1. Introduction
Walking is a fundamental activity that is essential for daily living because the kinetic energy generated during walking facilitates body movements [
1]. However, persistent abnormal gait patterns can lead to ankle joint problems. Numerous studies on gait analysis have highlighted that prolonged gait irregularities can result in chronic musculoskeletal injuries, particularly in the lower extremities [
2,
3]. Ankle sprains, one of the most common musculoskeletal injuries, are a notable example. Recurrent ankle sprains may progress to chronic ankle instability (CAI), further increasing the risk of injuries in the lower extremities. Standard gait-training protocols often focus on modifying cadence [
4], loading [
5], foot strike patterns [
6], speed [
7], and lower-extremity alignment [
8]. Customizing these protocols to fit individual patient needs is critical for their effectiveness.
Recent advancements in technology have introduced wearable devices, treadmills with integrated force plates, real-time feedback systems, and virtual reality (VR) for gait training [
4,
5,
6,
7,
8]. In particular, wearable devices now enable the real-time monitoring of various gait parameters in practical settings. Studies using such technologies have demonstrated their effectiveness. For instance, gait training with plantar pressure biofeedback has shown measurable effects by analyzing differences in peak pressure and time to peak pressure [
5]. Kinetic research has primarily focused on vertical ground reaction forces, whereas electromyography (EMG) studies have examined the activity of key muscles, such as the tibialis anterior (TA), peroneus longus (PL), and gluteus medius (G-MED), in relation to initial contact and the 200 ms preceding it. Similar findings have been observed in controlled laboratory environments. Moreover, recent research has shown that IMU-based systems significantly enhance gait training by providing real-time feedback, which is crucial for improving balance and reducing reinjury rates in individuals with CAI [
9].
Although the mechanisms underlying gait instability are not yet fully understood, research suggests that incorporating visual feedback and advanced gait-training strategies can help identify and correct abnormal gait patterns in real time [
1,
2]. Various gait-training approaches have shown promise in assisting individuals with pathological conditions, helping to improve gait patterns following injuries. Proper gait patterns are essential for preventing recurrent injuries. Real-time data exchange technology significantly contributes to injury prevention, particularly in sports settings. Developing treatment strategies with immediate feedback capabilities is crucial to promoting rapid recovery. Such strategies could provide tailored training methods for individuals, with technologies that monitor real-time scenarios during continuous gait training playing a vital role in reducing reinjury rates.
Currently, there is limited research on gait-training techniques for individuals with CAI, particularly regarding running gait. Effective interventions for CAI include destabilization devices that induce inversion perturbations during walking [
8], plantar pressure feedback systems, and novel gait-training devices aimed at medializing foot loading. This focus is critical because individuals with CAI tend to shift their center of pressure laterally while walking [
10].
Few studies have examined gait-training techniques specifically for CAI or the learning processes involved. A significant limitation of the current strategies is the inability to adequately control movements at the talocrural and subtalar joints [
11]. Addressing technological and cost barriers could pave the way for more effective gait-training strategies for patients with CAI.
Precise gait-training strategies can be realized through continuous moment-arm tracking in real-world scenarios in which injuries occur. The growing interest in wearable devices equipped with inertial measurement unit (IMU) sensors has driven advancements in smart healthcare. This study incorporates the recent progress in sensor technology and real-time measurement systems into a wearable device, building upon previous findings to enhance injury prevention.
2. Methods
2.1. Study Design
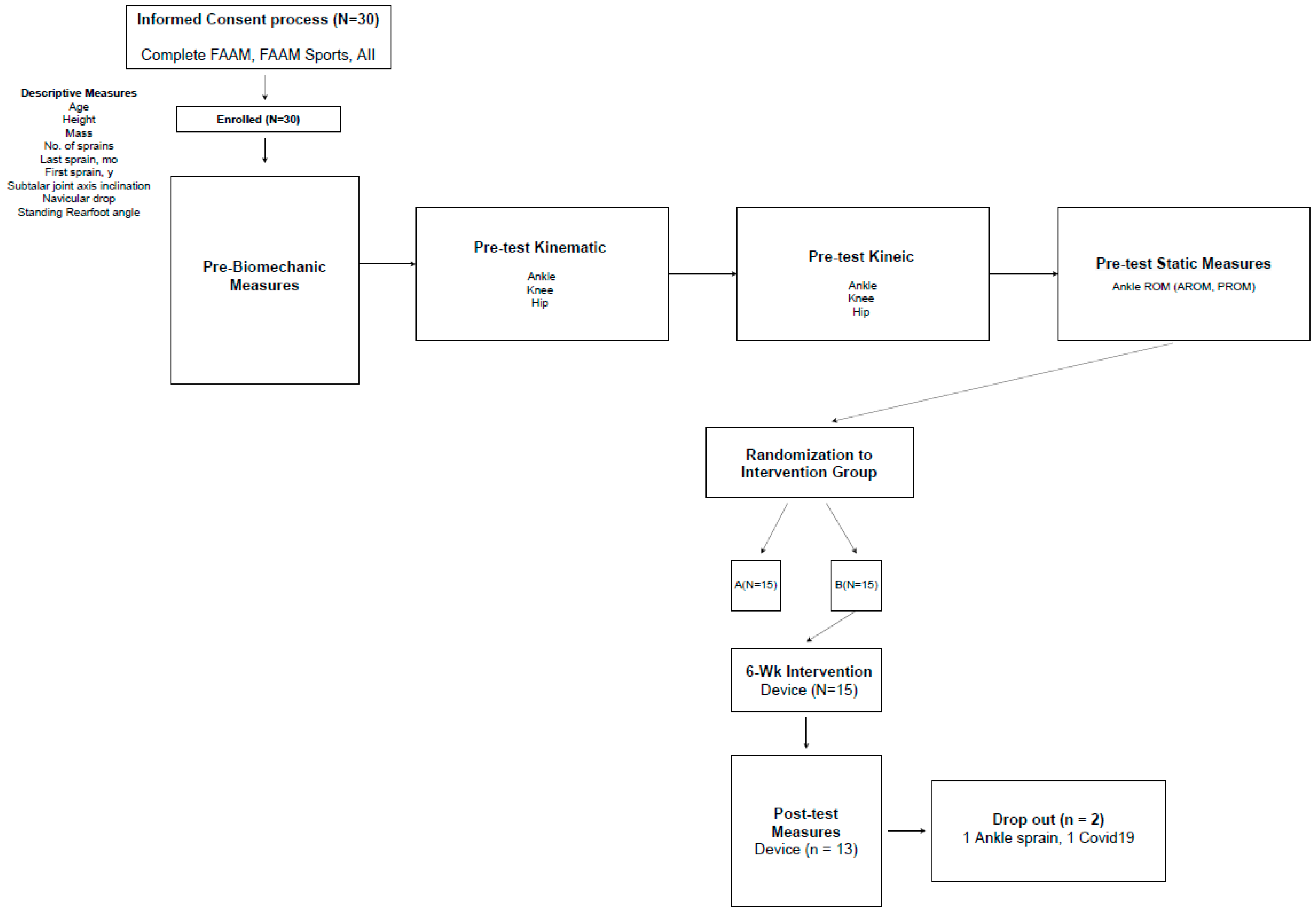
A single-blind randomized controlled trial was conducted to compare the effects of six weeks of supervised gait training (intervention group) with no training (control group) on sagittal and frontal plane ankle kinematics in adults with CAI. The intervention group participated in six weeks of gait training, incorporating both visual and auditory feedback, while the control group did not receive any form of intervention (
Table 1).
2.2. Subjects
Thirty physically active participants were voluntarily recruited for this study. The required sample size was determined through a priori power analysis using G*Power version 3.1.9.4. Based on the findings of [
10], the analysis incorporated parameters of 1 − β = 0.8, α = 0.05, and an effect size of 0.58. The results indicated that 24 participants with chronic ankle instability (CAI) were required. However, to account for an anticipated dropout rate of 20%, 30 participants were recruited. Screening was conducted using self-reported questionnaires that adhered to the standards established by the International Ankle Consortium. After enrollment, the participants were randomly assigned to one of the two CAI groups.
The inclusion criteria required the participants to have experienced at least one ankle sprain accompanied by symptoms such as swelling, pain, and temporary functional impairment. Additionally, they needed to report at least two episodes of “giving way” within the past six months, resulting in noticeable ankle instability and functional limitations in daily activities. Eligibility was further confirmed using the Ankle Instability Instrument (AII) and functional ankle instability (IdFAI) scale, with minimum required scores of 5 and 11, respectively. To assess the severity of their condition, the Foot and Ankle Ability Measure (FAAM) subscales for Activities of Daily Living (FAAM-ADL) and sports (FAAM-S) were also utilized, with higher scores indicating less severe ankle disability.
Participants were instructed to abstain from consuming stimulants, such as caffeine, to ensure the accuracy of the spinal reflex excitability measurements. Written informed consent was obtained from all participants as approved by the Institutional Review Board of Yonsei University, which reviewed and authorized the study.
2.3. Gait Analysis
Kinematic and kinetic data were acquired using an eight-camera motion capture system (VICON Motion Systems, Inc., Lake Forest, CA, USA) operating at a sampling frequency of 100 Hz, whereas ground reaction force data were recorded at 2000 Hz with a force plate (ORG-6 AMTI, Watertown, MA, USA). Three-dimensional joint kinematics were analyzed using the VICON Plug-In Gait model (Oxford Metrics, London, UK). The participants wore standardized running shoes (FTY no. CLU 60001, Adidas, Herzogenaurach, Germany) and completed walking and jogging tasks at controlled speeds of 1.34 m/s and 2.68 m/s, respectively, with timing measured by a running timer (TAKEI TKK 1274, Takei Scientific Instruments Co., Ltd., Niigata, Japan). The participants were provided with sufficient practice time to ensure consistent movement before recording three successful trials for analysis (
Table 2). "I have included the name of the manufacturer, city, and country in the revised manuscript."
For each walking and running trial, the kinematic and kinetic data were averaged across all gait cycles within the trial. The data were resampled to 100 points, representing the full gait cycle from initial contact to toe-off of the involved limb, using a custom MATLAB program. Joint angles and moments at the ankle, knee, and hip were processed using a low-pass filter with a cutoff frequency of 6 Hz to ensure smooth signal processing for both the walking and running tasks (
Figure 1).
2.4. Gait Training
The gait-training program was designed to challenge the feedback group’s ability to modify their gait patterns while walking and running. Each participant wore a wearable device with one sensor mounted on top of their right foot using a custom-designed shoe holder and another sensor securely attached to their right shin with a specially designed holder.
Figure 2 illustrates the developmental and implementation process of the gait-training intervention. Steps (1)–(4) summarize the preliminary validation of commercially available inertial sensors, as previously established in Reference [
11]. These steps involved matching IMU data with a 3D motion analysis system (VICON) to confirm the validity of the sensors before integrating them into the gait-training device. Steps (5)–(6) detail the core aspects of this study, focusing on the application of the validated IMU system for biofeedback gait training in individuals with chronic ankle instability (CAI). The validated system was used to develop a customized training device that provided real-time auditory and visual feedback to promote gait modifications.
Figure 2 visually represents the transition from sensor validation to the application of concurrent feedback-based training. The progressive gait-training program spanned six weeks, with participants completing two 20 min sessions per week. Each session focused on targeting a specific ankle angle, during which the participants walked on a treadmill while receiving continuous auditory and visual feedback provided by a Python-based program. Pre- and post-training assessments were conducted using a VICON 3D motion capture system and force plates to evaluate walking and running kinematics.
Over six weeks, the participants attended a total of 12 sessions, each targeting different ankle angles. Feedback was consistently delivered to the feedback group through both auditory and visual cues to ensure a standardized experience. Each session was conducted under controlled conditions by using a Python-based program. Following the completion of the program, the participants underwent additional 3D motion capture and force plate assessments to analyze their walking and running mechanics, as outlined in previous studies [
12].
2.5. Statistical Analysis
A paired t-test was used to assess the differences in gait between the pre- and post-test conditions. Eight dependent variables were analyzed for walking and running: active and passive ranges of motion for ankle inversion, eversion, plantar flexion, and dorsiflexion. Mean values and 95% confidence intervals (CIs) were calculated for each variable throughout the gait cycle. Non-overlapping periods between the CI bands for the pre- and post-test measures, as well as across the three groups, were identified.
Statistical significance was set at p < 0.05. Data analysis was performed using SPSS software (version 25.0; SPSS, Chicago, IL, USA).
3. Results
3.1. Self-Reported Functional Status
Table 3 presents the mean and standard deviation values of the FAAM-ADL and FAAM-sport measures. Significant improvements were observed in post-intervention compared with pre-test scores for both the FAAM-ADL (
p = 0.002) and FAAM-Sport (
p = 0.000). For the FAAM-ADL, the scores significantly increased from 88.66 ± 5.47 (pre-training) to 92.60 ± 4.45 (post-training). Likewise, the FAAM-Sport scores demonstrated a notable improvement, rising from 80.79 ± 8.20 (pre-training) to 85.67 ± 6.41 (post-training) (
Figure 3).
3.2. Ankle Range of Motion
Table 4 presents a comparison of the active and passive ranges of motion (AROM and PROM) between the pre- and post-intervention conditions. Eight variables were analyzed, including AROM (inversion, eversion, plantar flexion, and dorsiflexion) and PROM (inversion, eversion, plantar flexion, and dorsiflexion). Among these, a significant change was observed only in the PROM eversion (
p = 0.000). This significant improvement in passive eversion highlights the effectiveness of the gait-training device. Furthermore, these findings are consistent with those reported in a previous study [
10].
3.3. Pre- and Post-Internvention Joint Angle During Walking
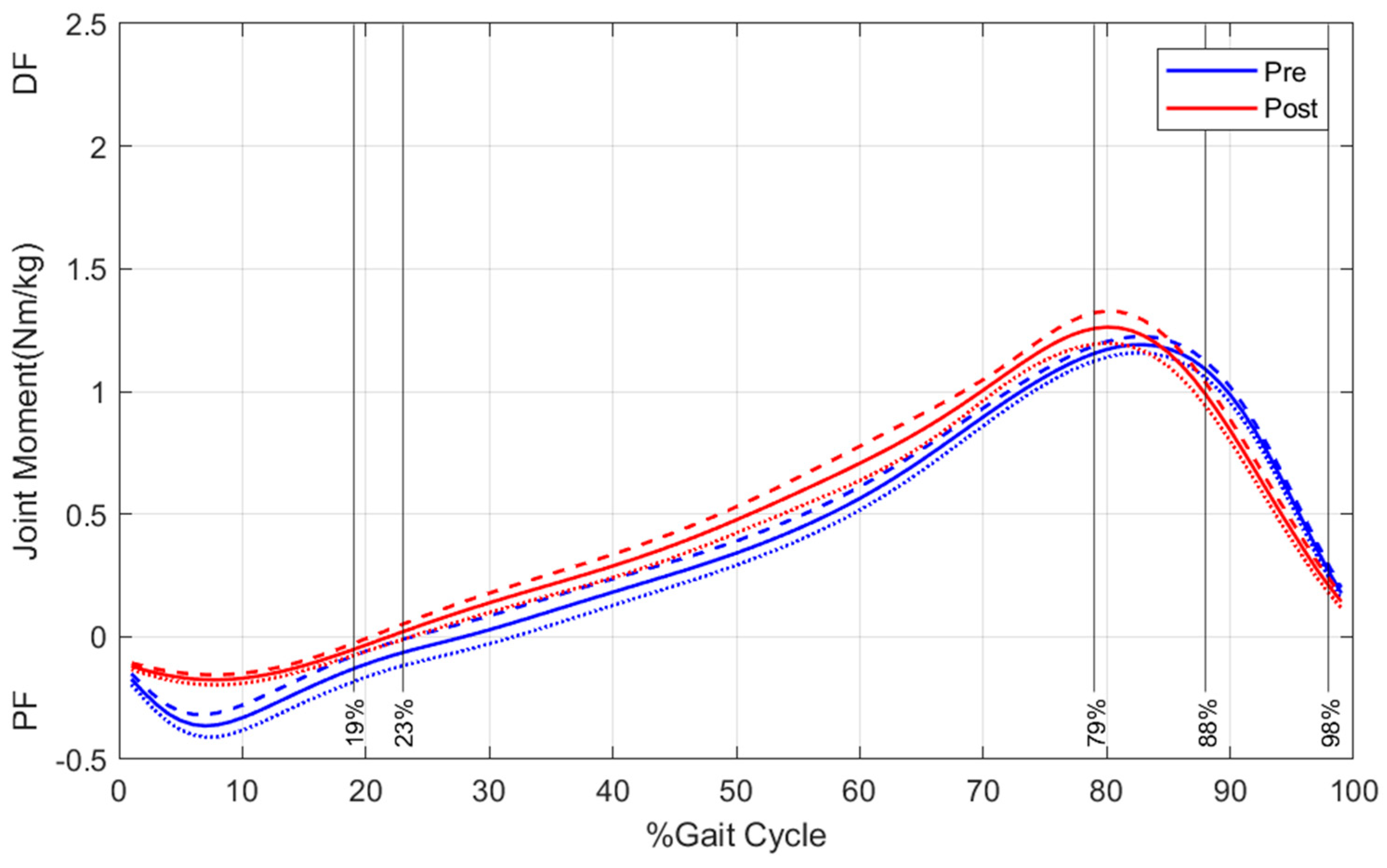
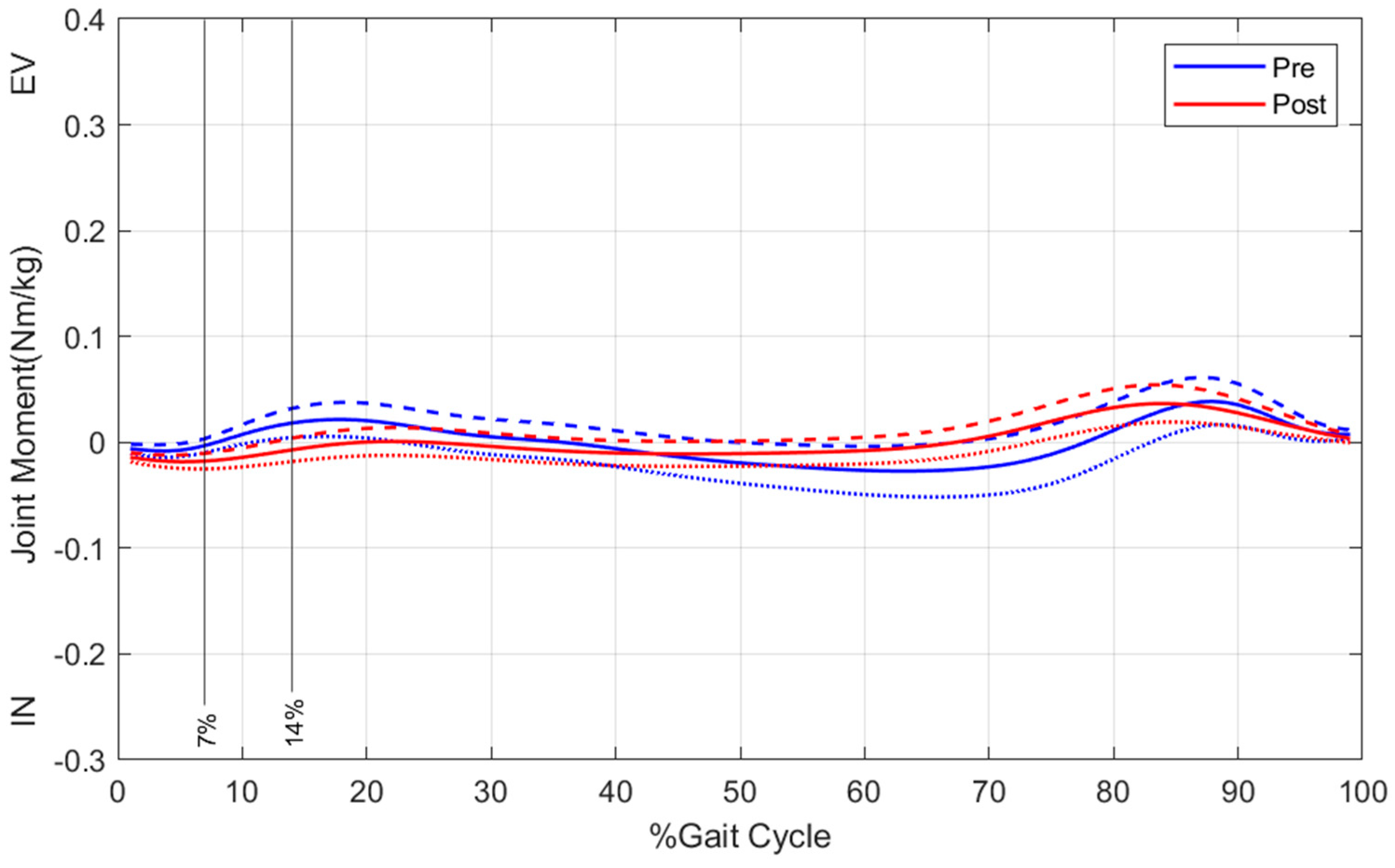
Figure 4,
Figure 5 and
Figure 6 depict ankle kinetics during walking, comparing the pre- and post-test conditions. Toe-off occurred at 100% of the gait cycle in all the subjects. Significant changes were observed in the ankle kinetics for plantarflexion/dorsiflexion, inversion/eversion, and adduction/abduction.
Post-intervention, increased dorsiflexion in the sagittal plane was observed during specific phases of the gait cycle: 0–19%, 23–79%, and 88–98%. In the frontal plane, the ankle exhibits a greater everted angle between 7% and 14% of the gait cycle. In addition, in the transverse plane, the ankle showed increased adduction from 0% to 5%, 13% to 29%, and 82% to 99% of the gait cycle.
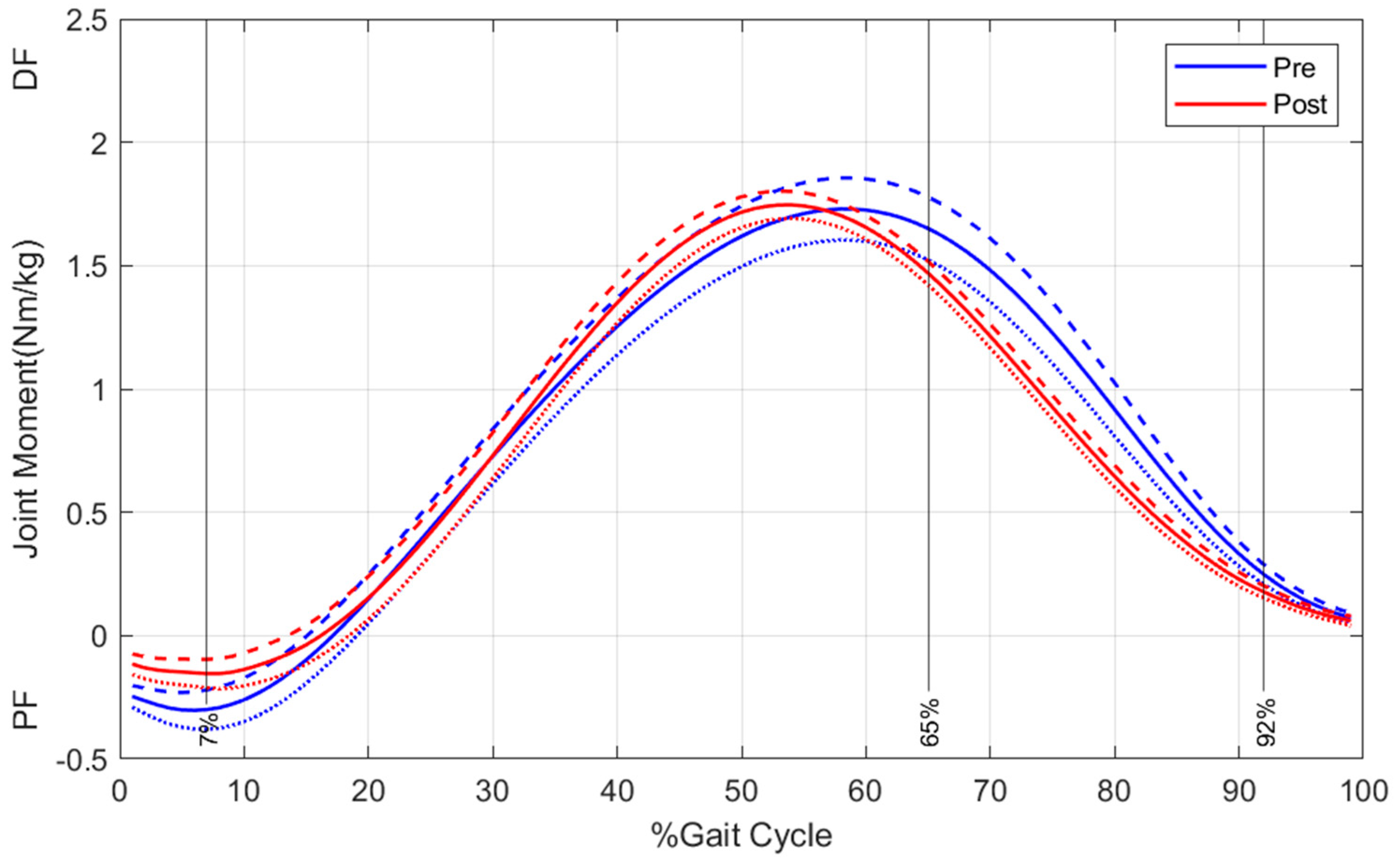
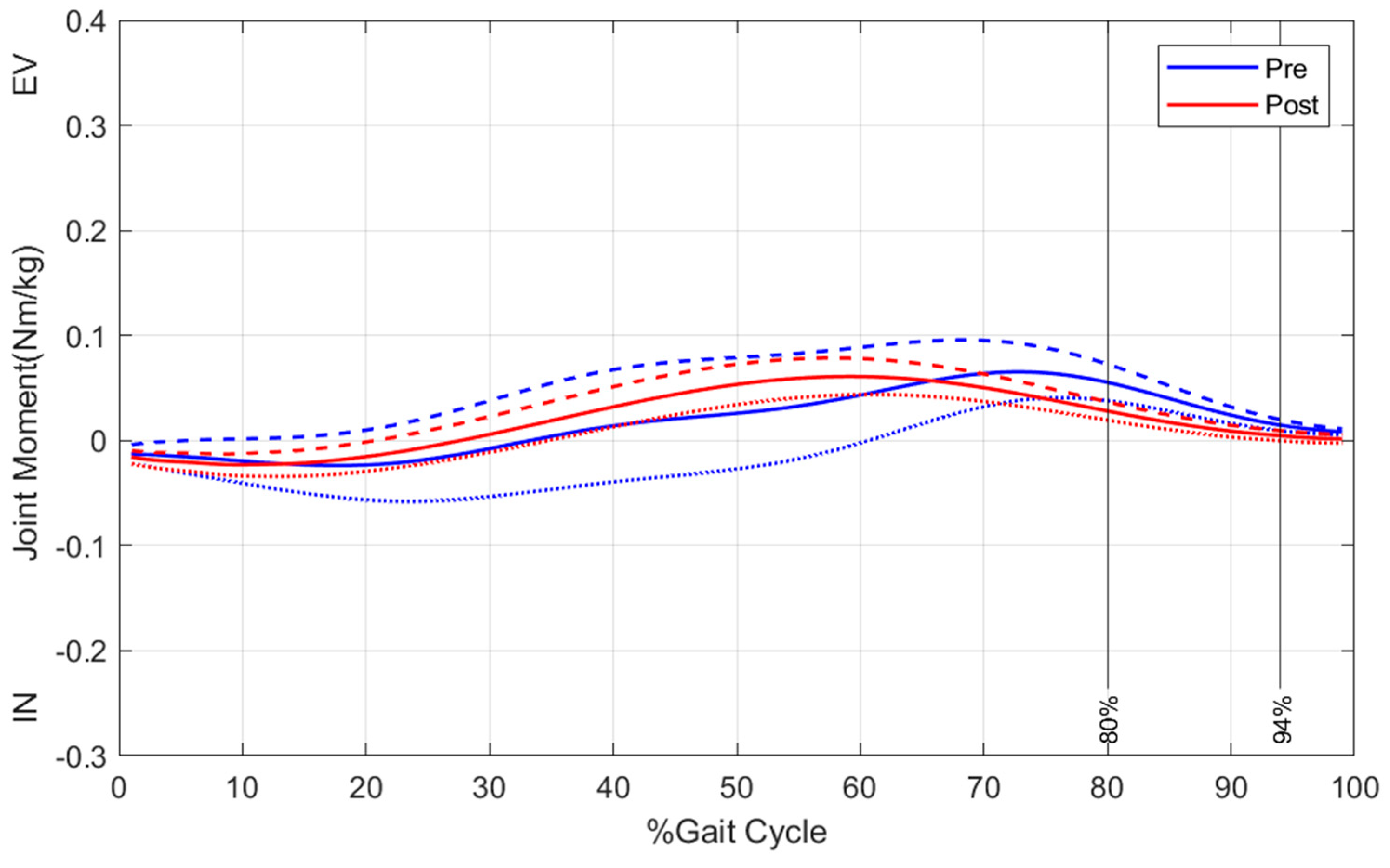
3.4. Pre- and Post-Intervention Joint Moment During Running
Figure 7,
Figure 8 and
Figure 9 depict ankle kinetics during running, comparing the pre- and post-test conditions. Across all the subjects, the average toe-off occurred at 100% of the gait cycle.
Significant changes were observed in the ankle kinetics for plantarflexion/dorsiflexion, inversion/eversion, and adduction/abduction. Post-intervention dorsiflexion in the sagittal plane was evident in 0–7% and 65–92% of the gait cycles. In the frontal plane, the ankle demonstrates greater eversion angles between 80% and 94% of the gait cycle. In addition, in the transverse plane, the ankle exhibited increased adduction during the 0–3%, 45–55%, 69–93%, and 97–99% gait cycles.
4. Discussion
This study aimed to assess the effects of a 6-week gait-training intervention on self-reported ankle function and changes in joint angles and moments during walking and running in individuals with chronic ankle instability (CAI). This program was specifically designed to improve the ankle mechanics in the frontal and sagittal planes throughout the gait cycle, offering potential benefits to individuals with CAI. These findings have significant relevance for sports medicine professionals and researchers and provide valuable insights into the analysis and rehabilitation of patients with CAI.
The primary objective of this study was to investigate the dynamic biomechanical characteristics of the gait. The results supported the study’s hypotheses, showing measurable changes in ankle kinematic and kinetic variables after the gait-training interventions.
4.1. Self-Reported Function
Self-reported outcomes from participants with CAI revealed improved ankle function after the 6-week gait-training program. The FAAM-ADL and FAAM-Sport scales showed increases of 3.94% and 4.88%, respectively, from the pre- to post-intervention values. These results highlight the importance of rehabilitating individuals with CAI by encouraging healthier and more normalized gait patterns. However, while the improvements observed were aligned with those of previous research [
13,
14], the increase in the FAAM-Sport scale score was lower than the 10.6% reported in other studies. This difference may stem from variations in training volume and frequency and the exclusion of functional exercises in this study, which focused solely on walking. Future training protocols that incorporate higher exercise volume, intensity, and functional activities may produce greater improvements in self-reported function.
4.2. Kinematic and Kinetic
In terms of kinematics, the results demonstrated increased dorsiflexion and eversion during walking and running after 6-week gait training. Dorsiflexion improvements were particularly evident during the early to mid-late stance and late swing phases of the gait cycle. Walking and running exhibited comparable enhancements, occurring during similar phases of the gait cycle.
Human gait transitions from dorsiflexion to plantar flexion during preparation for the swing phase. Previous studies have identified dorsiflexion deficits in individuals with CAI during the early to mid-late stance phase compared with healthy individuals [
15]. Reduced dorsiflexion angles have also been reported during the late stance phase of walking and running in patients [
16]. Limited dorsiflexion is often linked to mechanical deficits arising from ankle injuries such as arthrokinematic restrictions. These restrictions cause anterior, internal, and superior displacement of the talus relative to the tibia [
17,
18], leading to reduced dorsiflexion during gait [
16,
19,
20]. Furthermore, patients with CAI frequently exhibit greater inversion angles throughout the gait cycle than healthy individuals. Research consistently indicates significantly increased inversion during both walking and running in individuals with CAI [
14,
16].
The findings of this study are consistent with those of previous studies. Subjects with CAI showed increased dorsiflexion, eversion, and abduction moments throughout the gait cycle during both walking and running. The observed increase in the pronated moment trend likely supports shock absorption during walking. Improvements were evident in the patient-reported outcomes, joint angles, and moments. Significant increases in dorsiflexion and eversion moments, along with the corresponding confidence intervals, were observed. These enhancements in ankle strength following the intervention are consistent with prior research reporting significant gains in ankle eversion strength [
13,
21].
Additionally, this study identified a significant improvement in the passive eversion range of motion among patients with CAI, potentially contributing to the observed increase in eversion strength. These findings suggest that improved ankle joint stability in individuals with CAI may result from achieving a “close-packed position” due to reduced plantar flexion and inversion [
22].
4.3. Gait Training for CAI
Gait-training techniques specifically tailored to patients with chronic ankle instability (CAI) remain underexplored in the current literature. While numerous studies have addressed treatments for chronic pathological conditions, many rely on similar techniques and feedback methods, with limited emphasis on dynamic motions. As discussed previously, repeated ankle sprains often result in abnormal gait patterns. A notable prior study developed a destabilization device to induce inversion perturbations during walking [
8]. This approach demonstrated an increased activation of the peroneus muscles, highlighting the clinical utility of such devices. However, its utility may be constrained by the focus on motor control strategies [
23,
24] that are associated with abnormal neuromechanics in patients with CAI.
Abnormal movements in patients with CAI often involve supraspinal motor control functioning as a feed-forward mechanism [
23,
24,
25], potentially resulting in unstable movement patterns within the supraspinal sensorimotor pathways [
1,
23,
24,
26]. Effective gait-training strategies should ideally integrate both internal and external feedback [
27], with concurrent feedback being recognized as particularly effective [
28]. Previous studies have recommended exploring multimodal feedback approaches, including auditory and visual cues. However, auditory feedback is not always readily accessible to researchers [
29].
This study adopted a concurrent feedback strategy incorporating both auditory and visual feedback to optimize gait training for patients with CAI and reduce the risk of recurrent ankle sprains. The devices used in this study were designed specifically to provide concurrent feedback. We believe that employing targeted strategies in combination with gait-training devices can effectively enhance dorsiflexion and eversion, thereby offering substantial benefits to individuals with CAI.
5. Conclusions
This study evaluated the effectiveness of a gait-training device that incorporates IMU sensors in individuals with chronic ankle instability (CAI). After the intervention, the CAI group demonstrated significant improvements in kinematic and kinetic variables, self-reported ankle function, and passive eversion range of motion. These findings suggest that the newly developed IMU-based system is a practical and effective tool for gait training in patients with CAI. The use of a concurrent feedback device during gait training may provide additional benefits in addressing gait abnormalities and improving the deficits commonly associated with CAI. Further studies should explore the long-term retention of gait improvements, investigate different feedback modalities (e.g., haptic feedback), and compare the effectiveness of IMU-based training to other rehabilitation techniques.