Evaluation of Condylar and Airway Volume in Skeletal Class I Patients with Different Vertical Growth Patterns
Abstract
1. Introduction
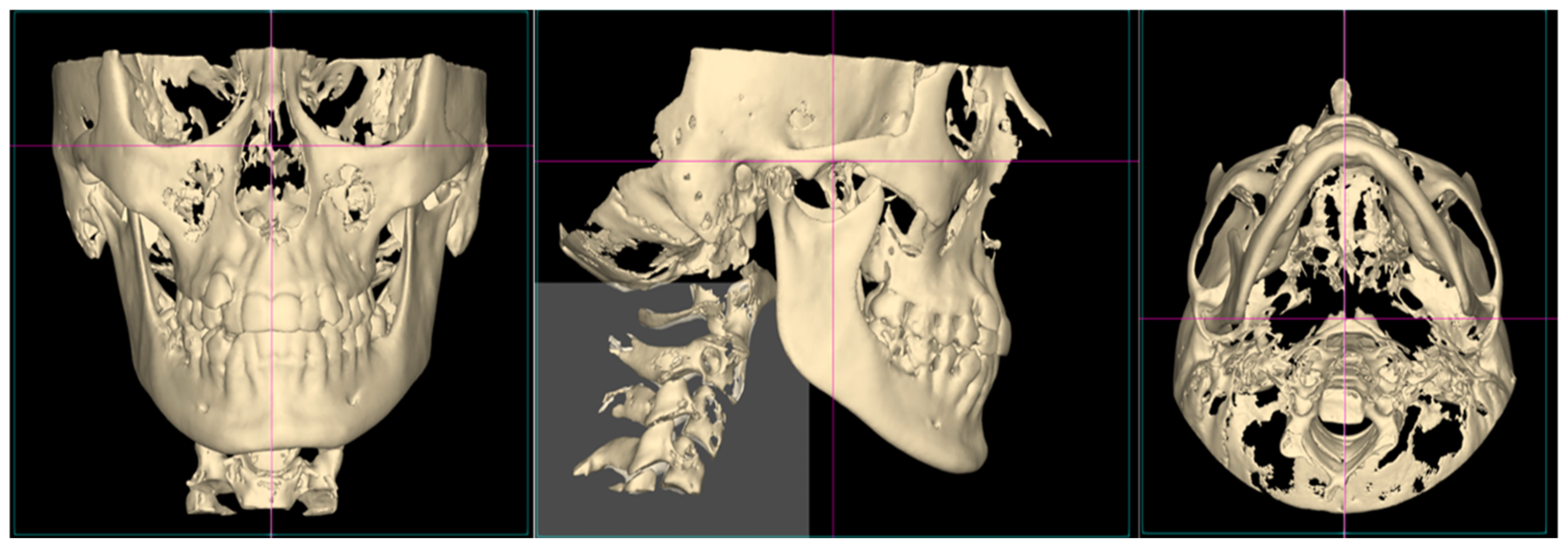
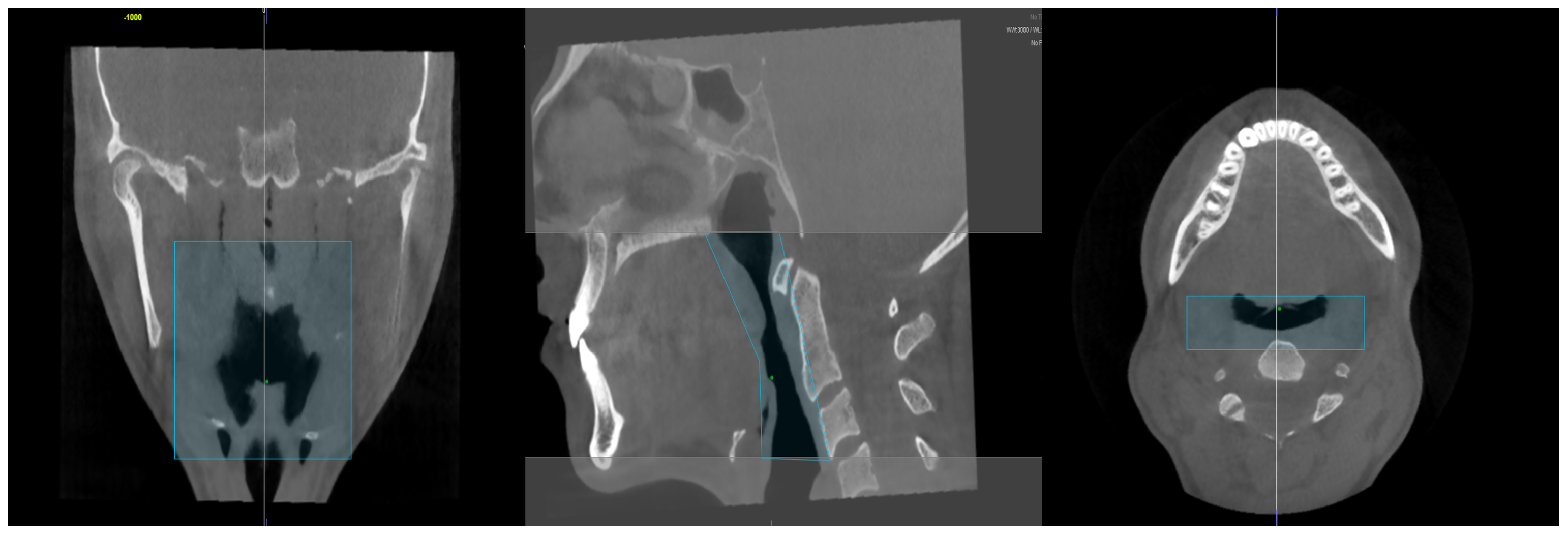
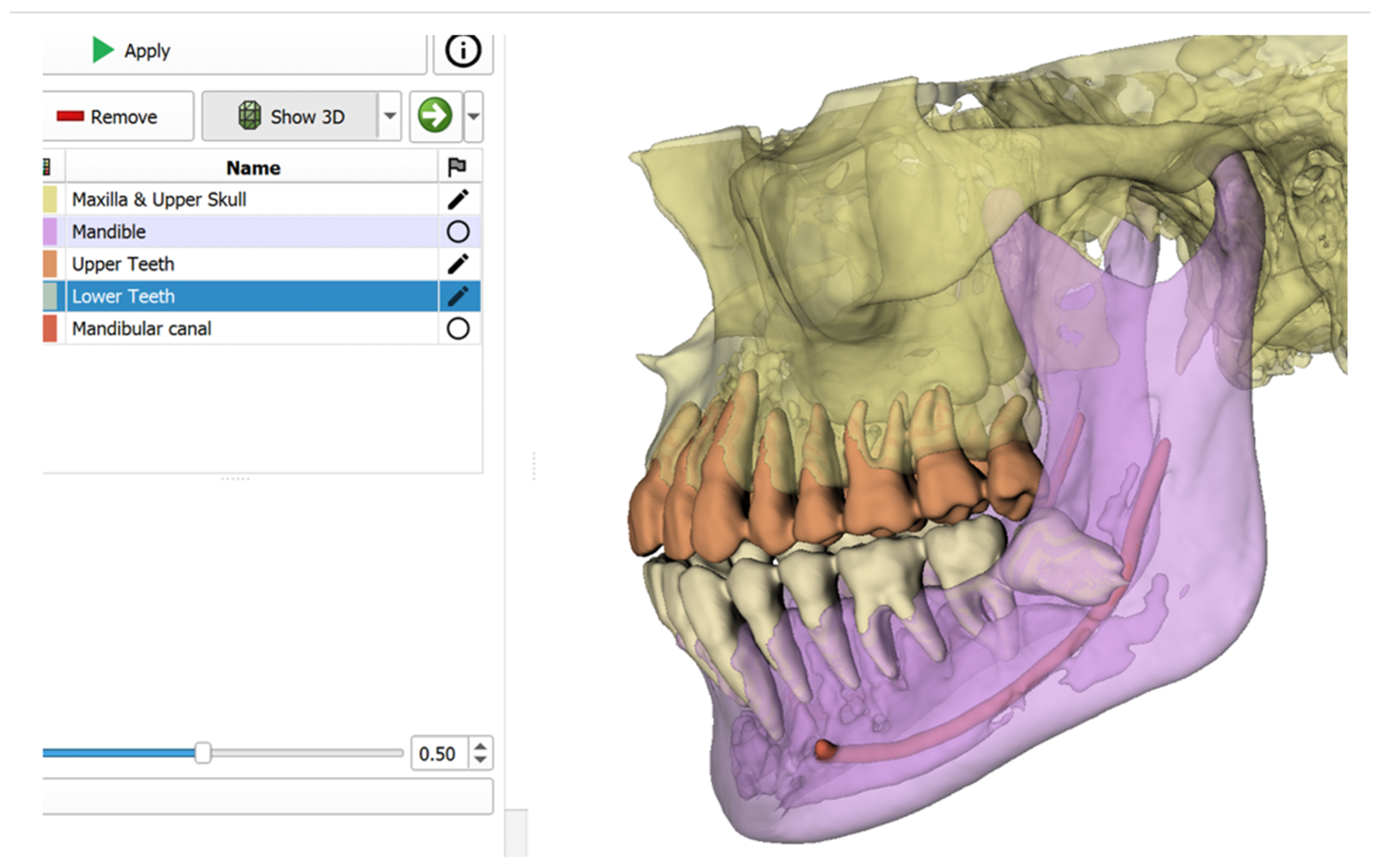
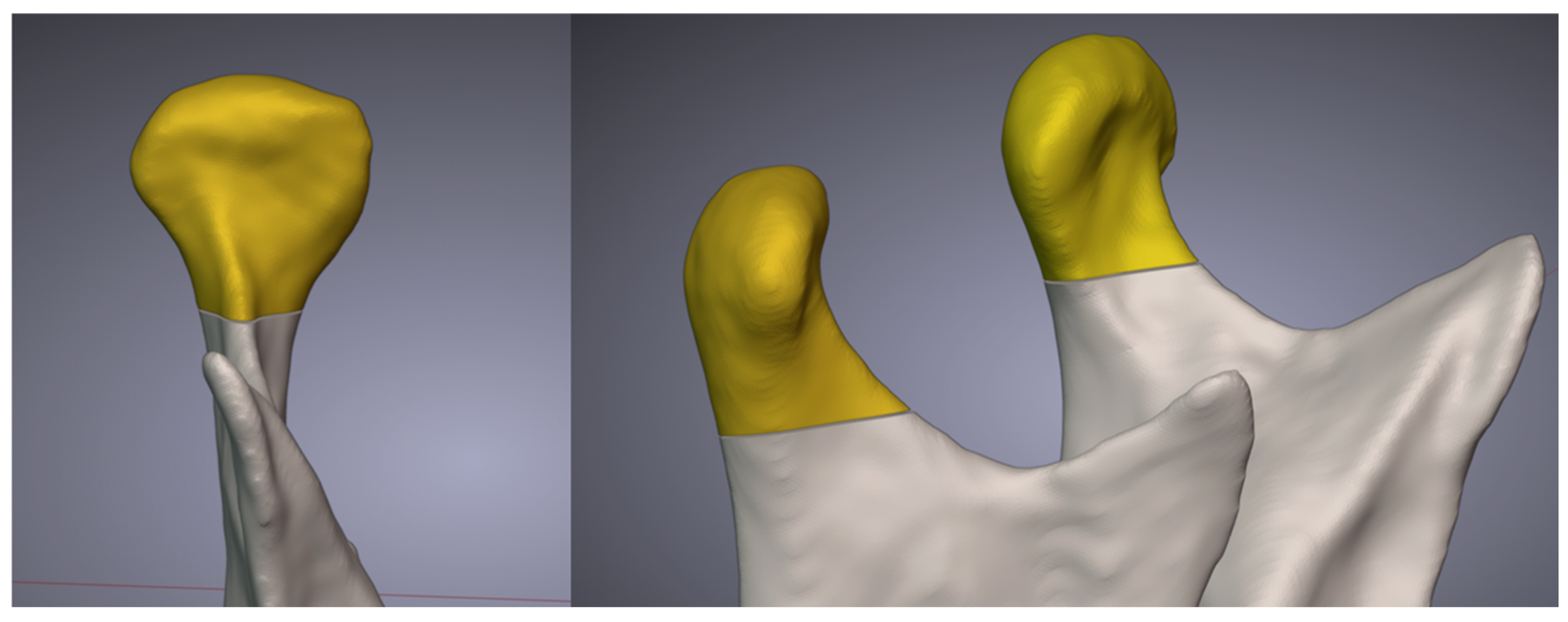
2. Materials and Methods
- Age range: Individuals between 18 and 30 years old,
- Skeletal Class I structure,
- No history of orthodontic or orthognathic surgical treatment,
- CBCT images of sufficient quality and resolution,
- No respiratory tract pathology or craniofacial syndromes.
2.1. Airway Volume Calculation
2.2. Condyle Volume Calculation
2.3. Statistical Analysis
3. Results
- Normodivergent Group: A weak and nonsignificant negative relationship was found between airway volume and right condylar volume (r = −0.204, p = 0.280).
- Hyperdivergent Group: No significant relationship was observed between airway volume and right condylar volume (r = −0.007, p = 0.971).
- Hypodivergent Group: A nonsignificant positive relationship was detected between airway volume and right condylar volume (r = 0.015, p = 0.936).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moss, M.L.; Salentijn, L. The primary role of functional matrices in facial growth. Am. J. Orthod. 1969, 55, 566–577. [Google Scholar] [CrossRef]
- El, H.; Palomo, J.M. Three-dimensional evaluation of upper airway following rapid maxillary expansion: A CBCT study. Angle Orthod. 2014, 84, 265–273. [Google Scholar] [CrossRef]
- Li, L.; Liu, H.; Cheng, H.; Han, Y.; Wang, C.; Chen, Y.; Song, J.; Liu, D. CBCT evaluation of the upper airway morphological changes in growing patients of class II division 1 malocclusion with mandibular retrusion using twin block appliance: A comparative research. PLoS ONE 2014, 9, e94378. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Almashraqi, A.A.; Halboub, E.; Almahdi, S.; Jali, T.; Atafi, A.; Alomar, F. Pharyngeal airway spaces in different skeletal malocclusions: A CBCT 3D assessment. Cranio 2021, 39, 97–106. [Google Scholar] [CrossRef]
- Brito, F.C.; Brunetto, D.P.; Nojima, M.C. Three-dimensional study of the upper airway in different skeletal Class II malocclusion patterns. Angle Orthod. 2019, 89, 93–101. [Google Scholar] [CrossRef]
- de Freitas, M.R.; Alcazar, N.M.P.V.; Janson, G.; de Freitas, K.M.S.; Henriques, J.F.C. Upper and lower pharyngeal airways in subjects with Class I and Class II malocclusions and different growth patterns. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 742–745. [Google Scholar] [CrossRef]
- Ucar, F.I.; Uysal, T. Orofacial airway dimensions in subjects with Class I malocclusion and different growth patterns. Angle Orthod. 2011, 81, 460–468. [Google Scholar] [CrossRef]
- Nielsen, I.L. Vertical malocclusions: Etiology, development, diagnosis and some aspects of treatment. Angle Orthod. 1991, 61, 247–260. [Google Scholar]
- Schudy, F.F. The rotation of the mandible resulting from growth: Its implications in orthodontic treatment. Angle Orthod. 1965, 35, 36–50. [Google Scholar]
- Isaacson, J.R.; Isaacson, R.J.; Speidel, T.M.; Worms, F.W. Extreme variation in vertical facial growth and associated variation in skeletal and dental relations. Angle Orthod 1971, 41, 219–229. [Google Scholar]
- Xu, J.; Sun, R.; Wang, L.; Hu, X. Cone-beam evaluation of pharyngeal airway space in adult skeletal Class II patients with different condylar positions. Angle Orthod. 2019, 89, 312–316. [Google Scholar] [CrossRef]
- Paul, P.; Thakur, A.; Mathur, A.; Chitra, P. Airway dimensions and mandibular position in adults with different growth patterns: A cone-beam computed tomography study. J. Stomatol. 2022, 75, 87–92. [Google Scholar] [CrossRef]
- Saccucci, M.; D’Attilio, M.; Rodolfino, D.; Festa, F.; Polimeni, A.; Tecco, S. Condylar volume and condylar area in Class I, Class II and Class III young adult subjects. Head Face Med. 2012, 8, 34. [Google Scholar] [CrossRef]
- Arieta-Miranda, J.M.; Silva-Valencia, M.; Flores-Mir, C.; Paredes-Sampen, N.A.; Arriola-Guillen, L.E. Spatial analysis of condyle position according to sagittal skeletal relationship, assessed by cone beam computed tomography. Prog. Orthod. 2013, 14, 36. [Google Scholar] [CrossRef]
- Paknahad, M.; Shahidi, S.; Iranpour, S.; Mirhadi, S.; Paknahad, M. Cone-beam computed tomographic assessment of mandibular condylar position in patients with temporomandibular joint dysfunction and in healthy subjects. Int. J. Dent. 2015, 2015, 301796. [Google Scholar] [CrossRef]
- Barandiaran, I.; Macía, I.; Berckmann, E.; Wald, D.; Dupillier, M.P.; Paloc, C.; Grana, M. An automatic segmentation and reconstruction of mandibular structures from CT-data. In Proceedings of the Intelligent Data Engineering and Automated Learning-IDEAL 2009: 10th International Conference, Burgos, Spain, 23–26 September 2009; pp. 649–655. [Google Scholar]
- Caruso, S.; Storti, E.; Nota, A.; Ehsani, S.; Gatto, R. Temporomandibular joint anatomy assessed by CBCT images. BioMed Res. Int. 2017, 2017, 2916953. [Google Scholar] [CrossRef]
- Sin, Ç.; Akkaya, N.; Aksoy, S.; Orhan, K.; Öz, U. A deep learning algorithm proposal to automatic pharyngeal airway detection and segmentation on CBCT images. Orthod. Craniofacial Res. 2021, 24, 117–123. [Google Scholar] [CrossRef]
- Evain, T.; Ripoche, X.; Atif, J.; Bloch, I. Semi-automatic teeth segmentation in cone-beam computed tomography by graph-cut with statistical shape priors. In Proceedings of the 2017 IEEE 14th International Symposium on Biomedical Imaging (ISBI 2017), Melbourne, Australia, 18–21 April 2017; pp. 1197–1200. [Google Scholar]
- Indraswari, R.; Kurita, T.; Arifin, A.Z.; Suciati, N.; Astuti, E.R.; Navastara, D.A. 3D region merging for segmentation of teeth on cone-beam computed tomography images. In Proceedings of the 2018 Joint 10th International Conference on Soft Computing and Intelligent Systems (SCIS) and 19th International Symposium on Advanced Intelligent Systems (ISIS), Toyama, Japan, 5–8 December 2018; pp. 341–345. [Google Scholar]
- Tarce, M.; Zhou, Y.; Antonelli, A.; Becker, K. The Application of Artificial Intelligence for Tooth Segmentation in CBCT Images: A Systematic Review. Appl. Sci. 2024, 14, 6298. [Google Scholar] [CrossRef]
- Orhan, K.; Shamshiev, M.; Ezhov, M.; Plaksin, A.; Kurbanova, A.; Ünsal, G.; Gusarev, M.; Golitsyna, M.; Aksoy, S.; Mısırlı, M. AI-based automatic segmentation of craniomaxillofacial anatomy from CBCT scans for automatic detection of pharyngeal airway evaluations in OSA patients. Sci. Rep. 2022, 12, 11863. [Google Scholar] [CrossRef]
- Elsonbaty, S.; Elgarba, B.M.; Fontenele, R.C.; Swaity, A.; Jacobs, R. Novel AI-based tool for primary tooth segmentation on CBCT using convolutional neural networks: A validation study. Int. J. Paediatr. Dent. 2025, 35, 97–107. [Google Scholar] [CrossRef]
- Celikoglu, M.; Bayram, M.; Sekerci, A.E.; Buyuk, S.K.; Toy, E. Comparison of pharyngeal airway volume among different vertical skeletal patterns: A cone-beam computed tomography study. Angle Orthod. 2014, 84, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Dot, G.; Chaurasia, A.; Dubois, G.; Savoldelli, C.; Haghighat, S.; Azimian, S.; Taramsari, A.R.; Sivaramakrishnan, G.; Issa, J.; Dubey, A. DentalSegmentator: Robust open source deep learning-based CT and CBCT image segmentation. J. Dent. 2024, 147, 105130. [Google Scholar] [CrossRef] [PubMed]
- Orhan, K.; Karslioğlu, H.; Özemre, M.Ö.; Köseoğlu Seçgin, C.; Kamburoğlu, K. Kondil hacmi ve şeklinin konik ışınlı bilgisayarlı tomografi kullanılarak değerlendirilmesi. Turk. Klin. J. Dent. Sci. 2021, 27, 199–204. [Google Scholar] [CrossRef]
- Castro-Silva, L.; Monnazzi, M.S.; Spin-Neto, R.; Moraes, M.; Miranda, S.; Gabrielli, M.F.R.; Pereira-Filho, V.A. Cone-beam evaluation of pharyngeal airway space in Class I, II, and III patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 679–683. [Google Scholar] [CrossRef]
- Muto, T.; Yamazaki, A.; Takeda, S. A cephalometric evaluation of the pharyngeal airway space in patients with mandibular retrognathia and prognathia, and normal subjects. Int. J. Oral Maxillofac. Surg. 2008, 37, 228–231. [Google Scholar] [CrossRef]
- Grauer, D.; Cevidanes, L.S.; Styner, M.A.; Ackerman, J.L.; Proffit, W.R. Pharyngeal airway volume and shape from cone-beam computed tomography: Relationship to facial morphology. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 805–814. [Google Scholar] [CrossRef]
- Flores-Blancas, A.P.; Carruitero, M.J.; Flores-Mir, C. Comparison of airway dimensions in skeletal Class I malocclusion subjects with different vertical facial patterns. Dent. Press J. Orthod. 2017, 22, 35–42. [Google Scholar] [CrossRef]
- Enache, A.M.; Nimigean, V.R.; Mihaltan, F.; Didilescu, A.C.; Munteanu, I.; Nimigean, V. Assessment of sagittal and vertical skeletal patterns in Romanian patients with obstructive sleep apnea. Rom. J. Morphol. Embryol. 2010, 51, 505–508. [Google Scholar]
- Salehi, P.; Shahidi, S.; Majdi, B. Evaluation of the relationship between airway volumes and vertical facial growth patterns in adult patients. J. Dentomaxillofacial Radiol. Pathol. Surg. 2015, 4, 20–30. [Google Scholar] [CrossRef]
- Burke, G.; Major, P.; Glover, K.; Prasad, N. Correlations between condylar characteristics and facial morphology in Class II preadolescent patients. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 328–336. [Google Scholar] [CrossRef]
- Park, I.-Y.; Kim, J.-H.; Park, Y.-H. Three-dimensional cone-beam computed tomography based comparison of condylar position and morphology according to the vertical skeletal pattern. Korean J. Orthod. 2015, 45, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.; Fields, H. Occlusal forces in normal-and long-face children. J. Dent. Res. 1983, 62, 571–574. [Google Scholar] [CrossRef] [PubMed]
- Al-koshab, M.; Nambiar, P.; John, J. Assessment of condyle and glenoid fossa morphology using CBCT in South-East Asians. PLoS ONE 2015, 10, e0121682. [Google Scholar]

| Group | Number of Patients | Females | Males | Mean Age (Years ± SD) |
|---|---|---|---|---|
| Normodivergent | 30 | 17 | 13 | 21.3 ± 2.8 |
| Hyperdivergent | 33 | 20 | 13 | 20.7 ± 3.1 |
| Hypodivergent | 30 | 18 | 12 | 21.9 ± 3.2 |
| Parameter | Normodivergent (n = 30) | Hyperdivergent (n = 33) | Hypodivergent (n = 30) | Test Statistic | p-Value |
|---|---|---|---|---|---|
| Airway Volume (cm3) | 14.4 ± 4.9 | 11.2 ± 5.0 | 14.1 ± 6.3 | χ2 = 7.444 | 0.024 * |
| Condylar Volume (Right) (cm3) | 1.5 ± 0.3 | 1.2 ± 0.2 | 1.5 ± 0.3 | F = 5.501 | 0.006 ** |
| Group | Pearson Correlation (r) | p-Value |
|---|---|---|
| Normodivergent | 0.909 *** | <0.001 |
| Hyperdivergent | 0.840 *** | <0.001 |
| Hypodivergent | 0.927 *** | <0.001 |
| Mean Difference (1–3) | Std. Error | p-Value | 95% CI Lower Bound | 95% CI Upper Bound | |
|---|---|---|---|---|---|
| 1 vs. 2 | 211.417 | 84.621 | 0.038 * | 9.758 | 413.076 |
| 1 vs. 3 | −51.602 | 86.612 | 0.823 | −258.007 | 154.803 |
| 2 vs. 3 | −263.019 | 84.621 | 0.007 ** | −464.678 | −61.359 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oğuz, F.; Bor, S.; Khanmohammadi, A.; Kıranşal, M. Evaluation of Condylar and Airway Volume in Skeletal Class I Patients with Different Vertical Growth Patterns. Appl. Sci. 2025, 15, 2794. https://doi.org/10.3390/app15052794
Oğuz F, Bor S, Khanmohammadi A, Kıranşal M. Evaluation of Condylar and Airway Volume in Skeletal Class I Patients with Different Vertical Growth Patterns. Applied Sciences. 2025; 15(5):2794. https://doi.org/10.3390/app15052794
Chicago/Turabian StyleOğuz, Fırat, Sabahattin Bor, Ayla Khanmohammadi, and Melike Kıranşal. 2025. "Evaluation of Condylar and Airway Volume in Skeletal Class I Patients with Different Vertical Growth Patterns" Applied Sciences 15, no. 5: 2794. https://doi.org/10.3390/app15052794
APA StyleOğuz, F., Bor, S., Khanmohammadi, A., & Kıranşal, M. (2025). Evaluation of Condylar and Airway Volume in Skeletal Class I Patients with Different Vertical Growth Patterns. Applied Sciences, 15(5), 2794. https://doi.org/10.3390/app15052794







