Predictive Factors of Inpatient Rehabilitation Stay After Elective Hip and Knee Replacement: A Scoping Review
Abstract
1. Introduction
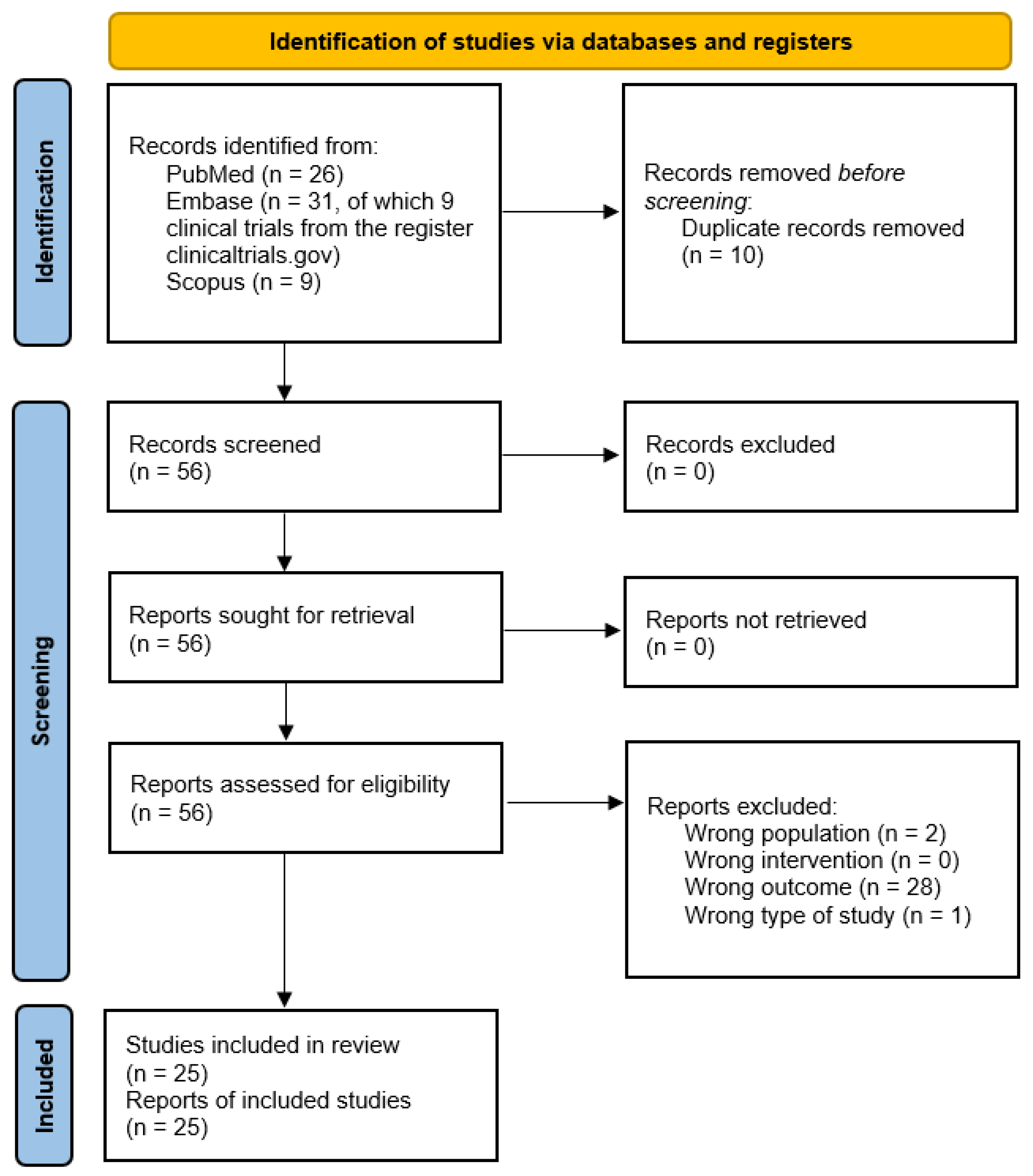
2. Materials and Methods
3. Results
3.1. Predictive Factors of Inpatient Rehabilitation Stay
3.2. Data Collection and Linking
4. Discussion
5. Conclusions
- Using comprehensive models supported by electronic health records and powerful information technologies;
- Analyzing specific inpatient rehabilitation LOS as distinguished from surgical ward rehabilitation;
- Using institutional registries, and including specific rehabilitation factors in these registries;
- Promoting vocabulary standardization (including inpatient rehabilitation LOS across different countries) and federated data sharing;The above can strongly enhance the predictivity of models investigating rehabilitation outcomes and support earlier discharge from acute wards when appropriate.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADL | Activities of Daily Living |
| ASA | American Society of Anesthesiologists |
| BI | Barthel Index |
| BMI | Body Mass Index |
| CCI | Charlson Comorbidity Index |
| CROMs | Clinician-Reported Outcome Measures |
| EQ-5D | EuroQol-5 Dimensions |
| FIM | Functional Independence Measure |
| GDS | Geriatric Depression Scale |
| HHS | Harris Hip Score |
| HOOS-JR | Hip dysfunction and Osteoarthritis Outcome Score–Joint Replacement |
| IKSS | International Knee Society Score |
| IPAQ | International Physical Activity Questionnaire |
| KOOS-JR | Knee dysfunction and Osteoarthritis Outcome Score–Joint Replacement |
| KSS | Knee Society Score |
| LEAS | Lower Extremity Activity Scale |
| LOS | Length Of Stay |
| MMSE | Mini-Mental State Examination |
| MOSS-SS | Medical Outcomes Study Social Support Scale |
| NICE | National Institute for health and Care Excellence |
References
- Nham, F.H.; Patel, I.; Zalikha, A.K.; El-Othmani, M.M. Epidemiology of primary and revision total knee arthroplasty: Analysis of demographics, comorbidities and outcomes from the national inpatient sample. Arthroplasty 2023, 5, 18. [Google Scholar] [CrossRef]
- Patel, I.; Nham, F.; Zalikha, A.K.; El-Othmani, M.M. Epidemiology of total hip arthroplasty: Demographics, comorbidities and outcomes. Arthroplasty 2023, 5, 2. [Google Scholar] [CrossRef]
- Simões, J.L.; Soares, S.; Sa-Couto, P.; Lopes, C.; Magina, D.; Melo, E.; Voegeli, D.; Bolhão, I. The Influence of Presurgical Factors on the Rehabilitation Outcome of Patients Following Hip Arthroplasty. Rehabil. Nurs. 2019, 44, 189–202. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020–2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.J.; Kaplan, R.J. Multivariate analysis of the factors affecting duration of acute inpatient rehabilitation after hip and knee arthroplasty. Am. J. Phys. Med. Rehabil. 2004, 83, 344–352. [Google Scholar] [CrossRef]
- Centers for Disease Control and prevention. Public Health and Aging: Projected Prevalence of Self-Reported Arthritis or Chronic Joint Symptoms Among Persons Aged >65 Years --- United States, 2005—2030; Atlanta: Morbidity and Mortality Week Report; CDC: Washington, DC, USA, 2003. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5221a1.htm (accessed on 7 October 2025).
- Weingarten, S.; Riedinger, M.; Conner, L.; Siebens, H.; Varis, G.; Alter, A.; Ellrodt, A.G. Hip replacement and hip hemiarthroplasty surgery: Potential opportunities to shorten lengths of hospital stay. Am. J. Med. 1994, 97, 208–213. [Google Scholar] [CrossRef]
- Kehlet, H. Fast-track hip and knee arthroplasty. Lancet 2013, 381, 1600–1602. [Google Scholar] [CrossRef]
- Riga, M.; Altsitzioglou, P.; Saranteas, T.; Mavrogenis, A.F. Enhanced recovery after surgery (ERAS) protocols for total joint replacement surgery. SICOT J. 2023, 9, E1. [Google Scholar] [CrossRef] [PubMed]
- Dawson-Bowling, S.J.; Jha, S.; Chettiar, K.K.; East, D.J.; Gould, G.C.; Apthorp, H.D. A multidisciplinary enhanced recovery programme allows discharge within two days of total hip replacement; three- to five-year results of 100 patients. Hip Int. 2014, 24, 167–174. [Google Scholar] [CrossRef]
- Jensen, C.B.; Troelsen, A.; Foss, N.B.; Nielsen, C.S.; Lindberg-Larsen, M.; Gromov, K. 10-year evolution of day-case hip and knee arthroplasty: A Danish nationwide register study of 166,833 procedures from 2010 to 2020. Acta Orthop. 2023, 94, 178–184. [Google Scholar] [CrossRef]
- Lan, R.H.; Samuel, L.T.; Grits, D.; Kamath, A.F. Contemporary Outpatient Arthroplasty Is Safe Compared with Inpatient Surgery: A Propensity Score-Matched Analysis of 574,375 Procedures. J. Bone Jt. Surg. Am. 2021, 103, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.; Fu, H.; Cheung, M.H.; Chan, W.K.V.; Chan, P.K.; Yan, C.H.; Chiu, K.Y. How well do elderly patients do after total knee arthroplasty in the era of fast-track surgery? Arthroplasty 2020, 22, 16. [Google Scholar] [CrossRef]
- Berg, U.; W-Dahl, A.; Rolfson, O.; Nauclér, E.; Sundberg, M.; Nilsdotter, A. Influence of fast-track programs on patient-reported outcomes in total hip and knee replacement (THR/TKR) at Swedish hospitals 2011–2015: An observational study including 51,169 THR and 8,393 TKR operations. Acta Orthop. 2020, 91, 306–312. [Google Scholar] [CrossRef]
- Vanni, F.; Foglia, E.; Pennestrì, F.; Ferrario, L.; Banfi, G. Introducing enhanced recovery after surgery in a high-volume orthopaedic hospital: A health technology assessment. BMC Health Serv. Res. 2020, 20, 773. [Google Scholar] [CrossRef]
- Sarpong, N.O.; Boddapati, V.; Herndon, C.L.; Shah, R.P.; Cooper, H.J.; Geller, J.A. Trends in Length of Stay and 30-Day Complications After Total Knee Arthroplasty: An Analysis From 2006 to 2016. J. Arthroplast. 2019, 34, 1575–1580. [Google Scholar] [CrossRef]
- Siciliani, L.; Wen, J.; Gaughan, J. Living alone and provider behaviour in public and private hospitals. J. Health Econ. 2025, 102, 103016. [Google Scholar] [CrossRef]
- Majeed, M.U.; Williams, D.T.; Pollock, R.; Amir, F.; Liam, M.; Foong, K.S.; Whitaker, C.J. Delay in discharge and its impact on unnecessary hospital bed occupancy. BMC Health Serv. Res. 2012, 12, 410. [Google Scholar] [CrossRef]
- LeBrun, D.G.; Nguyen, J.T.; Fisher, C.; Tuohy, S.; Lyman, S.; Gonzalez Della Valle, A.; Ast, M.P.; Carli, A.V. The Risk Assessment and Prediction Tool (RAPT) Score Predicts Discharge Destination, Length of Stay, and Postoperative Mobility After Total Joint Arthroplasty. J. Arthroplast. 2023, 38 (Suppl. S2), S121–S129. [Google Scholar] [CrossRef] [PubMed]
- Zalikha, A.K.; Court, T.; Nham, F.; El-Othmani, M.M.; Shah, R.P. Improved performance of machine learning models in predicting length of stay, discharge disposition, and inpatient mortality after total knee arthroplasty using patient-specific variables. Arthroplasty 2023, 5, 31. [Google Scholar] [CrossRef] [PubMed]
- Kurmis, A.P.; Ianunzio, J.R. Artificial intelligence in orthopedic surgery: Evolution, current state and future directions. Arthroplasty 2022, 4, 9. [Google Scholar] [CrossRef]
- Skov, C.D.; Lindberg-Larsen, M.; Wiil, U.K.; Varnum, C.; Schmal, H.; Jensen, C.M.; Holsgaard-Larsen, A. Impact of motivational feedback on levels of physical activity and quality of life by activity monitoring following knee arthroplasty surgery-protocol for a randomized controlled trial nested in a prospective cohort (Knee-Activity). BMC Musculoskelet. Disord. 2024, 25, 778. [Google Scholar] [CrossRef]
- Negrini, F.; de Sire, A.; Lazzarini, S.G.; Pennestrì, F.; Sorce, S.; Arienti, C.; Vitale, J.A. Reliability of activity monitors for physical activity assessment in patients with musculoskeletal disorders: A systematic review. J. Back Musculoskelet. Rehabil. 2021, 34, 915–923. [Google Scholar] [CrossRef]
- Pennestrì, F.; Banfi, G. Primary Care of the (Near) Future: Exploring the Contribution of Digitalization and Remote Care Technologies through a Case Study. Healthcare 2023, 11, 2147. [Google Scholar] [CrossRef]
- Cordani, C.; Perillo, S.; Corbetta, D.; Sarasso, E.; Agosta, F.; Filippi, M.; Mazzali, A.G.; Pennestrì, F. Developing Physiotherapy in Primary Health Care: A First Snapshot from the Italian Metropolitan City of Milan. Healthcare 2024, 12, 1628. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, H.J.F.; Botros, M.; Ramirez, G.; Thirukumaran, C.P.; Ricciardi, B.; Myers, T.G. Comparable performance of machine learning algorithms in predicting readmission and complications following total joint arthroplasty with external validation. Arthroplasty 2023, 5, 58. [Google Scholar] [CrossRef]
- Pennestrì, F.; Cabitza, F.; Picerno, N.; Banfi, G. Sharing reliable information worldwide: Healthcare strategies based on artificial intelligence need external validation. Position paper. BMC Med. Inform. Decis. Mak. 2025, 25, 56. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Khazi, Z.M.; Agarwalla, A.; Forsythe, B.; Taunton, M.J. Development of a Machine Learning Algorithm to Predict Nonroutine Discharge Following Unicompartmental Knee Arthroplasty. J. Arthroplast. 2021, 36, 1568–1576. [Google Scholar] [CrossRef]
- Seeber, G.H.; Wijnen, A.; Lazovic, D.; Bulstra, S.K.; Dietz, G.; van Lingen, C.P.; Stevens, M. Effectiveness of rehabilitation after a total hip arthroplasty: A protocol for an observational study for the comparison of usual care in the Netherlands versus Germany. BMJ Open 2017, 7, e016020. [Google Scholar] [CrossRef] [PubMed]
- Coudeyre, E.; Eschalier, B.; Descamps, S.; Claeys, A.; Boisgard, S.; Noirfalize, C.; Gerbaud, L. Transcultural validation of the Risk Assessment and Predictor Tool (RAPT) to predict discharge outcomes after total hip replacement. Ann. Phys. Rehabil. Med. 2014, 57, 169–184. [Google Scholar] [CrossRef]
- Colquhoun, H.L.; Levac, D.; O’Brien, K.K.; Straus, S.; Tricco, A.C.; Perrier, L.; Kastner, M.; Moher, D. Scoping reviews: Time for clarity in definition, methods, and reporting. J. Clin. Epidemiol. 2014, 67, 1291–1294. [Google Scholar] [CrossRef]
- Centre for Reviews and Dissemination. Systematic Reviews. In CRD’s Guidance for Undertaking Reviews in Health Care; University of York: York, UK, 2009; Available online: https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf (accessed on 7 October 2025).
- European Commission. Directive 2011/24/EU. Off. J. Eur. Union 2025. Available online: https://eur-lex.europa.eu/eli/dir/2011/24/oj/eng (accessed on 7 October 2025).
- The Swedish Knee Arthroplasty Register. Annual Report 2020; Svenska Knäprotesregistret: Lund, Sweden, 2020; Available online: https://www.myknee.se/en/ (accessed on 7 October 2025).
- Istituto Superiore di Sanità. Registro Italiano Artroprotesi. 2025. Available online: https://riap.iss.it/riap/it/ (accessed on 7 October 2025).
- American College of Surgeons. ACS National Surgical Quality Improvement Program. 2025. Available online: https://www.facs.org/quality-programs/data-and-registries/acs-nsqip/ (accessed on 7 October 2025).
- Tornese, D.; Robustelli, A.; Ricci, G.; Rancoita, P.M.V.; Maffulli, N.; Peretti, G.M. Predictors of postoperative hospital length of stay after total knee arthroplasty. Singapore Med. J. 2024, 65, 68–73. [Google Scholar] [CrossRef]
- Pennestrì, F.; Tosto, V.; Pelosi, C.; Grippa, D.; Negrini, S.; Kiekens, C.; Sarasso, E.; Banfi, G.; Cordani, C.; The PREPARE Project Group. Predictive Factors of Inpatient Rehabilitation Stay and Post-Discharge Burden of Care After Joint Replacement for Hip and Knee Osteoarthritis: A Retrospective Study on 1678 Patients. Appl. Sci. 2024, 14, 11993. [Google Scholar] [CrossRef]
- Dauty, M.; Smitt, X.; Menu, P.; Dubois, C. Which factors affect the duration of inpatient rehabilitation after total knee arthroplasty in the absence of complications? Ann. Phys. Rehabil. Med. 2009, 52, 234–245. [Google Scholar] [CrossRef]
- Skov, C.D. Motivational Feedback Following Total or Unicompartmental Knee Arthroplasty (KneeActivity). 2023. Available online: https://clinicaltrials.gov/study/NCT06005623?term=NCT06005623.&rank=1 (accessed on 7 October 2025).
- Masiero, S.; Avesani, R.; Pegoraro, S.; Frigo, A.C.; Bonaldo, L. Predictive factors for functional recovery in patients admitted to subacute care nursing home in Italy. Aging Clin. Exp. Res. 2011, 23, 74–77. [Google Scholar] [CrossRef]
- Raad, M.; Amin, R.M.; El Abiad, J.M.; Puvanesarajah, V.; Best, M.J.; Oni, J.K. Preoperative Patient Functional Status Is an Independent Predictor of Outcomes After Primary Total Hip Arthroplasty. Orthopedics 2019, 42, e326–e330. [Google Scholar] [CrossRef]
- Mont, M. Neuromuscular Electrical Stimulation (NMES) for Improving Outcomes Following Knee Arthroplasty (TKA). 2016. Available online: https://clinicaltrials.gov/study/NCT03044028?term=NCT03044028&rank=1 (accessed on 7 October 2025).
- Kirk, A.G.; Burge, A.T.; Ekegren, C.L.; Liew, S.M.; Kimmel, L.A. Physical Activity in the Acute Hospital Following Elective Lower Limb Joint Arthroplasty. N. Z. J. Physiother. 2022, 50, 42–49. [Google Scholar] [CrossRef]
- Poitras, S.; Au, K.; Wood, K.; Dervin, G.; Beaulé, P.E. Predicting hospital length of stay and short-term function after hip or knee arthroplasty: Are both performance and comorbidity measures useful? Int. Orthop. 2018, 42, 2295–2300. [Google Scholar] [CrossRef] [PubMed]
- Ciapini, G.; Cervi, V.; Dolfi, L.; Parchi, P.; Lisanti, M. In-Depth Oral Presentations and Oral Communications. J. Orthopaed Traumatol. 2013, 14 (Suppl. S1), S106. [Google Scholar]
- National Guideline Centre (UK). Evidence Review for Inpatient Hip Knee Postoperative Rehabilitation: Joint Replacement (Primary): Hip Knee Shoulder: Evidence Review; NICE Guideline, No. 157; National Institute for Health and Care Excellence (NICE): London, UK, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK561415/ (accessed on 7 October 2025).
- Maiorano, E.; Bodini, B.D.; Cavaiani, F.; Pelosi, C.; Sansone, V. Length of stay and short-term functional outcomes after total knee arthroplasty: Can we predict them? Knee 2017, 24, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Dall, G.F.; Ohly, N.E.; Ballantyne, J.A.; Brenkel, I.J. The influence of pre-operative factors on the length of in-patient stay following primary total hip replacement for osteoarthritis: A multivariate analysis of 2302 patients. J. Bone Jt. Surg. Br. 2009, 91, 434–440. [Google Scholar] [CrossRef]
- Menendez, M.E.; Schumacher, C.S.; Ring, D.; Freiberg, A.A.; Rubash, H.E.; Kwon, Y.M. Does "6-Clicks" Day 1 Postoperative Mobility Score Predict Discharge Disposition After Total Hip and Knee Arthroplasties? J. Arthroplast. 2016, 31, 1916–1920. [Google Scholar] [CrossRef] [PubMed]
- Robbins, S.M.; Rastogi, R.; McLaughlin, T.L. Predicting acute recovery of physical function following total knee joint arthroplasty. J. Arthroplast. 2014, 29, 299–303. [Google Scholar] [CrossRef]
- Bergman, L.; Guenna Holmgren, A.; Nilsson, U.; Amirpour, A.; Conte, H.; Eckerblad, J. The bumpy road to recovery: Older adults’ experiences during the first year after hip replacement surgery—A longitudinal qualitative study. BMC Geriatr. 2025, 25, 483. [Google Scholar] [CrossRef]
- Krakers, S.M.; Woudsma, S.; van Dartel, D.; Vermeer, M.; Vollenbroek-Hutten, M.M.R.; Hegeman, J.H.; On Behalf Of The Up Amp Go After A Hip Fracture Group. Rehabilitation of Frail Older Adults after Hip Fracture Surgery: Predictors for the Length of Geriatric Rehabilitation Stay at a Skilled Nursing Home. J. Clin. Med. 2024, 13, 4547. [Google Scholar] [CrossRef] [PubMed]
- Sikora-Klak, J.; Gupta, A.; Bergum, C.; Zarling, B.; Markel, D.C. The Evaluation of Comorbidities Relative to Length of Stay for Total Joint Arthroplasty Patients. J. Arthroplast. 2017, 32, 1085–1088. [Google Scholar] [CrossRef] [PubMed]
- den Hartog, Y.M.; Mathijssen, N.M.; Hannink, G.; Vehmeijer, S.B. Which patient characteristics influence length of hospital stay after primary total hip arthroplasty in a ‘fast-track’ setting? Bone Jt. J. 2015, 97, 19–23. [Google Scholar] [CrossRef]
- Kun, Y.; Pogoda, T. Orthopaedic patient outcomes following interdisciplinary inpatient rehabilitation. Int. J. Ther. Rehabil. 2013, 20, 361–366. [Google Scholar]
- Lewis, Z.H.; Hay, C.C.; Graham, J.E.; Lin, Y.L.; Karmarkar, A.M.; Ottenbacher, K.J. Social Support and Actual Versus Expected Length of Stay in Inpatient Rehabilitation Facilities. Arch. Phys. Med. Rehabil. 2016, 97, 2068–2075. [Google Scholar] [CrossRef][Green Version]
- Tal-Akabi, A.; Schmid, S.; Taeymans, J. Determinants of inpatient rehabilitation length of stay and discharge modality after hip and knee replacement surgery in Switzerland—A retrospective observational study. Swiss Med. Wkly. 2013, 143, w13832. [Google Scholar] [CrossRef]
- Takagawa, S.; Kobayashi, N.; Yukizawa, Y.; Oishi, T.; Tsuji, M.; Misumi, T.; Inaba, Y. Identifying factors predicting prolonged rehabilitation after simultaneous bilateral total knee arthroplasty: A retrospective observational study. BMC Musculoskelet. Disord. 2021, 22, 368. [Google Scholar] [CrossRef]
- Frontera, W.R.; Cordani, C.; Décary, S.; DEGroote, W.; Del Furia, M.J.; Feys, P.; Jette, A.M.; Kiekens, C.; Negrini, S.; Oral, A.; et al. Relevance and use of health policy, health systems and health services research for strengthening rehabilitation in real-life settings: Methodological considerations. Eur. J. Phys. Rehabil. Med. 2024, 60, 154–163. [Google Scholar] [CrossRef]
- Bozic, K.J.; Wagie, A.; Naessens, J.M.; Berry, D.J.; Rubash, H.E. Predictors of discharge to an inpatient extended care facility after total hip or knee arthroplasty. J. Arthroplast. 2006, 21 (Suppl. S2), 151–156. [Google Scholar] [CrossRef]
- Husted, H.; Holm, G.; Rud, K.; Bach-Dal, C.; Hansen, H.C.; Andersen, K.L.; Kehlet, H. Indlaeggelsesvarighed ved primaer total hofte- og knaealloplastik i Danmark 2001–2003 [Length of stay after primary total hip and knee arthroplasty in Denmark, 2001–2003]. Ugeskr. Laeger 2006, 168, 276–279. [Google Scholar]
- Vincent, H.K.; Alfano, A.P.; Lee, L.; Vincent, K.R. Sex and age effects on outcomes of total hip arthroplasty after inpatient rehabilitation. Arch. Phys. Med. Rehabil. 2006, 87, 461–467. [Google Scholar] [CrossRef]
- Winemaker, M.; Petruccelli, D.; Kabali, C.; de Beer, J. Not all total joint replacement patients are created equal: Preoperative factors and length of stay in hospital. Can. J. Surg. 2015, 58, 160–166. [Google Scholar] [CrossRef][Green Version]
- Oldmeadow, L.B.; McBurney, H.; Robertson, V.J. Predicting risk of extended inpatient rehabilitation after hip or knee arthroplasty. J Arthroplast. 2003, 18, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.; Reid, D.B.C.; Quinn, M.; Walsh, D.; Raducha, J.; Hubbard, L.; Froehlich, J. Modifying the RAPT Score to Reflect Discharge Destination in Current Practice. Arthroplast. Today 2020, 7, 17–21. [Google Scholar] [CrossRef]
- Sconza, C.; Respizzi, S.; Grappiolo, G.; Monticone, M. The Risk Assessment and Prediction Tool (RAPT) after Hip and Knee Replacement: A Systematic Review. Joints 2019, 7, 41–45. [Google Scholar] [CrossRef]
- Bieganowski, T.; Bloom, D.A.; Kugelman, D.N.; Davidovitch, R.I.; Schwarzkopf, R.; Rozell, J.C. Comparison of Two Previously Validated Risk Assessment and Prediction Tool Models in Extended Length of Stay Patients Following total Hip Arthroplasty. J. Arthroplast. 2024, 39, 2520–2524.e1. [Google Scholar] [CrossRef] [PubMed]
- Dibra, F.F.; Parvataneni, H.K.; Gray, C.F.; Vasilopoulos, T.; Prieto, H.A. The Risk Assessment and Prediction Tool Accurately Predicts Discharge Destination After Revision Hip and Knee Arthroplasty. J. Arthroplast. 2020, 35, 2972–2976. [Google Scholar] [CrossRef] [PubMed]
- Dibra, F.F.; Silverberg, A.J.; Vasilopoulos, T.; Gray, C.F.; Parvataneni, H.K.; Prieto, H.A. Arthroplasty Care Redesign Impacts the Predictive Accuracy of the Risk Assessment and Prediction Tool. J. Arthroplast. 2019, 34, 2549–2554. [Google Scholar] [CrossRef] [PubMed]
- Gabor, J.A.; Feng, J.E.; Schwarzkopf, R.; Slover, J.D.; Meftah, M. Machine Learning with Electronic Health Record Data Outperforms a Risk Assessment Prediction Tool in Predicting Discharge Disposition After Total Joint Arthroplasty. Orthopedics 2022, 45, e211–e215. [Google Scholar] [CrossRef]
- Edusei, E.; Grossman, K.; Payne, A.; Perez, B.; Inneh, I.; Nelson, C.L.; Slover, J. Impact of social support and pain coping ability on length of stay and discharge disposition following hip and knee arthroplasty: A prospective study. Bull. Hosp. Jt. Dis. 2017, 75, 134–139. [Google Scholar]
- University of Valencia. Multi-Variate Prediction Model of Total Knee Replacement Outcome. 2021. Available online: https://clinicaltrials.gov/study/NCT03894514?term=NCT03894514.&rank=1 (accessed on 7 October 2025).
- Keeney, T.; Kumar, A.; Erler, K.S.; Karmarkar, A.M. Making the Case for Patient-Reported Outcome Measures in Big-Data Rehabilitation Research: Implications for Optimizing Patient-Centered Care. Arch. Phys. Med. Rehabil. 2022, 103, S140–S145. [Google Scholar] [CrossRef]
- Langenberger, B. Who will stay a little longer? Predicting length of stay in hip and knee arthroplasty patients using machine learning. Intell.-Based Med. 2023, 8, 100111. [Google Scholar] [CrossRef]
- Campagner, A.; Milella, F.; Banfi, G.; Cabitza, F. Second opinion machine learning for fast-track pathway assignment in hip and knee replacement surgery: The use of patient-reported outcome measures. BMC Med. Inform. Decis. Mak. 2024, 24 (Suppl. S4), 203. [Google Scholar] [CrossRef]
- Katzman, J.L.; Cardillo, C.; Schaffler, B.C.; Schwarzkopf, R.; Rozell, J.C. Can Preoperative Patient-Reported Outcome Measures Predict Clinical Outcomes following Total Knee Arthroplasty? J. Arthroplast. 2025, online ahead of print. [Google Scholar] [CrossRef]
- Guida, S.; Vitale, J.A.; Swinnen, E.; Beckwée, D.; Bargeri, S.; Pennestrì, F.; Castellini, G.; Gianola, S. Effects of Prehabilitation with Advanced Technologies in Patients with Musculoskeletal Diseases Waiting for Surgery: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2024, 26, e52943. [Google Scholar] [CrossRef]
- De Klerk, T.C.; Dounavi, D.M.; Hamilton, D.F.; Clement, N.D.; Kaliarntas, K.T. Effects of home-based prehabilitation on pre- and postoperative outcomes following total hip and knee arthroplasty. Bone Jt. Open 2023, 4, 315–328. [Google Scholar] [CrossRef]
- van Aalst, M.J.; Oosterhof, J.; Nijhuis-van der Sanden, M.W.; Schreurs, B.W. Can the length of hospital stay after total hip arthroplasty be predicted by preoperative physical function characteristics? Am. J. Phys. Med. Rehabil. 2014, 93, 486–492. [Google Scholar] [CrossRef]
- Willis, R.; Edris, R.; Akehurst, S.; Ferraro, F.V. Do pre- and post- rehabilitation influence hospital length of stay and patient recovery following total hip replacement in the UK? A systematic scoping review and Delphi study. Int. J. Orthop. Trauma Nurs. 2025, 58, 101209. [Google Scholar] [CrossRef]
- Su, W.; Zhou, Y.; Qiu, H.; Wu, H. The effects of preoperative rehabilitation on pain and functional outcome after total knee arthroplasty: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2022, 17, 175. [Google Scholar] [CrossRef]
- Almeida, G.J.; Khoja, S.S.; Zelle, B.A. Effect of prehabilitation in older adults undergoing total joint replacement: An Overview of Systematic Reviews. Curr. Geriatr. Rep. 2020, 9, 280–287. [Google Scholar] [CrossRef]
- Garrison, S.R.; Schneider, K.E.; Singh, M.; Pogodzinski, J. Preoperative Physical Therapy Results in Shorter Length of Stay and Discharge Disposition Following Total Knee Arthroplasty: A Retrospective Study. J. Rehabil. Med. Clin. Commun. 2019, 23, 1000017. [Google Scholar] [CrossRef] [PubMed]
- Wallace, I.J.; Worthington, S.; Felson, D.T.; Jurmain, R.D.; Wren, K.T.; Maijanen, H.; Woods, R.J.; Lieberman, D.E. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc. Natl. Acad. Sci. USA 2017, 114, 9332–9336. [Google Scholar] [CrossRef]
- Bradley, B.M.; Griffiths, S.N.; Stewart, K.J.; Higgins, G.A.; Hockings, M.; Isaac, D.L. The effect of obesity and increasing age on operative time and length of stay in primary hip and knee arthroplasty. J. Arthroplast. 2014, 29, 1906–1910. [Google Scholar] [CrossRef]
- Fu, H.; Wang, C.; Afzal, I.; Kader, D.; Asopa, V.; Sochart, D. The effect of BMI and other factors on post-operative length of stay: A multivariable regression analysis of 860 patients undergoing total knee arthroplasty. Knee 2023, 42, 82–89. [Google Scholar] [CrossRef]
- Lozano, L.M.; Tió, M.; Rios, J.; Sanchez-Etayo, G.; Popescu, D.; Sastre, S.; Basora, M. Severe and morbid obesity (BMI ≥ 35 kg/m(2)) does not increase surgical time and length of hospital stay in total knee arthroplasty surgery. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 1713–1719. [Google Scholar] [CrossRef] [PubMed]
- Issa, K.; Pivec, R.; Kapadia, B.H.; Shah, T.; Harwin, S.F.; Delanois, R.E.; Mont, M.A. Does obesity affect the outcomes of primary total knee arthroplasty? J. Knee Surg. 2013, 26, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
| Identifying research question |
|
| Identifying relevant studies |
|
| Study selection |
|
| Charting the data |
|
| Collating, summarizing, reporting |
|
| Publication Identifier * | Year | Setting | Arthroplasty Procedure | Population | Intervention. | Outcome | Type of Study | Data Linkage | |
|---|---|---|---|---|---|---|---|---|---|
| Potential LOS Predictors | Actual LOS Predictors | ||||||||
| https://doi.org/10.1186/s12891-024-07878-0. (DOI) | 2024. | Denmark, two centers. | Knee replacement. | 200 (expected). | Pre-operative physical activity levels (as measured with a wireless medical accelerometer). | Not Applicable (N/A) (protocol). | Length of hospital stay. | Protocol for a Randomized Controlled Trial (RCT). | Multicentric database. |
| https://doi.org/10.3390/app142411993. (DOI) | 2024. | Italy, single-center. | Total hip and knee replacement. | 1678 | Age, sex, American Society of Anesthesiologists score (ASA), Body Mass Index (BMI), transfusion occurred, blood-borne infection, type of anesthesia, day of surgery, post-operative pain, post-operative cognitive function, living alone/presence of a caregiver/caregiver conditions, occupation, post-operative Barthel Index (BI) of autonomy in the Activities of Daily Living (ADL) at rehabilitation admission, duration of surgery, surgical ward LOS, hemoglobin at rehabilitation admission, post-operative verticalization day, anatomical region (hip or knee), post-operative autonomy in ADL, post-operative autonomy in postural transition, post-operative walking autonomy. | Age, living with a family, occupational status, post-operative BI, duration of surgery. | Length of rehabilitation unit stay. | Observational, retrospective. | Monocentric database. |
| https://doi.org/10.11622/smedj.2021142. (DOI) | 2024. | Italy, single-center. | Primary total knee replacement. | 1082 | Age, sex, comorbidities (number and type), BMI, presence of caregiver at home, BI at rehabilitation admission, Functional Independence Measure (FIM). | Age, sex, number of comorbidities, heart disease, BMI, presence of a caregiver at home. | Length of rehabilitation unit stay. | Observational, retrospective. | Monocentric database. |
| https://doi.org/10.21653/tjpr.998961. (DOI) | 2023. | Turkey, single-center. | Total knee arthroplasty. | 41 | Preoperative serum cytokine levels. | Preoperative serum cytokine levels were not predictive. | Length of rehabilitation unit stay up to five days or more. | Observational, prospective. | Monocentric database. |
| https://doi.org/10.1016/j.arth.2023.05.010. (DOI) | 2023. | United States, singe-center. | Primary unilateral knee and hip. | 17,713 | Single variables: anatomical region (hip or knee), age, sex, BMI, smoking status, payer status, ASA, type of anesthesia, operational time, estimated blood loss, preoperative Hip Osteoarthritis Outcome Score–Joint Replacement (HOOS-JR), Knee Osteoarthritis Outcome Score-Joint Replacement (KOOS-JR), Patient-Reported Outcome Measures Information System (PROMIS)–mental and physical health, Veterans Rand-12 Item Score–mental and physical health, Lower Extremity Activity Scale (LEAS), pain. Multivariate analysis: Risk Assessment and Prediction Tool (RAPT) score. | RAPT score, knee, operational time. | Length of hospital stay. | Observational, retrospective. | Monocentric database. |
| NCT06005623. (NCT) | 2023. | Denmark, two centers. | Total and unicompartmental knee arthroplasty. | 150 (expected). | Pre-operative physical activity levels (as measured with a wireless medical accelerometer). | N/A (protocol). | Length of hospital stay. | Protocol for an RCT. | Multicentric database. |
| https://doi.org/10.15619/NZJP/50.1.05. (DOI) | 2022. | Australia, single-center. | Total hip and knee replacement. | 74. | Age, sex, BMI, anatomical region (hip or knee), ASA, type of anesthesia, post-operative physical activity levels (as measured with step count, sit-to-stand transitions, time upright). | Post-operative physical activity measures (all). | Length of hospital stay. | Observational, prospective. | Monocentric database. |
| NCT03227120. (NCT) | 2020. | United States, single-center. | Total knee arthroplasty. | 60. | Prehabilitation compared to standard care. | N/A (protocol). | Length of hospital stay. | Protocol for an RCT. | Monocentric database. |
| https://doi.org/10.1186/s12891-021-04211-x. (DOI) | 2021. | Japan, single-center. | Simultaneous bilateral total knee arthroplasty. | 191. | Age, sex, BMI, living alone, Knee Society Function Score (KSFS), ASA, pre-operative hemoglobin, albumin level, Range of Motion (ROM), Kellgren-Lawrence scale. | Age, pre-operative hemoglobin. | Length of hospital stay (three weeks or more). | Observational, retrospective. | Monocentric database. |
| NCT03894514. (NCT) | 2021. | Spain, two-centers. | Total knee arthroplasty. | 243. | Pre-operative Oxford Knee Score (OKS), International Physical Activity Questionnaire (IPAQ)–short form, Euro Quality of Life 5D (EQ-5D), Geriatric Depression Scale (GSD), pain, expectations on pain and function, strength, ROM, Timed-Up-and-Go-Test (TUG), Five times sit to stand test, One leg balance test. | N/A (protocol). | Length of rehabilitation unit stay. | Protocol for an Observational, prospective. | Multicentric database. |
| https://doi.org/10.1503/cjs.003919. (DOI) | 2020. | Canada, single-center. | Unilateral primary total hip or knee arthroplasty. | 283. | Sat on the bedside on postoperative day 0 (POD0); stood by the bed or walked in place POD0; Walked in the room POD0; Walked in the hall POD0. | Walked in the hall at POD0. In turn, mobilization was predicted by other factors. | Length of hospital stay. | Observational, retrospective. | Multicentric database. |
| https://doi.org/10.3928/01477447-20190321-01. (DOI) | 2019. | United States, registry. | Primary total hip arthroplasty. | 43,179. | Age, sex, BMI, comorbidities (including chronic steroid use), preoperative hematocrit, smoking status, National Surgical Quality Improvement Program (NSQIP)-functional status, type of anesthesia, duration of surgery. | NSQIP functional status. | Length of hospital stay. | Observational, retrospective. | Professional/scientific society database. |
| https://doi.org/10.1097/rnj.0000000000000126. (DOI) | 2019. | Portugal, singe-center. | Total hip arthroplasty. | 40. | Age, sex, marital status, education level, number of household members, area of residence, comorbidities, pre-operative vital signs (heart rate, respiratory rate, blood pressure, body temperature), pain, clinical chemistry, BMI, body composition analysis, Mini-Mental State Examination (MMSE), GSD, FIM, Morse Fall Scale, Braden scale. | Weight of the lower limb not affected by osteoarthritis, general overweight, pain before surgery. | Length of hospital stay. | Observational, prospective. | Monocentric database. |
| https://doi.org/10.1007/s00264-018-3833-y. (DOI) | 2018. | Canada, single-center. | Hip or knee arthroplasty. | 108. | ASA, Charlson Comorbidity Index (CCI), TUG. | ASA, TUG. | Length of hospital stay. | Observational, prospective. | Monocentric database. |
| https://doi.org/10.1016/j.knee.2016.09.022. (DOI) | 2017. | Italy, single-center. | Unilateral total knee arthroplasty. | 353. | Age, BMI, CCI, depression, previous total hip or knee arthroplasty, pre-operative hemoglobin, BI at rehabilitation admission. | Age, BI at rehabilitation admission. | Length of rehabilitation unit stay. | Observational, retrospective. | Monocentric database. |
| https://doi.org/10.1016/j.arth.2016.02.017. (DOI) | 2016. | United States, singe-center. | Primary total hip and knee arthroplasty. | 744. | Model set score 1: age, sex, pre-existing medical conditions (quantified with the CCI); Medical set score 2: Activity Measure for Post-Acute Care 6 Clicks score (24 h after surgery), age, sex, CCI. | No-one. Model 2 was more accurate than model 1, but still characterized by poor predictive performance. | Length of hospital stay (3 days or more). | Observational, retrospective. | Monocentric database. |
| NCT03044028. (NCT) | 2016. | United States, single-center. | Unilateral total knee arthroplasty. | 66 (expected) | Use of NeuroMuscular Electrical Stimulation (NMES) device before and after surgery, use of NMES device only after surgery, no use of NMES device (traditional rehabilitation protocol). | N/A (protocol). | Length of hospital stay. | Protocol for an RCT. | Monocentric database. |
| https://doi.org/10.1016/j.rehab.2014.02.002. (DOI) | 2014. | France, 12 centers. | Total hip arthroplasty. | 134. | RAPT. | RAPT. | Place of discharge after surgical ward stay. (An RAPT score >9, combined with remote patient home, was predictive of external inpatient rehabilitation LOS). | Observational, retrospective. | Multicentric database. |
| https://doi.org/10.5301/hipint.5000100. (DOI) | 2014. | United Kingdom, single-center. | Unilateral total hip replacement. | 100. | ASA, CCI, age. | CCI, age. | Length of hospital stay. | Observational, prospective. | Monocentric database. |
| https://doi.org/10.1016/j.arth.2013.06.033. (DOI) | 2014. | Canada, single-center. | Total knee arthroplasty. | 72. | Age, BMI, comorbidity, post-operative pain, Pain Catastrophizing Scale (PCS), non-operative knee extensor isometric strength, TUG, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) -function score. | Age, comorbidity. | Length of hospital stay. | Observational, retrospective. | Monocentric database. |
| https://doi.org/10.1007/s10195-013-0264-9. (DOI) | 2013. | Italy, single-center. | Total knee replacement. | 100. | Age, sex, BMI, comorbidities, ASA, blood transfusion, postoperative analgesia protocol, physiotherapy protocol, day of surgery, surgical access. | ASA, BMI, blood transfusion, age. | Length of hospital stay. | Observational, retrospective. | Monocentric database. |
| 28583060. (PMID) | 2013. | United States, two centers. | Total hip or knee replacement. | 189. | Age, sex, race, PCS, Medical Outcomes Study Social Support Scale (MOSS-SS). | Sex, race, PCS, MOSS-SS. | Length of hospital stay. | Observational, prospective. | Multicentric database. |
| https://doi.org/10.1007/BF03337745. (DOI) | 2011. | Italy, single-center. | Total hip or knee replacement. | 214. | BI at rehabilitation admission. | BI at rehabilitation admission was not predictive. | Length of rehabilitation unit stay (30 days or more). | Observational, retrospective. | Monocentric database. |
| https://doi.org/10.1016/j.rehab.2009.01.001. (DOI) | 2009. | France, single-center (single rehabilitation center, receiving patients coming from five hospitals). | Primary total knee arthroplasty in absence of complications. | 244. | Age, sex, living alone, home help, previous leg arthroplasty, comorbidities, walking distance and autonomy before surgery, pain level, surgical ward LOS, IKSS (combining CROMs and PROMs), Lequesne Index. | Sex, living alone, home help, previous leg arthroplasty. | Length of rehabilitation unit stay. | Observational, retrospective. | Monocentric database. |
| https://doi.org/10.1302/0301-620X.91B4.21505. (DOI) | 2009. | Scotland, single-center. | Unilateral primary total hip replacement. | 2302. | Age, sex, BMI, operation day of the week, year of admission, knees, back and other musculoskeletal problems, comorbidities, ischemic heart disease, diabetes, pre-operative use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), pre-operative use of Aspirin, smoking status, pre-operative hemoglobin level, consultant code, Scottish Index of Multiple Deprivation, Harris Hip Score (HHS)-combining PROMs and CROMS, Short-Form 36 (SF-36). | Age, sex, pre-operative use of NSAIDS, surgeon performing the operation, operation day of the week, year of admission, HHS–function and activity, SF36 -general health perception. | Length of hospital stay. | Observational, retrospective. | Monocentric database. |
| Category | Analyzed | Predictive | Analyzed in Knee Procedures | Analyzed in Hip Procedures | Analyzed in Both Procedures in the Same Study |
|---|---|---|---|---|---|
| Pre-Existing Patient Characteristics. | |||||
| Age. | 13 | 7 | 5 | 4 | 4 |
| Anatomical region affected (hip or knee). | 3 | 1 | 3 | ||
| Area of residence. | 1 | 1 | |||
| Blood-borne transmissible infection. | 1 | 1 | |||
| Caregiver presence (not in a composite score). * | 5 | 3 | 4 | 1 | |
| CCI. | 2 | 1 | 1 | 1 | |
| Chronic steroid use. | 1 | 1 | |||
| Comorbidities (general presence). | 9 | 2 | 5 | 4 | |
| Comorbidities (specific: diabetes, heart disease, other musculoskeletal problems). | 4 | 1 | 1 | 3 | |
| Educational level. | 1 | 1 | |||
| Marital status. | 1 | 1 | |||
| Occupation. | 1 | 1 | 1 | ||
| Payer status. | 1 | 1 | |||
| Race. | 1 | 1 | 1 | ||
| Previous leg arthroplasty. | 1 | 1 | 1 | ||
| Scottish Index of Multiple Deprivation. | 1 | 1 | |||
| Sex. | 10 | 4 | 4 | 3 | 3 |
| Smoking status. | 3 | 2 | 1 | ||
| Use of drugs (NSAIDs, Aspirine). | 1 | 1 | 1 | ||
| Category. | Analyzed. | Predictive. | Analyzed in knee procedures. | Analyzed in hip procedures. | Analyzed in both procedures in the same study. |
| Pre-operative factors. | |||||
| ASA score. | 8 | 1 | 2 | 1 | 5 |
| BMI. | 11 | 2 | 5 | 3 | 3 |
| Clinical chemistry. ** | 6 | 1 | 3 | 3 | |
| Composite scores (e.g., RAPT). | 3 | 2 | 1 | 2 | |
| CROMs. *** | 8 | 2 | 2 | 6 | |
| Expectations on pain and function. | 1 | 1 | |||
| Hospitalization year. | 1 | 1 | 1 | ||
| Non-operated limb weight. | 1 | 1 | 1 | ||
| Pain. | 4 | 1 | 2 | 1 | 1 |
| Pain catastrophizing. | 2 | 1 | 1 | 1 | |
| Performance measures. **** | 4 | 4 | 1 | ||
| Physical activity measures. | 2 | 2 | |||
| Prehabilitation. | 2 | 1 | 1 | ||
| PROMs (pain excluded). *** | 15 | 3 | 7 | 1 | 7 |
| Vital signs. | 1 | 1 | |||
| Walking autonomy and/or distance (separated from composite scores). | 1 | 1 | |||
| Intra-operative factors. | |||||
| Blood loss amounts/transfusion(s) performed. | 3 | 1 | 1 | 2 | |
| Day of surgery in the week. | 3 | 1 | 1 | 1 | 1 |
| Duration of surgery/operational time. | 3 | 1 | 1 | 2 | |
| Surgeon. | 1 | 1 | 1 | ||
| Surgical access technique. | 1 | 1 | |||
| Type of anesthesia. | 4 | 1 | 3 | ||
| Category. | Analyzed. | Predictive. | Analyzed in knee procedures. | Analyzed in hip procedures. | Analyzed in both procedures in the same study. |
| Post-operative factors. | |||||
| Analgesia protocol. | 1 | 1 | |||
| Autonomy in ADL (multiple measures, Barthel excluded). | 1 | 1 | |||
| Autonomy in postural transitions. | 1 | 1 | |||
| Barthel Index (original or modified). | 3 | 2 | 1 | 2 | |
| Clinical chemistry. ** | 1 | 1 | |||
| Cognitive function. | 1 | 1 | |||
| Composite scores (e.g., RAPT). | 1 | 1 | |||
| CROMS. *** | 1 | 1 | |||
| Pain. | 1 | 1 | |||
| Performance measures. **** | 2 | 2 | |||
| Physical activity measures. | 1 | 1 | 1 | ||
| Physiotherapy protocol. | 1 | 1 | |||
| PROMs (pain excluded). *** | 2 | 2 | |||
| Surgical ward LOS. | 2 | 1 | 1 | ||
| Verticalization day, including moving away from bed. | 2 | 1 | 2 | ||
| Walking autonomy and/or distance (separated from composite scores). | 2 | 1 | 2 | ||
| Prospective Data Collection | ||
|---|---|---|
| Data Management | Data Source: Hospital | Data Source: Inpatient Rehabilitation Facility |
| Professional/scientific society registry. | ||
| Institutional registry. | ||
| Monocentric database. | 7 | |
| Multicentric database. | 4 | |
| Retrospective data collection. | ||
| Data management. | Data source: hospital. | Data source: inpatient rehabilitation facility. |
| Professional/scientific society registry. | 1 | |
| Institutional registry. | ||
| Monocentric database. | 9 | 2 |
| Multicentric database. | 2 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pennestrì, F.; Banfi, G. Predictive Factors of Inpatient Rehabilitation Stay After Elective Hip and Knee Replacement: A Scoping Review. Appl. Sci. 2025, 15, 11957. https://doi.org/10.3390/app152211957
Pennestrì F, Banfi G. Predictive Factors of Inpatient Rehabilitation Stay After Elective Hip and Knee Replacement: A Scoping Review. Applied Sciences. 2025; 15(22):11957. https://doi.org/10.3390/app152211957
Chicago/Turabian StylePennestrì, Federico, and Giuseppe Banfi. 2025. "Predictive Factors of Inpatient Rehabilitation Stay After Elective Hip and Knee Replacement: A Scoping Review" Applied Sciences 15, no. 22: 11957. https://doi.org/10.3390/app152211957
APA StylePennestrì, F., & Banfi, G. (2025). Predictive Factors of Inpatient Rehabilitation Stay After Elective Hip and Knee Replacement: A Scoping Review. Applied Sciences, 15(22), 11957. https://doi.org/10.3390/app152211957








