Retinal Straylight Measurements for Assessing Wear-Related Changes in Monthly Soft Contact Lenses
Abstract
1. Introduction
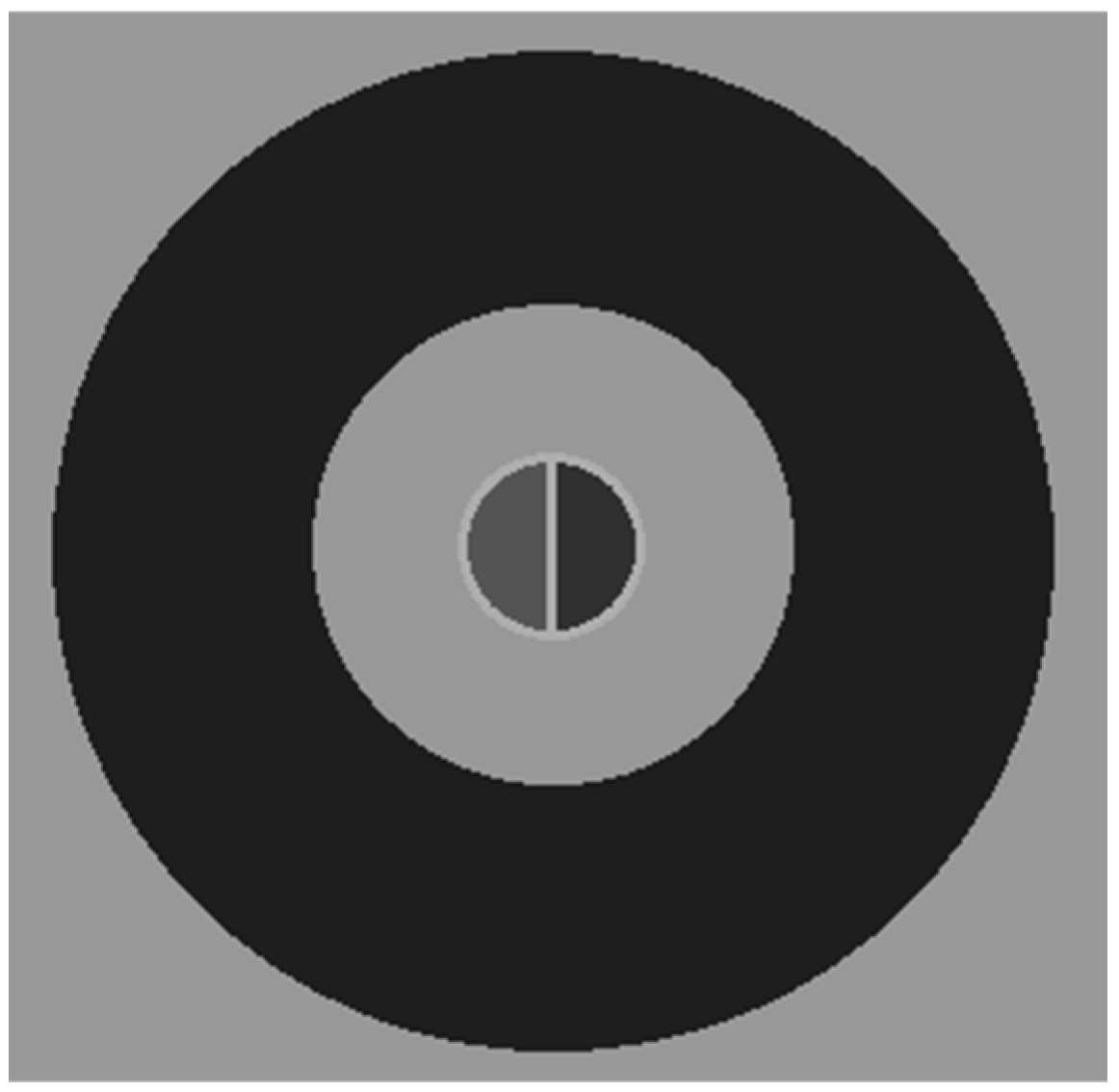
2. Materials and Methods
3. Results
3.1. Retinal Straylight with New and Worn Contact Lenses
3.2. Contact Lens Material and Discomfort
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SCLs | Soft contact lenses |
References
- Woods, C.A.; Bentley, S.A.; Fonn, D. Temporal changes in contact lens comfort over a day of wear. Ophthalmic Physiol. Opt. 2016, 36, 643–648. [Google Scholar] [CrossRef]
- Navascues-Cornago, M.; Morgan, P.B.; Maldonado-Codina, C. Effect of Three Interventions on Contact Lens Comfort in Symptomatic Wearers: A Randomized Clinical Trial. PLoS ONE 2015, 10, e0135323. [Google Scholar] [CrossRef]
- Fogt, J.S.; Menner, A.; Patton, K. Evaluation of wear experience with water surface daily disposable lenses in satisfied reusable soft contact lens wearers. J. Contact Lens. Res. Sci. 2022, 6, e18–e24. [Google Scholar] [CrossRef]
- Dumbleton, K.; Woods, C.A.; Jones, L.W.; Fonn, D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens 2013, 39, 93–99. [Google Scholar] [CrossRef]
- Guillon, M.; Dumbleton, K.A.; Theodoratos, P.; Wong, S.; Patel, K.; Banks, G.; Patel, T. Association Between Contact Lens Discomfort and Pre-lens Tear Film Kinetics. Optom. Vis. Sci. 2016, 93, 881–891. [Google Scholar] [CrossRef]
- Sapkota, K.; Franco, S.; Lira, M. Daily versus monthly disposable contact lens: Which is better for ocular surface physiology and comfort? Contact Lens Anterior Eye 2018, 41, 252–257. [Google Scholar] [CrossRef]
- Grupcheva, C. Visual, perceptual and cosmetic comfort: Daily disposable versus monthly silicone-hydrogel lenses. Ophthalmol. East. Eur. 2020, 10, 148–156. [Google Scholar]
- Dumbleton, K.; Woods, C.; Jones, L.; Richter, D.; Fonn, D. Comfort and vision with silicone hydrogel lenses: Effect of compliance. Optom. Vis. Sci. 2010, 87, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Guthrie, S.; Ng, A.; Woods, J.; Vega, J.; Orsborn, G.; Jones, L. Exploring the factors which impact overall satisfaction with single vision contact lenses. Contact Lens Anterior Eye 2022, 45, 101579. [Google Scholar] [CrossRef]
- Pucker, A.D.; Franklin, Q.X.; Perkins, A.F.; May, K.; Kannarr, S.R.; Bromley, M.; Lievens, C. Performance of a Toric, Monthly, Soft Contact Lens in Digital Device Users. Clin. Optom. 2025, 17, 11–20. [Google Scholar] [CrossRef]
- Belda-Salmerón, L.; Ferrer-Blasco, T.; Albarrán-Diego, C.; Madrid-Costa, D.; Montés-Micó, R. Diurnal variations in visual performance for disposable contact lenses. Optom. Vis. Sci. 2013, 90, 682–690. [Google Scholar] [CrossRef] [PubMed]
- Sapkota, K.; Franco, S.; Lira, M. Contrast sensitivity function with soft contact lens wear. J. Optom. 2020, 13, 96–101. [Google Scholar] [CrossRef]
- Williams, M.A.; Moutray, T.N.; Jackson, A.J. Uniformity of visual acuity measures in published studies. Investig. Ophthalmol. Vis. Sci. 2008, 49, 4321–4327. [Google Scholar] [CrossRef] [PubMed]
- Elliott, D.B.; Bullimore, M.A.; Patla, A.E.; Whitaker, D. Effect of a cataract simulation on clinical and real world vision. Br. J. Ophthalmol. 1996, 80, 799–804. [Google Scholar] [CrossRef]
- de Wit, G.C.; Coppens, J.E. Stray light of spectacle lenses compared with stray light in the eye. Optom. Vis. Sci. 2003, 80, 395–400. [Google Scholar] [CrossRef] [PubMed]
- van Den Berg, T.J.; Franssen, L.; Coppens, J.E. Straylight in the human eye: Testing objectivity and optical character of the psychophysical measurement. Ophthalmic Physiol. Opt. 2009, 29, 345–350. [Google Scholar] [CrossRef]
- van der Meulen, I.J.; Gjertsen, J.; Kruijt, B.; Witmer, J.P.; Rulo, A.; Schlingemann, R.O.; van den Berg, T.J. Straylight measurements as an indication for cataract surgery. J. Cataract Refract. Surg. 2012, 38, 840–848. [Google Scholar] [CrossRef]
- van Bree, M.C.; van Verre, H.P.; Devreese, M.T.; Larminier, F.; van den Berg, T.J. Straylight values after refractive surgery: Screening for ocular fitness in demanding professions. Ophthalmology 2011, 118, 945–953. [Google Scholar] [CrossRef]
- Vos, J.J. On the cause of disability glare and its dependence on glare angle, age and ocular pigmentation. Clin. Exp. Ophthalmol. 2003, 86, 363–370. [Google Scholar] [CrossRef]
- Liesegang, T.J. Physiologic changes of the cornea with contact lens wear. CLAO J. 2002, 28, 12–27. [Google Scholar] [PubMed]
- van der Meulen, I.J.; Engelbrecht, L.A.; van Vliet, J.M.; Lapid-Gortzak, R.; Nieuwendaal, C.P.; Mourits, M.P.; Schlingemann, R.O.; van den Berg, T.J. Straylight measurements in contact lens wear. Cornea 2010, 29, 516–522. [Google Scholar] [CrossRef]
- Cerviño, A.; Gonzalez-Meijome, J.M.; Linhares, J.M.M.; Hosking, S.L.; Montes-Mico, R. Effect of sport-tinted contact lenses for contrast enhancement on retinal straylight measurements. Ophthalmic Physiol. Opt. 2008, 28, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Gaurisankar, Z.S.; van Rijn, G.A.; Luyten, G.P.; van den Berg, T.J. Straylight as The Result of Refractive Correction. Clin. Ophthalmol. 2019, 13, 2195–2201. [Google Scholar] [CrossRef]
- Franssen, L.; Coppens, J.E.; van den Berg, T.J. Compensation comparison method for assessment of retinal straylight. Investig. Ophthalmol. Vis. Sci. 2006, 47, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A.G. *Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Beck, T.W. The importance of a priori sample size estimation in strength and conditioning research. J. Strength Cond. Res. 2013, 27, 2323–2337. [Google Scholar] [CrossRef]
- de Wit, G.C.; Franssen, L.; Coppens, J.E.; van den Berg, T.J. Simulating the straylight effects of cataracts. J. Cataract Refract. Surg. 2006, 32, 294–300. [Google Scholar] [CrossRef]
- Cerviño, A.; Bansal, D.; Hosking, S.L.; Montés-Micó, R. Objective measurement of intraocular forward light scatter using Hartmann-Shack spot patterns from clinical aberrometers: Model-eye and human-eye study. J. Cataract Refract. Surg. 2008, 34, 1089–1095. [Google Scholar] [CrossRef]
- van Rijn, L.J.; Nischler, C.; Gamer, D.; Franssen, L.; de Wit, G.; Kaper, R.; Vonhoff, D.; Grabner, G.; Wilhelm, H.; Völker-Dieben, H.J.; et al. Measurement of stray light and glare: Comparison of Nyktotest, Mesotest, stray light meter, and computer implemented stray light meter. Br. J. Ophthalmol. 2005, 89, 345–351. [Google Scholar] [CrossRef]
- Queirós, A.; Villa-Collar, C.; Gutiérrez, A.R.; Jorge, J.; González-Méijome, J.M. Quality of life of myopic subjects with different methods of visual correction using the NEI RQL-42 questionnaire. Eye Contact Lens 2012, 38, 116–121. [Google Scholar] [CrossRef]
- González-Pérez, J.; Sánchez García, Á.; Villa-Collar, C. Vision-Specific Quality of Life: Laser-Assisted in situ Keratomileusis Versus Overnight Contact Lens Wear. Eye Contact Lens 2019, 45, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Sauer, A.; Meyer, N.; Bourcier, T. French Study Group for Contact Lens–Related Microbial Keratitis. Risk Factors for Contact Lens-Related Microbial Keratitis: A Case-Control Multicenter Study. Eye Contact Lens 2016, 42, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Łabuz, G.; López-Gil, N.; van den Berg, T.J.; Vargas-Martín, F. Ocular Straylight with Different Multifocal Contact Lenses. Optom. Vis. Sci. 2017, 94, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Tauste, A.; Ronda, E.; Molina, M.J.; Seguí, M. Effect of contact lens use on Computer Vision Syndrome. Ophthalmic Physiol. Opt. 2016, 36, 112–119. [Google Scholar] [CrossRef]
- Goudie, C.; Tatham, A.; Davies, R.; Sifton, A.; Wright, M. The effect of the timing of the cessation of contact lens use on the results of biometry. Eye 2018, 32, 1048–1054. [Google Scholar] [CrossRef]
- Hashemi, H.; Firoozabadi, M.R.; Mehravaran, S.; Gorouhi, F. Corneal stability after discontinued soft contact lens wear. Contact Lens Anterior Eye 2008, 31, 122–125. [Google Scholar] [CrossRef]
- Rozema, J.J.; Van den Berg, T.J.; Tassignon, M.J. Retinal straylight as a function of age and ocular biometry in healthy eyes. Investig. Ophthalmol. Vis. Sci. 2010, 51, 2795–2799. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ikaunieks, G.; Petrovica, I. Retinal Straylight Measurements for Assessing Wear-Related Changes in Monthly Soft Contact Lenses. Appl. Sci. 2025, 15, 11345. https://doi.org/10.3390/app152111345
Ikaunieks G, Petrovica I. Retinal Straylight Measurements for Assessing Wear-Related Changes in Monthly Soft Contact Lenses. Applied Sciences. 2025; 15(21):11345. https://doi.org/10.3390/app152111345
Chicago/Turabian StyleIkaunieks, Gatis, and Inese Petrovica. 2025. "Retinal Straylight Measurements for Assessing Wear-Related Changes in Monthly Soft Contact Lenses" Applied Sciences 15, no. 21: 11345. https://doi.org/10.3390/app152111345
APA StyleIkaunieks, G., & Petrovica, I. (2025). Retinal Straylight Measurements for Assessing Wear-Related Changes in Monthly Soft Contact Lenses. Applied Sciences, 15(21), 11345. https://doi.org/10.3390/app152111345





