DBSCAN Clustering and Entropy Optimization for Geospatial Analysis of Urban–Rural Healthcare Inequities in Latin America
Abstract
1. Introduction
1.1. Research Background
Existing Problems and Conventional Approaches
1.2. Literature Review and Related Studies
1.3. Our Contributions
2. Materials and Methods
2.1. Study Design
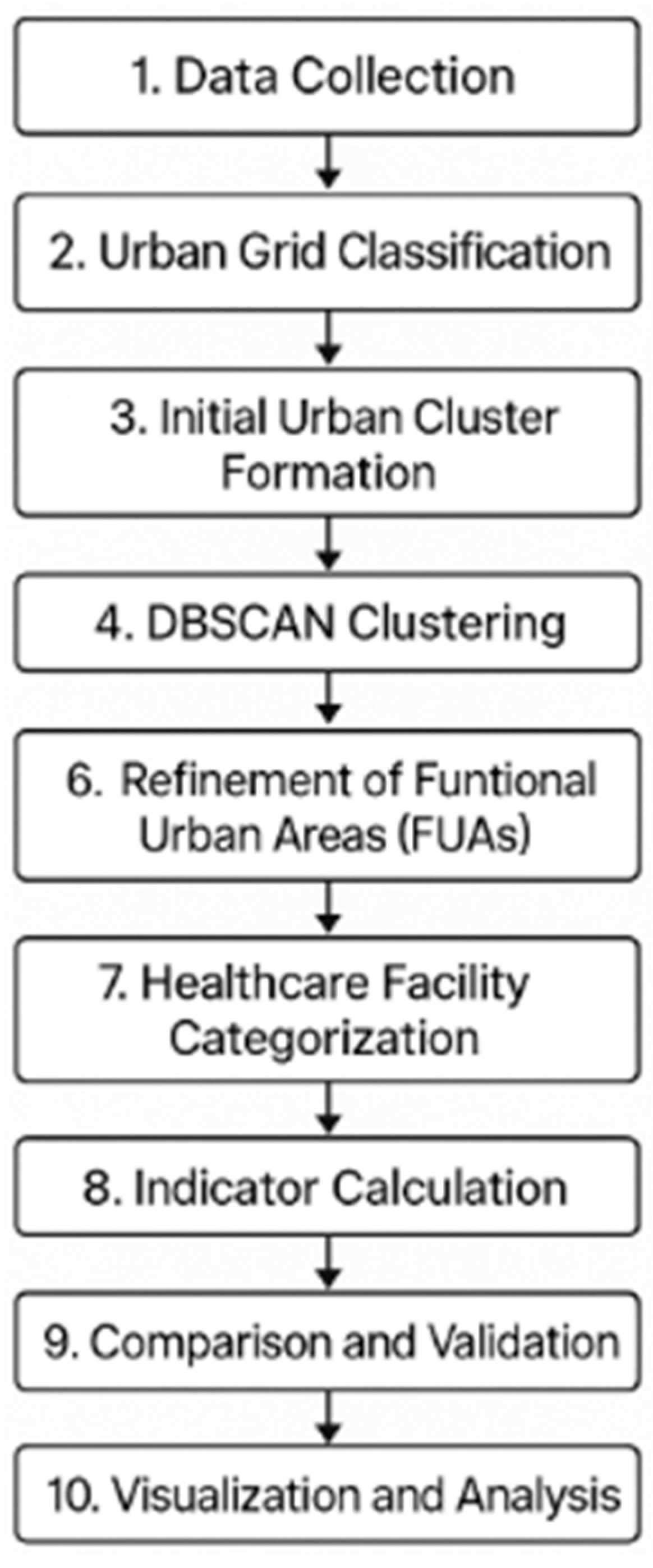
- Data Collection: Gather high-resolution population density raster datasets (HRSL and GPWv4) and administrative boundary shapefiles for each country and obtain geolocated healthcare facility data from open sources (Healthsites.io).
- Urban Grid Classification: Process population raster data in R and classify each grid cell as “urban” or “rural” based on country-specific population density thresholds. Cells above the threshold are labeled urban, and those below are rural.
- Initial Urban Cluster Formation: Group contiguous high-density (urban) grid cells to form preliminary urban clusters. Align these clusters with second-level administrative units (ADM2, e.g., municipios, cantones, or comunas) to identify potential Functional Urban Areas.
- DBSCAN Clustering: Apply DBSCAN to the spatial coordinates of high-density grid cell centroids. MinPts was set to 5 based on the foundational DBSCAN methodology (requiring each core point to have at least four neighbors). We iteratively test different epsilon (ε) distance values (ranging from 10 m to 1000 m in 10 m increments) for clustering.
- Entropy Optimization: For each candidate ε, compute Shannon’s entropy of the resulting cluster size distribution (based on population in each cluster). Identify the ε value that maximizes the entropy, which indicates the most representative clustering (balancing between one single cluster and many overly fragmented clusters). This optimal ε is selected as the clustering parameter for that country.
- Refinement of FUAs: Using the optimal ε, perform DBSCAN clustering to define final urban clusters. Discard trivial clusters that do not meet a minimum population size (small clusters below country-specific population thresholds, e.g., 25,000 people, are filtered out to avoid over-fragmentation). Assign municipalities with ≥50% of their population in urban clusters as FUAs; those below 50% are non-FUA (predominantly rural) regions.
- Healthcare Facility Categorization: Join each healthcare facility point to the corresponding municipality and label it as “urban” (if within an FUA) or “rural” (if in a non-FUA area). Categorize facilities by type (hospital, clinic/primary, other).
- Indicator Calculation: Calculate per-capita healthcare facility densities for urban vs. rural populations in each country. Compute ratios of FUA to non-FUA facility density for each facility category (total facilities, hospitals, primary care, specialized).
- Comparison and Validation: Compare the clustering-based delineation of urban areas to traditional definitions. We qualitatively assess if our identified FUAs align with known metropolitan regions and check population sums against official totals (validating that population estimation error is within acceptable bounds). No formal ground-truth for cluster boundaries is available, but results are reviewed for face validity.
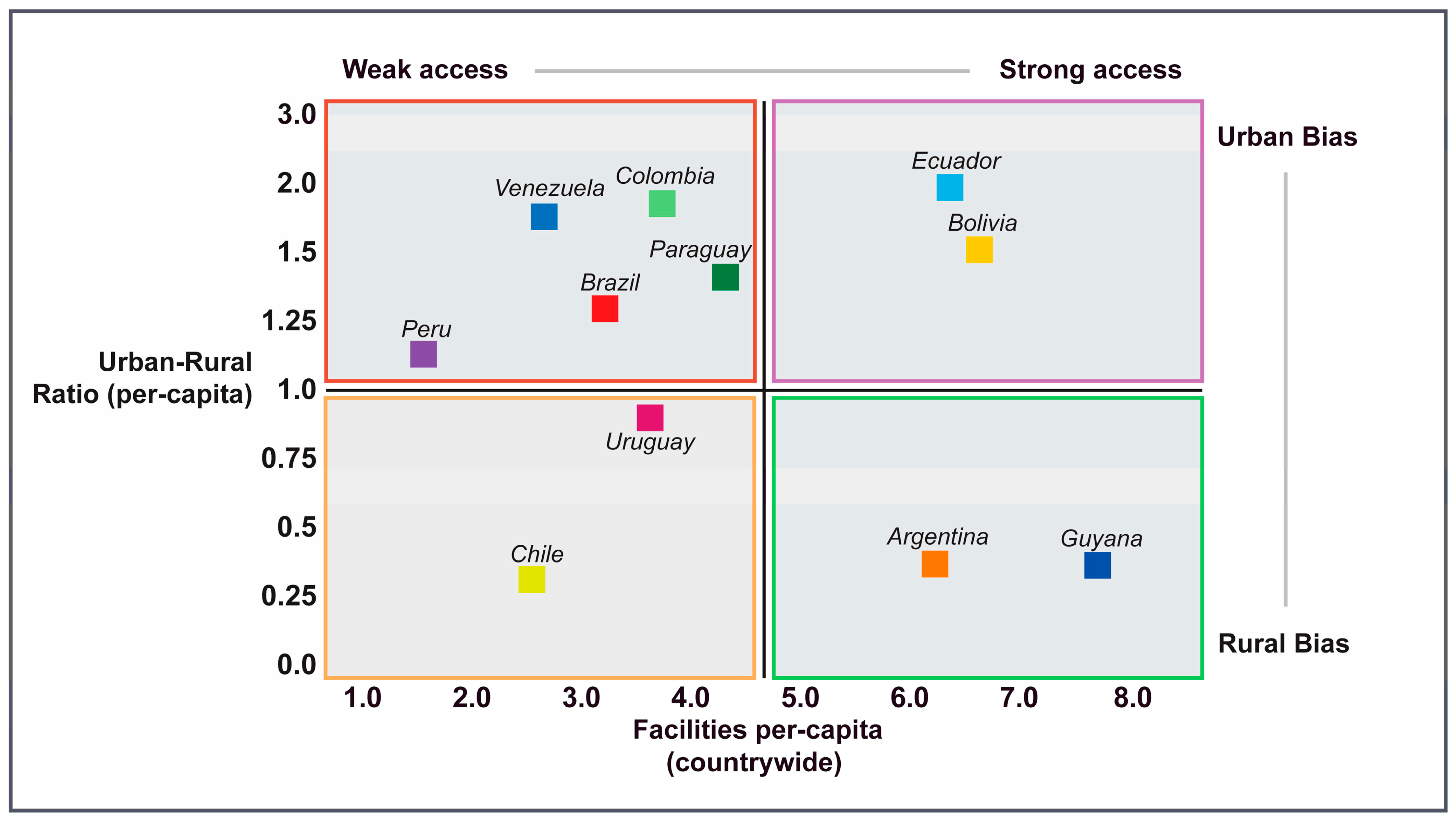
- Visualization and Analysis: Generate choropleth maps and scatter plots to visualize the distribution of FUAs and healthcare facilities. Interpret patterns of urban bias or rural shortfall in healthcare resources for each country and perform cross-country comparisons.
2.2. Country Selection
2.3. Urban Grid Classification and Clustering Procedure
2.3.1. Density-Based Spatial Clustering of Applications with Noise (DBSCAN)
2.3.2. Entropy Optimization
2.3.3. Identification of Functional Urban Areas
2.4. Healthcare Facility Data and Analysis
2.5. Data Synthesis and Visualization
3. Results
3.1. Population Distribution and Functional Urban Area Delineation
3.2. Overall Healthcare Infrastructure Distribution Patterns
3.3. Hospital Distribution Patterns
3.4. Primary Healthcare Distribution
3.5. Specialized Services Distribution
4. Discussion
4.1. Urban-Dominated Healthcare Systems: Centralization and Accessibility Trade-Offs
4.2. Rural-Oriented Systems: Decentralized Healthcare Frameworks
4.3. Limitations
4.4. Future Work
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FUA | Functional Urban Area |
| LMIC | Low- and Middle-Income Country |
| DBSCAN | Density-Based Spatial Clustering of Applications with Noise |
| OECD | Organization for Economic Cooperation and Development |
| OSM | OpenStreetMap |
| HOTOSM | Humanitarian OpenStreetMap Team |
| CIESIN | Center for International Earth Science Information Network |
| OCHA | United Nations Office for the Coordination of Humanitarian Affairs |
| UTM | Universal Transverse Mercator |
Appendix A
| >2 M | 1 M–2 M | 0.5 M–1 M | 0.2 M–0.5 M | 0.1 M–0.2 M | 0.05 M–0.1 M | 0.025 M–0.05 M | FUA Population | Non-FUA Population | Total Population | |
|---|---|---|---|---|---|---|---|---|---|---|
| Argentina | 3,239,564 | 3,434,659 | 12,626,422 | 13,231,903 | 2,455,137 | 0 | 0 | 34,987,685 | 10,668,294 | 45,655,978 |
| Bolivia | 4,656,016 | 0 | 1,371,175 | 2,347,069 | 286,892 | 73,655.41 | 126,921.92 | 8,861,729 | 3,026,652 | 20,750,110 |
| Brazil | 34,042,787 | 15,845,364 | 21,651,828 | 36,170,359 | 23,945,827 | 0 | 0 | 131,656,165 | 97,424,832 | 229,080,997 |
| Chile | 0 | 2,749,409 | 500,306 | 6,890,170 | 4,674,279 | 2,389,865 | 0 | 17,204,029 | 3,112,987 | 37,521,046 |
| Colombia | 15,253,204 | 2,469,795 | 7,037,649 | 4,844,541 | 1,580,344 | 0 | 0 | 31,185,533 | 25,190,104 | 87,561,171 |
| Ecuador | 5,417,755 | 0 | 600,676 | 3,112,451 | 710,237 | 539,201 | 0 | 10,380,321 | 7,308,720 | 28,069,362 |
| Guyana | 0 | 0 | 0 | 295,614 | 0 | 280,132 | 163,668 | 739,414 | 106,311 | 1,585,139 |
| Paraguay | 0 | 0 | 701,059 | 1,487,347 | 2,068,747 | 918,795 | 544,806 | 5,720,754 | 1,368,210 | 7,088,964 |
| Peru | 11,525,311 | 5,538,966 | 1,685,938 | 4,554,063 | 1,491,205 | 247,430 | 0 | 25,042,914 | 11,590,823 | 36,633,736 |
| Uruguay | 0 | 1,294,271 | 0 | 0 | 372,502 | 258,833 | 355,662 | 2,281,268 | 1,308,437 | 3,589,705 |
| Venezuela | 0 | 4,937,658 | 2,307,711 | 9,184,469 | 3,151,796 | 1,765,426 | 0 | 21,347,060 | 8,598,949 | 51,293,069 |
| Software/Package | Version | Reference |
|---|---|---|
| R (Core software) | 4.4.0 | [55] R Core Team (2023) |
| RStudio (IDE) | 2023.06.2 | [53] RStudio Team (2023) |
| R Packages: | ||
| - dplyr | 1.1.4 | [56] Wickham et al., dplyr (2023) |
| - sf | 1.0-14 | [57] Pebesma & Bivand, sf (2018/2023) |
| - terra | 1.7-29 | [58] Hijmans, terra (2023) |
| - ggplot2 | 3.5.2 | [59] Wickham et al., ggplot2 (2025) |
| Data Set | Version/Year | Reference(s) |
|---|---|---|
| Meta High Resolution Settlement Layer (HRSL) | v1.2 (2020 release) | [24,25,26,27,28,29,30,31,32,33,34] OCHA/FB Population Estimates |
| CIESIN Gridded Population of the World (GPWv4) | Revision 11 (2020) | [53] CIESIN (2018) GPWv4 |
| OCHA Common Operational Datasets-Boundaries | 2024 editions | [35,36,37,38,39,40,41,42,43,44] OCHA COD-AB (country-specific) |
| Healthsites.io Global Facilities Database | 2024 (data freeze) | [60] Healthsites.io (2024) |
References
- Quizhpe, E.; Teran, E.; Pulkki-Brännström, A.M.; San Sebastián, M. Social inequalities in healthcare utilization during Ecuadorian healthcare reform (2007–2017): A before-and-after cross-sectional study. BMC Public Health 2022, 22, 499. [Google Scholar] [CrossRef]
- Atun, R.; de Andrade, L.O.; Almeida, G.; Cotlear, D.; Dmytraczenko, T.; Frenz, P.; Garcia, P.; Gómez-Dantés, O.; Knaul, F.M.; Muntaner, C.; et al. Health-system reform and universal health coverage in Latin America. Lancet 2015, 385, 1230–1247. [Google Scholar] [CrossRef] [PubMed]
- Gilardino, A.; Torres, J.; Martinez, S. Healthcare access in Latin America: Challenges, progress, and the impact of COVID-19. Arch. Public Health 2022, 80, 38. [Google Scholar] [CrossRef]
- Espinola, N.; Palacios, A.; Rojas-Roque, C. Inequalities in health and healthcare access in Argentina: A systematic assessment. Int. J. Equity Health 2020, 19, 94. [Google Scholar]
- Bilal, U.; Hessel, P.; Perez-Ferrer, C.; Michael, Y.L.; Alfaro, T.; Tenorio-Mucha, J.; Friche, A.A.L.; Pina, M.F.; Vives, A.; Diez-Roux, A.V.; et al. Life expectancy and mortality in 363 cities of Latin America. Nat. Med. 2021, 27, 463–470. [Google Scholar] [CrossRef]
- Rios Quituizaca, P.; Gatica-Domínguez, G.; Nambiar, D.; Ferreira Santos, J.L.; Brück, S.; Vidaletti Ruas, L.; Barros, A.J. Territorial inequalities and public health interventions in Latin America: Insights from Ecuador. Int. J. Equity Health 2021, 20, 48. [Google Scholar] [CrossRef]
- Macharia, P.M.; Beňová, L.; Pinchoff, J.; Semaan, A.; Pembe, A.B.; Christou, A.; Hanson, C. Neonatal and perinatal mortality in the urban continuum: A geospatial analysis of household survey, satellite imagery and travel time data in Tanzania. BMJ Glob. Health 2023, 8, e011253. [Google Scholar] [CrossRef]
- Ríos-Quituizaca, P.; Gatica-Domínguez, G.; Nambiar, D.; Santos, J.L.F.; Brück, S.; Ruas, L.V.; Barros, A.J. National and subnational coverage and inequalities in reproductive, maternal, newborn, child, and sanitary health interventions in Ecuador: A comparative study between 1994 and 2012. Int. J. Equity Health 2021, 20, 48. [Google Scholar] [CrossRef]
- Palacios, A.; Espinola, N.; Rojas-Roque, C. Need and inequality in the use of healthcare services in a fragmented and decentralized health system: Evidence for Argentina. Int. J. Equity Health 2020, 19, 67. [Google Scholar] [CrossRef]
- de Andrade, L.O.M.; Filho, A.P.; Solar, O.; Rígoli, F.; de Salazar, L.M.; Serrate, P.C.-F.; Ribeiro, K.G.; Koller, T.S.; Cruz, F.N.B.; Atun, R. Social determinants of health, universal health coverage, and sustainable development: Case studies from Latin American countries. Lancet 2015, 385, 1343–1351. [Google Scholar] [CrossRef] [PubMed]
- González, C.; Triunfo, P. Horizontal inequity in the use and access to health care in Uruguay. Int. J. Equity Health 2020, 19, 127. [Google Scholar] [CrossRef] [PubMed]
- Almeida, G.; Sarti, F.M. Measuring evolution of income-related inequalities in health and healthcare utilization in selected Latin American and Caribbean countries. Pan Am. J. Public Health 2013, 33, 83–89. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development (OECD). OECD Definition of Cities and Functional Urban Areas; OECD Data: Paris, France, 2024; Available online: https://www.oecd.org/en/data/datasets/oecd-definition-of-cities-and-functional-urban-areas.html (accessed on 19 July 2025).
- Caudillo-Cos, C.A.; Montejano-Escamilla, J.A.; Tapia-McClung, R.; Ávila-Jiménez, F.G.; Barrera-Alarcón, I.G. Defining urban boundaries through DBSCAN and Shannon’s entropy: The case of the Mexican National Urban System. Cities 2024, 149, 104969. [Google Scholar] [CrossRef]
- Gabaix, X. Zipf’s law for cities: An explanation. Q. J. Econ. 1999, 114, 739–767. [Google Scholar] [CrossRef]
- Florio, P.; Freire, S.; Melchiorri, M. Estimating geographic access to healthcare facilities in sub-Saharan Africa by degree of urbanisation. Appl. Geogr. 2023, 160, 103118. [Google Scholar] [CrossRef] [PubMed]
- Agbenyo, F.; Nunbogu, A.M.; Dongzagla, A. Accessibility mapping of health facilities in rural Ghana. J. Transp. Health 2017, 6, 73–83. [Google Scholar] [CrossRef]
- Stock, R. Distance and the utilization of health facilities in rural Nigeria. Soc. Sci. Med. 1983, 17, 563–570. [Google Scholar] [CrossRef]
- United Nations. Sustainable Development Goals; United Nations Department of Economic and Social Affairs: New York, NY, USA, 2023; Available online: https://sdgs.un.org/goals (accessed on 19 July 2025).
- Ruano, A.L.; Rodríguez, D.; Gaitán-Rossi, P.; Maceira, D. Understanding inequities in health and health systems in Latin America and the Caribbean: A thematic series. Int. J. Equity Health 2021, 20, 94. [Google Scholar] [CrossRef]
- Weiss, D.J.; Nelson, A.; Vargas-Ruiz, C.A.; Gligorić, K.; Bavadekar, S.; Gabrilovich, E.; Bertozzi-Villa, A.; Rozier, J.; Gibson, H.S.; Shekel, T.; et al. Global maps of travel time to healthcare facilities. Nat. Med. 2020, 26, 1835–1838. [Google Scholar] [CrossRef]
- Moreno-Monroy, A.I.; Schiavina, M.; Veneri, P. Metropolitan areas in the world: Delineation and population trends. J. Urban Econ. 2021, 125, 103242. [Google Scholar] [CrossRef]
- Obaco, M.; Díaz-Sánchez, J.P. An overview of urbanization in Ecuador under functional urban area definition. Region 2018, 5, 38–48. [Google Scholar] [CrossRef]
- OCHA. Argentina: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/argentina-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Bolivia: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/bolivia-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Brazil: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/brazil-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Chile: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/chile-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Colombia: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/colombia-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Ecuador: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/ecuador-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Guyana: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/guyana-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Paraguay: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/paraguay-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Peru: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/peru-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Uruguay: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/uruguay-high-resolution-population-density-maps-demographic-estimates (accessed on 1 January 2024).
- OCHA. Venezuela: High Resolution Population Density Maps and Demographic Estimates. Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/worldpop-population-density-for-venezuela-bolivarian-republic-of (accessed on 1 January 2024).
- OCHA. Argentina: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-arg (accessed on 1 January 2024).
- OCHA. Bolivia: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-bol (accessed on 1 January 2024).
- OCHA. Brazil: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-bra (accessed on 1 January 2024).
- OCHA. Chile: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-chl (accessed on 1 January 2024).
- OCHA. Colombia: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-col (accessed on 1 January 2024).
- OCHA. Ecuador: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-ecu (accessed on 1 January 2024).
- OCHA. Guyana: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-guy (accessed on 1 January 2024).
- OCHA. Paraguay: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-pry (accessed on 1 January 2024).
- OCHA. Peru: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-per (accessed on 1 January 2024).
- OCHA. Uruguay: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-ury (accessed on 1 January 2024).
- OCHA. Venezuela: Common Operational Dataset—Administrative Boundaries (COD-AB). Humanitarian Data Exchange. Available online: https://data.humdata.org/dataset/cod-ab-ven (accessed on 1 January 2024).
- World Bank. The World by Income and Region. World Development Indicators. Available online: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html (accessed on 19 July 2025).
- Ester, M.; Kriegel, H.-P.; Sander, J.; Xu, X. A density-based algorithm for discovering clusters in large spatial databases with noise. In Proceedings of the 2nd International Conference on Knowledge Discovery and Data Mining (KDD’96), Portland, OR, USA, 2–4 August 1996; AAAI Press: Portland, OR, USA, 1996; pp. 226–231. [Google Scholar]
- Espinel-Flores, V.; Tiburcio-Lara, G.; Vargas, I.; Eguiguren, P.; Mogollón-Pérez, A.-S.; Ferreira-De-Medeiros-Mendes, M.; López-Vázquez, J.; Bertolotto, F.; Amarilla, D.; Vázquez, M.-L. Relational continuity of chronic patients with primary and secondary care doctors: A study of public healthcare networks of six Latin American countries. Int. J. Environ. Res. Public Health 2022, 19, 13008. [Google Scholar] [CrossRef] [PubMed]
- Khatri, R.; Endalamaw, A.; Erku, D.; Wolka, E.; Nigatu, F.; Zewdie, A.; Assefa, Y. Continuity and coordination of primary health care: A scoping review. BMC Health Serv. Res. 2023, 23, 750. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Egido, I.; Simó-Reigadas, J.; Liñán-Benítez, L.; García-Giganto, V.; Martínez-Fernández, A. Telemedicine networks of EHAS Foundation in Latin America. Front. Public Health 2014, 2, 188. [Google Scholar] [CrossRef]
- Almeida, P.F.; Santos, A.M.D.; Cabral, L.M.S.; Bousquat, A.; Fausto, M.C. Provision of specialized care in remote rural municipalities of the Brazilian semi-arid region. Rural Remote Health 2021, 21, 6652. [Google Scholar] [CrossRef]
- Mahmoud, K.; Jaramillo, C.; Barteit, S. Telemedicine in low- and middle-income countries during the COVID-19 pandemic: A scoping review. Front. Public Health 2022, 10, 914423. [Google Scholar] [CrossRef]
- RStudio Team. RStudio: Integrated Development Environment for R; Posit Software, PBC: Boston, MA, USA, 2023; Available online: https://posit.co/ (accessed on 19 July 2025).
- Ministerio de Salud Del Perú. Sistema de Salud Del Perú. Gobierno Del Perú. Available online: https://www.gob.pe/minsa (accessed on 19 July 2025).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023; Available online: https://www.R-project.org/ (accessed on 19 July 2025).
- Wickham, H.; François, R.; Henry, L.; Müller, K.; Dahan, L. dplyr: A Grammar of Data Manipulation. R Package Version 1.1.4. 2023. Available online: https://CRAN.R-project.org/package=dplyr (accessed on 19 July 2025).
- Pebesma, E.; Bivand, R. Simple Features for R (sf): Standardized Support for Spatial Vector Data. R Package Version 1.0-14. 2023. Available online: https://CRAN.R-project.org/package=sf (accessed on 19 July 2025).
- Hijmans, R.J. terra: Spatial Data Analysis. R Package Version 1.7-29. 2023. Available online: https://CRAN.R-project.org/package=terra (accessed on 19 July 2025).
- Wickham, H.; Chang, W.; Henry, L.; Pedersen, T.L.; Takahashi, K.; Wilke, C.; Woo, K.; Yutani, H.; Dunnington, D. ggplot2: Elegant Graphics for Data Analysis. R Package Version 3.5.2. 2025. Available online: https://CRAN.R-project.org/package=ggplot2 (accessed on 19 July 2025).
- Healthsites.io. Global Health Facility Data Platform. Available online: https://www.healthsites.io/ (accessed on 19 July 2025).


| Country | Healthcare Facilities (Urban:Rural) | Hospitals (Urban:Rural) | Primary Facilities (Urban:Rural) | Specialized Facilities (Urban:Rural) |
|---|---|---|---|---|
| Argentina | 0.37:1 | 0.18:1 | 0.82:1 | 0.27:1 |
| Bolivia | 1.50 *:1 | 0.33:1 | 1.36 *:1 | 0.65:1 |
| Brazil | 1.25 *:1 | 0.79:1 | 1.10 *:1 | 1.84 *:1 |
| Chile | 1.04:1 | 0.22:1 | 0.98:1 | 0.82:1 |
| Colombia | 1.75 *:1 | 0.91:1 | 2.97 *:1 | 2.40 *:1 |
| Ecuador | 1.84 *:1 | 0.82:1 | 3.56 *:1 | 2.65 *:1 |
| Guyana | 0.37:1 | 0.31:1 | 1.36 *:1 | 0.63:1 |
| Paraguay | 1.59 *:1 | 0.98:1 | 2.95 *:1 | 1.59 *:1 |
| Peru | 0.73:1 | 0.91:1 | 1.11 *:1 | 0.59:1 |
| Uruguay | 0.85:1 | 0.98:1 | 0.72:1 | 0.85:1 |
| Venezuela | 1.60 *:1 | 0.65:1 | 2.50 *:1 | 3.15 *:1 |
| Average () | 1.12 *:1 | 0.58:1 | 1.77 *:1 | 1.91 *:1 |
| Country | Calculated Population (Persons) | Official Census Population (Persons) | Percent Error (%) | Population Category | Entropy | Optimal ε (m) |
|---|---|---|---|---|---|---|
| Argentina | 45,655,978 | 45,306,215 | 0.77 | 15 M–50 M | 0.0489 | 300 |
| Bolivia | 11,888,381 | 12,311,974 | −3.44 | <15 M | 0.0076 | 340 |
| Brazil | 229,077,968 | 220,051,512 | 4.10 | >50 M | 0.0190 | 120 |
| Chile | 20,317,815 | 18,998,355 | 6.95 | 15 M–50 M | 0.0454 | 1000 |
| Colombia | 56,375,637 | 49,588,357 | 13.69 | >50 M | 0.0071 | 360 |
| Ecuador | 17,689,041 | 18,309,984 | −3.39 | 15 M–50 M | 0.2334 | 680 |
| Guyana | 845,725 | 794,099 | 6.50 | <15 M | 0.0126 | 990 |
| Paraguay | 7,088,964 | 7,522,549 | −5.76 | <15 M | 0.0060 | 470 |
| Peru | 36,633,736 | 32,600,249 | 12.37 | 15 M–50 M | 0.0048 | 330 |
| Uruguay | 3,589,705 | 3,451,805 | 4.00 | <15 M | 0.0095 | 800 |
| Venezuela | 29,946,009 | 31,250,306 | −4.17 | 15 M–50 M | 0.0434 | 370 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roach, C.S.; Shawwa, J.J.; Kis, M.A.; Nee, C.S.; Dong, G.; Stillman, K.; Brown, E.C. DBSCAN Clustering and Entropy Optimization for Geospatial Analysis of Urban–Rural Healthcare Inequities in Latin America. Appl. Sci. 2025, 15, 12278. https://doi.org/10.3390/app152212278
Roach CS, Shawwa JJ, Kis MA, Nee CS, Dong G, Stillman K, Brown EC. DBSCAN Clustering and Entropy Optimization for Geospatial Analysis of Urban–Rural Healthcare Inequities in Latin America. Applied Sciences. 2025; 15(22):12278. https://doi.org/10.3390/app152212278
Chicago/Turabian StyleRoach, Caleigh S., Jacob J. Shawwa, Matthew A. Kis, Connor S. Nee, George Dong, Kate Stillman, and Eric C. Brown. 2025. "DBSCAN Clustering and Entropy Optimization for Geospatial Analysis of Urban–Rural Healthcare Inequities in Latin America" Applied Sciences 15, no. 22: 12278. https://doi.org/10.3390/app152212278
APA StyleRoach, C. S., Shawwa, J. J., Kis, M. A., Nee, C. S., Dong, G., Stillman, K., & Brown, E. C. (2025). DBSCAN Clustering and Entropy Optimization for Geospatial Analysis of Urban–Rural Healthcare Inequities in Latin America. Applied Sciences, 15(22), 12278. https://doi.org/10.3390/app152212278






