1. Introduction
Vibration therapy (VT) is a low-magnitude high-intensity physical agent modality representing a proper way to safely deliver relevant mechanical stimuli as an option to improve musculoskeletal strength and physical performance in the rehabilitation field [
1,
2,
3,
4]. Two wide categories of vibrating devices are available: the whole-body vibration (WBV) approach and vibration devices locally applied, i.e., the mechanical Focal Vibration (mFV). Both modality applications exploit a mechanical stimulation defined by a frequency (in Hz) and by the amplitude of the oscillation generated by a peak-to-peak micrometer shift, but the modality applications differ in area and application [
5,
6,
7,
8,
9].
WBV appears to increase muscle spindle activity, thus lowering the muscle activation threshold and providing greater background tension and less disruption of excitation–contraction coupling [
10].
The mFV is able to activate single muscle fibers, selectively stimulating the Ia and IIb fibers as well as the Golgi tendon organs with respect to a selected application frequency, thus ensuring an improvement in proprioceptive response as well as in muscle trophism [
11]. Regarding the sensitivity of proprioceptors to low-amplitude vibrations applied to muscle tendons, Ia fibers were found to be the most sensitive, responding in a one-to-one fashion up to 180 Hz, thus firing harmonically with vibrations up to 80 Hz and then subharmonically at higher frequencies [
12]. In this scenario, with tonic contraction of the receptor muscle, the sensitivity of the Golgi tendon organs increased in response to the vibratory stimulus [
12]. Aboutorabi et al. [
13] demonstrated the positive effect of mFV on balance and gait in the elderly; the administration of vibrating insoles in conjunction with limited ankle and foot mFV application provided reliability. Among other things, the mFV approach might deliver mechanical stimulation to the bone and muscle–tendon structures, thus reproducing motion and exercise as well as influencing muscle functioning and recovery [
14].
In this scenario, numerous applications of mFV diverge based on the body areas considered, the parameters set, the amplitude and frequency of administration, as well as, in part, the therapist coordinating the physical therapy and any considerations subsequent to the follow-up of short- and long-term outcomes [
5]. Further, there are widespread differences between protocols in the characterization of conceivable advantageous application properties and thus of the most active vibrational features [
15].
Muscle injuries are the most prevalent type of injury encountered in sports, presenting a significant challenge for primary care physicians and sports medicine specialists [
16]. The general process of injury and subsequent repair is remarkably consistent across various muscle injury types; nevertheless, this process is characterized by three distinct phases: The destruction and inflammatory phase, with a breakdown of muscle tissue and the activation of the body’s inflammatory response, which lasts up to a maximum of 3 days. The next phase is the repair phase; the body focuses on regenerating the damaged muscle fibers and forming new connective tissue, which lasts for 3 to 4 weeks. Lastly, we have the remodeling phase, which can take 3 to 6 months and involves a gradual strengthening and reorganization of the repaired muscle tissue [
17].
In elite athletes, McAleer et al. reported that the time to return to training for grade II rectus femoris injuries ranges from 26 to 42 days [
18].
The scar tissue shaped during the healing process is structurally inferior to the original muscle fibers, making it less capable of performing the same functions and more susceptible to re-injury. To minimize disability and promote a full recovery, current conservative treatment focuses on limiting bleeding and inflammation through compression, elevation, and local cooling. Nonsteroidal anti-inflammatory drugs (NSAIDs) are also used to reduce pain and inflammation, while physical therapy plays a crucial role in restoring muscle strength, flexibility, and range of motion [
19]. This comprehensive approach aims to optimize healing and minimize the long-term impact of musculoskeletal injuries [
20]. Turner et al. [
21] demonstrated that local dynamic loading can stimulate and influence musculoskeletal tissue. In fact, the acute efficacy of a single WBV administration might comprise a rise in muscular strength, power output, and jump performance [
22,
23]. Currently, there is little data on the definition of vibrational recovery approaches, and these gaps provide little reliable research regarding the characterization of the most effective and appropriate intensities, frequencies, and application of mFV.
Therefore, the aim of this case report was to assess the administration of mechanical Focal Vibration, via a 2-probes application, in an adult male amateur runner with a grade II lesion of the rectus femoris muscle.
2. Materials and Methods
This case study was conducted in accordance with the ethical guidelines outlined in the Helsinki Declaration, ensuring the well-being and rights of the participant. The study was also approved by the Regional Ethics Committee of Calabria (number: 267/2024), demonstrating its adherence to ethical standards for human research.
2.1. Case Presentation
An adult male (age, 39 years; weight, 76 kg; height, 1.74 m) volunteered and gave informed consent to participate in this study and to publish the images. This is a healthy and trained individual; he is a runner. He had to stop training two years ago and recently started running at least 2 days a week (5 km for 30 min/session). Two weeks later, he wasn’t feeling well. He described a distressing muscle pain, muscle soreness, and stiffness in the right thigh. He performed an ultrasound exam of the thigh, which showed a grade II muscle injury of the rectus femoris. The patient came to our observation in the outpatient service of the University Hospital of Catanzaro and the specialist prescribed him treatment with focal vibration.
2.2. Vibratory Stimulation Technique
The mechanical perturbation was applied by a ViSS One Evolution device v5.2.13 (Manufactured by Vissman S.r.l., Rome, Italy), a device equipped with a source that releases square wave mechano–sonic vibrations. The device further features an electromechanical probe and incorporates a transducer, a structural support, and a control unit for square-modulated power wave generation at a frequency of 100 Hz and a force ranging from 4 to 6 Newtons, thus resulting in a minimal displacement of 5 to 15 μm peak-to-peak [
24,
25]. Two probes were administered—one for the rectus femoris muscle and the other for the vastus lateralis—through 80 mm diameter, 140 mm rectangular cups made of acrylonitrile butadiene styrene (ABS).
The patient was instructed to sustain an isometric contraction of the targeted muscle while the force sequences were applied. This contraction was maintained at about 50% of the patient’s Maximum Voluntary Contraction (MVC). The experimental approach involved delivering vibratory stimulation to the skin covering the middle third of the injured quadriceps muscle, as illustrated in
Figure 1.
In this scenario, MI followed a conventional two-week rehabilitation protocol for a quadriceps injury to restore function and minimize pain. The first week involved rest, ice application, and lower limb elevation. As active rest, we recommended light, pain-free movements to maintain mobility. The second week introduced active exercises (isometric contractions) to help preserve strength. Proprioceptive and stretching exercises improve flexibility and prevent tightness.
Ten sessions (5 applications per week) of mechanical vibration were performed across 2 weeks (duration of each application was 20 min, pause time interval between two consecutive applications was approximately 30 s). The quadriceps was maintained in isometric contraction throughout the stimulation. Measurements were performed at baseline (T0) one day after the injury, at the end of treatment (T1), and four weeks after the end of the treatment (T2). This particular vibratory stimulation protocol was designed taking into account the results obtained in our preliminary study on normal subjects, where the extensor torque was measured after vibration.
2.3. Outcome Measures
2.3.1. Pain
As a primary measure, we evaluated the reduction in pain in the treated areas, estimated using the NRS scale that is used to evaluate the pain intensity perceived by the patient during the clinical evaluation, with a score from 0 (no pain) to 10 (worst pain ever experienced) [
26].
2.3.2. Balance
Balance was assessed by analyzing the displacement of the center of pressure from a force plate (Biotech Corporation, Doral, FL, USA) [
27,
28]. The patient’s balance was assessed using a specific protocol that involved standing on one leg under controlled conditions. Before the test, the patient warmed up to adapt to the one-legged stance. The patient stood on one leg for one minute, with the following specifications: knee flexed at 15°, hip joint fully extended, arms crossed over the chest. The Center of Pressure (COP) movement was monitored using a platform that converted analog signals to digital at a sampling rate of 100 Hz. A low-pass filter was applied at 1050 Hz to ensure signal clarity. The mean velocity of the COP was measured in mm/s and the area of the COP ellipse was calculated in mm
2. This method provides a detailed analysis of the patient’s balance and stability, offering insights into their postural control and potential areas for improvement. The COP ellipse area and mean velocity are crucial metrics for evaluating balance performance, especially in clinical settings [
29].
2.3.3. EQ-5D-5L
The EQ-5D-5L is a tool used to measure health-related quality of life. The score consists of five aspects of health (mobility, self-care, daily activities, pain, and mood), grading overall health via a thermometer-like visual analog scale (EQ-VAS) numbered from 0 (“worst” HRQL) to 100 (“best” HRQL) [
30]. The tool can generate 3125 different health profiles and uses a numerical score to reflect how positive or negative a person’s health is. The tool has been shown to be reliable, with scores of 0.81 and 0.83 on two different measures of consistency [
31].
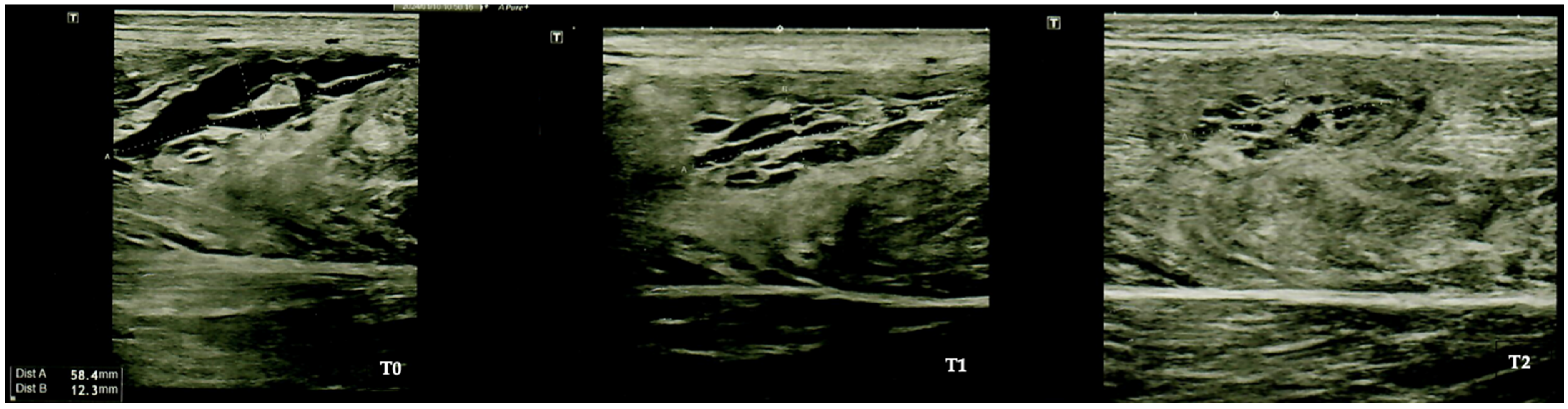
2.3.4. Ultrasound Evaluation
The evaluation of muscle improvements using panoramic B-mode ultrasound involves the use of a sonographic device (Toshiba Aplio 400 ultrasound system, Tokyo, Japan). This advanced diagnostic tool was equipped with a 9 MHz linear array transducer that has a width of 60 mm; the tool was employed by a qualified operator [
32]. Panoramic ultrasound imaging has been repeatedly demonstrated as a valuable tool for monitoring muscle injuries.
3. Results
In the first week post-injury, a joint brace was placed, locked at 0°, and, with the aid of Canadian canes, without putting weight on the injured side. Extended leg raises were performed twice a day, cryotherapy three times a day, as was ankle flexion–extension re-education. After 4 days, the patient removed the brace and performed active and passive knee flexion up to 90°, active and passive flexor stretching, extended leg raises, and cryotherapy, all twice a day. After 21 days, independent walking began and he recovered the correct gait.
The patient followed all prescribed sessions, complaining of no side effects or any discomfort. The results are reported in
Table 1.
Furthermore, through ultrasound evaluation, we observed a significant improvement in the echostructure of the recovery from muscle injury, as depicted in
Figure 2.
4. Discussion
The aim of the study was to evaluate the administration of mechanical Focal Vibration in an adult male amateur runner with a grade II lesion of the rectus femoris muscle. In the last years, VT has been gaining popularity as a possible post-exercise recovery modality to reduce pain and muscle soreness [
33,
34]. The increase in blood flow from WBV could accelerate the recovery process by increasing oxygen delivery, raising muscle temperature, and enhancing the removal of waste products that inhibit tissue repair [
35,
36,
37]. However, the efficacy of WBV for post-exercise recovery remains equivocal; acute WBV showed no benefit on running performance recovery or metabolism following high intensity intermittent running, whereas a repeated bout of WBV following downhill running reduced muscle soreness and muscle inflammation [
33,
38].
The recovery time for mild to moderate muscle injuries usually ranges from 1 to 4 weeks. Severe injuries, however, can require up to 9–12 months to heal completely; furthermore, some factors have a negative impact on recovery: involvement of the tendon tissue, proximity of the injury to the bone, length and sectional area of the lesion [
39,
40].
In this scenario, four weeks after the therapy, the lesion was healed, in line with the healing times demonstrated in the literature; however, we believe it is very interesting to underline the early good recovery in balance (as demonstrated by the reduction in CoP speed (mm/s) from 70.2 ± 13 to 46.7 ± 8 when asking the patient to stand on one leg for 20 s with eyes closed and the knee flexed at 15°, the hip joint fully extended, and with arms crossed over the chest) and the relief of pain (VAS reduced from 8 to 2) which occurred from T0 to T2, allowing the patient a return to sport in a short time.
Regarding muscle recovery and proprioception, the adjunct of mFV to conventional physical therapy highlighted that mFV effectively enhances muscle recovery and balance awareness of the participant. Major findings might suggest that mFV could be considered as safe an approach as other physical agent modalities, such as shortwave diathermy or neuromuscular electrostimulation [
41]. In this scenario, mFV might influence motor coordination and performance [
42]. Finally, mFV may produce short-term recovery effects as early as 60 min after the end of treatment, perhaps suggesting its potential for rapid recovery and rehabilitation from muscle injury [
43].
This case report has some strengths. To the best of our knowledge, no previous study has evaluated the administration of mechanical focal vibration on a grade II muscle injury. The safety of the approach could suggest a relative expansion of the sample; furthermore, the method could reduce the use of pharmacological or minimally invasive therapies, especially in professional sports contexts.
Nonetheless, this study has some limitations. First, it was presented as a case report, which does not provide substantial evidence. Second, it was not possible to investigate the organic and structural improvements in muscle recovery, but only the functional outcomes. Third, the subject included in the study was a senior amateur athlete, so the results might not be generalizable to younger professional subjects.
5. Conclusions
Taken together, the findings of this case report showed that an appropriate mFV might show potential effectiveness in terms of recovery from a grade II rectus femoris muscle injury in a senior runner. Overall, major findings demonstrated a safe role of mFV in sports rehabilitation, particularly in improving pain perception, proprioception, and motor coordination recovery. Major findings suggested that mFV might offer safe physical agent modalities, with noticeable results in a relatively short timeframe.
Further observation studies with larger sample sizes and longer follow-up periods should be performed to provide further evidence on this novel rehabilitative approach in sportsmen with muscle injuries.
Author Contributions
Conceptualization, N.M., E.L., A.d.S. and A.A.; methodology, N.M. and A.d.S.; validation, E.P., V.A. and M.M.; formal analysis, N.M.; investigation, L.S., F.P. and M.T.I.; writing—original draft preparation, N.M. and E.L.; writing—review and editing, U.G.L., A.d.S. and A.A.; visualization, E.P., V.A., M.M., L.S., F.P. and M.T.I.; supervision, A.d.S. and A.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Regional Ethics Committee of Calabria (number: 267/2024).
Informed Consent Statement
Informed consent was obtained from the subject involved in the study. Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The dataset is available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Sañudo, B.; Seixas, A.; Gloeckl, R.; Rittweger, J.; Rawer, R.; Taiar, R.; van der Zee, E.A.; van Heuvelen, M.J.G.; Lacerda, A.C.; Sartorio, A.; et al. Potential Application of Whole Body Vibration Exercise for Improving the Clinical Conditions of COVID-19 Infected Individuals: A Narrative Review from the World Association of Vibration Exercise Experts (Wavex) Panel. Int. J. Environ. Res. Public Health 2020, 17, 3650. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, G. The Use of Vibration as Physical Exercise and Therapy. J. Funct. Morphol. Kinesiol. 2017, 2, 17. [Google Scholar] [CrossRef]
- Moggio, L.; de Sire, A.; Marotta, N.; Demeco, A.; Ammendolia, A. Vibration Therapy Role in Neurological Diseases Rehabilitation: An Umbrella Review of Systematic Reviews. Disabil. Rehabil. 2022, 44, 5741–5749. [Google Scholar] [CrossRef]
- de Sire, A.; Lippi, L.; Ammendolia, A.; Cisari, C.; Venetis, K.; Sajjadi, E.; Fusco, N.; Invernizzi, M. Physical Exercise with or without Whole-Body Vibration in Breast Cancer Patients Suffering from Aromatase Inhibitor—Induced Musculoskeletal Symptoms: A Pilot Randomized Clinical Study. J. Pers. Med. 2021, 11, 1369. [Google Scholar] [CrossRef]
- Germann, D.; El Bouse, A.; Shnier, J.; Abdelkader, N.; Kazemi, M. Effects of Local Vibration Therapy on Various Performance Parameters: A Narrative Literature Review. J. Can. Chiropr. Assoc. 2018, 62, 170–181. [Google Scholar]
- Veqar, Z.; Imtiyaz, S. Vibration Therapy in Management of Delayed Onset Muscle Soreness. J. Clin. Diagn. Res. 2014, 8, LE01–LE04. [Google Scholar] [CrossRef]
- Chu, Y.; Wang, Q.; Chu, M.; Geng, B.; Jia, H.; Li, X.; Lv, T.; Jiang, S. Long-Term Effect of Vibration Therapy for Training-Induced Muscle Fatigue in Elite Athletes. Int. J. Environ. Res. Public Health 2022, 19, 7531. [Google Scholar] [CrossRef]
- Furness, N.D.; Phillips, A.; Gallacher, S.; Beazley, J.C.S.; Evans, J.P.; Toms, A.D.; Thomas, W.; Smith, C.D. Vibration Therapy versus Standard Treatment for Tennis Elbow: A Randomized Controlled Study. J. Orthop. Surg. 2018, 26, 1–7. [Google Scholar] [CrossRef]
- Rabini, A.; de Sire, A.; Marzetti, E.; Gimigliano, R.; Ferriero, G.; Piazzini, D.B.; Iolascon, G.; Gimigliano, F. Effects of Focal Muscle Vibration on Physical Functioning in Patients with Knee Osteoarthritis: A Randomized Controlled Trial. Eur. J. Phys. Rehabil. Med. 2015, 51, 513–520. [Google Scholar]
- Kosar, A.C.; Candow, D.G.; Putland, J.T. Potential Beneficial Effects of Whole-Body Vibration Formuscle Recovery after Exercise. J. Strength Cond. Res. 2012, 26, 2907–2911. [Google Scholar] [CrossRef]
- Fattorini, L.; Rodio, A.; Pettorossi, V.E.; Filippi, G.M. Is the Focal Muscle Vibration an Effective Motor Conditioning Intervention? A Systematic Review. J. Funct. Morphol. Kinesiol. 2021, 6, 39. [Google Scholar] [CrossRef] [PubMed]
- Roll, J.P.; Vedel, J.P.; Ribot, E. Alteration of Proprioceptive Messages Induced by Tendon Vibration in Man: A Microneurographic Study. Exp. Brain Res. 1989, 76, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Aboutorabi, A.; Arazpour, M.; Bahramizadeh, M.; Farahmand, F.; Fadayevatan, R. Effect of Vibration on Postural Control and Gait of Elderly Subjects: A Systematic Review. Aging Clin. Exp. Res. 2018, 30, 713–726. [Google Scholar] [CrossRef] [PubMed]
- Peterson, B.E.; Rolfe, R.A.; Kunselman, A.; Murphy, P.; Szczesny, S.E. Mechanical Stimulation via Muscle Activity Is Necessary for the Maturation of Tendon Multiscale Mechanics During Embryonic Development. Front. Cell Dev. Biol. 2021, 9, 725563. [Google Scholar] [CrossRef]
- de Sire, A.; Lippi, L.; Marotta, N.; Ferrillo, M.; Folli, A.; Turco, A.; Ammendolia, A.; Invernizzi, M. Myths and Truths on Biophysics-Based Approach in Rehabilitation of Musculoskeletal Disorders. Ther. Adv. Musculoskelet. Dis. 2023, 15, 1–11. [Google Scholar] [CrossRef]
- Baoge, L.; Van Den Steen, E.; Rimbaut, S.; Philips, N.; Witvrouw, E.; Almqvist, K.F.; Vanderstraeten, G.; Vanden Bossche, L.C. Treatment of Skeletal Muscle Injury: A Review. ISRN Orthop. 2012, 2012, 689012. [Google Scholar] [CrossRef]
- Järvinen, T.A.H.; Järvinen, M.; Kalimo, H. Regeneration of Injured Skeletal Muscle after the Injury. Muscles Ligaments Tendons J. 2013, 3, 337–345. [Google Scholar] [CrossRef]
- McAleer, S.; Macdonald, B.; Lee, J.; Zhu, W.; Giakoumis, M.; Maric, T.; Kelly, S.; Brown, J.; Pollock, N. Time to Return to Full Training and Recurrence of Rectus Femoris Injuries in Elite Track and Field Athletes 2010–2019; a 9-Year Study Using the British Athletics Muscle Injury Classification. Scand. J. Med. Sci. Sports 2022, 32, 1109–1118. [Google Scholar] [CrossRef]
- Santanna, J.P.C.; Pedrinelli, A.; Hernandez, A.J.; Fernandes, T.L. Muscle Injury: Pathophysiology, Diagnosis, and Treatment. Rev. Bras. Ortop. 2021, 57, 1–13. [Google Scholar] [CrossRef]
- Liao, C.H.; Lin, L.P.; Yu, T.Y.; Hsu, C.C.; Pang, J.H.S.; Tsai, W.C. Ibuprofen Inhibited Migration of Skeletal Muscle Cells in Association with Downregulation of P130cas and CrkII Expressions. Skelet. Muscle 2019, 9, 23. [Google Scholar] [CrossRef]
- Turner, C.H. Functional Determinants of Bone Structure: Beyond Wolff’s Law of Bone Transformation. Bone 1992, 13, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Bosco, C.; Cardinale, M.; Tsarpela, O. Influence of Vibration on Mechanical Power and Electromyogram Activity in Human Arm Flexor Muscles. Eur. J. Appl. Physiol. Occup. Physiol. 1999, 79, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Cerciello, S.; Rossi, S.; Visonà, E.; Corona, K.; Oliva, F. Clinical Applications of Vibration Therapy in Orthopaedic Practice. Muscles Ligaments Tendons J. 2016, 6, 147–156. [Google Scholar] [CrossRef]
- Paolucci, T.; Agostini, F.; Bernetti, A.; Paoloni, M.; Mangone, M.; Santilli, V.; Pezzi, L.; Bellomo, R.G.; Saggini, R. Integration of Focal Vibration and Intra-Articular Oxygen–ozone Therapy in Rehabilitation of Painful Knee Osteoarthritis. J. Int. Med. Res. 2021, 49, 1–12. [Google Scholar] [CrossRef]
- Paolucci, T.; Bellomo, R.G.; Pezzi, L.; Frondaroli, F.; Frondaroli, S.; Santarelli, A.; Barbato, C.; Porreca, A.; Saggini, R. A Novel Rehabilitative Protocol in the Treatment of Mixed Urinary Incontinence in Women: The Effects of Focused Mechano-Acoustic Vibration. Biores. Open Access 2019, 8, 219–228. [Google Scholar] [CrossRef]
- Karcioglu, O.; Topacoglu, H.; Dikme, O.; Dikme, O. A Systematic Review of the Pain Scales in Adults: Which to Use? Am. J. Emerg. Med. 2018, 36, 707–714. [Google Scholar] [CrossRef]
- Marotta, N.; Moggio, L.; Calafiore, D.; Prestifilippo, E.; Spanó, R.; Tasselli, A.; Drago Ferrante, V.; Invernizzi, M.; de Sire, A.; Ammendolia, A. Efficacy of Proprioceptive Training on Plantar Pressure and Jump Performance in Volleyball Players: A Proof-of-Principle Study. Sensors 2023, 23, 1906. [Google Scholar] [CrossRef]
- de Sire, A.; Demeco, A.; Marotta, N.; Spanò, R.; Curci, C.; Farì, G.; Fortunato, F.; Iona, T.; Lippi, L.; Paolucci, T.; et al. Neuromuscular Impairment of Knee Stabilizer Muscles in a COVID-19 Cluster of Female Volleyball Players: Which Role for Rehabilitation in the Post-COVID-19 Return-to-Play? Appl. Sci. 2022, 12, 557. [Google Scholar] [CrossRef]
- Chen, B.; Liu, P.; Xiao, F.; Liu, Z.; Wang, Y. Review of the Upright Balance Assessment Based on the Force Plate. Int. J. Environ. Res. Public Health 2021, 18, 2696. [Google Scholar] [CrossRef]
- Balestroni, G.; Bertolotti, G. EuroQol-5D (EQ-5D): An Instrument for Measuring Quality of Life. Monaldi Arch. Chest Dis. Card. Ser. 2012, 78, 155–159. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and Preliminary Testing of the New Five-Level Version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- Marotta, N.; de Sire, A.; Lippi, L.; Moggio, L.; Mondardini, P.; Sgro, M.; Bartalotta, I.; Zito, R.; Giroldini, T.; Invernizzi, M.; et al. Effectiveness of High-Power Laser Therapy via Shear Wave Speed Analysis on Pain and Functioning in Patients with Lateral Epicondylitis: A Proof-of-Concept Study. J. Clin. Med. 2024, 13, 2014. [Google Scholar] [CrossRef]
- Broadbent, S.; Rousseau, J.J.; Thorp, R.M.; Choate, S.L.; Jackson, F.S.; Rowlands, D.S. Vibration Therapy Reduces Plasma IL6 and Muscle Soreness after Downhill Running. Br. J. Sports Med. 2010, 44, 888–894. [Google Scholar] [CrossRef]
- Rhea, M.R.; Bunker, D.; Marín, P.J.; Lunt, K. Effect of ITonic Whole-Body Vibration on Delayed-Onset Muscle Soreness among Untrained Individuals. J. Strength Cond. Res. 2009, 23, 1677–1682. [Google Scholar] [CrossRef]
- Kerschan-Schindl, K.; Grampp, S.; Henk, C.; Resch, H.; Preisinger, E.; Fialka-Moser, V.; Imhof, H. Whole-Body Vibration Exercise Leads to Alterations in Muscle Blood Volume. Clin. Physiol. 2001, 21, 377–382. [Google Scholar] [CrossRef]
- Cafarelli, E.; Sim, J.; Carolan, B.; Liebesman, J. Vibratory Massage and Short-Term Recovery from Muscular Fatigue. Int. J. Sports Med. 1990, 11, 474–478. [Google Scholar] [CrossRef]
- Weerapong, P.; Hume, P.A.; Kolt, G.S. The Mechanisms of Massage and Effects on Performance, Muscle Recovery and Injury Prevention. Sports Med. 2005, 35, 235–256. [Google Scholar] [CrossRef]
- Edge, J.; Mündel, T.; Weir, K.; Cochrane, D.J. The Effects of Acute Whole Body Vibration as a Recovery Modality Following High-Intensity Interval Training in Well-Trained, Middle-Aged Runners. Eur. J. Appl. Physiol. 2009, 105, 421–428. [Google Scholar] [CrossRef]
- Brumitt, J.; Cuddeford, T. Current Concepts of Muscle and Tendon Adaptation To Strength and Conditioning. Int. J. Sports Phys. Ther. 2015, 10, 748–759. [Google Scholar]
- Heiderscheit, B.C.; Sherry, M.A.; Silder, A.; Chummanov, E.S.; Thelen, D.G. Hamstring Strain Injuries: Recommendations for Diagnosis, Rehabilitation, and Injury Prevention. J. Orthop. Sports Phys. Ther. 2010, 40, 67–81. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Inzitari, M.T.; Caruso, M.G.; Ammendolia, A.; Enix, D. Neuromuscular Electrical Stimulation and Shortwave Diathermy in Unrecovered Bell Palsy: A Randomized Controlled Study. Medicine 2020, 99, e19152. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, O.; Botti, F.M.; Roscini, M.; Brunetti, A.; Panichi, R.; Filippi, G.M.; Biscarini, A.; Pettorossi, V.E. Focal Vibration of Quadriceps Muscle Enhances Leg Power and Decreases Knee Joint Laxity in Female Volleyball Players. J. Sports Med. Phys. Fit. 2012, 52, 596–605. [Google Scholar]
- Filippi, G.M.; Brunetti, O.; Botti, F.M.; Panichi, R.; Roscini, M.; Camerota, F.; Cesari, M.; Pettorossi, V.E. Improvement of Stance Control and Muscle Performance Induced by Focal Muscle Vibration in Young-Elderly Women: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2009, 90, 2019–2025. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).