control and efficiency of movement: A review. Somat. Mot. Res. 2012, 29, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Ghamkhar, L.; Kahlaee, A.H. The effect of trunk muscle fatigue on postural control of upright stance: A systematic review. Gait Posture 2019, 72, 167–174. [Google Scholar] [CrossRef]
- Cretual, A. Which biomechanical models are currently used in standing posture analysis? Neurophysiol. Clin. 2015, 45, 285–295. [Google Scholar] [CrossRef]
- Smith, A.; O’Sullivan, P.; Straker, L. Classification of sagittal thoraco-lumbo-pelvic alignment of the adolescent spine in standing and its relationship to low back pain. Spine (Phila. Pa. 1976) 2008, 33, 2101–2107. [Google Scholar] [CrossRef]
- Dunk, N.M.; Lalonde, J.; Callaghan, J.P. Implications for the use of postural analysis as a clinical diagnostic tool: Reliability of quantifying upright standing spinal postures from photographic images. J. Manip. Physiol. Ther. 2005, 28, 386–392. [Google Scholar] [CrossRef]


| Age | 16.61 ± 0.28 years |
| Height | 179.38 ± 6.40 cm |
| Weight | 70.35 ± 7.79 kg |
| BMI | 21.81 ± 1.63 kg/m2 |
| Parameter | Posture | T1 | T2 | T3 |
|---|---|---|---|---|
| Mean ± SD [95% CI] | Mean ± SD [95% CI] | Mean ± SD [95% CI] | ||
| Pelvic tilt | Hab | 11.91 ±3.96 [9.95; 13.88] | 12.42 ± 3.57 [10.65; 14.20] | 12.60 ± 4.18 [10.52; 14.67] |
| Act | 11.56 ± 3.52 [9.80; 13.31] | 12.09 ± 3.55 [10.32; 13.85] | 11.74 ± 3.92 [10.32; 13.85] | |
| Aec | 12.75 ± 3.54 [10.99; 14.51] | 13.22 ± 3.90 [11.28; 15.16] | 13.09 ± 4.12 [11.04; 15.14] | |
| Body lean | Hab | 0.88 ± 0.95 [0.41; 1.36] | 0.62 ± 0.74 [0.25; 0.99] | 0.68 ± 0.68 [0.34; 1.02] |
| Act | 1.46 ± 0.81 [1.06; 1.86] | 1.51 ± 0.84 [1.09; 1.93] | 1.32 ± 0.70 [0.97; 1.67] | |
| Aec | 0.63 ± 0.87 [0.20; 1.06] | 0.71 ±0.96 [0.23; 1.19] | 0.37 ± 0.87 [−0.07; 0.80] | |
| Pelvic displacement | Hab | 4.14 ± 1.57 [3.36; 4.93] | 4.72 ±1.64 [3.91; 5.54] | 4.52 ± 1.62 [3.72; 5.33] |
| Act | 3.74 ±2.87 [2.81; 4.67] | 4.07 ± 1.63 [3.26; 4.88] | 4.22 ±1.69 [3.38; 5.06] | |
| Aec | 4.23 ±1.55 [3.46; 5.00] | 4.78 ±1.40 [4.07; 5.47] | 4.91 ±1.64 [4.10; 5.73] | |
| Trunk lean | Hab | 6.79 ±1.86 [5.86; 7.71] | 7.66 ± 1.69 [6.82; 8.50] | 7.56 ± 2.04 [6.55; 8.57] |
| Act | 7.52 ±1.98 [6.53; 8.50] | 8.71 ± 1.93 [7.75; 9.67] | 8.16 ± 2.02 [7.16; 9.17] | |
| Aec | 6.50 ±2.07 [5.47; 7.53] | 7.83 ±1.97 [6.85; 8.82] | 7.14 ± 1.77 [6.26; 8.03] |
| Parameter | Effect | F | DF1 | DF2 | p |
|---|---|---|---|---|---|
| Pelvic tilt | time | 1.05 | 2 | 34 | 0.363 |
| posture | 15.89 | 2 | 34 | <0.001 ** | |
| interaction | 0.59 | 4 | 68 | 0.669 | |
| Body lean | time | 0.85 | 2 | 34 | 0.437 |
| posture | 32.70 | 2 | 34 | <0.001 ** | |
| interaction | 2.11 | 2.87 | 48.83 | 0.113 | |
| Pelvic displacement | time | 3.28 | 2 | 34 | 0.05 * |
| posture | 17.05 | 1.19 | 20.29 | <0.001 ** | |
| interaction | 1.54 | 4 | 68 | 0.20 | |
| Trunk lean | time | 8.00 | 2 | 34 | 0.001 * |
| posture | 13.03 | 1.51 | 25.71 | <0.001 ** | |
| interaction | 1.48 | 4 | 68 | 0.217 |
| Parameter | Comparison | t | p | Cohen’s d | 95% Confidence Interval |
|---|---|---|---|---|---|
| Pelvic tilt | Hab–Act | 2.55 | 0.041 * | 0.35 | [0.11; 0.92] |
| Hab–Aec | −3.89 | <0.001 ** | 0.53 | [−1.07; −0.34] | |
| Act–Aec | −8.16 | <0.001 ** | 1.11 | [−1.52; −0.92] | |
| Body lean | Hab–Act | −9.56 | <0.001 ** | 1.30 | [−0.85; −0.56] |
| Hab–Aec | 1.62 | 0.111 | 0.22 | [−0.04; 0.36] | |
| Act–Aec | 10.4 | <0.001 ** | 1.41 | [0.70; 1.03] | |
| Trunk lean | Hab–Act | −4.69 | <0.001 ** | 0.64 | [−1.13; −0.46] |
| Hab–Aec | 1.38 | 0.522 | 0.19 | [−0.08; 0.43] | |
| Act–Aec | 6.95 | <0.001 ** | 0.95 | [0.69; 1.25] | |
| Pelvic displacement | Hab–Act | 5.93 | <0.001 ** | 0.81 | [0.30; 0.61] |
| Hab–Aec | −1.86 | 0.206 | 0.25 | [−0.36; 0.014] | |
| Act–Aec | −6.27 | <0.001 ** | 0.85 | [−0.83; −0.43] |
| Comparison | t | p | Cohen’s d | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Trunk lean | T1 vs. T2 | −5.85 | <0.001 ** | 0.66 | [−1.52; −0.74] |
| T1 vs. T3 | −3.89 | <0.001 ** | 0.48 | [−1.04; −0.33] | |
| T2 vs. T3 | 2.39 | 0.061 | 0.17 | [0.07; 0.82] | |
| Pelvic displacement | T1 vs. T2 | −3.31 | 0.005 * | 0.45 | [−0.77; −0.19] |
| T1 vs. T3 | −3.71 | 0.001 * | 0.51 | [−0.79; −0.24] | |
| T2 vs. T3 | −0.23 | 1.00 | 0.03 | [−0.32; 0.26] |
| Parameter | Posture | SEM | MDC |
|---|---|---|---|
| Pelvic tilt | Hab | 1.41 | 3.91 |
| Act | 1.01 | 2.81 | |
| Aec | 1.42 | 3.93 | |
| Body lean | Hab | 0.51 | 1.42 |
| Act | 0.56 | 1.55 | |
| Aec | 0.60 | 1.66 | |
| Trunk lean | Hab | 0.76 | 2.12 |
| Act | 0.81 | 2.25 | |
| Aec | 0.67 | 1.86 | |
| Pelvic displacement | Hab | 0.87 | 2.42 |
| Act | 1.06 | 2.94 | |
| Aec | 0.98 | 2.70 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ludwig, O.; Dully, J.; Baun, E.; Fröhlich, M. Sagittal Posture Measurement in Adolescent Athletes: Which Parameters Are Reliable over the Course of a Day? Appl. Sci. 2025, 15, 3277. https://doi.org/10.3390/app15063277
Ludwig O, Dully J, Baun E, Fröhlich M. Sagittal Posture Measurement in Adolescent Athletes: Which Parameters Are Reliable over the Course of a Day? Applied Sciences. 2025; 15(6):3277. https://doi.org/10.3390/app15063277
Chicago/Turabian StyleLudwig, Oliver, Jonas Dully, Edwin Baun, and Michael Fröhlich. 2025. "Sagittal Posture Measurement in Adolescent Athletes: Which Parameters Are Reliable over the Course of a Day?" Applied Sciences 15, no. 6: 3277. https://doi.org/10.3390/app15063277
APA StyleLudwig, O., Dully, J., Baun, E., & Fröhlich, M. (2025). Sagittal Posture Measurement in Adolescent Athletes: Which Parameters Are Reliable over the Course of a Day? Applied Sciences, 15(6), 3277. https://doi.org/10.3390/app15063277








