Sleep Matters: Profiling Sleep Patterns to Predict Sports Injuries in Recreational Runners
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design and Procedure
2.2. Sample
2.3. Required Sample Size
2.4. Instruments
2.4.1. Sleep
2.4.2. Sports Injuries
2.4.3. Demographic and Training Variables
2.5. Statistical Analyses
3. Results
3.1. Means, Standard Deviations, and Correlations of Variables
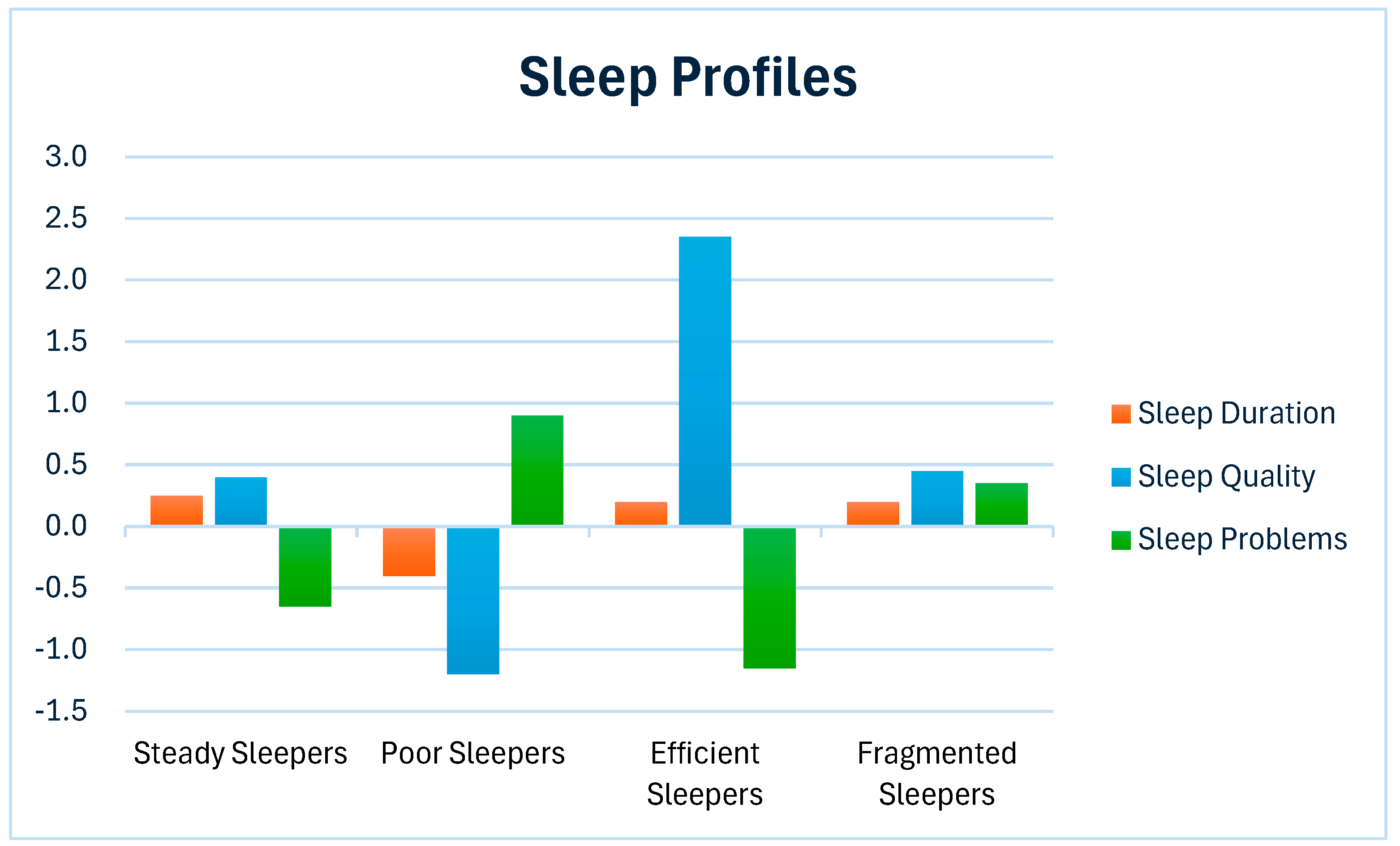
3.2. Latent Risk Profiles for Sleep
3.3. Association Between Sleep Profiles and Sports Injuries
4. Discussion
4.1. Theoretical Implications
4.2. Limitations and Future Research
4.3. Practical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hulteen, R.M.; Smith, J.J.; Morgan, P.J.; Barnett, L.M.; Hallal, P.C.; Colyvas, K.; Lubans, D.R. Global participation in sport and leisure-time physical activities: A systematic review and meta-analysis. Prev. Med. 2017, 95, 14–25. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, G.; Romm, D.; Féré, C.; Guerrero Balarezo, M.L. Gender differences in urban recreational running: A data-driven approach. J. Transp. Geogr. 2025, 124, 104171. [Google Scholar] [CrossRef]
- Wonder. Globally, how Many People Practice Running (as a Sport), and What Is the Global Market Size for This Sport?. 2017. Available online: https://askwonder.com/research/globally-people-practice-running-as-sport-global-market-size-sport-dba00dqvc (accessed on 22 August 2025).
- RIVM/CBS. Gezondheidsenquête/Leefstijlmonitor CBS in Samenwerking met het RIVM [Health Survey/Lifestyle Monitor CBS in Collaboration with RIVM]; Rijksinstituut voor Volksgezondheid en Milieu: Bilthoven, The Netherlands, 2024. [Google Scholar]
- Lee, D.C.; Brellenthin, A.G.; Thompson, P.D.; Sui, X.; Lee, I.M.; Lavie, C.J. Running as a key lifestyle medicine for longevity. Prog. Cardiovasc. Dis. 2017, 60, 45–55. [Google Scholar] [CrossRef]
- Vajda, M.; Oreská, Ľ.; Černáčková, A.; Čupka, M.; Tirpáková, V.; Cvečka, J.; Hamar, D.; Protasi, F.; Šarabon, N.; Zampieri, S.; et al. Aging and possible benefits or negatives of lifelong endurance running: How master male athletes differ from young athletes and elderly sedentary? Int. J. Environ. Res. Public Health 2022, 19, 13184. [Google Scholar] [CrossRef]
- Van Poppel, D.; Scholten-Peeters, G.G.; Van Middelkoop, M.; Verhagen, A.P. Prevalence, incidence and course of lower extremity injuries in runners during a 12-month follow-up period. Scand. J. Med. Sci. Sports 2014, 24, 943–949. [Google Scholar] [CrossRef]
- Van der Does, H.; Stam, C.; Valkenberg, H. Sportblessures in Nederland: Cijfers 2023 [Sports Injuries in The Netherlands: Figures 2023]; VeiligheidNL: Amsterdam, The Netherlands, 2024. [Google Scholar]
- Fredette, A.; Roy, J.S.; Perreault, K.; Dupuis, F.; Napier, C.; Esculier, J.F. The association between running injuries and training parameters: A systematic review. J. Athl. Train. 2022, 57, 650–671. [Google Scholar] [CrossRef]
- Jungmalm, J.; Grau, S.; Desai, P.; Karlsson, J.; Nielsen, R.O. Study protocol of a 52-week Prospective Running Injury study in Gothenburg (SPRING). BMJ Open Sport Exerc. Med. 2018, 4, e000394. [Google Scholar] [CrossRef]
- Ivarsson, A.; Johnson, U.; Andersen, M.B.; Tranaeus, U.; Stenling, A.; Lindwall, M. Psychosocial factors and sport injuries: Meta-analyses for prediction and prevention. Sports Med. 2017, 47, 353–365. [Google Scholar] [CrossRef]
- Jones, C.M.; Griffiths, P.C.; Mellalieu, S.D. Training load and fatigue marker associations with injury and illness: A systematic review of longitudinal studies. Sports Med. 2017, 47, 943–974. [Google Scholar] [CrossRef]
- De Jonge, J.; Balk, Y.A.; Taris, T.W. Mental recovery and running-related injuries in recreational runners: The moderating role of passion for running. Int. J. Environ. Res. Public Health 2020, 17, 1044. [Google Scholar] [CrossRef]
- Kline, C.E.; McConnell, E.J. Sleep and injury prevention in athletes. In Sleep and Sport; Grandner, M.A., Athey, A.B., Eds.; Academic Press: Cambridge, MA, USA, 2024; pp. 183–203. [Google Scholar] [CrossRef]
- Kennedy, K.E.R.; Ghani, S.B.; Mason, B.J.; Hansen, E.T.; Grandner, M.A. Basics of sleep–wake physiology for athletes and sports professionals. In Sleep and Sport; Grandner, M.A., Athey, A.B., Eds.; Academic Press: Cambridge, MA, USA, 2024; pp. 1–27. [Google Scholar] [CrossRef]
- Moore, B.A.; Rouska, A.; Ritland, B.; Brager, A.J.; Mysliwiec, V. Assessment of sleep in athletes. In Sleep and Sport; Grandner, M.A., Athey, A.B., Eds.; Academic Press: Cambridge, MA, USA, 2024; pp. 87–102. [Google Scholar] [CrossRef]
- Huang, K.; Ihm, J. Sleep and injury risk. Curr. Sports Med. Rep. 2021, 20, 286–290. [Google Scholar] [CrossRef]
- Buysse, D.J. Sleep health: Can we define it? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Dauvilliers, Y.; Ferri, R.; Fung, C.; Gozal, D.; et al. National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health 2017, 3, 6–19. [Google Scholar] [CrossRef]
- Charest, J.; Grandner, M.A. Sleep and athletic performance: Impacts on physical performance, mental performance, injury risk and recovery, and mental health: An update. Sleep Med. Clin. 2022, 17, 263–282. [Google Scholar] [CrossRef]
- Gao, B.; Dwivedi, S.; Milewski, M.D.; Cruz, A.I., Jr. Lack of sleep and sports injuries in adolescents: A systematic review and meta-analysis. J. Pediatr. Orthop. 2019, 39, e324–e333. [Google Scholar] [CrossRef]
- Hatia, M.; Loureiro, N.; Ribeiro, J.; Moeda, F.; Melo, M.; Tocha, J.; Schonenberger, A.; Correia, C. A narrative review of the impact of sleep on athletes: Sleep restriction causes and consequences, monitoring, and interventions. Cureus 2024, 16, e76635. [Google Scholar] [CrossRef]
- Dobrosielski, D.A.; Sweeney, L.; Lisman, P.J. The association between poor sleep and the incidence of sport and physical training-related injuries in adult athletic populations: A systematic review. Sports Med. 2021, 51, 777–793. [Google Scholar] [CrossRef]
- Wilkes, J.R.; Walter, A.E.; Chang, A.-M.; Miller, S.J.; Sebastianelli, W.J.; Seidenberg, P.H.; Slobounov, S. Effects of sleep disturbance on functional and physiological outcomes in collegiate athletes: A scoping review. Sleep Med. 2021, 81, 8–19. [Google Scholar] [CrossRef]
- Milewski, M.D.; Skaggs, D.L.; Bishop, G.A.; Pace, J.L.; Ibrahim, D.A.; Wren, T.A.; Barzdukas, A. Chronic lack of sleep is associated with increased sports injuries in adolescent athletes. J. Pediatr. Orthop. 2014, 34, 129–133. [Google Scholar] [CrossRef]
- Von Rosen, P.; Frohm, A.; Kottorp, A.; Fridén, C.; Heijne, A. Too little sleep and an unhealthy diet could increase the risk of sustaining a new injury in adolescent elite athletes. Scand. J. Med. Sci. Sports 2017, 27, 1364–1371. [Google Scholar] [CrossRef]
- Johnston, R.; Cahalan, R.; Bonnett, L.; Maguiree, M.; Glasgow, P.; Madigan, S.; O’Sullivan, K.; Comyns, T. General health complaints and sleep associated with new injury within an endurance sporting population: A prospective study. J. Sci. Med. Sport 2019, 23, 252–257. [Google Scholar] [CrossRef]
- Messman, B.A.; Petrie, K.A.; Moore, E.W.G.; Petrie, T.A. Sleep disturbances and risk of sports injury among collegiate student-athletes. Clin. J. Sport Med. 2025, 35, e54–e60. [Google Scholar] [CrossRef]
- Van Iperen, L.P. Psychological Predictors of Recreational Runners’ Health: Self-Regulatory Processes and Running-Related Injuries, Fatigue, and Vigor. Ph.D. Thesis, Eindhoven University of Technology, Eindhoven, The Netherlands, 2022. [Google Scholar]
- Van Poppel, D.; De Koning, J.; Verhagen, A.P.; Scholten-Peeters, G.G. Risk factors for lower extremity injuries among half marathon and marathon runners of the Lage Landen Marathon Eindhoven 2012: A prospective cohort study in the Netherlands. Scand. J. Med. Sci. Sports 2016, 26, 226–234. [Google Scholar] [CrossRef]
- Ferguson, S.L.; G. Moore, E.W.; Hull, D.M. Finding latent groups in observed data: A primer on latent profile analysis in Mplus for applied researchers. Int. J. Behav. Dev. 2020, 44, 458–468. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum: Mahwah, NJ, USA, 1988. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Ouality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Driller, M.W.; Mah, C.D.; Halson, S.L. Development of the athlete sleep behavior questionnaire: A tool for identifying maladaptive sleep practices in elite athletes. Sleep Sci. 2018, 11, 37–44. [Google Scholar] [CrossRef]
- Kline, C. Sleep duration. In Encyclopedia of Beshavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1808–1810. [Google Scholar] [CrossRef]
- Snyder, E.; Cai, B.; DeMuro, C.; Morrison, M.F.; Ball, W. A new single-item sleep quality scale: Results of psychometric evaluation in patients with chronic primary insomnia and depression. J. Clin. Sleep Med. 2018, 14, 1849–1857. [Google Scholar] [CrossRef]
- Appels, A.; Höppener, P.; Mulder, P.A. A questionnaire to assess premonitory symptoms of myocardial infarction. Int. J. Cardiol. 1987, 17, 15–24. [Google Scholar] [CrossRef]
- McDonald, R.P. Test Theory: A Unified treatment; Lawrence Erlbaum: Mahwah, NJ, USA, 1999. [Google Scholar]
- Bahr, R.; Engebretsen, L.; Laprade, R.; McCrory, P.; Meeuwisse, W. (Eds.) The IOC Manual of Sports Injuries: An Illustrated Guide to the Management of Injuries in Physical Activity; John Wiley & Sons: Chichester, UK, 2012. [Google Scholar]
- Yamato, T.P.; Saragiotto, B.T.; Lopes, A.D. A consensus definition of running-related injury in recreational runners: A modified Delphi approach. J. Orthop. Sports Phys. Ther. 2015, 45, 375–380. [Google Scholar] [CrossRef]
- Smits, D.-W.; Backx, F.; Van der Worp, H.; Van Middelkoop, M.; Hartgens, F.; Verhagen, E.; Kluitenberg, B.; Huisstede, B. Validity of injury self-reports by novice runners: Comparison with reports by sports medicine physicians. Res. Sports Med. 2019, 27, 72–87. [Google Scholar] [CrossRef]
- Van Poppel, D.; Van der Worp, M.; Slabbekoorn, A.; Van den Heuvel, S.S.P.; Van Middelkoop, M.; Koes, B.W.; Verhagen, A.P.; Scholten-Peeters, G.G.M. Risk factors for overuse injuries in short- and long-distance running: A systematic review. J. Sport Health Sci. 2021, 10, 14–28. [Google Scholar] [CrossRef]
- Walsh, N.P.; Halson, S.L.; Sargent, C.; Roach, G.D.; Nédélec, M.; Gupta, L.; Leeder, J.; Fullagar, H.H.; Coutts, A.J.; Edwards, B.J.; et al. Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. Br. J. Sports Med. 2021, 55, 356–368. [Google Scholar] [CrossRef]
- Rosenberg, J.M.; Beymer, P.N.; Anderson, D.J.; Van Lissa, C.J.; Schmidt, J.A. tidyLPA: An R package to easily carry out latent profile analysis (LPA) using open-source or commercial software. J. Open Source Softw. 2018, 3, 978. [Google Scholar] [CrossRef]
- Bauer, J. A primer to latent profile and latent class analysis. In Methods for Researching Professional Learning and Development: Challenges, Applications and Empirical Illustrations; Goller, M., Kyndt, E., Paloniemi, S., Damşa, C., Eds.; Springer: Cham, Switzerland, 2022; Volume 33, pp. 243–268. [Google Scholar] [CrossRef]
- Nylund-Gibson, K.; Choi, A.Y. Ten frequently asked questions about latent class analysis. Transl. Issues Psychol. Sci. 2018, 4, 440–461. [Google Scholar] [CrossRef]
- Ogunleye, L.I.; Oyejola, B.A.; Obisesan, K.O. Comparison of some common tests for normality. Int. J. Probab. Stat. 2018, 7, 130–137. [Google Scholar] [CrossRef]
- Leckey, C.; Van Dyk, N.; Doherty, C.; Lawlor, A.; Delahunt, E. Machine learning approaches to injury risk prediction in sport: A scoping review with evidence synthesis. Br. J. Sports Med. 2025, 59, 491–500. [Google Scholar] [CrossRef]
- Ruddy, J.D.; Cormack, S.J.; Whiteley, R.; Williams, M.D.; Timmins, R.G.; Opar, D.A. Modeling the risk of team sport injuries: A narrative review of different statistical approaches. Front. Physiol. 2019, 10, 829. [Google Scholar] [CrossRef]
- Conte, F.; Cerasuolo, M.; Fusco, G.; Giganti, F.; Inserra, I.; Malloggi, S.; Di Iorio, I.; Ficca, G. Sleep continuity, stability and organization in good and bad sleepers. J. Health Psychol. 2021, 26, 2131–2142. [Google Scholar] [CrossRef]
- Knufinke, M.; Nieuwenhuys, A.; Geurts, S.A.E.; Coenen, A.M.L.; Kompier, M.A.J. Self-reported sleep quantity, quality and sleep hygiene in elite athletes. J. Sleep Res. 2018, 27, 78–85. [Google Scholar] [CrossRef]
- Ramlee, F.; Sanborn, A.N.; Tang, N.K.Y. What sways people’s judgment of sleep quality? A quantitative choice-making study with good and poor sleepers. Sleep 2017, 40, zsx091. [Google Scholar] [CrossRef]
- Dong, Q.; Gentry, N.W.; McMahon, T.; Yamazaki, M.; Benitez-Rivera, L.; Wang, T.; Gan, L.; Ptáček, L.J.; Fu, Y.-H. Familial natural short sleep mutations reduce Alzheimer pathology in mice. iScience 2022, 25, 103964. [Google Scholar] [CrossRef]
- Santos, M.; Gabani, F.L.; De Andrade, S.M.; Bizzozero-Peroni, B.; Martínez-Vizcaíno, V.; González, A.D.; Eumann Mesas, A. The bidirectional association between chronic musculoskeletal pain and sleep-related problems: A systematic review and meta-analysis. Rheumatology 2023, 62, 2951–2962. [Google Scholar] [CrossRef]
- Engert, L.C.; Besedovsky, L. Sleep and inflammation: A bidirectional relationship. Somnologie 2025, 29, 3–9. [Google Scholar] [CrossRef]
- Cunha, L.A.; Costa, J.A.; Marques, E.A.; Brito, J.; Lastella, M.; Figueiredo, P. The impact of sleep interventions on athletic performance: A systematic review. Sports Med. Open 2023, 9, 58. [Google Scholar] [CrossRef]
- Lastella, M.; Vitale, J.A.; Halson, S.L.; Vincent, G.E. Strategic napping. In Sleep and Sport; Grandner, M.A., Athey, A.B., Eds.; Academic Press: Cambridge, MA, USA, 2024; pp. 225–231. [Google Scholar] [CrossRef]
- Romdhani, M.; Souissi, N.; Chaabouni, Y.; Mahdouani, K.; Driss, T.; Chamari, K.; Hammouda, O. Improved physical performance and decreased muscular and oxidative damage with postlunch napping after partial sleep deprivation in athletes. Int. J. Sports Physiol. Perform. 2020, 15, 874–883. [Google Scholar] [CrossRef]
- St-Onge, M.P.; Mikic, A.; Pietrolungo, C.E. Effects of diet on sleep quality. Adv. Nutr. 2016, 7, 938–949. [Google Scholar] [CrossRef]
- Colrain, I.M.; Nicholas, C.L.; Baker, F.C. Alcohol and the sleeping brain. Handb. Clin. Neurol. 2014, 125, 415–431. [Google Scholar] [CrossRef]
| Variables | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender # | 0.43 | 0.50 | ||||||||
| 2. Age | 44.66 | 11.74 | −0.23 ** | |||||||
| 3. Body Mass Index | 22.83 | 2.53 | −0.23 ** | 0.06 | ||||||
| 4. Body Height | 177.09 | 9.16 | −0.66 ** | 0.02 | 0.09 | |||||
| 5. Running Experience | 11.70 | 10.54 | −0.13 ** | 0.51 ** | −0.02 | 0.01 | ||||
| 6. Sleep Duration | 7.30 | 0.85 | 0.12 * | −0.19 ** | −0.16 ** | −0.04 | −0.01 | |||
| 7. Sleep Quality | 3.64 | 0.74 | −0.14 ** | 0.02 | 0.01 | 0.07 | 0.15 ** | 0.29 ** | ||
| 8. Sleep Problems | 1.60 | 0.51 | 0.17 ** | −0.01 | −0.03 | −0.15 ** | −0.10 * | −0.27 ** | −0.70 ** | |
| 9. Sports Injuries # | 0.60 | 0.49 | −0.05 | 0.02 | 0.11 * | −0.03 | −0.05 | −0.02 | −0.10 * | 0.10 * |
| LPA Profiles | BIC | SABIC | AIC | Entropy |
|---|---|---|---|---|
| 1 | 3373 | 3344 | 3336 | 1.00 |
| 2 | 3364 | 3323 | 3312 | 0.66 |
| 3 | 3388 | 3335 | 3319 | 0.38 |
| 4 | 2965 | 2899 | 2881 | 0.85 |
| 5 | 2990 | 2911 | 2889 | 0.70 |
| 6 | 3014 | 2922 | 2897 | 0.64 |
| Variables | Steady Sleepers | Poor Sleepers | Efficient Sleepers | Fragmented Sleepers | Group Differences |
|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | F (3,422) | |
| Gender # | 0.38 (0.49) | 0.53 (0.50) | 0.26 (0.44) | 0.43 (0.50) | 4.11 ** |
| Age | 43.78 (12.23) | 44.78 (10.54) | 49.80 (12.41) | 43.97 (12.63) | 2.69 * |
| Body Mass Index | 22.97 (2.59) | 22.85 (2.49) | 22.52 (2.20) | 22.14 (2.67) | 1.12 |
| Body Height | 177.83 (9.30) | 176.18 (9.00) | 177.17 (9.20) | 176.80 (8.99) | 0.98 |
| Running Experience | 11.20 (10.15) | 10.74 (10.06) | 18.71 (12.93) | 11.93 (10.01) | 5.96 *** |
| Sports Injuries | ||||
|---|---|---|---|---|
| b | SE | OR (95% CI) | Injury Probability | |
| Control Variables | ||||
| Gender | 0.49 | 0.30 | 1.63 (0.91–2.92) | |
| Age | 0.00 | 0.01 | 1.00 (0.98–1.02) | |
| Body Mass Index | 0.08 | 0.04 | 1.08 (1.00–1.18) | |
| Body Height | −0.02 | 0.02 | 0.98 (0.95–1.01) | |
| Running Experience | −0.01 | 0.01 | 0.99 (0.97–1.01) | |
| Predictor Variables | ||||
| Steady Sleepers | 1.00 | 55% | ||
| Poor Sleepers | 0.58 ** | 0.23 | 1.78 (1.14–2.78) | 68% |
| Efficient Sleepers | 0.28 | 0.39 | 1.32 (0.62–2.81) | 61% |
| Fragmented Sleepers | 0.17 | 0.40 | 1.18 (0.54–2.60) | 59% |
| Omnibus Model Test | Χ2(8) = 16.03, p = 0.04 | |||
| Nagelkerke R2 | 5% | |||
| Classification Table (Accuracy) | 60% | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Jonge, J.; Taris, T.W. Sleep Matters: Profiling Sleep Patterns to Predict Sports Injuries in Recreational Runners. Appl. Sci. 2025, 15, 10814. https://doi.org/10.3390/app151910814
de Jonge J, Taris TW. Sleep Matters: Profiling Sleep Patterns to Predict Sports Injuries in Recreational Runners. Applied Sciences. 2025; 15(19):10814. https://doi.org/10.3390/app151910814
Chicago/Turabian Stylede Jonge, Jan, and Toon W. Taris. 2025. "Sleep Matters: Profiling Sleep Patterns to Predict Sports Injuries in Recreational Runners" Applied Sciences 15, no. 19: 10814. https://doi.org/10.3390/app151910814
APA Stylede Jonge, J., & Taris, T. W. (2025). Sleep Matters: Profiling Sleep Patterns to Predict Sports Injuries in Recreational Runners. Applied Sciences, 15(19), 10814. https://doi.org/10.3390/app151910814








