Is Pain Stronger in Adults or in Adolescents During Semi-Rapid Maxillary Expansion (SRME) and Fixed Appliance (FA) Therapies?
Abstract
1. Introduction
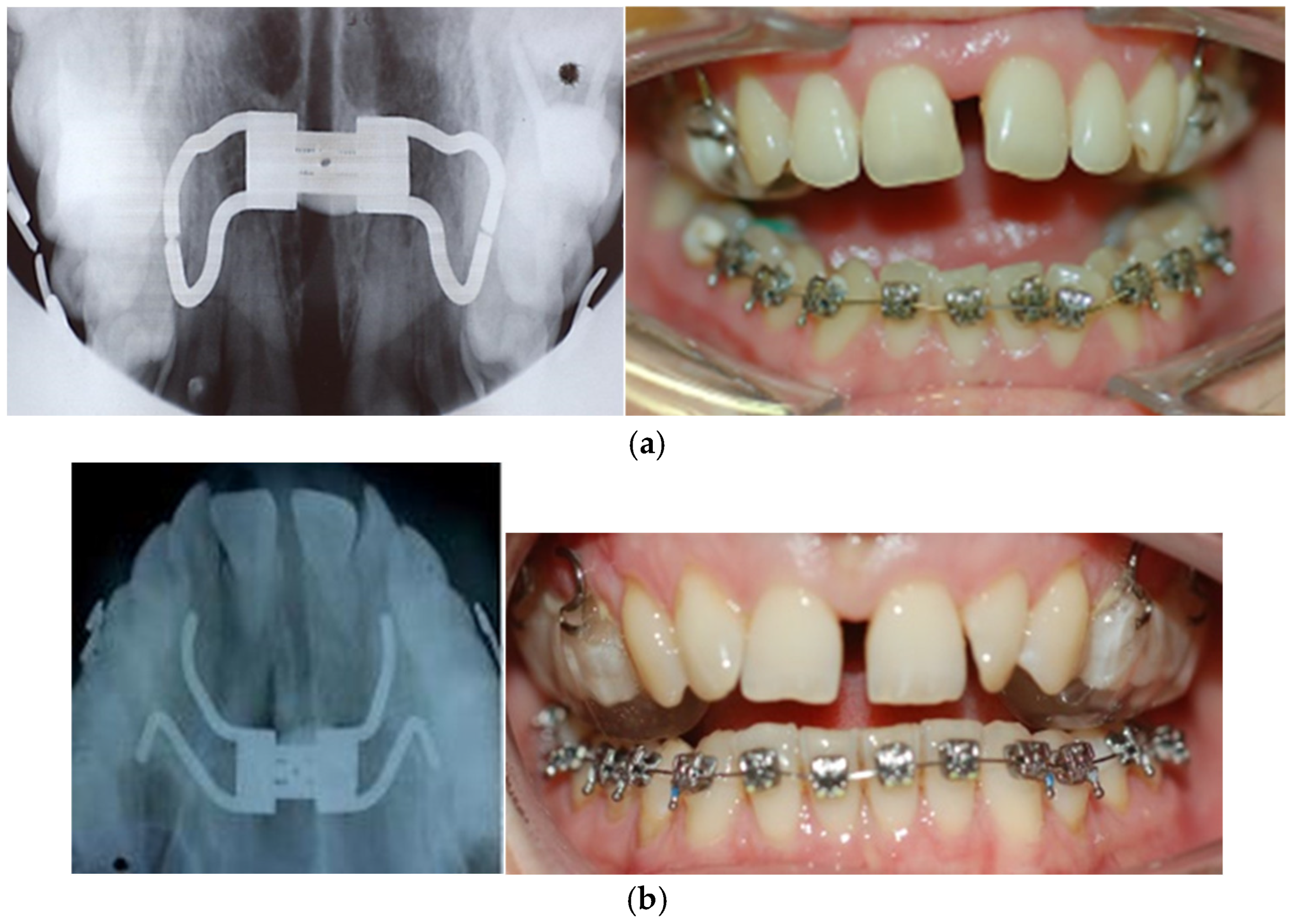
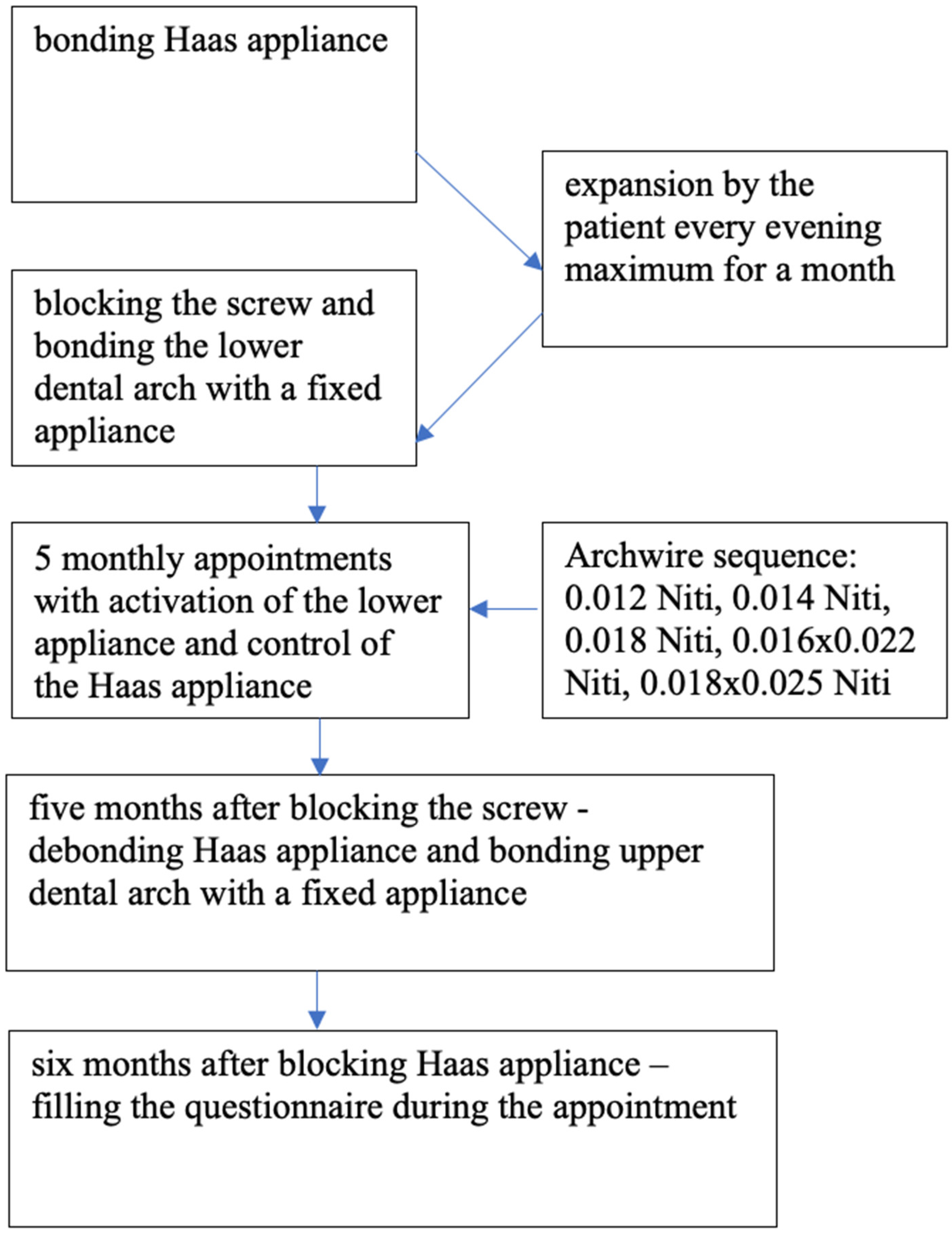
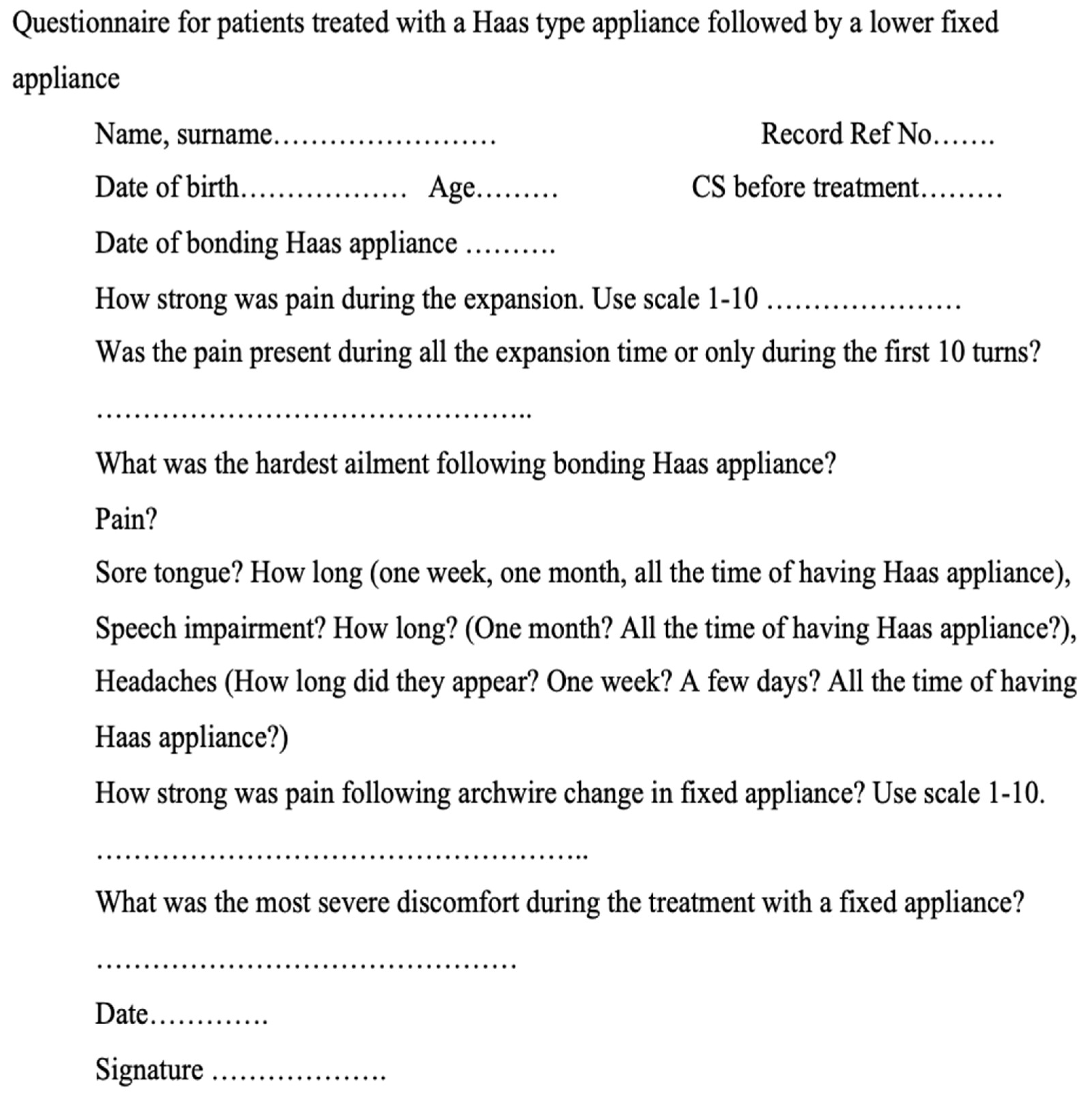
2. Materials and Methods
3. Statistical Analysis
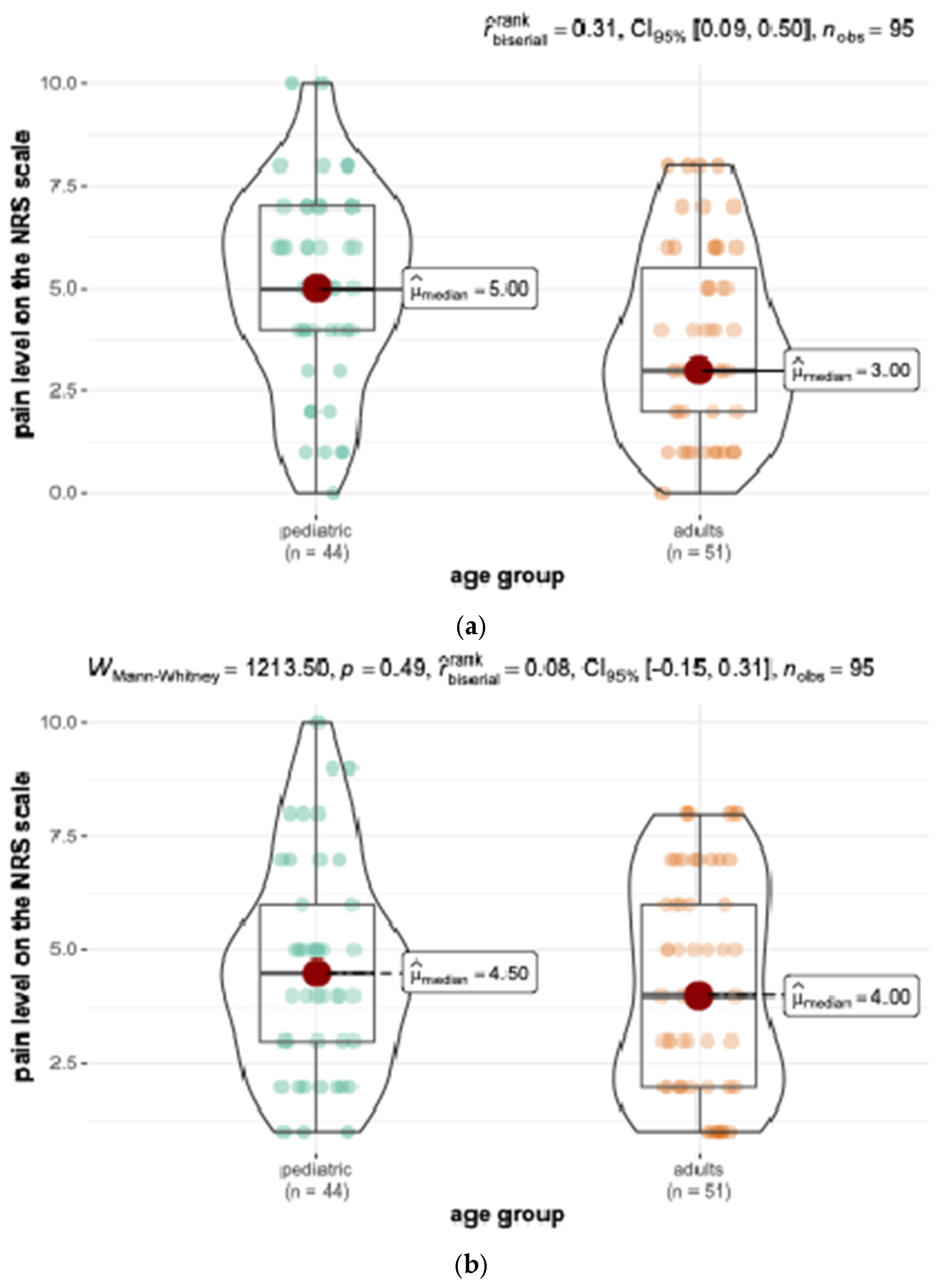
4. Results
5. Discussion
| Author, Year (Ref. No.) | Study Group—Number, Age, Gender | Type of Appliance (Rate of Activation) | Pain Level (Scale Used) and Other Discomfort |
|---|---|---|---|
| Capelozza F et al. 1996 [32] |
38 patients No data referring to age and gender |
RME appliance of the Haas design 4× daily |
Mild discomfort to significant pain Subjective pain assessment—no scale was used |
| Handelman et al. 2000 [22] |
Adults 94 patients 47 adults 19 M, 28 F 47 children as CG |
a Haas-type palatal expander followed by edgewise appliance therapy
1× daily | 9 of the 47 subjects (19%) reported palatal swelling and pain, and 1 subject reported headaches Subjective pain assessment—no scale was used |
| Needleman et al. 2000 [18] |
Children and adolescents 80 patients 38 M, 59 F 5 to 13 years (median 7.7 years) |
RPE procedures with the Hyrax (Dentaurum, Newtown, PA, USA) 1× daily or 2× daily | the Facial Pain Scale and the Color Analog Scale (0–10). Two turns/day—pain stronger than those expanding once/day. No statistically significant difference between females and males. |
| Önçağ G et al. 2011 [27] | Adolescents 30 patients 16 M, 14 F between the ages of 13 and 15 years (mean 14.4 years). | Acrylic bonded Hyrax expander 2× daily during a period of 10 days (0.5 mm/day) | A color pain scale (0–10) Pain was found to be most severe in the dental arch, while it decreases with the distance from the activation region No significant differences in pain perception between males and females (p > 0.05) |
| Gecgelen M et al. 2012 [25] | Adolescents 40 patients 20 F, 20 M aged 10.9–14.7 y | RME an acrylic-bonded RME appliance 1× daily for 36 days | Pressure pain threshold (PPT) Male = 8.84, Female = 7.43 |
| Halicioglu K et al. 2012 [35] |
Adolescents 60 patients 32 F, 28 M (mean age 13.5 y) | RME 1. The memory screw (9 F, 9 M), combining intermittent and continuous force modules, 6× daily 2. The second group (10 F, 10 M), conventional Hyrax appliance, activated 2× daily until the mid-palatal suture opened, after which activation was reduced to 1× daily 3. The third group (13 F, 9 M), a conventional Hyrax screw 2× daily during the entire expansion phase | Numerical rating scale (NRS) 98% of the patients reported pain during RME to a mild degree The majority of the patients undergoing RME suffered pain and pressure sensations especially after the fifth activation Patients who were treated with RME appliances experienced headache and slight dizziness No activation-related differences were found No gender-related differences were found |
| Baldini A, Nota A 2015 [16] |
Children 112 prepubertal patients (54 M, 58 F) m.a. 11.00 ± 1.80 y | A stainless-steel banded expander cemented to the maxillary first molars. RME with two different activation protocols Group 1: 1× daily Group 2: 2× daily | NRS and the Faces Pain Scale (FPS) RME at 2×/day reported significantly greater amounts of pain than subjects treated with RME at 1×/day Pain reported during RME: F = 2.5, M = 2.2 Younger and female patients were more sensitive to the activation protocol |
| Feldman I, Bazargani F. 2017 [28] | Children 54 patients 28 F, 26 M age: 9.8 ± 1.28 | Conventional Hyrax with 2 bands and metal bar from 6 to IV vs. Hybrid Hyrax | The VAS Median values for pain were 8.0 (range 0–50) Hyrax and 3.0 (0–82) HH No statistically significant differences in pain Age was positively correlated with overall pain and discomfort |
| Cossellu G et al. 2019 [31] | Children Phase 1: 101 patients. KLS G: 28 p: 7 F, 11 M, m.a. 8.5 ± 1.8 y. PG: 35 p (17 F, 18 M), m.a. 8.7 ± 1.8 y. CTRL G: 35 p: 17 F, 19 M, m.a. 8.9 ± 1.2 y. Phase 2: added KLS-B 31 p: 15 F, 16 M, m.a. 8.7 ± 1.6 y. | Haas-expander, bonded through bands on the maxillary first permanent molars 2× daily | VAS associated with a numeric rating scale (NRS) Ketoprofen lysine salt vs. paracetamol on pain perception during RME KLS is more effective than P during the fourth, fifth and sixth days |
| Ugolini A et al. 2020 [7] RCT | 101 patients (48 RME G, 53 LE G) RME G: 26 F, 23 M. m.a. 9.4 years LE G: 28 F, 25 M m.a. 9.1. years | Leaf expander vs. Hyrax LE: 2× at chairside, followed by two 1/4 turns/d (1 in the morning and 1 in the evening, 0.40 mm/d) | Wong–Baker FPS (0–10) from the 1st to the 7th d of screw activation, with a double registration/d (morning and evening) Pain is influenced by clinical activation protocol and by the screw type. Patients treated with Leaf expander reported significantly lower pain level in the first 7 days of treatment |
| Abed Al Jawad FH, Alhashimi NA. 2021 [19] | Adolescents 55 patients 43 F, 12 M aged 10.2 to 15 y | Quadhelix group (QG) vs. Hyrax on 4 bands |
Hyrax group reported significantly higher scores for difficulty in swallowing (moderate to severe) during the first 6 days. No differences in pain between QG vs. HG. No correlations between age, gender or malocclusion type |
| Nieri M et al. 2021 [8] | Children (CS 1–2) 56 patients 28 LE: 61% F, 39% M. 8 y 28 RME: 43% F, 57% M. m.a. 8.4 y RME: 8.4 ± 1.0 y SME: 8.0 ± 1.3 y RME: 12 F, 16 M MSME: 17 F, 11 M RME: 21 subjects in CS 1; 6 subjects in CS 2 SME: 24 subjects in CS 1; 4 subjects in CS 2 | Butterfly expander anchored with bands on second primary molars LE activation protocol: initial expansion of 4.5 mm in about 2–3 m, followed by ten 1/4 turns/m for spring reactivation (1 mm) RME activation protocol: 1/4 turn/d (0.2 mm) until the desired expansion was achieved | VAS and Wong–Baker Faces Pain Scale for pain assessment with a complementary NRS from 0 to 10 VAS scale (0–10 pt) once/w for 12 w VAS for pain was 0.3 ± 0.4 in the Leaf group and 0.6 ± 0.5 in the RME group
|
| Rutili V et al. 2022 [10] Systematic review and meta | Children and adolescents 157 patients between 5.7 and 13 years | RME vs. SME | NRS and VRS
|
| Yacout YM et al. 2022 [17] RCT |
Adolescents 30 patients aged 12–16 years SME group (n = 12, mean age = 14.30 ± 1.37 years) RME group (n = 12, mean age = 15.07 ± 1.59 years) |
Penn expanders anchored by four palatal miniscrews (HH) (SME) group activated the appliance once every other day (RME) group activated the appliance twice daily |
NRS at the following four time points:
before appliance insertion (t1), after first activation (t2), after 1 week of activation (t3) and after last activation (t4)
|
| Barone M et al. 2023 [5] Systematic Review. | RME different types RME vs. SME |
Different pain scales
| |
| Pasqua et al. 2023 [13] | Adolescents 42 patients 17 F, 25 M aged 11–14 years Female sex presenting higher scores for pain and functional limitation |
Hybrid Hyrax (12 F and 9 M, m.a. 13.3 ± 1.3 years), and TB GROUP (tooth-borne expander), treated with Hyrax (5 F and 16 M, m.a 13.3 ± 1.4 years) |
NRS and the instrument MFIQ
(Mandibular Functional Impairment Questionnaire).
|
| Hasson S et al. 2023 [10] | Children 35 patients in each group 13 F, 22 M Age: 9.3 F, 9.6 M | Quad Helix (QH) vs. RME (Marco Rosa Hyrax-type) | VAS and VRS
|
| Altuhafy M et al. 2023. [20] Syst Rev. |
Growing patients The number of participants in the included RCTs ranged between 34 to 114 and included both male and female growing patients | Hyrax vs. other maxillary expansion orthodontic appliances (Leaf expander, Haas appliance) |
Graphic rating scale for pain, the Wong–Baker Faces Pain Scale, the NRS, VAS and a questionnaire
|
| El Naghy R et al. 2023 [34] |
Adolescents 30 patients aged between 12 to 16 y total of 24 patients (12 patients in each group) |
Miniscrew-supported Penn expanders allocated (ratio 1:1) into two groups based on the activation protocol SME = 1×/daily or RME = 2×/day | NRS at 4 time points: t1 = before appliance insertion, t2 = after first activation, t3 = after 1 week of activation, t4 = after last activation.
|
6. Conclusions
- -
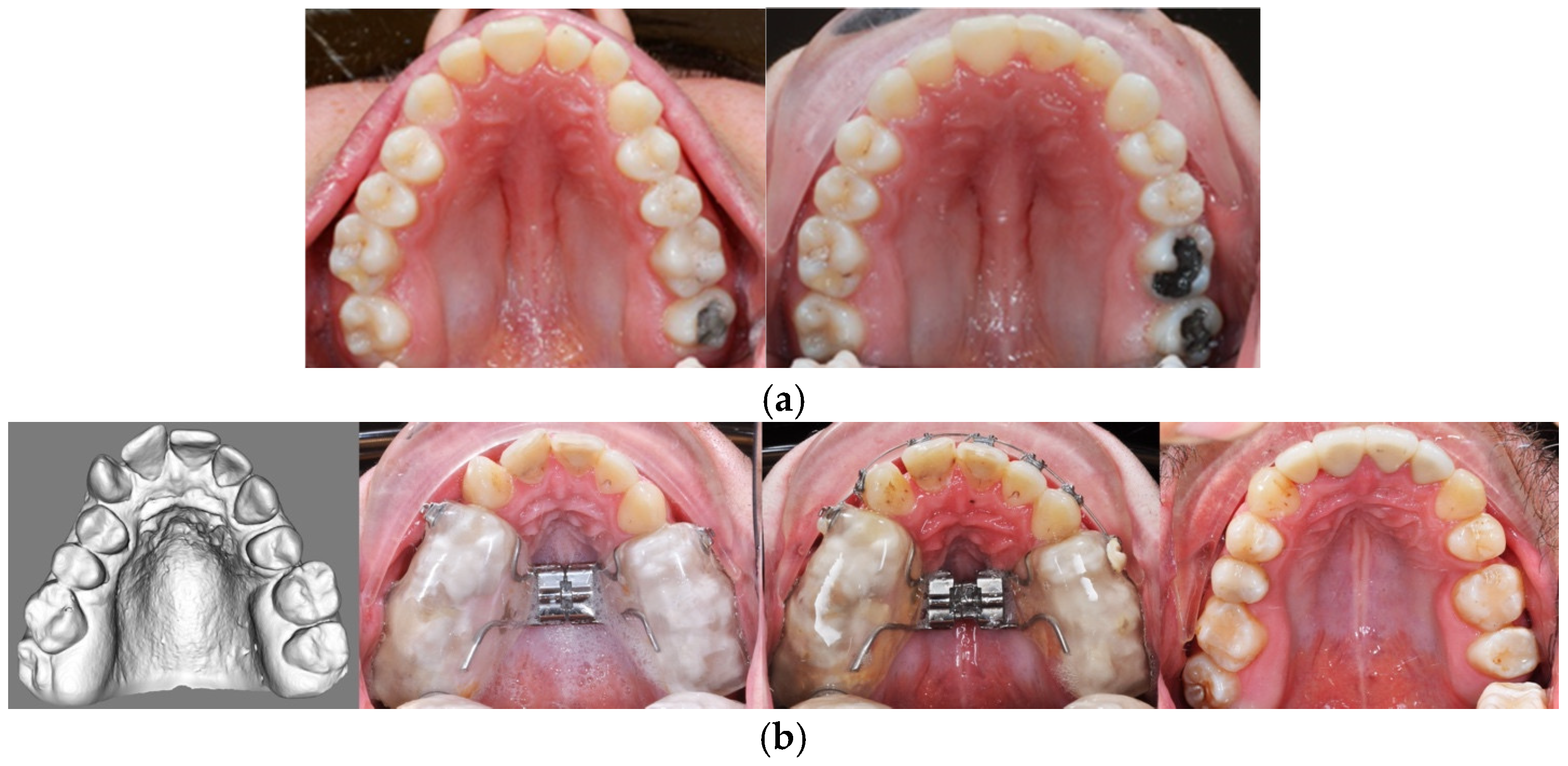
- SRME with activating the screw in Haas-type acrylic splint expander by one turn daily just before going to bed is a relatively untroublesome procedure.
- -
- SRME is more painful for adolescents than for adults.
- -
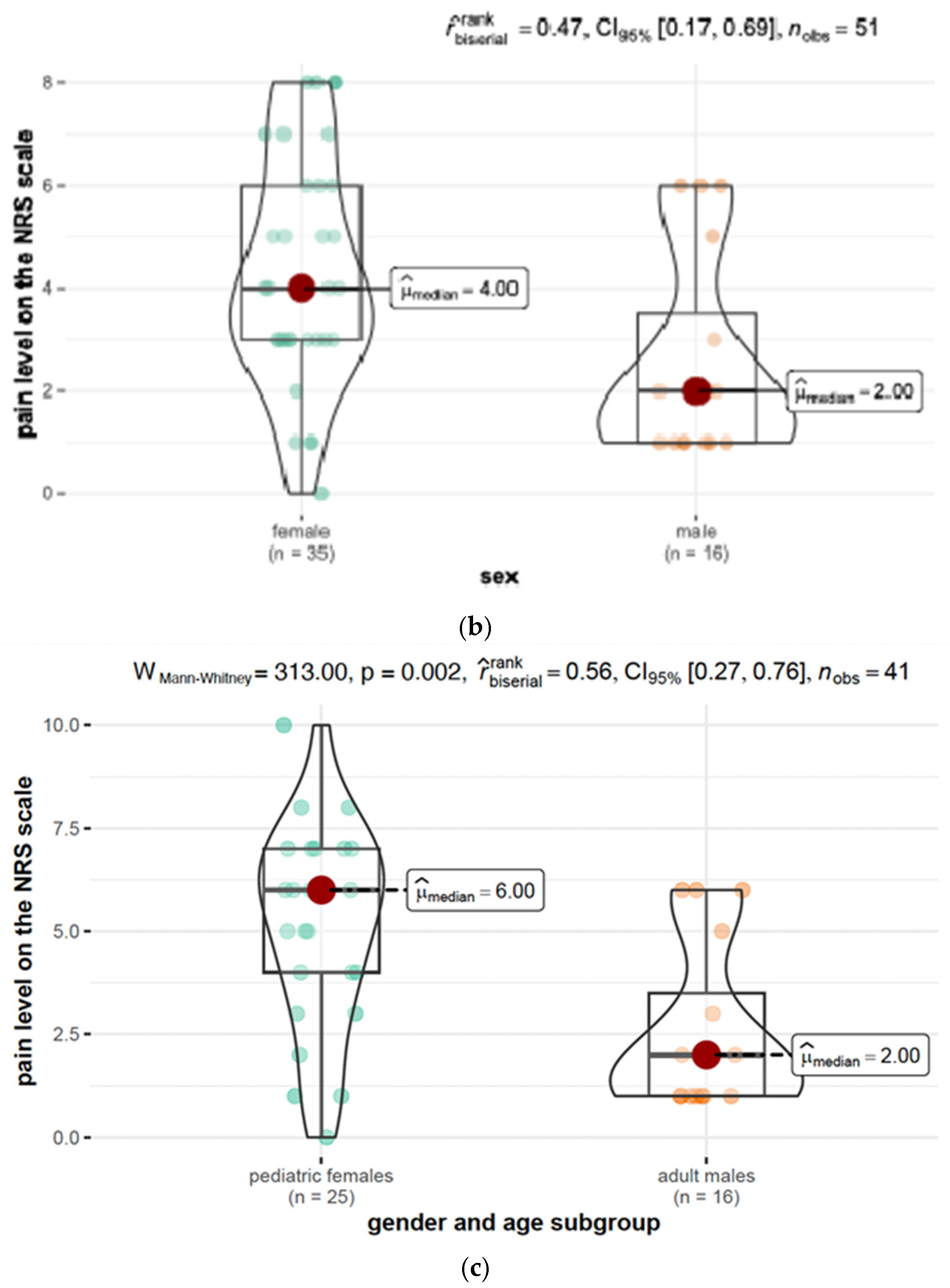
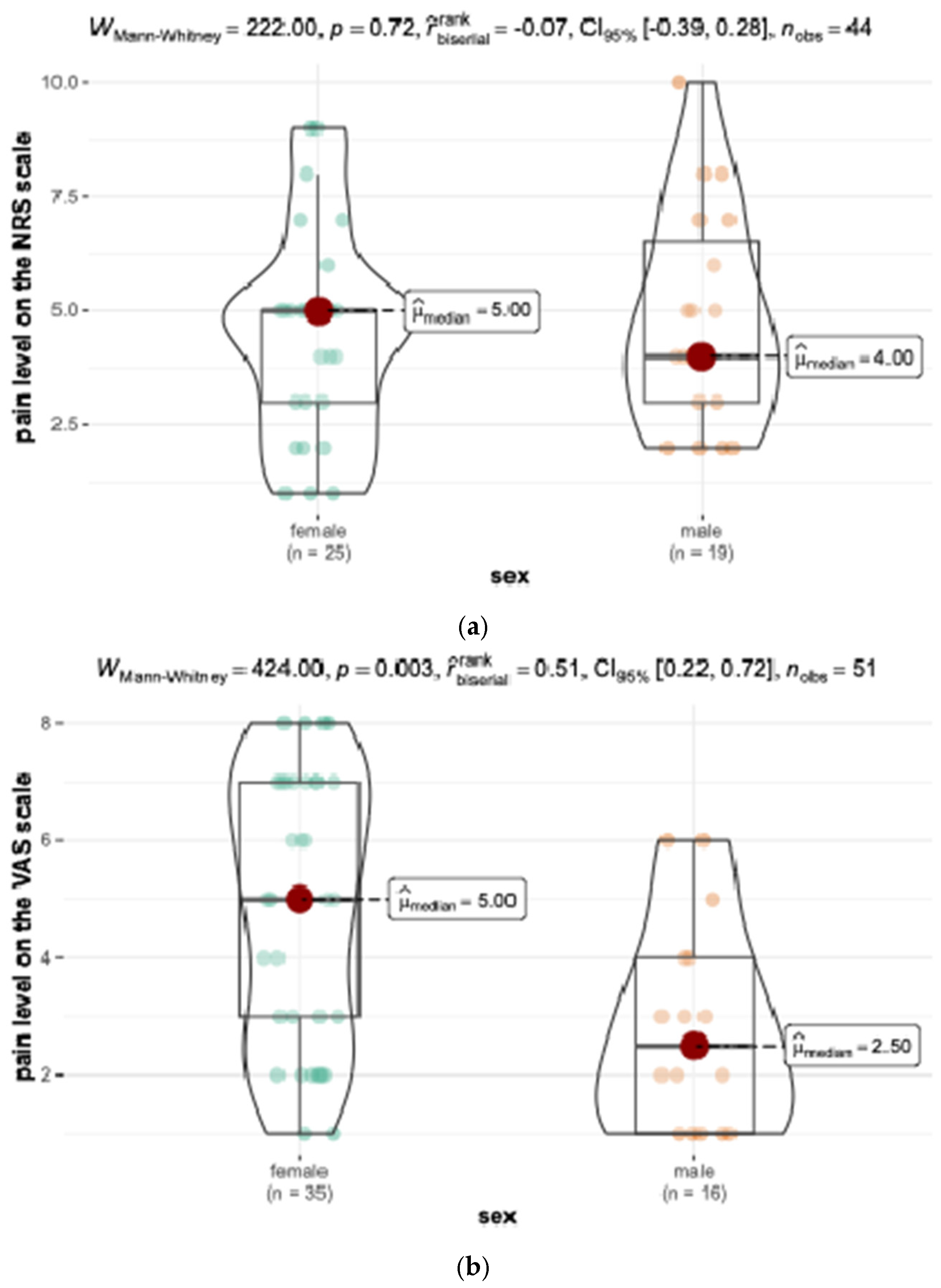
- Adult males reported the lowest pain level, whereas adolescent females reported the highest pain level, both during SRME and FA treatments.
- -
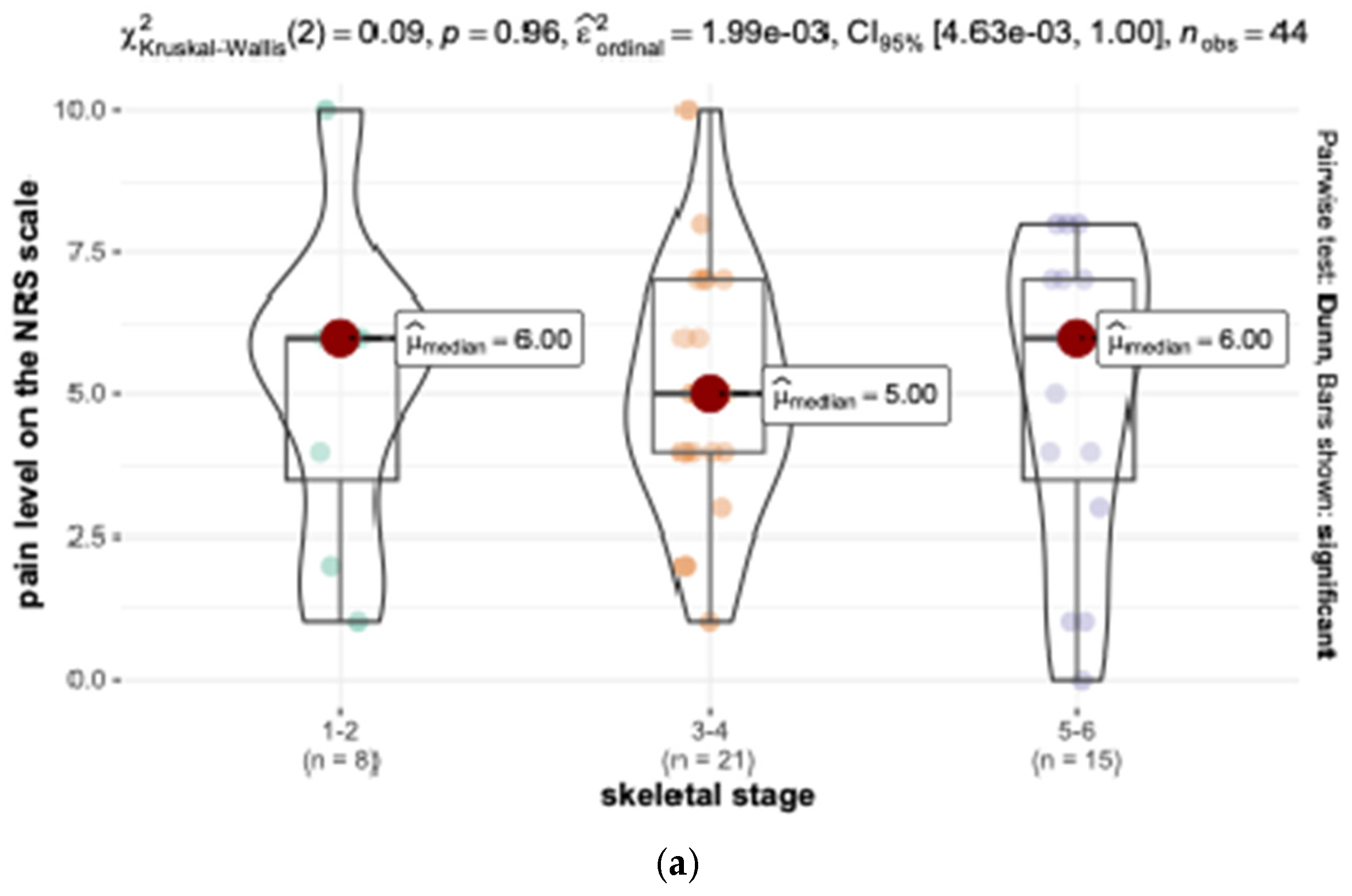
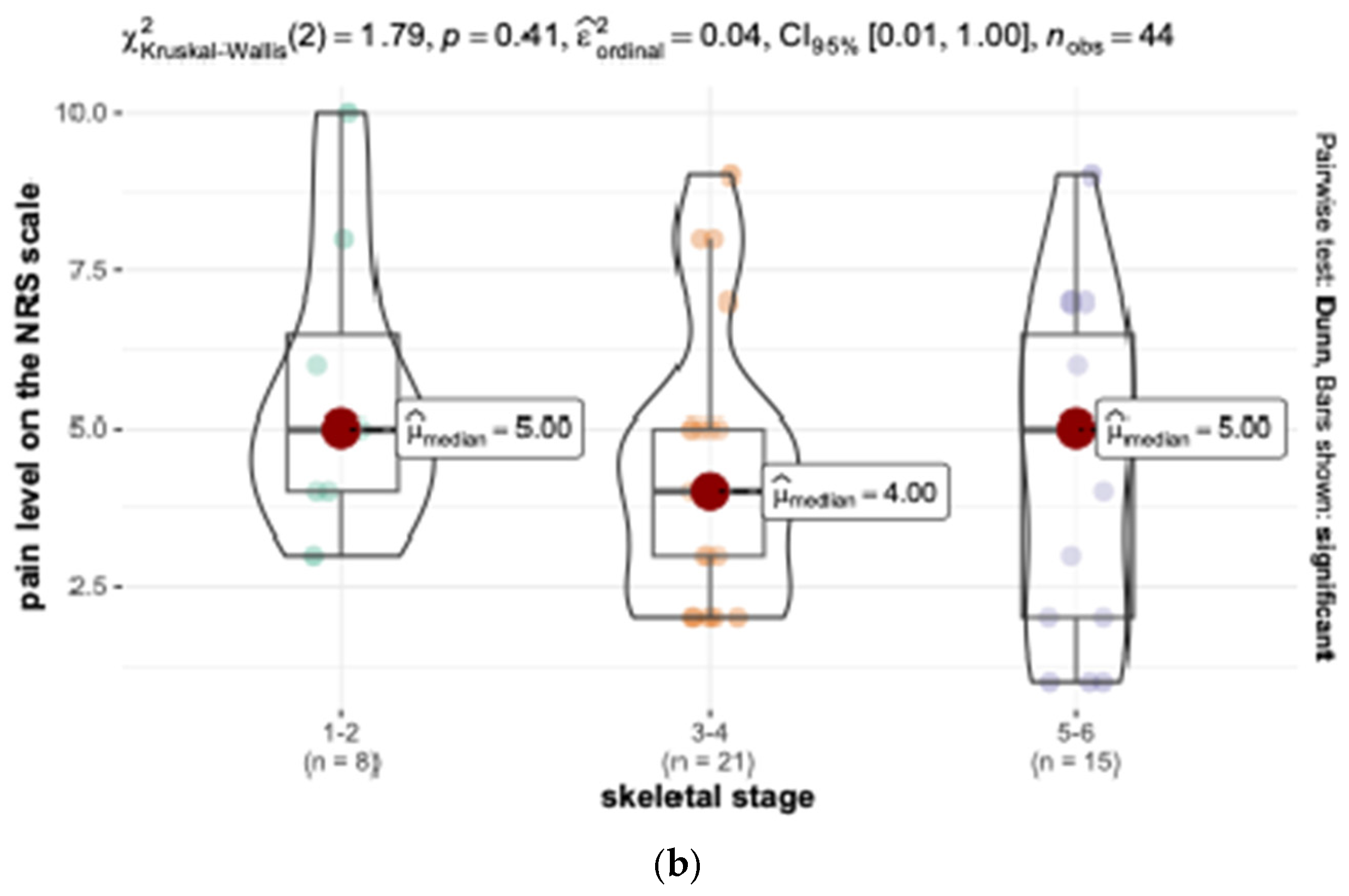
- Both SRME and FA therapies seemed to be less painful for adolescents during peak pubertal growth than during other stages.
- -
- The relation between palatal suture opening and metrical age of patients needs more research on larger groups of adult and adolescent patients.
- -
- Speaking difficulties were most pronounced during the treatment with the Haas-type acrylic splint expander, while pressure sores were most uncomfortable during FA therapy.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Negruțiu, B.M.; Vaida, L.L.; Judea-Pusta, C.; Romanec, C.; Moca, A.E.; Costea, C.P.; Staniș, C.E.; Rus, M. Orthodontic Pain and Dietary Impact Considering Age Groups: A Comparative Study. J. Clin. Med. 2024, 13, 1069. [Google Scholar] [CrossRef] [PubMed]
- Ganzer, N.; Feldmann, I.; Bondemark, L. Pain and discomfort following insertion of miniscrews and premolar extractions: A randomized controlled trial. Angle Orthod. 2016, 86, 891–899. [Google Scholar] [CrossRef]
- Diddige, R.; Negi, G.; Kiran, K.V.S.; Chitra, P. Comparison of pain levels in patients treated with 3 different orthodontic appliances—A randomized trial. Med. Pharm. Rep. 2020, 93, 81–88. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- de Paiva, T.T.; Barros, D.M.C.; Bittencourt, R.C.; Savelli, M.B.B.; Lorenzoni, D.C.; de Alcantara Cury-Saramago, A.; Mattos, C.T. Pain perception and expectation related to interradicular mini-implants insertion: A systematic review and meta-analysis. Clin. Oral. Investig. 2023, 27, 7029–7043. [Google Scholar] [CrossRef]
- Barone, M.; De Stefani, A.; Cavallari, F.; Gracco, A.; Bruno, G. Pain during Rapid Maxillary Expansion: A Systematic Review. Children 2023, 10, 666. [Google Scholar] [CrossRef]
- Rutili, V.; Nieri, M.; Franceschi, D.; Pierleoni, F.; Giuntini, V.; Franchi, L. Comparison of rapid versus slow maxillary expansion on patient-reported outcome measures in growing patients: A systematic review and meta-analysis. Prog. Orthod. 2022, 12, 23–47. [Google Scholar] [CrossRef] [PubMed]
- Ugolini, A.; Cossellu, G.; Farronato, M.; Silvestrini-Biavati, A.; Lanteri, V. A multicenter, prospective, randomized trial of pain and discomfort during maxillary expansion: Leaf expander versus hyrax expander. Int. J. Paediatr. Dent. 2020, 30, 421–428. [Google Scholar] [CrossRef]
- Nieri, M.; Paoloni, V.; Lione, R.; Barone, V.; Marino Merlo, M., Jr.; Giuntini, V.; Cozza, P.; Franchi, L. Comparison between two screws for maxillary expansion: A multicenter randomized controlled trial on patient’s reported outcome measures. Eur. J. Orthod. 2021, 43, 293–300. [Google Scholar] [CrossRef]
- Pasqua, B.P.M.; André, C.B.; Paiva, J.B.; Rino Neto, J. Short-term assessment of pain and discomfort during rapid maxillary expansion with tooth-bone-borne and tooth-borne appliances: Randomized clinical trial. Dental Press. J. Orthod. 2023, 28, e2322220. [Google Scholar] [CrossRef]
- Hansson, S.; Josefsson, E.; Lindsten, R.; Magnuson, A.; Bazargani, F. Pain and discomfort during the first week of maxillary expansion using two different expanders: Patient-reported outcomes in a randomized controlled trial. Eur. J. Orthod. 2023, 45, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.; Zhou, J.; Long, H.; Gao, Y.; Wang, Q.; Li, X.; Wang, Y.; Lai, W.; Jian, F. Molecular mechanism in trigeminal nerve and treatment methods related to orthodontic pain. J. Oral. Rehabil. 2022, 49, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Ko, C.C.; Chung, M.K. Nociceptor mechanisms underlying pain and bone remodeling via orthodontic forces: Toward no pain, big gain. Front. Pain Res. 2024, 22, 1365194, eCollection 2024. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, V. Orthodontic pain: From causes to management—A review. Eur. J. Orthod. 2007, 29, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, S.S.; Sandhu, J. Orthodontic pain: An interaction between age and sex in early and middle adolescence. Angle Orthod. 2013, 83, 966–972. [Google Scholar] [CrossRef]
- Banker, A.M.; Thakkar, M.N.; Desai, B.B.; Huja, S.S. Post-Expansion and End of Treatment Outcomes of Semi-Rapid Maxillary Expansion with a Modified Removable Appliance. Indian J. Dent. Res. 2022, 33, 63–68. [Google Scholar] [CrossRef]
- Baldini, A.; Nota, A.; Santariello, C.; Assi, V.; Ballanti, F.; Cozza, P. Influence of activation protocol on perceived pain during rapid maxillary expansion. Angle Orthod. 2015, 85, 1015–1020. [Google Scholar] [CrossRef]
- Yacout, Y.M.; Abdalla, E.M.; El Harouny, N.M. Patient-reported outcomes of slow vs rapid miniscrew-supported maxillary expansion in adolescents: Secondary outcomes of a randomized clinical trial. Angle Orthod. 2022, 93, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Needleman, H.L.; Hoang, C.D.; Allred, E.; Hertzberg, J.; Berde, C. Reports of pain by children undergoing rapid palatal expansion. Pediatr. Dent. 2000, 22, 221–226. [Google Scholar]
- Abed Al Jawad, F.H.; Alhashimi, N.A. Evaluation of self-perceived pain and jaw function impairment in children undergoing slow and rapid maxillary expansion. Angle Orthod. 2021, 91, 725–732, Bihelix vs Hyrax on 4 bands. [Google Scholar] [CrossRef] [PubMed]
- Altuhafy, M.; Jabr, L.; Michelogiannakis, D.; Khan, J. Self-perceived pain in Hyrax versus other maxillary expansion orthodontic appliances: A systematic review of clinical studies. Eur. Arch. Paediatr. Dent. 2023, 24, 279–292. [Google Scholar] [CrossRef] [PubMed]
- Williamson, A.; Hoggart, B. Pain: A review of three commonly used pain rating scales. J. Clin. Nurs. 2005, 14, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Handelman, C.S.; Wang, L.; BeGole, E.A.; Haas, A.J. Nonsurgical rapid maxillary expansion in adults: Report on 47 cases using the Haas expander. Angle Orthod. 2000, 70, 129–144. [Google Scholar] [PubMed]
- Ramoglu, S.I.; Sari, Z. Maxillary expansion in the mixed dentition: Rapid or semi-rapid? Eur. J. Orthod. 2010, 32, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Bin Dakhil, N.; Bin Salamah, F. The Diagnosis Methods and Management Modalities of Maxillary Transverse Discrepancy. Cureus 2021, 13, e20482. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gecgelen, M.; Aksoy, A.; Kirdemir, P.; Doguc, D.K.; Cesur, G.; Koskan, O.; Ozorak, O. Evaluation of stress and pain during rapid maxillary expansion treatments. J. Oral. Rehabil. 2012, 39, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Basciftci, F.A.; Karaman, A.I. Effects of a modified acrylic bonded rapid maxillary expansion appliance and vertical chin cap on dentofacial structures. Angle Orthod. 2002, 72, 61–71. [Google Scholar] [CrossRef] [PubMed]
- Önçağ, G.; Dindaroğlu, F.; Doğan, S. Perception of pain during rapid palatal expansion. Turk. J. Orthod. 2011, 24, 111–122. [Google Scholar] [CrossRef]
- Feldmann, I.; Bazargani, F. Pain and discomfort during the first week of rapid maxillary expansion (RME) using two different RME appliances: A randomized controlled trial. Angle Orthod. 2017, 87, 391–396. [Google Scholar] [CrossRef]
- Ghergu Jianu, A.; Chaqués-Asensi, J.; Llamas Carreras, J.M.; Perillo, L. Nonsurgical maxillary expansion in adults: Report on clinical cases using the Hyrax expander. Minerva Stomatol. 2019, 68, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Cerritelli, L.; Hatzopoulos, S.; Catalano, A.; Bianchini, C.; Cammaroto, G.; Meccariello, G.; Iannella, G.; Vicini, C.; Pelucchi, S.; Skarzynski, P.H.; et al. Rapid Maxillary Expansion (RME): An Otolaryngologic Perspective. J. Clin. Med. 2022, 11, 5243. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cossellu, G.; Lanteri, V.; Lione, R.; Ugolini, A.; Gaffuri, F.; Cozza, P.; Farronato, M. Efficacy of ketoprofen lysine salt and paracetamol/ acetaminophen to reduce pain during rapid maxillary expansion: A randomized controlled clinical trial. Int. J. Paediatr. Dent. 2019, 29, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Capelozza Filho, L.; da Silva Filho, O.G.; Ursi, W.J. Non-surgically assisted rapid maxillary expansion in adults. Int. J. Adults Orthodon Orthognath. Surg. 1996, 11, 57–66. [Google Scholar]
- Alpernern, M.C.; Yurosko, J. Rapid palatal expansion in adults with and without surgery. Angle Orthod. 1987, 3, 245–263. [Google Scholar]
- El Naghy, R.; Al-Qawasmi, R.; Hasanin, M. Do patient-reported outcomes of miniscrew-supported maxillary expansion in adolescent patients differ between slow and rapid activation protocol? Evid. Based Dent. 2023, 24, 28–29. [Google Scholar] [CrossRef] [PubMed]
- Halicioglu, K.; Kiki, A.; Yayuz, I. Subjective symptoms of RME patients treated with three different screw activation protocols: A randomised clinical trial. Aust. Orthod. J. 2012, 28, 225–231. [Google Scholar]
- Canalis, E.; Delany, A.M. Mechanisms of glucocorticoid action in bone. Ann. N. Y Acad. Sci. 2002, 966, 73–81. [Google Scholar] [CrossRef]
- Debono, M.; Ghobadi, C.; Rostami-Hodjegan, A.; Huatan, H.; Campbell, M.J.; Newell-Price, J.; Darzy, K.; Merke, D.P.; Arlt, W.; Ross, R.J. Modified-release hydrocortisone to provide circadian cortisol profiles. J. Clin. Endocrinol. Metab. 2009, 94, 1548–1554. [Google Scholar] [CrossRef]
- Bhake, R.C.; Kluckner, V.; Stassen, H.; Russell, G.M.; Leendertz, J.; Stevens, K.; Linthorst, A.C.E.; Lightman, S.L. Continuous Free Cortisol Profiles—Circadian Rhythms in Healthy Men. J. Clin. Endocrinol. Metab. 2019, 104, 5935–5947. [Google Scholar] [CrossRef]
- Chyun, Y.S.; Kream, B.E.; Raisz, L.G. Cortisol Decreases Bone Formation by Inhibiting Periosteal Cell Proliferation. Endocrinology 1984, 114, 477–480. [Google Scholar] [CrossRef]
- Kucharz, E.J. Hormonal control of collagen metabolism. Part. II. Endocrinol. 1988, 26, 229–237. [Google Scholar] [PubMed]
- Chiodini, I.; Scillitani, A. Role of cortisol hypersecretion in the pathogenesis of osteoporosis. Recenti Prog. Med. 2008, 99, 309–313. [Google Scholar] [PubMed]
- Chotiyarnwong, P.; McCloskey, E.V. Pathogenesis of glucocorticoid-induced osteoporosis and options for treatment. Nat. Rev. Endocrinol. 2020, 16, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Heshmati, H.M.; Riggs, B.L.; Burritt, M.F.; McAlister, C.A.; Wollan, P.C.; Khosla, S. Effects of the circadian variation in serum cortisol on markers of bone turnover and calcium homeostasis in normal postmenopausal women. J. Clin. Endocrinol. Metab. 1998, 83, 751–756. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, S.S.; Leckie, G. Diurnal variation in orthodontic pain: Clinical implications and pharmacological management. Semin. Orthod. 2018, 24, 217–224. [Google Scholar] [CrossRef]
- Inauen, D.S.; Papadopoulou, A.K.; Eliades, T.; Papageorgiou, S.N. Pain profile during orthodontic levelling and alignment with fixed appliances reported in randomized trials: A systematic review with metaanalyses. Clinical Oral. Investig. 2023, 27, 1851–1868. [Google Scholar] [CrossRef]
- Lord, S.M.; Kepreotes, E.A. Pain in adolescence: A time of vulnerability and opportunity. Pain. Manag. Today 2017, 4, 6–14. [Google Scholar]
- Gobina, I.; Villberg, J.; Välimaa, R.; Tynjälä, J.; Whitehead, R.; Cosma, A.; Brooks, F.; Cavallo, F.; Ng, K.; de Matos, M.G.; et al. Prevalence of self-reported chronic pain among adolescents: Evidence from 42 countries and regions. Eur. J. Pain. 2019, 23, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Chambers, C.T.; Dol, J.; Tutelman, P.R.; Langley, C.L.; Parker, J.A.; Cormier, B.T.; Macfarlane, G.J.; Jones, G.T.; Chapman, D.; Proudfoot, N.; et al. The prevalence of chronic pain in children and adolescents: A systematic review update and meta-analysis. Pain. 2024, 165, 2215–2234. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Almallah, M.M.E.; Hajeer, M.Y.; Almahdi, W.H.; Burhan, A.S.; Latifeh, Y.; Madkhaneh, S.K. Assessment of a single versus double application of low-level laser therapy in pain reduction following orthodontic elastomeric separation: A randomized controlled trial. Dent. Med. Probl. 2020, 57, 45–52. [Google Scholar] [CrossRef]
- Adamczyk, W.M.; Farley, D.; Wiercioch-Kuzianik, K.; Bajcar, E.A.; Buglewicz, E.; Nastaj, J.; Gruszka, A.; Bąbel, P. Memory of pain in adults: A protocol for systematic review and meta-analysis. Syst. Rev. 2019, 8, 201. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kamińska, I. Orthodontic effects of midpalatal suture separation. Ann. Acad. Medicae Stetin. 2008, 54, 94–105. [Google Scholar]
- Chamberland, S. Maxillary expansion in nongrowing patients. Conventional, surgical, or miniscrew-assisted, an update. J. World Fed. Orthod. 2023, 12, 173–183. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | N (%) | Age Group | p | |
|---|---|---|---|---|
| Adolescents, | Adults, | |||
| female | 60 (63.16%) | 25 (56.82%) | 35 (68.63%) | 0.234 (Pearson’s chi-square test) |
| male | 35 (36.84%) | 19 (43.18%) | 16 (31.37%) | |
| total | 95 (100%) | 44 (46.32%) | 51 (53.68%) | |
| age, years. Mdn (Q1, Q3): | 18.34 (16.08, 25.61) | 15.77 (13.26, 16.60) | 25.23 (21.51, 29.03) | <0.001 (Mann–Whitney U test) |
| skeletal class: | ||||
| Class I | 9 (9.47%) | 6 (13.64%) | 3 (5.88%) | 0.222 (Fisher’s exact test) |
| Class II | 18 (18.95%) | 8 (18.18%) | 10 (19.61%) | |
| Class III | 68 (71.58%) | 30 (68.18%) | 38 (74.5%) | |
| Characteristic | Overall Cohort (N = 95) | Age Group | p c | |
|---|---|---|---|---|
| Adolescents n1 = 44 a | Adults n2 = 51 a | |||
| Skeletal stage: Mdn (Q1, Q3) b | 6.00 (4.00, 6.00) | 4.00 (3.00, 5.00) | 6.00 (6.00, 6.00) | <0.001 d |
| Diastema occurrence | 69 (72.63%) | 36 (81.82%) | 33 (64.71%) | 0.062 |
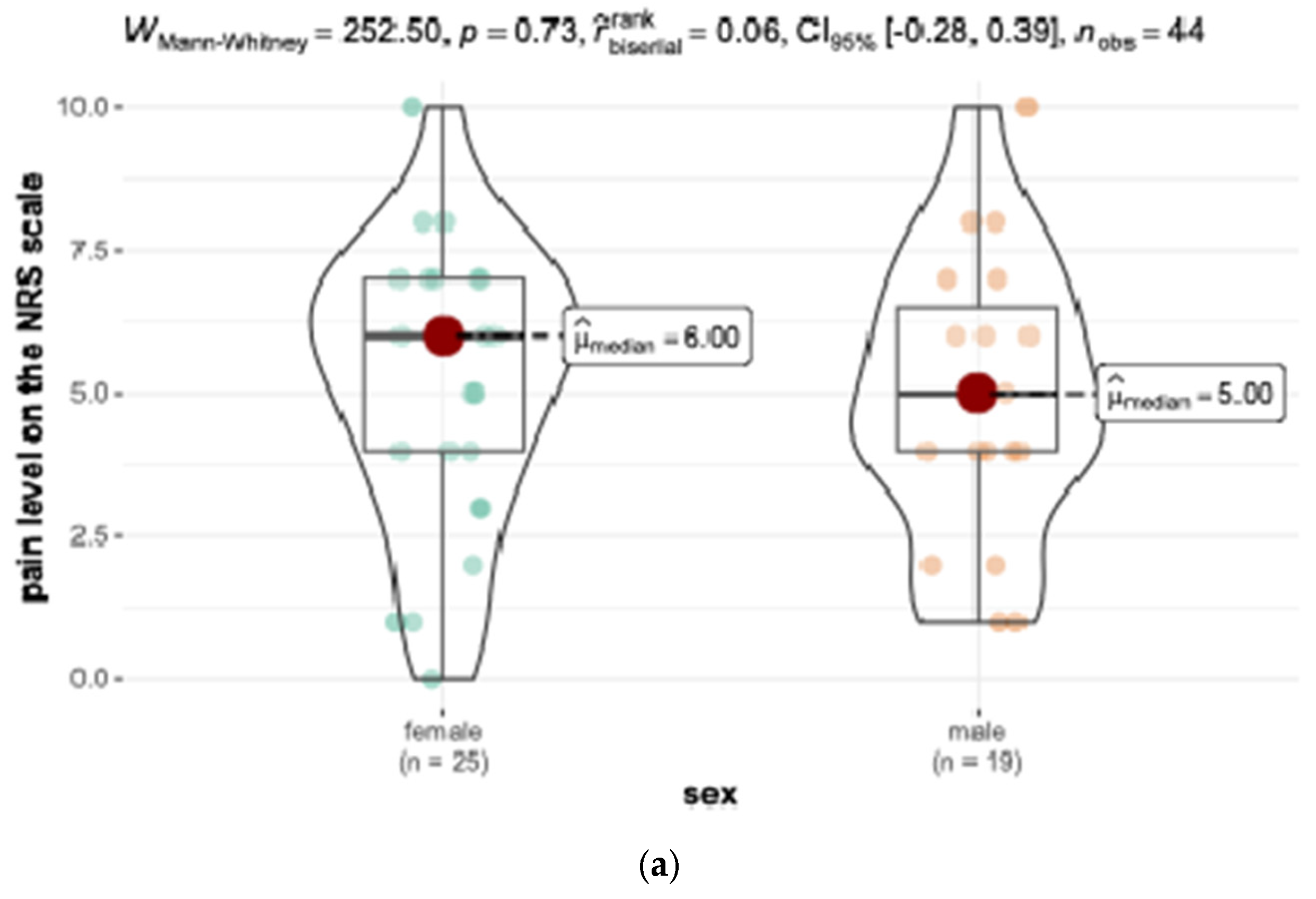
| Level of pain on NRS during the SRME activation: Mdn (Q1, Q3) b | 4.00 (2.50, 6.00) | 5.00 (4.00, 7.00) | 3.00 (2.00, 5.50) | 0.009 d |
| Main disadvantage reported: | ||||
| pain | 18 (18.95%) | 12 (27.27%) | 6 (11.76%) | 0.054 |
| pressure sores | 14 (14.74%) | 7 (15.91%) | 7 (13.73%) | 0.765 |
| speech difficulties | 48 (50.53%) | 20 (45.45%) | 28 (54.90%) | 0.358 |
| headache | 2 (2.11%) | 0 (0.00%) | 2 (3.92%) | 0.497 e |
| other ailments | 12 (12.63%) | 4 (9.09%) | 8 (15.69%) | 0.335 e |
| no ailments | 2 (2.11%) | 1 (2.27%) | 1 (1.96%) | 1.000 e |
| Level of pain on the NRS during fixed appliance therapy: Mdn (Q1, Q3) b | 4.00 (2.00, 6.00) | 4.50 (3.00, 6.00) | 4.00 (2.00, 6.00) | 0.493 d |
| pain | 19 (20.00%) | 12 (27.27%) | 7 (13.73%) | 0.100 |
| pressure sores | 31 (32.63%) | 13 (29.55%) | 18 (35.29%) | 0.551 |
| speech difficulties | 2 (2.11%) | 1 (2.27%) | 1 (1.96%) | 1.000 e |
| eating difficulties | 5 (5.26%) | 1 (2.27%) | 4 (7.84%) | 0.369 e |
| other ailments | 19 (20.00%) | 8 (18.18%) | 11 (21.57%) | 0.681 |
| no ailments | 20 (21.05%) | 10 (22.73%) | 10 (19.61%) | 0.710 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuc-Michalska, M.; Pokucińska, M.; Janiszewska-Olszowska, J. Is Pain Stronger in Adults or in Adolescents During Semi-Rapid Maxillary Expansion (SRME) and Fixed Appliance (FA) Therapies? Appl. Sci. 2025, 15, 2622. https://doi.org/10.3390/app15052622
Kuc-Michalska M, Pokucińska M, Janiszewska-Olszowska J. Is Pain Stronger in Adults or in Adolescents During Semi-Rapid Maxillary Expansion (SRME) and Fixed Appliance (FA) Therapies? Applied Sciences. 2025; 15(5):2622. https://doi.org/10.3390/app15052622
Chicago/Turabian StyleKuc-Michalska, Małgorzata, Magdalena Pokucińska, and Joanna Janiszewska-Olszowska. 2025. "Is Pain Stronger in Adults or in Adolescents During Semi-Rapid Maxillary Expansion (SRME) and Fixed Appliance (FA) Therapies?" Applied Sciences 15, no. 5: 2622. https://doi.org/10.3390/app15052622
APA StyleKuc-Michalska, M., Pokucińska, M., & Janiszewska-Olszowska, J. (2025). Is Pain Stronger in Adults or in Adolescents During Semi-Rapid Maxillary Expansion (SRME) and Fixed Appliance (FA) Therapies? Applied Sciences, 15(5), 2622. https://doi.org/10.3390/app15052622







