The Prevalence and Clinical Implications of Atlantal Posterior Arch Defects: A CBCT Analysis of 500 Italian Patients
Abstract
1. Introduction
2. Materials and Methods
- Insufficient image quality (e.g., due to patient movement);
- Region of interest cut-off;
- Presence of congenital lip and palate anomalies or other craniofacial syndromes;
- History of trauma or surgery in the cervical spine;
- Non-Italian nationality.
- Field-of-view (FOV): 240 × 190 mm;
- Normal resolution quality;
- Tube voltage: 80 kVp;
- Tube current: 5 mA;
- Acquisition time: 15 s.
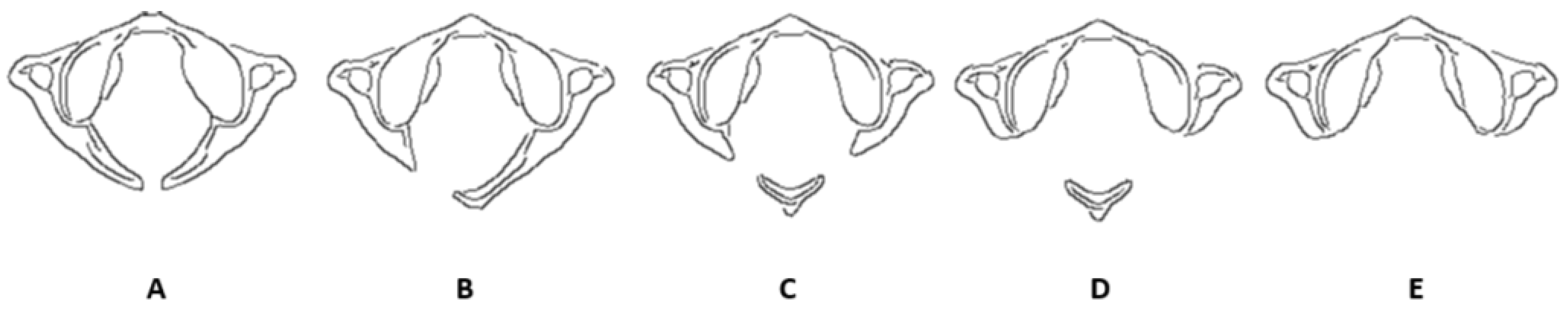
- Type A: Failure of posterior midline fusion of the two hemiarches;
- Type B: Unilateral defect;
- Type C: Bilateral defects;
- Type D: Absence of the posterior arch with a persistent posterior tubercle;
- Type E: Absence of the entire posterior arch, including the tubercle.
- The transverse plane coinciding with the Frankfurt plane (FH), passing through Orbital (Or) and porion (Po);
- The sagittal plane coinciding with the mid-sagittal plane (MSP), perpendicular to the FH and passing through the Crista galli (Cg) and Basion (Ba);
- The coronal plane coinciding with the anteroposterior (PO) plane, perpendicular to the FH and MSP, and passing through the right and left porion.
3. Results
3.1. Prevalence and Classification of APAD
- Partial APAD was the most common form, occurring in twelve cases;
- Complete APAD was observed in one case.
3.2. Age Distribution
- 17–29 years: two cases (15.4% of APAD cases; 1.7% within this age group)
- 30–39 years: four cases (30.8% of APAD cases; 3.1% within this age group)
- 40–49 years: three cases (23.1% of APAD cases; 2.4% within this age group)
- 50–60 years: four cases (30.8% of APAD cases; 3.1% within this age group)
| Age Range | Number of Cases | Percentage (%) |
|---|---|---|
| 17–29 | 2 | 15.4 |
| 30–39 | 4 | 30.8 |
| 40–49 | 3 | 23.1 |
| 50–60 | 4 | 30.8 |
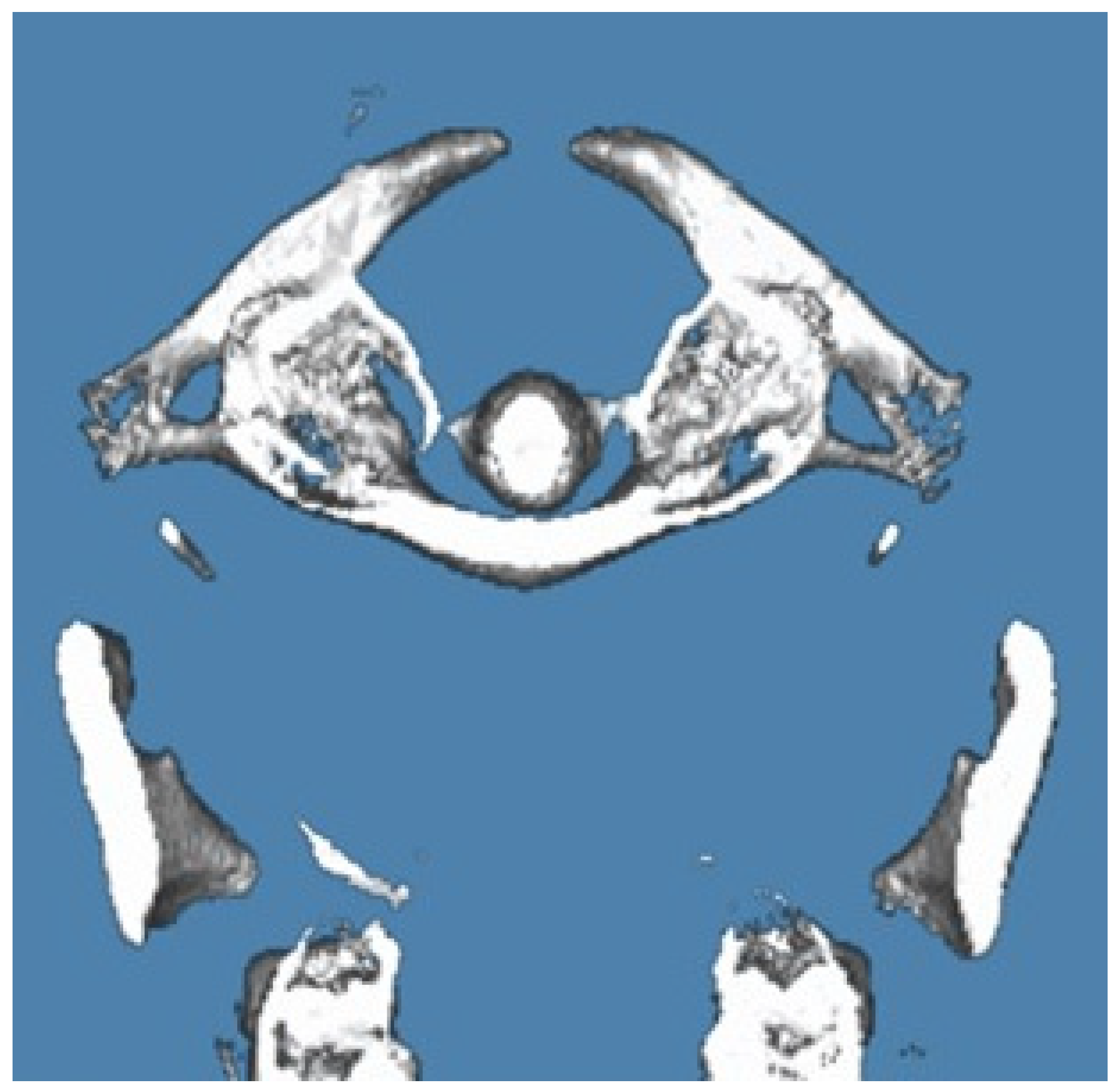
3.2.1. Case Report 1: Bilateral Complete Ponticulus Posticus and Complete Atlantal Posterior Arch Defect Type A in a 17-Year-Old Female: Clinical and Imaging Findings
3.2.2. Case Report 2: Unilateral Partial Ponticulus Posticus and Partial Atlantal Posterior Arch Defect Type A in a 54-Year-Old Female: Clinical Presentation and Imaging Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pasini, M.; Giuca, M.R.; Ligori, S.; Mummolo, S.; Fiasca, F.; Marzo, G.; Quinzi, V. Association between Anatomical Variations and maxillary canine impaction: A retrospective study in orthodontics. Appl. Sci. 2020, 10, 5638. [Google Scholar] [CrossRef]
- Visocchi, M.; Signorelli, F.; Parrilla, C.; Paludetti, G.; Rigante, M. Multidisciplinary approach to the craniovertebral junction. Historical insights, current and future perspectives in the neurosurgical and otorhinolaryngological alliance. ACTA Otorhinolaryngol. Ital. 2021, 41 (Suppl. S1), S51. [Google Scholar] [CrossRef] [PubMed]
- Izzo, R.; Popolizio, T.; Balzano, R.F.; Simeone, A.; Gasparotti, R.; Scarabino, T.; Muto, M. Imaging of cranio-cervical junction traumas. Eur. J. Radiol. 2020, 127, 108960. [Google Scholar] [CrossRef] [PubMed]
- Khanna, R.; Smith, Z.A.; Dlouhy, B.J.; Dahdaleh, N.S. Complete absence of the posterior arch of C1: Case report. J. Craniovertebral Junction Spine 2014, 5, 176–178. [Google Scholar] [CrossRef]
- Wu, W.L.; Shao, X.B.; Shen, Y.G.; Chen, J.S.; Shu, Q. Sex-specific differences in ossification patterns of the atlas and axis: A computed tomography study. World J. Pediatr. WJP 2022, 18, 263–270. [Google Scholar] [CrossRef]
- Currarino GRollins, N.; Diehl, J.T. Congenital defects of the posterior arch of the atlas: A report of seven cases including an affected mother and son. Am. J. Neuroradiol. 1994, 15, 249–254. [Google Scholar]
- Choi, J.W.; Jeong, J.H.; Moon, S.M.; Hwang, H.S. Congenital cleft of anterior arch and partial aplasia of the posterior arch of the c1. J. Korean Neurosurg. Soc. 2011, 49, 178. [Google Scholar] [CrossRef]
- Klimo, P., Jr.; Blumenthal, D.T.; Couldwell, W.T. Congenital partial aplasia of the posterior arch of the atlas causing myelopathy: Case report and review of the literature. Spine 2003, 28, E224–E228. [Google Scholar] [CrossRef]
- Hyun, G.; Allam, E.; Sander, P.; Hasiak, C.; Zhou, Y. The prevalence of congenital C1 arch anomalies. Eur. Spine J. 2018, 27, 1266–1271. [Google Scholar] [CrossRef]
- Elmalky, M.M.; Elsayed, S.; Arealis, G.; Mehdian, H. Congenital C1 arch deficiency: Grand Round presentation. Eur. Spine J. 2013, 22, 1223–1226. [Google Scholar] [CrossRef]
- Macrì, M.; Perrella, G.; Varvara, G.; Murmura, G.; Traini, T.; Rendina, F.; Festa, F. Assessments of Prevalence of Ponticulus Posticus, Atlas Posterior Arch Deficiency, Sella Turcica Bridging, Maxillary Canine Impaction, and Associations Among Them in 500 CBCTs of Italian Orthodontic Patients. Front. Dent. Med. 2021, 2, 708169. [Google Scholar] [CrossRef]
- Torriani, M.; Lourenço, J.L.G. Agenesis of the posterior arch of the atlas. Rev. Do Hosp. Das Clínicas 2002, 57, 73–76. [Google Scholar] [CrossRef] [PubMed]
- Izaki, T.; Shiota, E.; Zhang, J. Aplasia of the posterior arch of the atlas: A proposal for a new clinical classification. Med. Bull. Fukuoka Univ. 2009, 36, 11–16. [Google Scholar]
- Junior, M.G.P.; Ribeiro, R.T.; Landeiro, J.A.; Pessoa, B.L. Hypoplasia of C1’s posterior arch: Is there an ideal anatomical classification? Surg. Neurol. Int. 2021, 12, 623. [Google Scholar] [CrossRef]
- Jin, M.; Asadoorian, M.; Hiller, L.P.; Hughes, T.H. Hypertrophy of the anterior arch of the atlas associated with congenital nonunion of the posterior arch: A retrospective case-control study. Spine J. 2014, 14, 1155–1158. [Google Scholar] [CrossRef]
- Butt, B.B.; Gagnet, P.; Patel, R.; Aleem, I. Congenital defect of the posterior arch of C1: A case report. J. Spine Surg. 2021, 7, 214. [Google Scholar] [CrossRef]
- Ogata, T.; Morino, T.; Hino, M.; Miura, H. Cervical myelopathy caused by atlantoaxial instability in a patient with an os odontoideum and total aplasia of the posterior arch of the atlas: A case report. J. Med. Case Rep. 2012, 6, 171. [Google Scholar] [CrossRef]
- Chau, A.M.T.; Wong, J.H.Y.; Mobbs, R.J. Cervical myelopathy associated with congenital C2/3 canal stenosis and deficiencies of the posterior arch of the atlas and laminae of the axis: Case report and review of the literature. Spine 2009, 34, E886–E891. [Google Scholar] [CrossRef]
- Tan, E.C.; Soon, H.C.; Kevin, M.; To, S. Congenital absence of the posterior arch of the atlas—A strange but benign anomaly. Malays. Orthop. J. 2007, 1, 30–32. [Google Scholar] [CrossRef]
- Sabuncuoğlu, H.; Özdoğan, S.; Karadağ, D.; Timurkaynak, E. Congenital hypoplasia of the posterior arch of the atlas: Case report and extensive review of the literature. Turk. Neurosurg. 2011, 21, 97–103. [Google Scholar] [CrossRef]
- Monsarrat, P.; Galibourg, A.; Nasr, K.; Telmon, N.; Maret, D. Incidental findings in dental radiology are concerning for family doctors. Open Med. 2019, 14, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Senoglu, M.; Safavi-Abbasi, S.; Theodore, N.; Bambakidis, N.C.; Crawford, N.R.; Sonntag, V.K. The frequency and clinical significance of congenital defects of the posterior and anterior arch of the atlas. J. Neurosurg. Spine 2007, 7, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Chitroda, P.K.; Katti, G.; Baba, I.A.; Najmudin, M.; Ghali, S.R.; Kalmath, B.; Vijay, G. Ponticulus posticus on the posterior arch of atlas, prevalence analysis in symptomatic and asymptomatic patients of Gulbarga population. J. Clin. Diagn. Res. JCDR 2013, 7, 3044. [Google Scholar] [PubMed]
- He, Q.; Xu, J. Congenital anterior midline cleft of the atlas and posterior atlanto-occipital fusion associated with symptomatic anterior atlantoaxial subluxation. Eur. J. Orthop. Surg. Traumatol. 2012, 22, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.Y.; Chan, R.T.M.; Fung, V.K.P.; Cheng, C.S. Congenital posterior arch defect of the atlas: Report of a rare anomaly. Hong Kong J. Radiol. 2011, 14, 102–105. [Google Scholar]
- Kim, M.S. Anatomical variant of atlas: Arcuate foramen, occpitalization of atlas, and defect of posterior arch of atlas. J. Korean Neurosurg. Soc. 2015, 58, 528–533. [Google Scholar] [CrossRef]
- Macrì, M.; Rendina, F.; Feragalli, B.; Pegreffi, F.; Festa, F. Prevalence of ponticulus posticus and migraine in 220 orthodontic patients: A cross-sectional study. Biology 2023, 12, 471. [Google Scholar] [CrossRef]

| Classification | Number of Cases | Percentage (%) |
|---|---|---|
| Partial APAD | 12 | 92.3 |
| Complete APAD | 1 | 7.7 |
| APAD with Ponticulus Posticus | 2 | 15.4 |
| Case | Age | Type of APAD | Presence of Ponticulus Posticus | Symptoms | Management | Outcome |
|---|---|---|---|---|---|---|
| 1 | 17 years | Complete APAD | Bilateral Complete | Occasional mild neck stiffness; no significant neurological symptoms | Routine monitoring; no immediate intervention required | Remained symptom-free; routine imaging for follow-up |
| 2 | 54 years | Partial APAD | Unilateral Partial | Mild to moderate neck pain; intermittent tingling in right upper limb | Physical therapy and NSAIDs; follow-up imaging recommended | Symptoms improved; no significant defect progression |
| 3 | 35 years | Partial APAD | None | Occasional neck pain; no significant symptoms reported | Conservative treatment; monitoring for any symptoms or changes | Stable condition; no significant progression noted |
| 4 | 42 years | Partial APAD | None | Mild neck discomfort; no significant symptoms | Conservative management; regular follow-up and monitoring | Stable; no notable changes during follow-up |
| 5 | 31 years | Partial APAD | None | Mild neck stiffness; no significant symptoms | Routine monitoring; conservative care as needed | No progression; symptoms remained stable |
| 6 | 55 years | Partial APAD | None | Occasional discomfort in neck | Managed with physical therapy; regular follow-up | Symptoms improved; condition stable |
| 7 | 28 years | Partial APAD | None | Mild symptoms; no significant impact | Monitoring; conservative care if symptoms arise | No progression; stable condition |
| 8 | 37 years | Partial APAD | None | Occasional pain; no significant neurological symptoms | Physical therapy and monitoring | Condition stable; no significant changes |
| 9 | 46 years | Partial APAD | None | Mild discomfort; no significant symptoms | Regular follow-up; conservative management if symptoms develop | Stable; no major changes noted |
| 10 | 53 years | Partial APAD | None | Mild neck stiffness; no significant symptoms | Routine monitoring; conservative management | Symptoms stable; no progression observed |
| 11 | 26 years | Partial APAD | None | Minimal symptoms; no impact on daily activities | Regular follow-up; conservative care if needed | Condition stable; no notable progression |
| 12 | 29 years | Partial APAD | None | No significant symptoms | Monitoring; conservative management if symptoms arise | Stable; no significant changes during follow-up |
| 13 | 51 years | Partial APAD | None | Mild neck stiffness; no significant symptoms | Monitoring; conservative management if symptoms arise | Stable; no significant changes during follow-up |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Macrì, M.; Alhotan, A.; Festa, M.; Rendina, F.; Festa, F. The Prevalence and Clinical Implications of Atlantal Posterior Arch Defects: A CBCT Analysis of 500 Italian Patients. Appl. Sci. 2025, 15, 1877. https://doi.org/10.3390/app15041877
Macrì M, Alhotan A, Festa M, Rendina F, Festa F. The Prevalence and Clinical Implications of Atlantal Posterior Arch Defects: A CBCT Analysis of 500 Italian Patients. Applied Sciences. 2025; 15(4):1877. https://doi.org/10.3390/app15041877
Chicago/Turabian StyleMacrì, Monica, Abdulaziz Alhotan, Mario Festa, Fabiola Rendina, and Felice Festa. 2025. "The Prevalence and Clinical Implications of Atlantal Posterior Arch Defects: A CBCT Analysis of 500 Italian Patients" Applied Sciences 15, no. 4: 1877. https://doi.org/10.3390/app15041877
APA StyleMacrì, M., Alhotan, A., Festa, M., Rendina, F., & Festa, F. (2025). The Prevalence and Clinical Implications of Atlantal Posterior Arch Defects: A CBCT Analysis of 500 Italian Patients. Applied Sciences, 15(4), 1877. https://doi.org/10.3390/app15041877






