The Effect of Implant Thread’s Pitch on Primary Stability: An In Vitro Polyurethane Study with Under-Preparation and Low-Speed Drilling
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Drilling Procedure
2.3. Insertion Torque (IT) and Removal Torque (RT) Assessment
2.4. Resonance Frequency Analysis (RFA)
2.5. Statistical Analysis
3. Results
3.1. IT Values
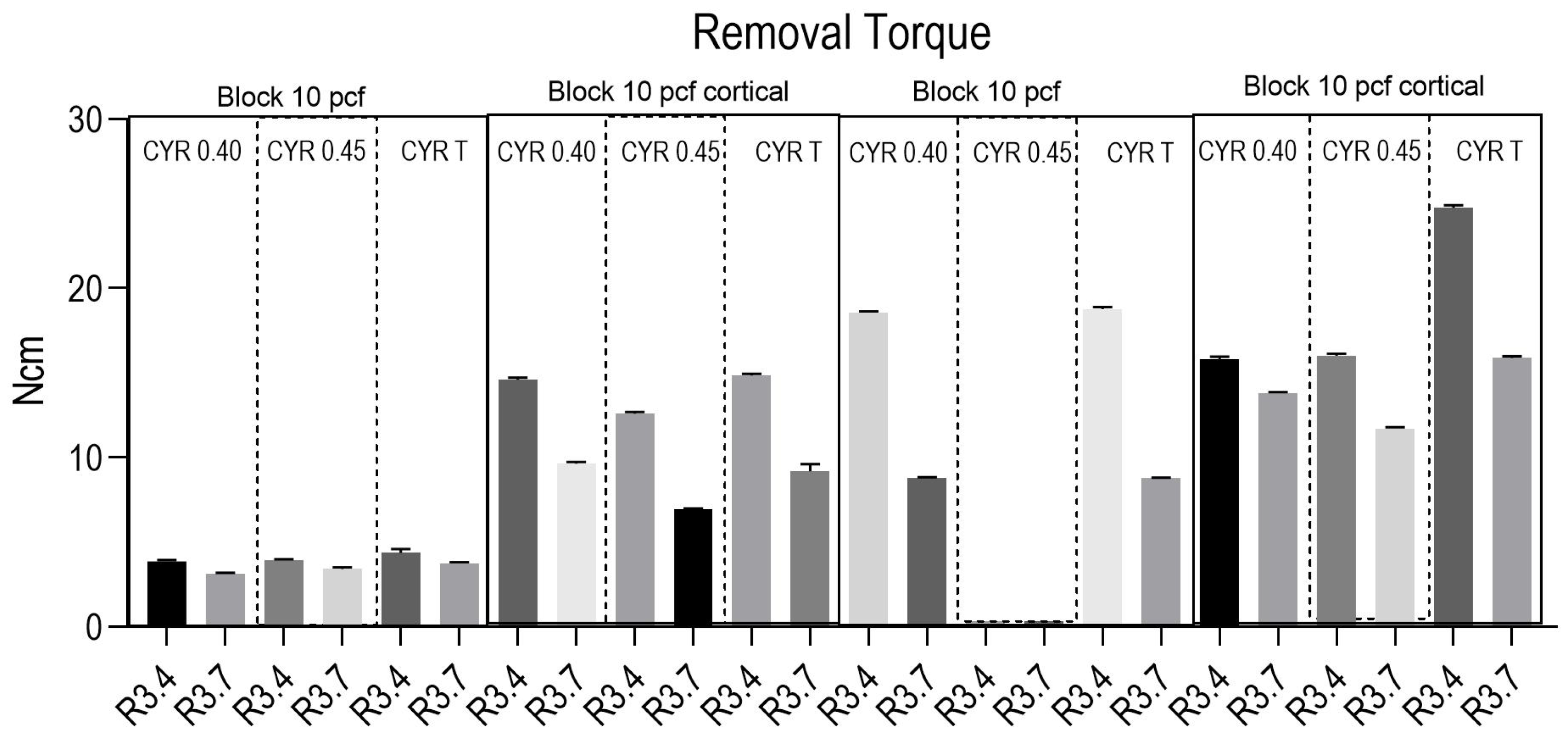
3.2. RT Values
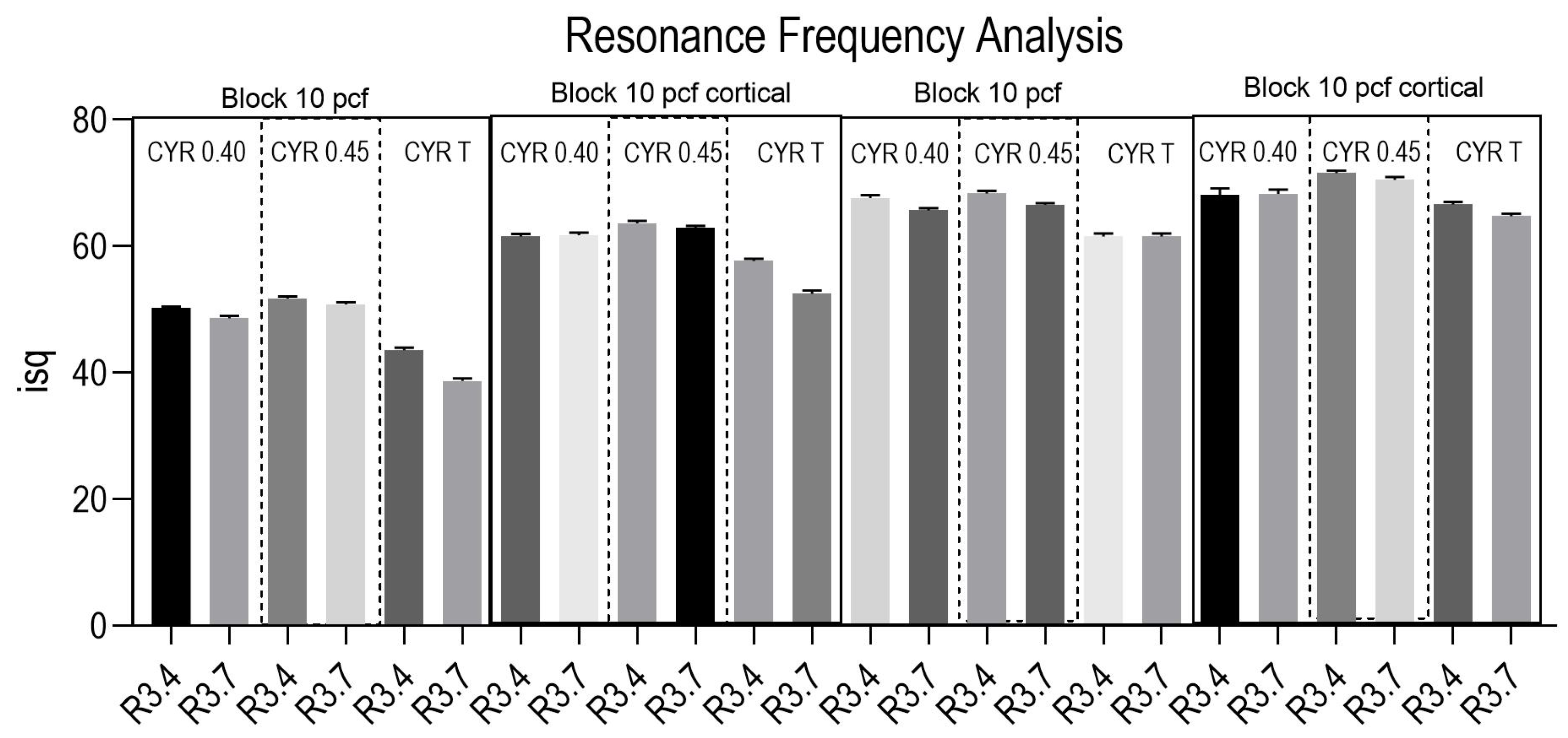
3.3. RFA Values
3.4. Pairwise Comparison
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anitua, E.; Alkhraisat, M.H.; Piñas, L.; Orive, G. Efficacy of Biologically Guided Implant Site Preparation to Obtain Adequate Primary Implant Stability. Ann. Anat. Anat. Anz. 2015, 199, 9–15. [Google Scholar] [CrossRef]
- Abbou, M. Primary Stability and Osseointegration: Preliminary Clinical Results with a Tapered Diminishing-Thread Implant. Pract. Proced. Aesthetic Dent. 2003, 15, 161–168, quiz 170. [Google Scholar]
- Nevins, M.; Nevins, M.L.; Schupbach, P.; Fiorellini, J.; Lin, Z.; Kim, D.M. The Impact of Bone Compression on Bone-to-Implant Contact of an Osseointegrated Implant: A Canine Study. Int. J. Periodontics Restor. Dent. 2012, 32, 637–645. [Google Scholar]
- Barberá-Millán, J.; Larrazábal-Morón, C.; Enciso-Ripoll, J.-J.; Pérez-Pevida, E.; Chávarri-Prado, D.; Gómez-Adrián, M.-D. Evaluation of the Primary Stability in Dental Implants Placed in Low Density Bone with a New Drilling Technique, Osseodensification: An in Vitro Study. Med. Oral Patol. Oral Y Cir. Bucal 2021, 26, e361–e367. [Google Scholar] [CrossRef]
- Abuhussein, H.; Pagni, G.; Rebaudi, A.; Wang, H.-L. The Effect of Thread Pattern upon Implant Osseointegration. Clin. Oral. Implant. Res. 2010, 21, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Benalcázar-Jalkh, E.B.; Nayak, V.V.; Gory, C.; Marquez-Guzman, A.; Bergamo, E.T.; Tovar, N.; Coelho, P.G.; Bonfante, E.A.; Witek, L. Impact of Implant Thread Design on Insertion Torque and Osseointegration: A Preclinical Model. Med. Oral Patol. Oral Y Cirugía Bucal 2023, 28, e48–e55. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Z.-C.; Chen, Y.-J.; Tung, Y.-Y.; Chiang, Y.-Y.; Lai, E.H.-H.; Chen, W.-P.; Lin, C.-P. Effects of Thread Depth, Taper Shape, and Taper Length on the Mechanical Properties of Mini-Implants. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 279–288. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; De Angelis, F.; Lorusso, F.; Piattelli, A.; Iezzi, G. Influence of the Dental Implant Macrogeometry and Threads Design on Primary Stability: An in Vitro Simulation on Artificial Bone Blocks. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 1242–1250. [Google Scholar] [CrossRef] [PubMed]
- Amid, R.; Raoofi, S.; Kadkhodazadeh, M.; Movahhedi, M.R.; Khademi, M. Effect of Microthread Design of Dental Implants on Stress and Strain Patterns: A Three-Dimensional Finite Element Analysis. Biomed. Tech./Biomed. Eng. 2013, 58, 457–467. [Google Scholar] [CrossRef]
- Bilhan, H.; Geckili, O.; Mumcu, E.; Bozdag, E.; Sünbüloğlu, E.; Kutay, O. Influence of Surgical Technique, Implant Shape and Diameter on the Primary Stability in Cancellous Bone. J. Oral Rehabil. 2010, 37, 900–907. [Google Scholar] [CrossRef]
- Irinakis, T.; Wiebe, C. Initial Torque Stability of a New Bone Condensing Dental Implant. A Cohort Study of 140 Consecutively Placed Implants. J. Oral Implant. 2009, 35, 277–282. [Google Scholar] [CrossRef]
- Bolind, P.K.; Johansson, C.B.; Becker, W.; Langer, L.; Sevetz, E.B.; Albrektsson, T.O. A Descriptive Study on Retrieved Non-threaded and Threaded Implant Designs. Clin. Oral Implant. Res. 2005, 16, 447–455. [Google Scholar] [CrossRef]
- Trisi, P.; Berardini, M.; Falco, A.; Podaliri Vulpiani, M. Validation of Value of Actual Micromotion as a Direct Measure of Implant Micromobility after Healing (Secondary Implant Stability). An in Vivo Histologic and Biomechanical Study. Clin. Oral Implant. Res. 2016, 27, 1423–1430. [Google Scholar] [CrossRef]
- Willenegger, H.; Perren, S.M.; Schenk, R. Primary and Secondary Healing of Bone Fractures. Der Chir. Z. Fur Alle Geb. Der Oper. Medizen 1971, 42, 241–252. [Google Scholar]
- Schenk, R.K. Histology of Primary Bone Healing. Fortschritte Der Kiefer-Und Gesichts-Chir. 1975, 19, 8–12. [Google Scholar]
- Schenk, R.K.; Willenegger, H.R. Histology of Primary Bone Healing: Modifications and Limits of Recovery of Gaps in Relation to Extent of the Defect (Author’s Transl). Unfallheilkunde 1977, 80, 155–160. [Google Scholar] [PubMed]
- Comuzzi, L.; Tumedei, M.; Piattelli, A.; Iezzi, G. Short vs. Standard Length Cone Morse Connection Implants: An In Vitro Pilot Study in Low Density Polyurethane Foam. Symmetry 2019, 11, 1349. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; Romasco, T.; Petrini, M.; Afrashtehfar, K.I.; Inchingolo, F.; Piattelli, A.; Di Pietro, N. Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An in Vitro Study on Polyurethane Foam Sheets. J. Funct. Biomater. 2022, 14, 10. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Arosio, P.; Gastaldi, G.; Gherlone, E. The Insertion Torque-Depth Curve Integral as a Measure of Implant Primary Stability: An in Vitro Study on Polyurethane Foam Blocks. J. Prosthet. Dent. 2018, 120, 706–714. [Google Scholar] [CrossRef]
- ASTM F1839-08; Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopedic Devices and Instruments. ASTM: West Conshohcken, PA, USA, 2021.
- Attanasio, F.; Antonelli, A.; Brancaccio, Y.; Averta, F.; Figliuzzi, M.M.; Fortunato, L.; Giudice, A. Primary Stability of Three Different Osteotomy Techniques in Medullary Bone: An in Vitro Study. Dent. J. 2020, 8, 21. [Google Scholar] [CrossRef]
- Cavallaro, J.; Greenstein, B.; Greenstein, G. Clinical Methodologies for Achieving Primary Dental Implant Stability: The Effects of Alveolar Bone Density. J. Am. Dent. Assoc. (1939) 2009, 140, 1366–1372. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, D.A.; Arosio, P. Correlation Between Bone Density and Instantaneous Torque at Implant Site Preparation: A Validation on Polyurethane Foam Blocks of a Device Assessing Density of Jawbones. Int. J. Oral Maxillofac. Implant. 2016, 31, e128–e135. [Google Scholar] [CrossRef]
- Schrotenboer, J.; Tsao, Y.-P.; Kinariwala, V.; Wang, H.-L. Effect of Microthreads and Platform Switching on Crestal Bone Stress Levels: A Finite Element Analysis. J. Periodontol. 2008, 79, 2166–2172. [Google Scholar] [CrossRef]
- Al-Sabbagh, M.; Eldomiaty, W.; Khabbaz, Y. Can Osseointegration Be Achieved Without Primary Stability? Dent. Clin. N. Am. 2019, 63, 461–473. [Google Scholar] [CrossRef]
- de Carvalho Formiga, M.; Gehrke, A.F.; de Bortoli, J.P.; Gehrke, S.A. Can the Design of the Instruments Used for Undersized Osteotomies Influence the Initial Stability of Implants Installed in Low-Density Bone? An in Vitro Pilot Study. PLoS ONE 2021, 16, e0257985. [Google Scholar] [CrossRef]
- Danza, M.; Quaranta, A.; Carinci, F.; Paracchini, L.; Pompa, G.; Vozza, I. Biomechanical evaluation of dental implants in D1 and D4 bone by Finite Element Analysis. Minerva Stomatol. 2010, 59, 305–313. [Google Scholar]
- Almasoud, N.N.; Tanneru, N.; Marei, H.F. Alveolar Bone Density and Its Clinical Implication in the Placement of Dental Implants and Orthodontic Mini-Implants. Saudi Med. J. 2016, 37, 684–689. [Google Scholar] [CrossRef] [PubMed]


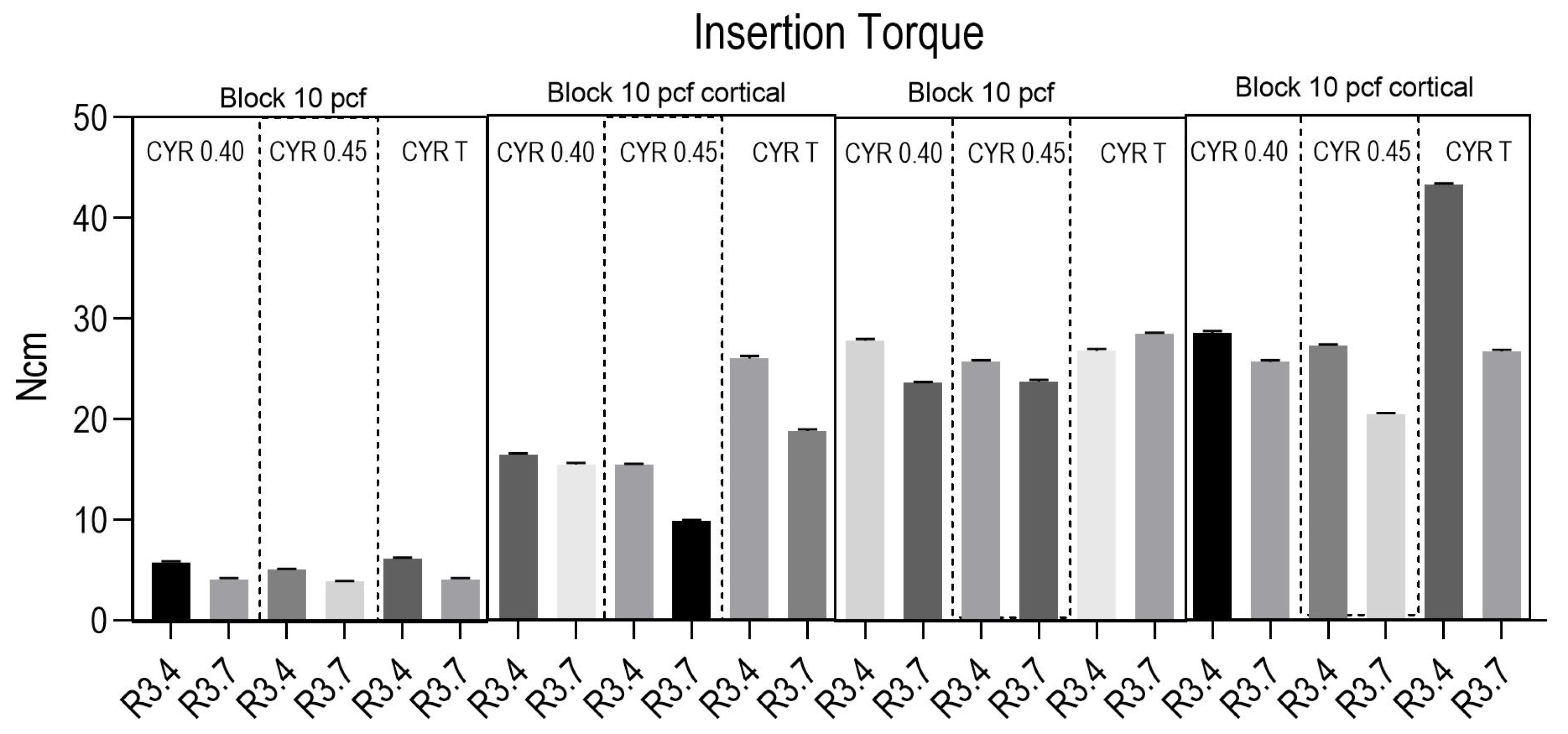
| 10 PCF | 10 PCF CORTICAL | 20 PCF | 20 PCF CORTICAL | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | |||||||||||||
| R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | |
| 25% Percentile | 5.58 | 3.9 | 4.9 | 3.8 | 5.98 | 3.98 | 16.4 | 15.3 | 15.4 | 9.8 | 25.8 | 18.7 | 27.7 | 23.5 | 25.6 | 23.6 | 26.6 | 28.4 | 28.4 | 25.5 | 27.2 | 20.4 | 43.2 | 26.6 |
| Median | 5.7 | 4.05 | 5 | 3.9 | 6.1 | 4.1 | 16.5 | 15.5 | 15.5 | 9.9 | 26 | 18.8 | 27.9 | 23.6 | 25.8 | 23.8 | 26.8 | 28.5 | 28.6 | 25.8 | 27.4 | 20.5 | 43.3 | 26.8 |
| 75% Percentile | 5.9 | 4.2 | 5.1 | 3.9 | 6.2 | 4.2 | 16.6 | 15.6 | 15.6 | 10 | 26.3 | 19 | 28 | 23.7 | 25.8 | 23.8 | 27 | 28.6 | 28.8 | 25.8 | 27.4 | 20.6 | 43.4 | 26.9 |
| Mean | 5.72 | 4.05 | 5.01 | 3.86 | 6.09 | 4.08 | 16.5 | 15.5 | 15.5 | 9.91 | 26 | 18.8 | 27.8 | 23.6 | 25.7 | 23.7 | 26.8 | 28.5 | 28.6 | 25.7 | 27.3 | 20.5 | 43.3 | 26.7 |
| Std. Deviation | 0.155 | 0.127 | 0.08 | 0.05 | 0.12 | 0.12 | 0.13 | 0.16 | 0.12 | 0.09 | 0.279 | 0.16 | 0.16 | 0.08 | 0.13 | 0.16 | 0.21 | 0.13 | 0.212 | 0.163 | 0.106 | 0.116 | 0.149 | 0.177 |
| Std. Error of the Mean | 0.04 | 0.04 | 0.02 | 0.02 | 0.03 | 0.03 | 0.04 | 0.05 | 0.04 | 0.03 | 0.09 | 0.05 | 0.05 | 0.03 | 0.04 | 0.05 | 0.068 | 0.04 | 0.06 | 0.05 | 0.03 | 0.03 | 0.0471 | 0.0559 |
| Lower 95% CI of the mean | 5.61 | 3.96 | 4.95 | 3.82 | 6 | 3.99 | 16.4 | 15.4 | 15.4 | 9.85 | 25.8 | 18.7 | 27.7 | 23.5 | 25.6 | 23.6 | 26.6 | 28.4 | 28.4 | 25.6 | 27.3 | 20.4 | 43.2 | 26.6 |
| Upper 95% CI of the mean | 5.83 | 4.14 | 5.07 | 3.9 | 6.18 | 4.17 | 16.6 | 15.6 | 15.5 | 9.97 | 26.2 | 18.9 | 27.9 | 23.7 | 25.8 | 23.8 | 26.9 | 28.6 | 28.7 | 25.8 | 27.4 | 20.6 | 43.4 | 26.9 |
| 10 PCF | 10 PCF CORTICAL | 20 PCF | 20 PCF CORTICAL | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | |||||||||||||
| R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | |
| 25% Percentile | 3.80 | 3.00 | 3.90 | 3.38 | 4.30 | 3.68 | 14.5 | 9.50 | 12.5 | 3.80 | 3.00 | 3.90 | 3.38 | 4.30 | 3.68 | 14.5 | 9.50 | 12.5 | 3.80 | 3.00 | 3.90 | 3.38 | 4.30 | 3.68 |
| Median | 3.90 | 3.10 | 3.90 | 3.45 | 4.45 | 3.80 | 14.6 | 9.60 | 12.6 | 3.90 | 3.10 | 3.90 | 3.45 | 4.45 | 3.80 | 14.6 | 9.60 | 12.6 | 3.90 | 3.10 | 3.90 | 3.45 | 4.45 | 3.80 |
| 75% Percentile | 3.90 | 3.20 | 4.00 | 3.50 | 4.50 | 3.80 | 14.7 | 9.73 | 12.7 | 3.90 | 3.20 | 4.00 | 3.50 | 4.50 | 3.80 | 14.7 | 9.73 | 12.7 | 3.90 | 3.20 | 4.00 | 3.50 | 4.50 | 3.80 |
| Mean | 3.87 | 3.11 | 3.94 | 3.42 | 4.36 | 3.74 | 14.6 | 9.63 | 12.6 | 3.87 | 3.11 | 3.94 | 3.42 | 4.36 | 3.74 | 14.6 | 9.63 | 12.6 | 3.87 | 3.11 | 3.94 | 3.42 | 4.36 | 3.74 |
| Std. Deviation | 0.0675 | 0.0876 | 0.0516 | 0.103 | 0.222 | 0.0843 | 0.120 | 0.116 | 0.0816 | 0.0675 | 0.0876 | 0.0516 | 0.103 | 0.222 | 0.0843 | 0.120 | 0.116 | 0.0816 | 0.0675 | 0.0876 | 0.0516 | 0.103 | 0.222 | 0.0843 |
| Std. Error of the Mean | 0.0213 | 0.0277 | 0.0163 | 0.0327 | 0.0702 | 0.0267 | 0.0379 | 0.0367 | 0.0258 | 0.0213 | 0.0277 | 0.0163 | 0.0327 | 0.0702 | 0.0267 | 0.0379 | 0.0367 | 0.0258 | 0.0213 | 0.0277 | 0.0163 | 0.0327 | 0.0702 | 0.0267 |
| Lower 95% CI of the mean | 3.82 | 3.05 | 3.90 | 3.35 | 4.20 | 3.68 | 14.5 | 9.55 | 12.5 | 3.82 | 3.05 | 3.90 | 3.35 | 4.20 | 3.68 | 14.5 | 9.55 | 12.5 | 3.82 | 3.05 | 3.90 | 3.35 | 4.20 | 3.68 |
| Upper 95% CI of the mean | 3.92 | 3.17 | 3.98 | 3.49 | 4.52 | 3.80 | 14.7 | 9.71 | 12.7 | 3.92 | 3.17 | 3.98 | 3.49 | 4.52 | 3.80 | 14.7 | 9.71 | 12.7 | 3.92 | 3.17 | 3.98 | 3.49 | 4.52 | 3.80 |
| 10 PCF | 10 PCF CORTICAL | 20 PCF | 20 PCF CORTICAL | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | CYROTH 0.40 | CYROTH 0.45 | CYROTH T | |||||||||||||
| R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | R3.4 | R3.7 | |
| 25% Percentile | 50.0 | 48.0 | 51.5 | 50.5 | 43.0 | 38.4 | 61.0 | 61.4 | 63.0 | 62.5 | 57.4 | 52.0 | 67.0 | 65.5 | 68.0 | 66.5 | 61.0 | 61.0 | 67.3 | 67.9 | 71.0 | 70.0 | 66.0 | 64.4 |
| Median | 50.0 | 48.5 | 51.8 | 51.0 | 43.5 | 38.8 | 61.5 | 62.0 | 63.5 | 63.0 | 57.5 | 52.3 | 67.8 | 65.5 | 68.0 | 66.5 | 61.5 | 61.5 | 68.3 | 68.5 | 71.5 | 70.5 | 66.5 | 65.0 |
| 75% Percentile | 50.5 | 49.0 | 52.0 | 51.0 | 44.0 | 39.0 | 62.0 | 62.0 | 64.0 | 63.0 | 58.0 | 53.0 | 68.0 | 66.0 | 68.6 | 66.5 | 62.0 | 62.0 | 69.0 | 68.6 | 72.0 | 71.0 | 67.0 | 65.0 |
| Mean | 50.2 | 48.6 | 51.7 | 50.8 | 43.5 | 38.7 | 61.5 | 61.7 | 63.6 | 62.8 | 57.6 | 52.5 | 67.6 | 65.7 | 68.3 | 66.5 | 61.5 | 61.5 | 68.1 | 68.3 | 71.5 | 70.5 | 66.6 | 64.7 |
| Std. Deviation | 0.258 | 0.438 | 0.350 | 0.354 | 0.408 | 0.412 | 0.408 | 0.422 | 0.438 | 0.350 | 0.394 | 0.497 | 0.497 | 0.337 | 0.422 | 0.236 | 0.471 | 0.471 | 0.994 | 0.635 | 0.408 | 0.438 | 0.438 | 0.422 |
| Std. Error of Mean | 0.0816 | 0.138 | 0.111 | 0.112 | 0.129 | 0.130 | 0.129 | 0.133 | 0.138 | 0.111 | 0.125 | 0.157 | 0.157 | 0.107 | 0.133 | 0.0745 | 0.149 | 0.149 | 0.314 | 0.201 | 0.129 | 0.138 | 0.138 | 0.133 |
| Lower 95% CI of mean | 50.0 | 48.2 | 51.4 | 50.5 | 43.2 | 38.4 | 61.2 | 61.4 | 63.2 | 62.5 | 57.3 | 52.1 | 67.2 | 65.4 | 68.0 | 66.3 | 61.2 | 61.2 | 67.4 | 67.8 | 71.2 | 70.1 | 66.2 | 64.4 |
| Upper 95% CI of mean | 50.4 | 48.9 | 52.0 | 51.0 | 43.8 | 38.9 | 61.8 | 62.0 | 63.9 | 63.1 | 57.9 | 52.8 | 67.9 | 65.9 | 68.6 | 66.7 | 61.8 | 61.8 | 68.8 | 68.7 | 71.8 | 70.8 | 66.9 | 65.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tumedei, M.; Di Pietro, N.; Romasco, T.; Piattelli, A.; Comuzzi, L. The Effect of Implant Thread’s Pitch on Primary Stability: An In Vitro Polyurethane Study with Under-Preparation and Low-Speed Drilling. Appl. Sci. 2025, 15, 11245. https://doi.org/10.3390/app152011245
Tumedei M, Di Pietro N, Romasco T, Piattelli A, Comuzzi L. The Effect of Implant Thread’s Pitch on Primary Stability: An In Vitro Polyurethane Study with Under-Preparation and Low-Speed Drilling. Applied Sciences. 2025; 15(20):11245. https://doi.org/10.3390/app152011245
Chicago/Turabian StyleTumedei, Margherita, Natalia Di Pietro, Tea Romasco, Adriano Piattelli, and Luca Comuzzi. 2025. "The Effect of Implant Thread’s Pitch on Primary Stability: An In Vitro Polyurethane Study with Under-Preparation and Low-Speed Drilling" Applied Sciences 15, no. 20: 11245. https://doi.org/10.3390/app152011245
APA StyleTumedei, M., Di Pietro, N., Romasco, T., Piattelli, A., & Comuzzi, L. (2025). The Effect of Implant Thread’s Pitch on Primary Stability: An In Vitro Polyurethane Study with Under-Preparation and Low-Speed Drilling. Applied Sciences, 15(20), 11245. https://doi.org/10.3390/app152011245










