An In Vitro Study Comparing Debonding of Orthodontic Ceramic and Metal Brackets Using Er:YAG Laser and Conventional Pliers
Abstract
1. Introduction
2. Materials and Methods
- -
- Group C (n = 12): polycrystalline ceramic brackets (Transcend Series 6000, 3M Unitek, Monrovia, CA, USA);
- -
- Group M (n = 12): twin orthodontic metal bracket (Mini Master Series, American Orthodontics, Sheboygan, WI, USA).
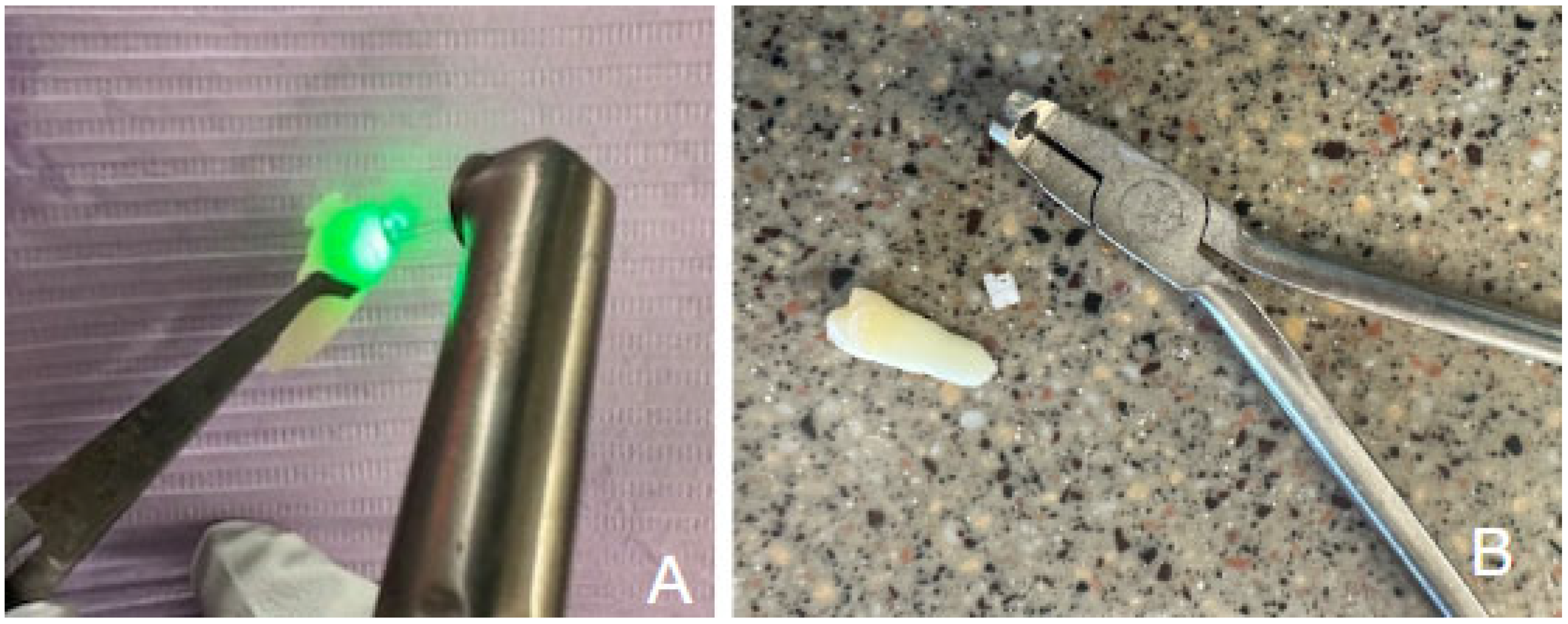
2.1. Laser-Assisted Debonding
2.2. Sample-Size Calculation and Study Endpoints
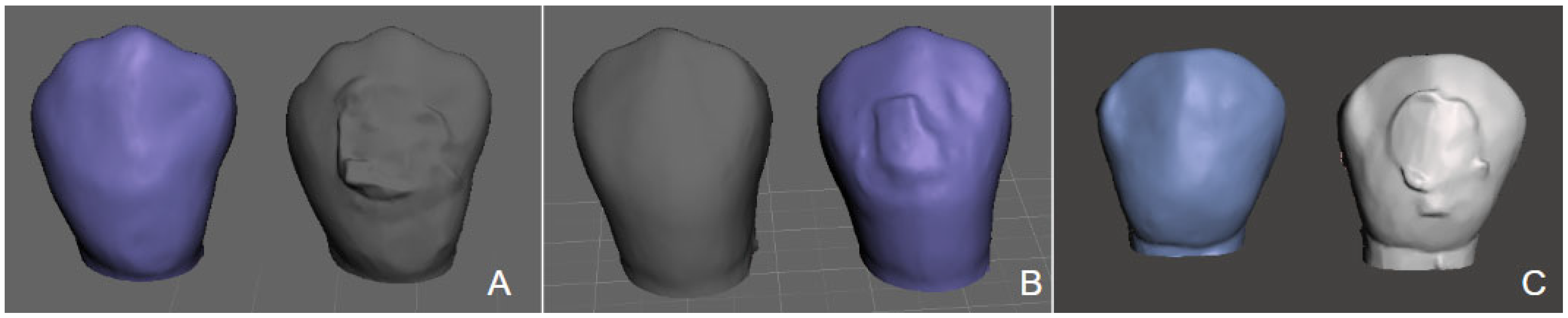
2.3. 3D Volumetric Analysis
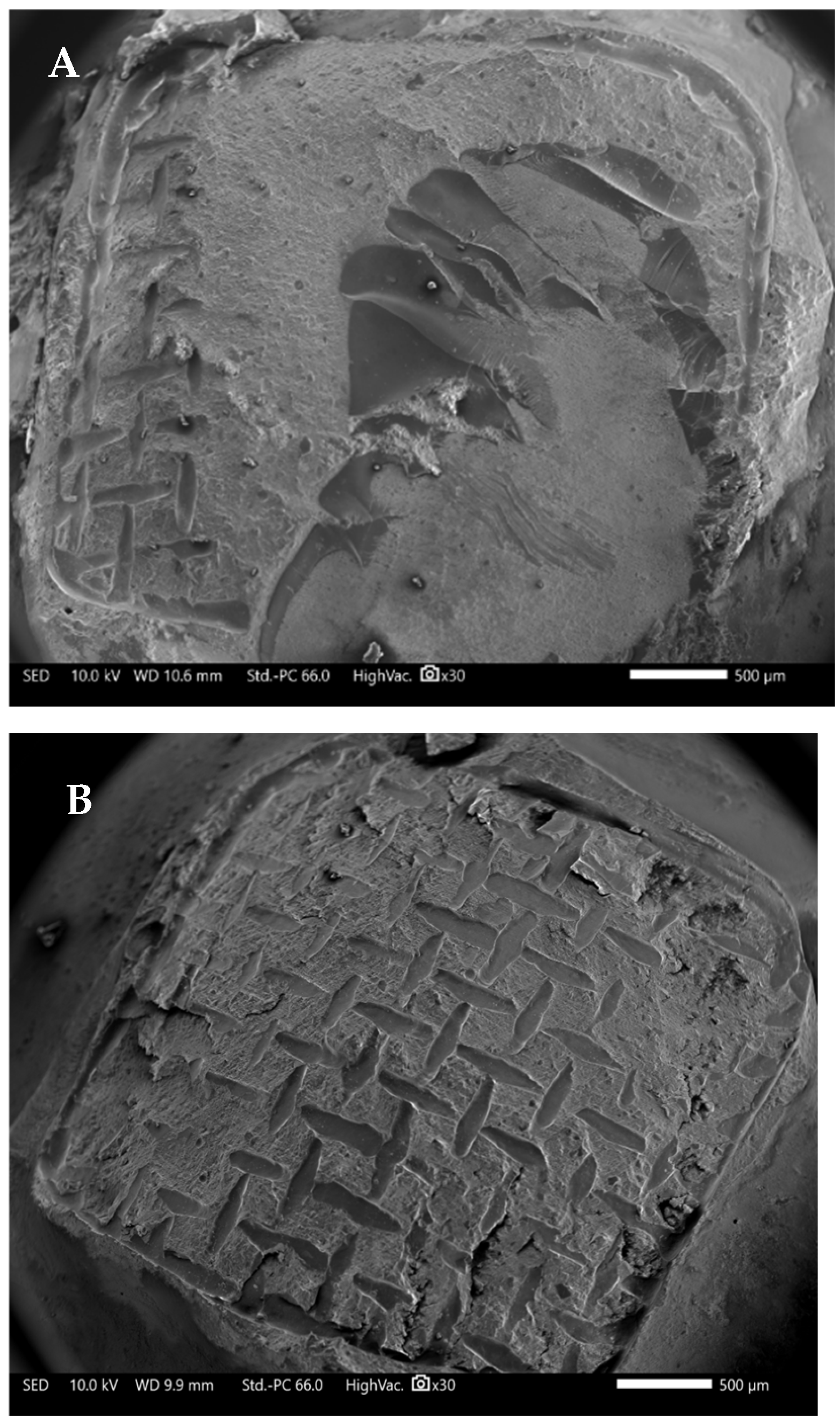
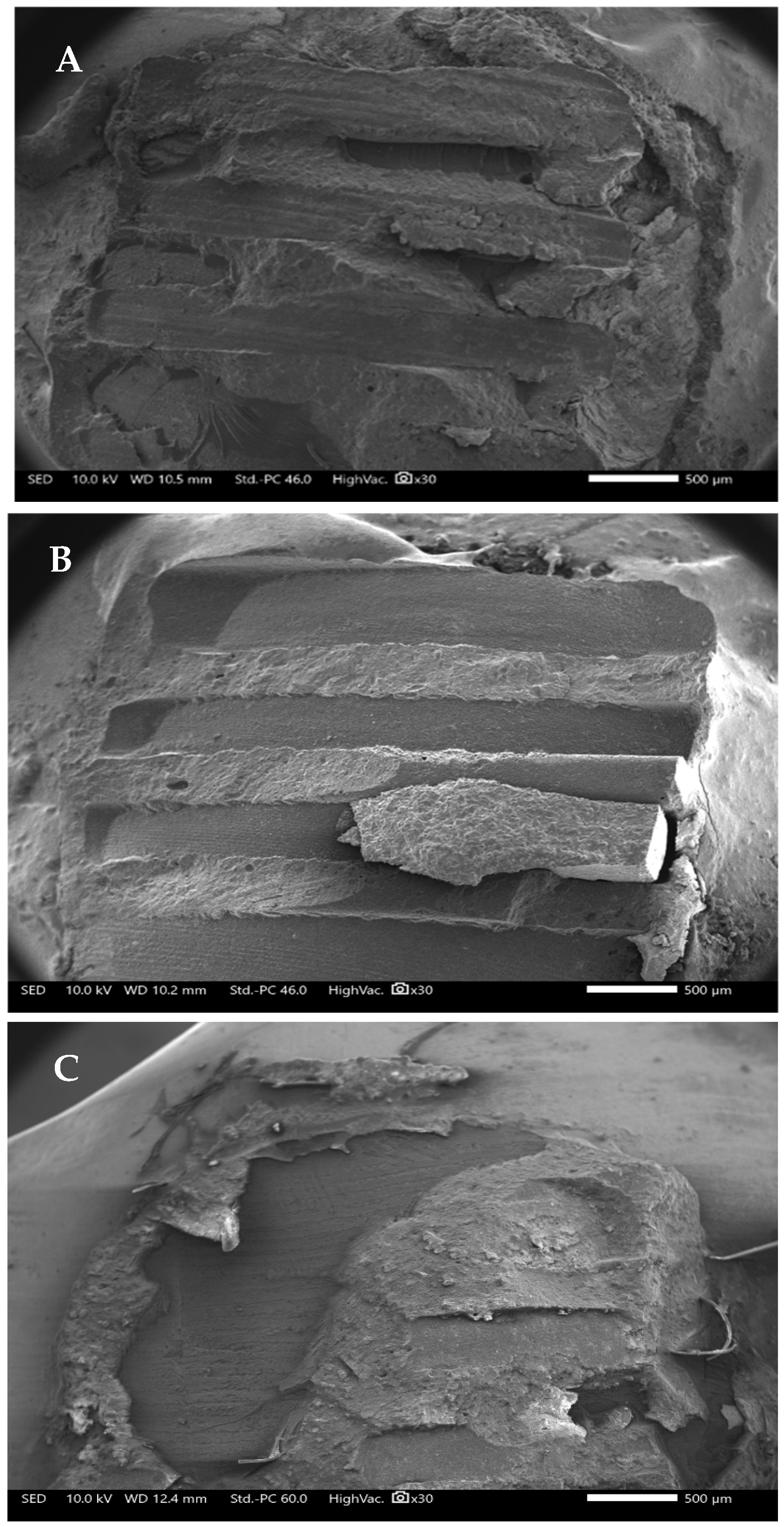
2.4. Surface Analysis
3. Results
3.1. Debonding Time
3.2. Residual Composite
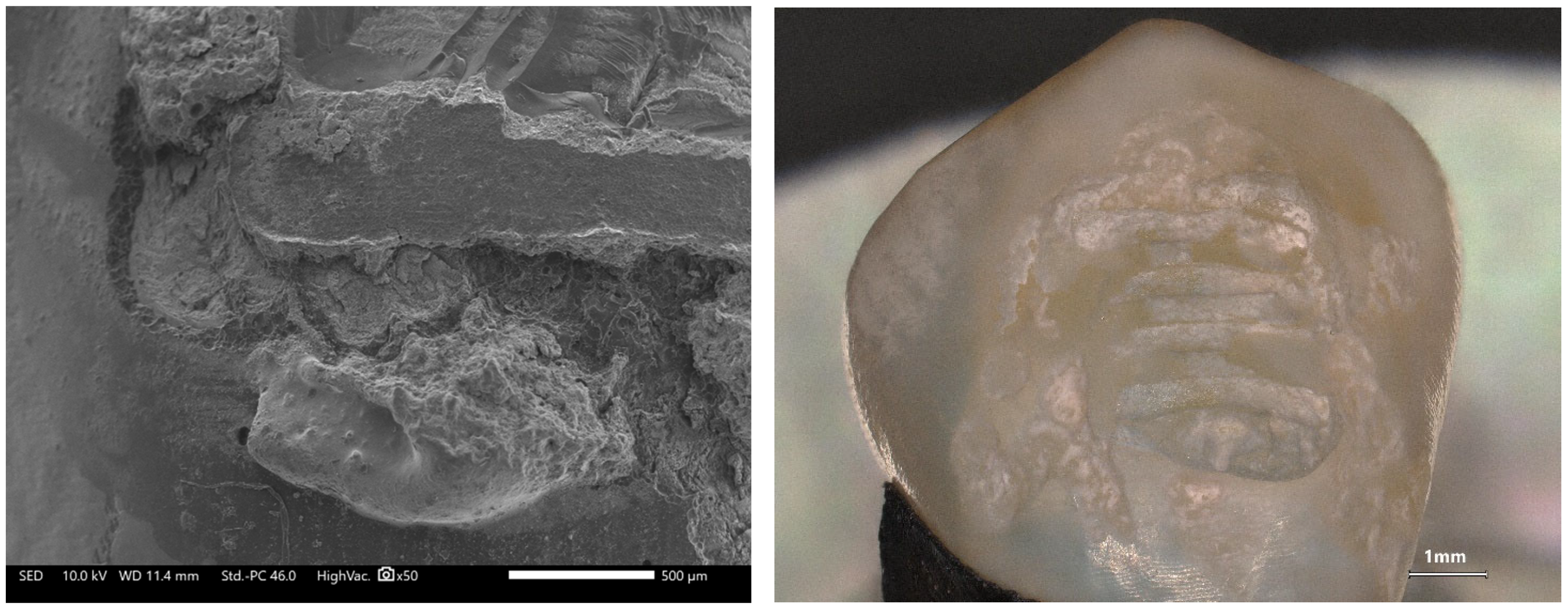
3.3. SEM Evaluation of Surface Morphology
4. Discussion
4.1. Limitation of the Study
4.2. Recommendations for the Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Azzeh, E.; Feldon, P.J. Laser debonding of ceramic brackets: A comprehensive review. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; Trulove, T.S. Comparisons of different debonding techniques for ceramic brackets: An in vitro study. Part I. Background and methods. Am. J. Orthod. Dentofac. Orthop. 1990, 98, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Eliades, T.; Eliades, G.; Brantley, W.A. Orthodontic brackets. In Orthodontic Materials Scientific and Clinical Aspects; Brantley, W.A., Eliades, T., Eds.; Thieme: Stuttgart, Germany, 2001; pp. 143–172. [Google Scholar]
- Macri, R.T.; de Lima, F.A.; Bachmann, L.; Galo, R.; Romano, F.L.; Borsatto, M.C.; Matsumoto, M.A. CO2 laser as auxiliary in the debonding of ceramic brackets. Lasers Med. Sci. 2015, 30, 1835–1841. [Google Scholar] [CrossRef] [PubMed]
- Saito, A.; Namura, Y.; Isokawa, K.; Shimizu, N. CO2 laser debonding of a ceramic bracket bonded with orthodontic adhesive containing thermal expansion microcapsules. Lasers Med. Sci. 2015, 30, 869–874. [Google Scholar] [CrossRef]
- Tu, S.; Sun, C.; Zhao, N.; Xiong, Z. Safety and Efficacy of the Erbium Laser in Debonding Dental Accessories: A Narrative Review. Photobiomodulation Photomed. Laser Surg. 2024, 42, 327–338. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Bencharit, S.; Dalal, N.; Mroczka, K.; Deeb, J.G. In Vitro Examination of the Use of Er:YAG Laser to Retrieve Lithium Disilicate Crowns from Titanium Implant Abutments. J. Prosthodont. 2019, 28, 672–676. [Google Scholar] [CrossRef]
- Deeb, J.G.; Grzech-Leśniak, K.; Weaver, C.; Matys, J.; Bencharit, S. Retrieval of Glass Fiber Post Using Er:YAG Laser and Conventional Endodontic Ultrasonic Method: An In Vitro Study. J. Prosthodont. 2019, 28, 1024–1028. [Google Scholar] [CrossRef]
- Elkharashi, A.; Grzech-Leśniak, K.; Deeb, J.G.; Abdulmajeed, A.A.; Bencharit, S. Exploring the use of pulsed erbium lasers to retrieve a zirconia crown from a zirconia implant abutment. PLoS ONE 2020, 15, e0233536. [Google Scholar] [CrossRef]
- Deeb, J.G.; Skrjanc, L.; Kanduti, D.; Carrico, C.; Saturno, A.M.; Grzech-Leśniak, K. Evaluation of Er:YAG and Er,Cr:YSGG laser irradiation for the debonding of prefabricated zirconia crowns. Adv. Clin. Exp. Med. 2021, 30, 7–15. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Bencharit, S.; Skrjanc, L.; Kanduti, D.; Matys, J.; Deeb, J.G. Utilization of Er:YAG Laser in Retrieving and Reusing of Lithium Disilicate and Zirconia Monolithic Crowns in Natural Teeth: An In Vitro Study. Appl. Sci. 2020, 10, 4357. [Google Scholar] [CrossRef]
- Deeb, J.G.; McCall, C.; Carrico, C.K.; Dahlke, W.O.; Grzech-Leśniak, K. Retrieval of Prefabricated Zirconia Crowns with Er,Cr:YSGG Laser from Primary and Permanent Molars. Materials 2020, 13, 5569. [Google Scholar] [CrossRef]
- Deeb, J.G.; Grzech-Leśniak, K.; Brody, E.R.; Matys, J.; Bencharit, S. Erbium laser-assisted ceramic debonding: A scoping review. J. Prosthodont. 2022, 31, e100–e124. [Google Scholar] [CrossRef]
- Raafat, S.; Zohdy, M.; Eldemellawy, M.; Ghali, R.; Taha, D. Efficiency of dry versus wet Er,Cr:YSGG laser debonding of lithium disilicate veneers using different power outputs. J. Prosthet. Dent. 2025, 133, 193.e1–193.e8. [Google Scholar] [CrossRef]
- Khalil, A.S.; Tamish, N.M.; Elkalza, A.R. Assessment of chemical, ultrasonic, diode laser, and Er:YAG laser application on debonding of ceramic brackets. BMC Oral Health 2022, 22, 79. [Google Scholar] [CrossRef]
- Villalobos-Tinoco, J.; Andretti, F.; Conner, C.; Rojas-Rueda, S.; Fischer, N.G.; Pagan-Banchs, M.; Jurado, C.A. A Narrative Review and Clinical Study on Er:YAG Laser Debonding of Ceramic and Composite Veneers. Biomimetics 2025, 10, 295. [Google Scholar] [CrossRef]
- Florczak-Matyjek, A.; Nikodem, A.; Kensy, J.; Matys, J.; Grzech-Leśniak, K. The Efficacy of Erbium-Ion, Diode, and CO2 Lasers in Debonding Attachments Used During Overlay Orthodontic Treatment and the Risk of Hard Tooth Tissue Damage Compared to Traditional Methods—An In Vitro Study. Photonics 2025, 12, 621. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J. The Effect of Er:YAG Lasers on the Reduction of Aerosol Formation for Dental Workers. Materials 2021, 14, 2857. [Google Scholar] [CrossRef]
- Alves, L.V.G.L.; da Silva, M.B.F.; Borsatto, M.C.; Corona, S.A.M. Do erbium lasers promote changes in the tooth enamel during debonding of ceramic laminate veneers? A systematic review. Lasers Med. Sci. 2023, 38, 217. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K.; Flieger, R.; Dominiak, M. Assessment of an Impact of a Diode Laser Mode with Wavelength of 980 nm on a Temperature Rise Measured by Means of k-02 Thermocouple: Preliminary Results. Dent. Med. Probl. 2016, 53, 345–351. [Google Scholar] [CrossRef]
- Arnabat-Dominguez, J.; Vecchio, A.D.; Todea, C.; Grzech-Leśniak, K.; Vescovi, P.; Romeo, U.; Nammour, S. Laser dentistry in daily practice during the COVID-19 pandemic: Benefits, risks and recommendations for safe treatments. Adv. Clin. Exp. Med. 2021, 30, 119–125. [Google Scholar] [CrossRef]
- Ma, T.; Marangoni, R.D.; Flint, W. In vitro comparison of debonding force and intrapulpal temperature changes during ceramic orthodontic bracket removal using a carbon dioxide laser. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 203–210. [Google Scholar] [CrossRef]
- Mimura, H.; Deguchi, T.; Obata, A.; Yamagishi, T.; Ito, M. Comparison of different bonding materials for laser debonding. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 267–273. [Google Scholar] [CrossRef]
- Obata, A.; Tsumura, T.; Niwa, K.; Ashizawa, Y.; Deguchi, T.; Ito, M. Super pulse CO2 laser for bracket bonding and debonding. Eur. J. Orthod. 1999, 21, 193–198. [Google Scholar] [CrossRef]
- Dostalova, T.; Jelinkova, H.; Remes, M.; Šulc, J.; Němec, M. The Use of the Er:YAG Laser for Bracket Debonding and Its Effect on Enamel Damage. Photomed. Laser Surg. 2016, 34, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Downarowicz, P.; Noszczyk, P.; Mikulewicz, M.; Nowak, R. Thermal effect of Er:YAG and Er,Cr:YSGG used for debonding ceramic and metal orthodontic brackets: An experimental analysis. Adv. Clin. Exp. Med. 2020, 29, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Sabuncuoglu, F.A.; Ersahan, S.; Erturk, E. Debonding of ceramic brackets by Er:YAG laser. J. Istanb. Univ. Fac. Dent. 2016, 50, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Crooks, M.; Hood, J.; Harkness, M. Thermal debonding of ceramic brackets: An in vitro study. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 163–172. [Google Scholar] [CrossRef]
- Mundethu, A.R.; Gutknecht, N.; Franzen, R. Rapid debonding of polycrystalline ceramic orthodontic brackets with an Er:YAG laser: An in vitro study. Lasers Med. Sci. 2014, 29, 1551–1556. [Google Scholar] [CrossRef]
- Khalil, A.S.; Baowideen, F.A.; Alhujaili, A.S.; Alotaibi, N.F.; Almanjhi, W.A.; Yassin, H.Y.; Nasser, M.M.; Alzahrani, A.F.; Alrehaili, R.S. Efficacy of Lasers in Debonding Ceramic Brackets: Exploring the Rationale and Methods. Cureus 2024, 16, e61050. [Google Scholar] [CrossRef]
- Sohrabpoor, H.; Issa, A.; Al Hamaoy, A.; Ahad, I.U.; Chikarakara, E.; Bagga, K.; Brabazon, D. Chapter 24—Development of Laser Processing Technologies via Experimental Design. In Woodhead Publishing Series in Welding and Other Joining Technologies, Advances in Laser Materials Processing, 2nd ed.; Lawrence, J., Ed.; Woodhead Publishing: Cambridge, UK, 2018; pp. 707–729. ISBN 9780081012529. [Google Scholar] [CrossRef]
- Luo, Q.; Huang, N.; Fu, T.; Wang, J.; Bartles, D.L.; Simpson, T.W.; Beese, A.M. New insight into the multivariate relationships among process, structure, and properties in laser powder bed fusion AlSi10Mg. Addit. Manuf. 2023, 77, 103804. [Google Scholar] [CrossRef]
- Xian, G.; Qi, X.; Shi, J.; Tian, J.; Xiao, H. Toughened and self-healing carbon nanotube/epoxy resin composites modified with polycaprolactone filler for coatings, adhesives and FRP. J. Build. Eng. 2025, 111, 113207. [Google Scholar] [CrossRef]
- Zhang, S.-Q.; Dong, H.; Han, Y.; Xu, L.; Feng, Y.-K.; Li, P.-Y. Coupling Effect of Disconnected Pores and Grain Morphology on the Corrosion Tolerance of Laser-Clad 316L Coating. Coatings 2024, 14, 40. [Google Scholar] [CrossRef]
- Vlasa, A.; Bud, E.S.; Păcurar, M.; Lazăr, L.; Streiche, L.; Bucur, S.M.; Cocoș, D.I.; Bud, A. Effects of Composite Resin on the Enamel after Debonding: An In Vitro Study-Metal Brackets vs. Ceramic Brackets. Appl. Sci. 2021, 11, 7353. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J.; Żmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Junior, A.B.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM, and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef]
- Abdulaziz, A.; El-Kholy, M.M.; Bushra, S.S.; Ali, S.M.; Shehab, K.A. Performance of two laser motion modes versus conventional orthodontic ceramic brackets debonding technique on enamel surface topography. Lasers Med. Sci. 2024, 39, 156. [Google Scholar] [CrossRef]
- Behnaz, M.; Dalaie, K.; Mirmohammadsadeghi, H.; Salehi, H.; Rakhshan, V.; Aslani, F. Shear bond strength and adhesive remnant index of orthodontic brackets bonded to enamel using adhesive systems mixed with TiO2 nanoparticles. Dental Press J. Orthod. 2018, 23, 43.e1–43.e7. [Google Scholar] [CrossRef]
- Deeb, J.G.; Crowell, A.; Richey, K.H.; Bencharit, S.; Carrico, C.K.; Williams, T.L.; Grzech-Leśniak, K. In Vitro Study of Laser-Assisted Prefabricated Ceramic Crown Debonding as Compared to Traditional Rotary Instrument Removal. Materials 2022, 15, 3617. [Google Scholar] [CrossRef]
- Jena, A.K.; Duggal, R.; Mehrotra, A.K. Physical properties and clinical characteristics of ceramic brackets: A comprehensive review. Trends Biomater. Artif. Organs 2007, 20, 101–115. [Google Scholar]
- Suliman, S.N.; Trojan, T.M.; Tantbirojn, D.; Versluis, A. Enamel loss following ceramic bracket debonding: A quantitative analysis in vitro. Angle Orthod. 2015, 85, 651–656. [Google Scholar] [CrossRef]
- Bora, N.; Mahanta, P.; Kalita, D.; Deka, S.; Konwar, R.; Phukan, C. Enamel Surface Damage following Debonding of Ceramic Brackets: A Hospital-Based Study. Sci. World J. 2021, 2021, 5561040. [Google Scholar] [CrossRef]
- Hoteit, M.; Nammour, S.; Zeinoun, T. Evaluation of Enamel Topography after Debonding Orthodontic Ceramic Brackets by Different Er,Cr:YSGG and Er:YAG Lasers Settings. Dent. J. 2020, 8, 6. [Google Scholar] [CrossRef]
- Ghazanfari, R.; Nokhbatolfoghahaei, H.; Alikhasi, M. Laser-Aided Ceramic Bracket Debonding: A Comprehensive Review. J. Lasers Med. Sci. 2016, 7, 2–11. [Google Scholar] [CrossRef]
- Beltrami, R.; Chiesa, M.; Scribante, A.; Allegretti, J.; Poggio, C. Comparison of shear bond strength of universal adhesives on etched and nonetched enamel. J. Appl. Biomater. Funct. Mater. 2016, 14, e78–e83. [Google Scholar] [CrossRef]
- Polat, S.; Çinar, Ç. The effect of the use of the deproteinization agent hypochlorous acid and two different pit and fissure sealant self-adhesive flowable composites upon its bonding with the enamel. J. Clin. Pediatr. Dent. 2024, 48, 144–151. [Google Scholar] [CrossRef]
| Group (n = 12) | Mean Time (Secs) | St.dev |
|---|---|---|
| Laser-assisted removal/metal bracket | 52.5 a | 13.57 |
| Laser-assisted removal/ceramic bracket | 56.25 a | 9.32 |
| Traditional removal/metal bracket | 0.76 b | 0.28 |
| Traditional removal/ceramic bracket | 0.64 b | 0.25 |
| Group (n = 12) | Volume Change (mm3) | St.dev |
|---|---|---|
| Laser-assisted removal/metal bracket | 1.99 a | 1.04 |
| Laser-assisted removal/ceramic | 1.80 a | 1.29 |
| Traditional mechanical removal | 4.21 b | 1.22 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdulmajeed, A.; Phan, T.; Grzech-Leśniak, K.; Deeb, J.G. An In Vitro Study Comparing Debonding of Orthodontic Ceramic and Metal Brackets Using Er:YAG Laser and Conventional Pliers. Appl. Sci. 2025, 15, 11844. https://doi.org/10.3390/app152111844
Abdulmajeed A, Phan T, Grzech-Leśniak K, Deeb JG. An In Vitro Study Comparing Debonding of Orthodontic Ceramic and Metal Brackets Using Er:YAG Laser and Conventional Pliers. Applied Sciences. 2025; 15(21):11844. https://doi.org/10.3390/app152111844
Chicago/Turabian StyleAbdulmajeed, Aous, Tiannie Phan, Kinga Grzech-Leśniak, and Janina Golob Deeb. 2025. "An In Vitro Study Comparing Debonding of Orthodontic Ceramic and Metal Brackets Using Er:YAG Laser and Conventional Pliers" Applied Sciences 15, no. 21: 11844. https://doi.org/10.3390/app152111844
APA StyleAbdulmajeed, A., Phan, T., Grzech-Leśniak, K., & Deeb, J. G. (2025). An In Vitro Study Comparing Debonding of Orthodontic Ceramic and Metal Brackets Using Er:YAG Laser and Conventional Pliers. Applied Sciences, 15(21), 11844. https://doi.org/10.3390/app152111844







