4.1. Specific Case Discussion
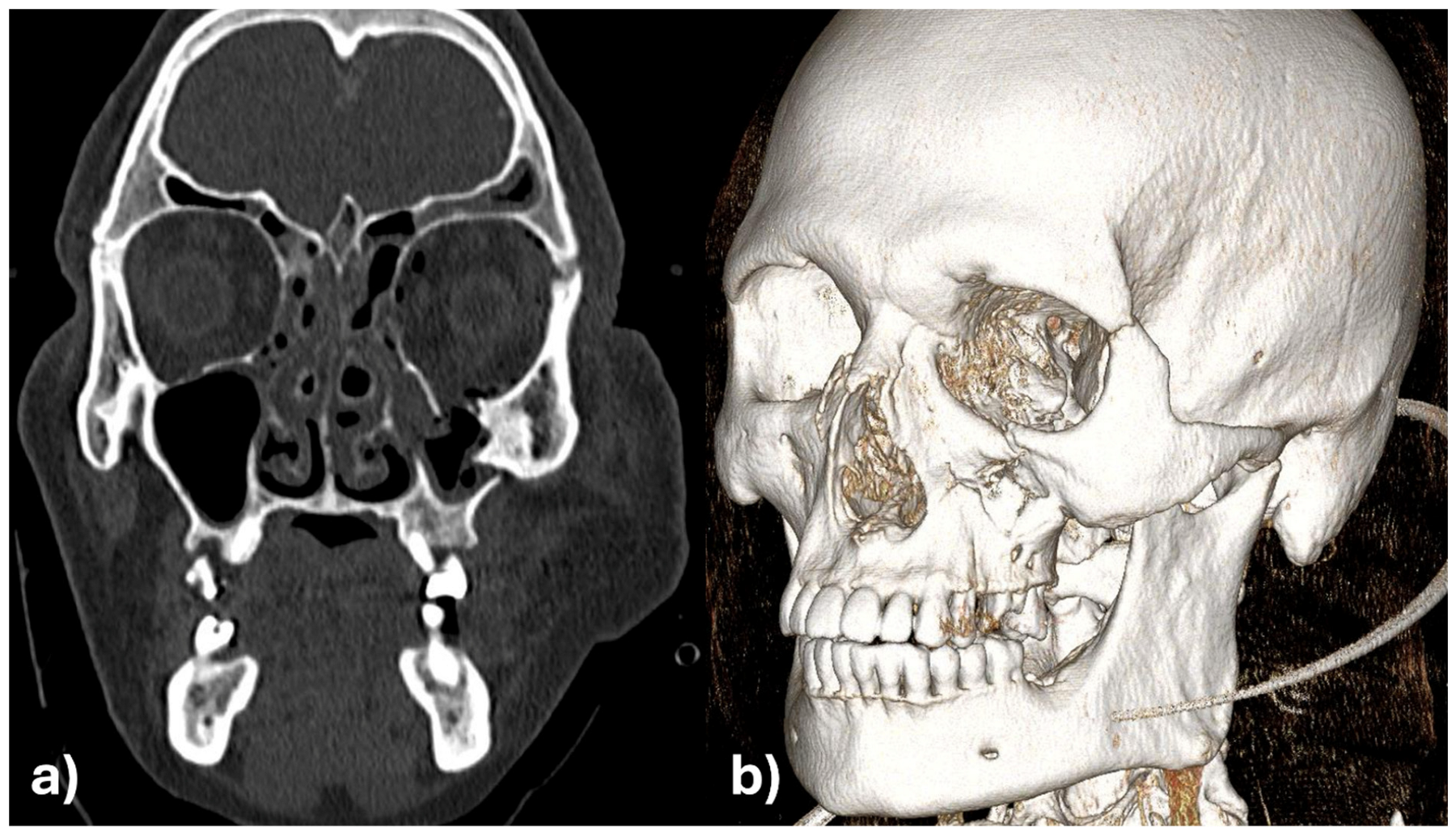
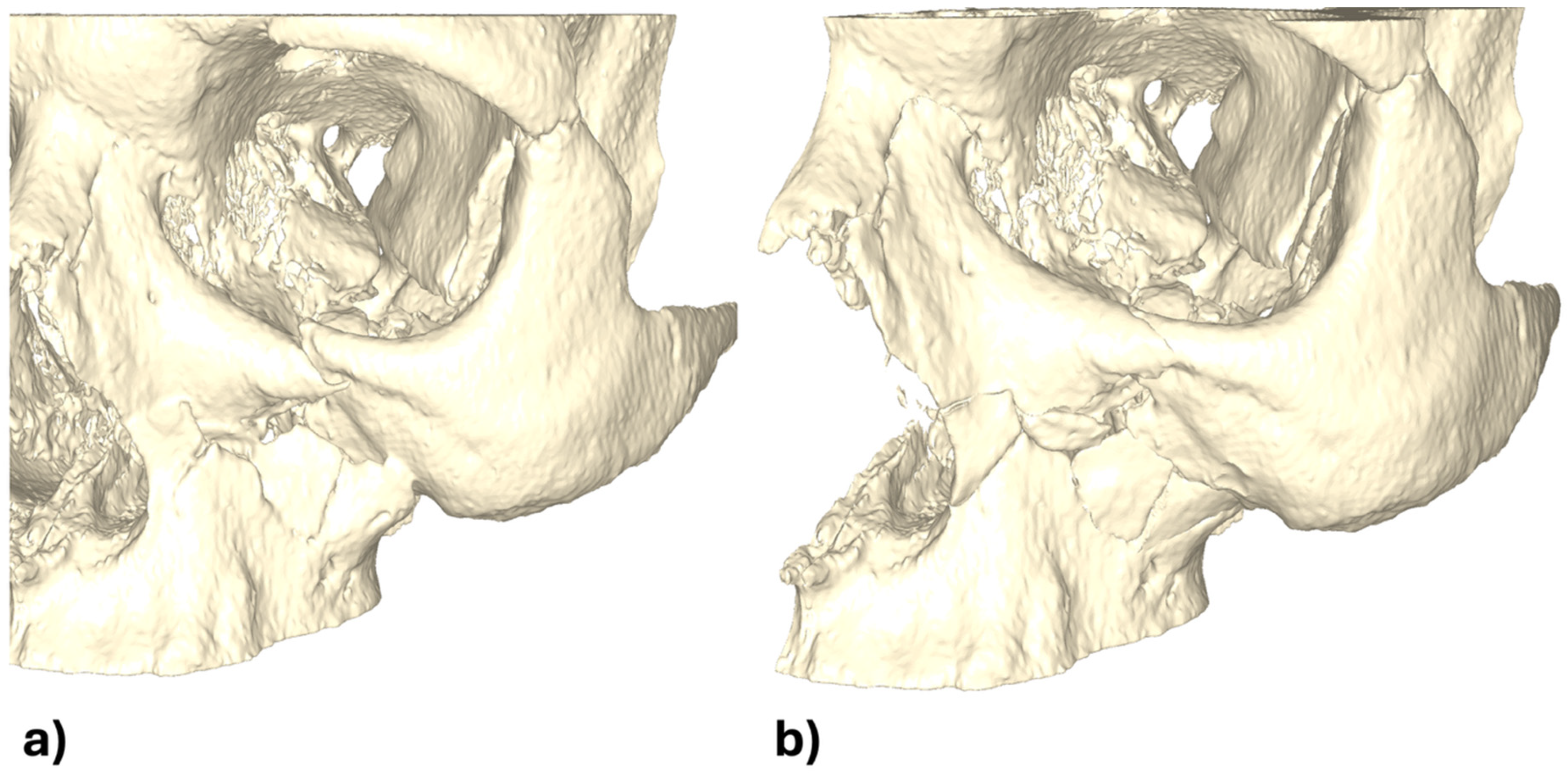
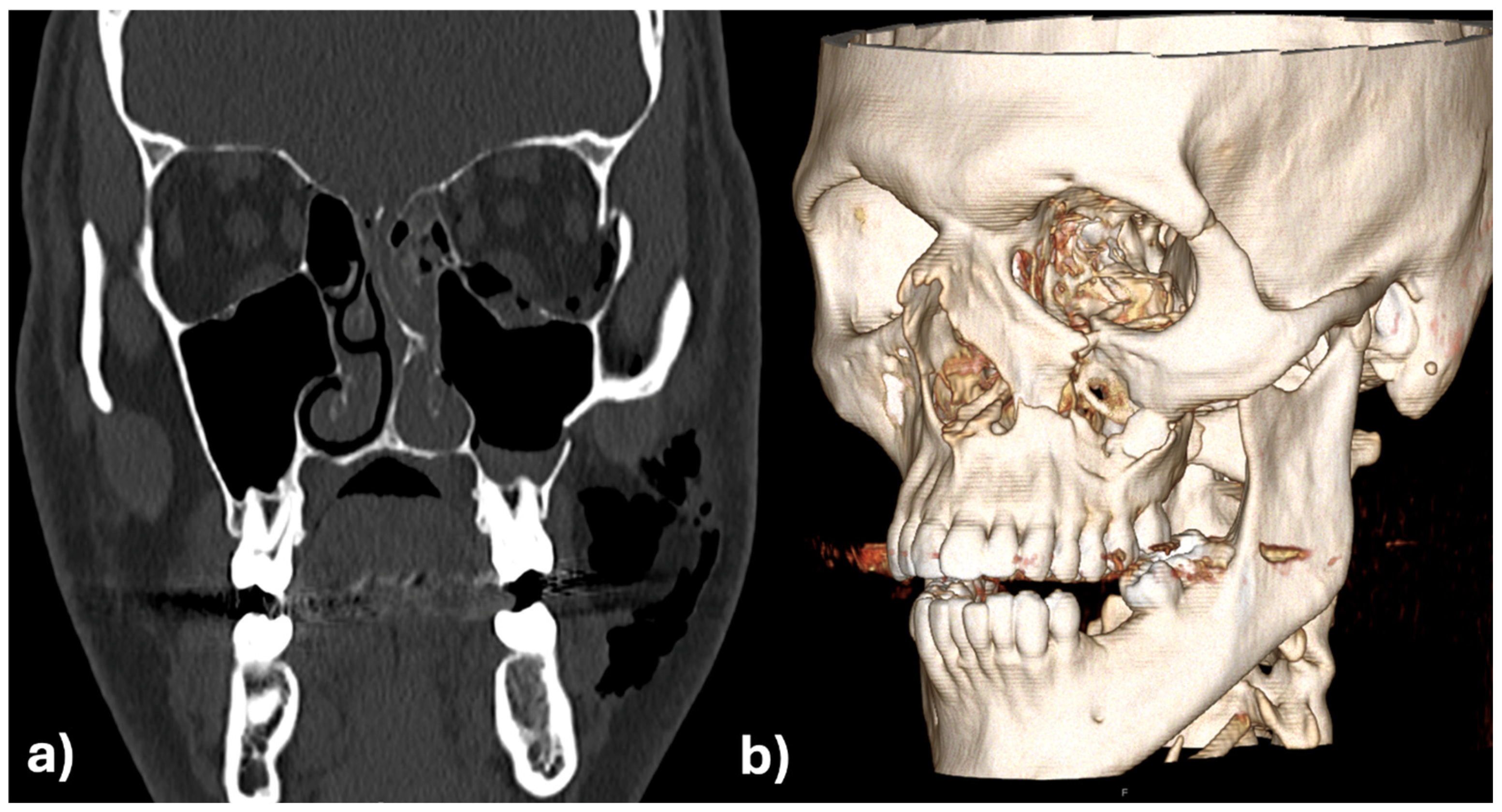
These two cases provides promising early evidence in the evolving application of CAD/CAM technology for the primary treatment of maxillofacial fractures. Specifically, they demonstrate the technical feasibility and clinical utility of employing patient-specific surgical guides and implants for midfacial reconstruction, with a particular emphasis on the orbital and zygomatic regions.
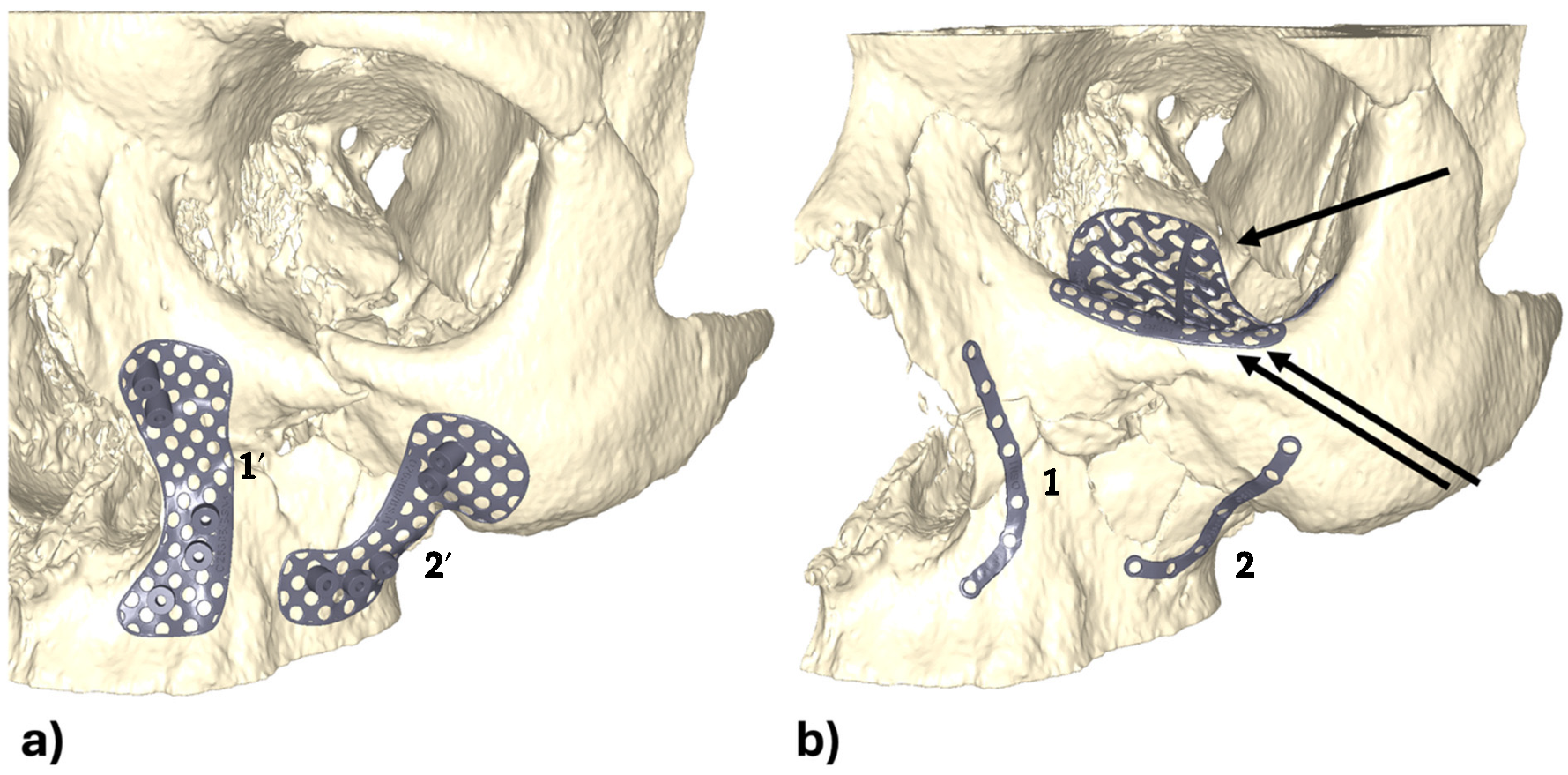
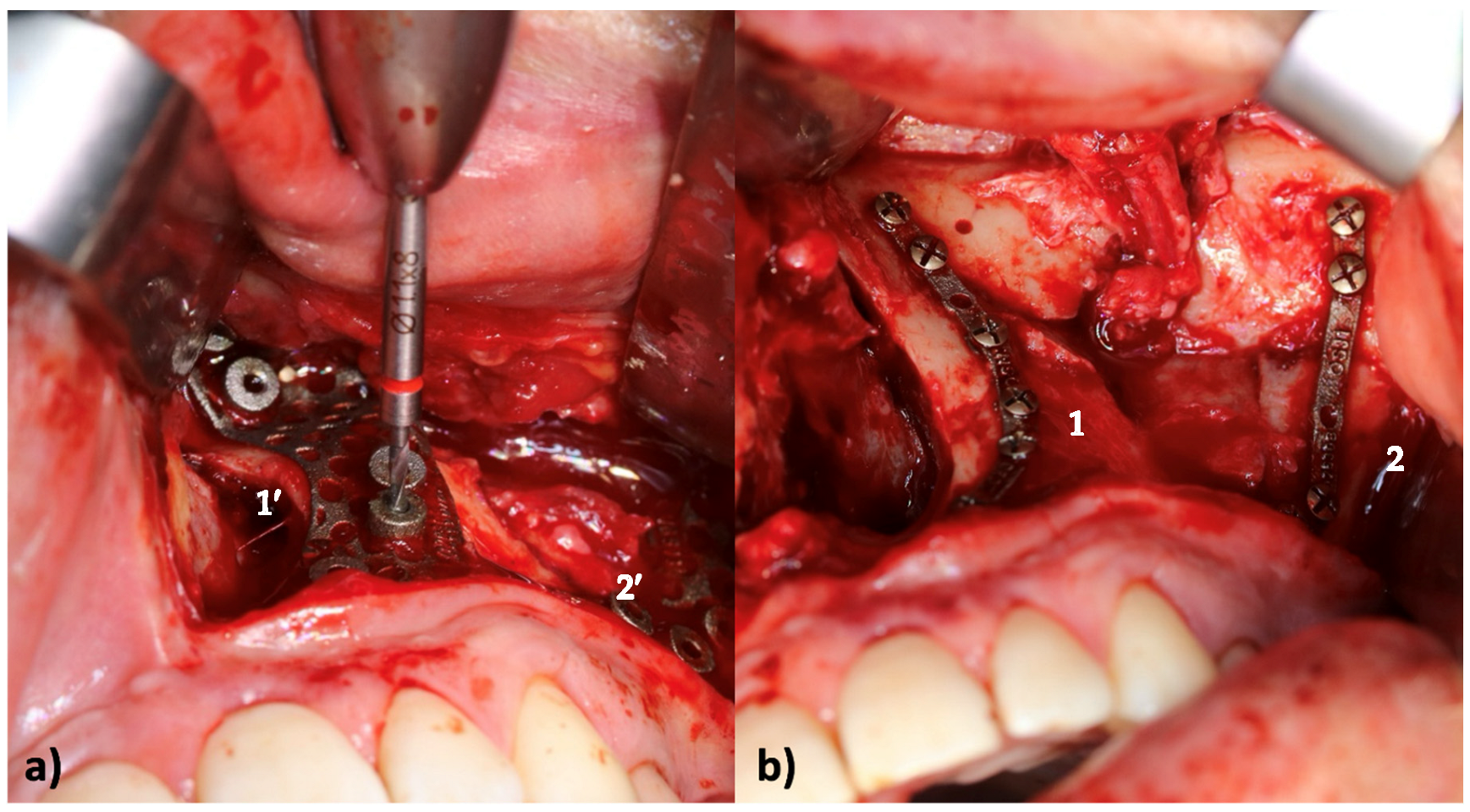
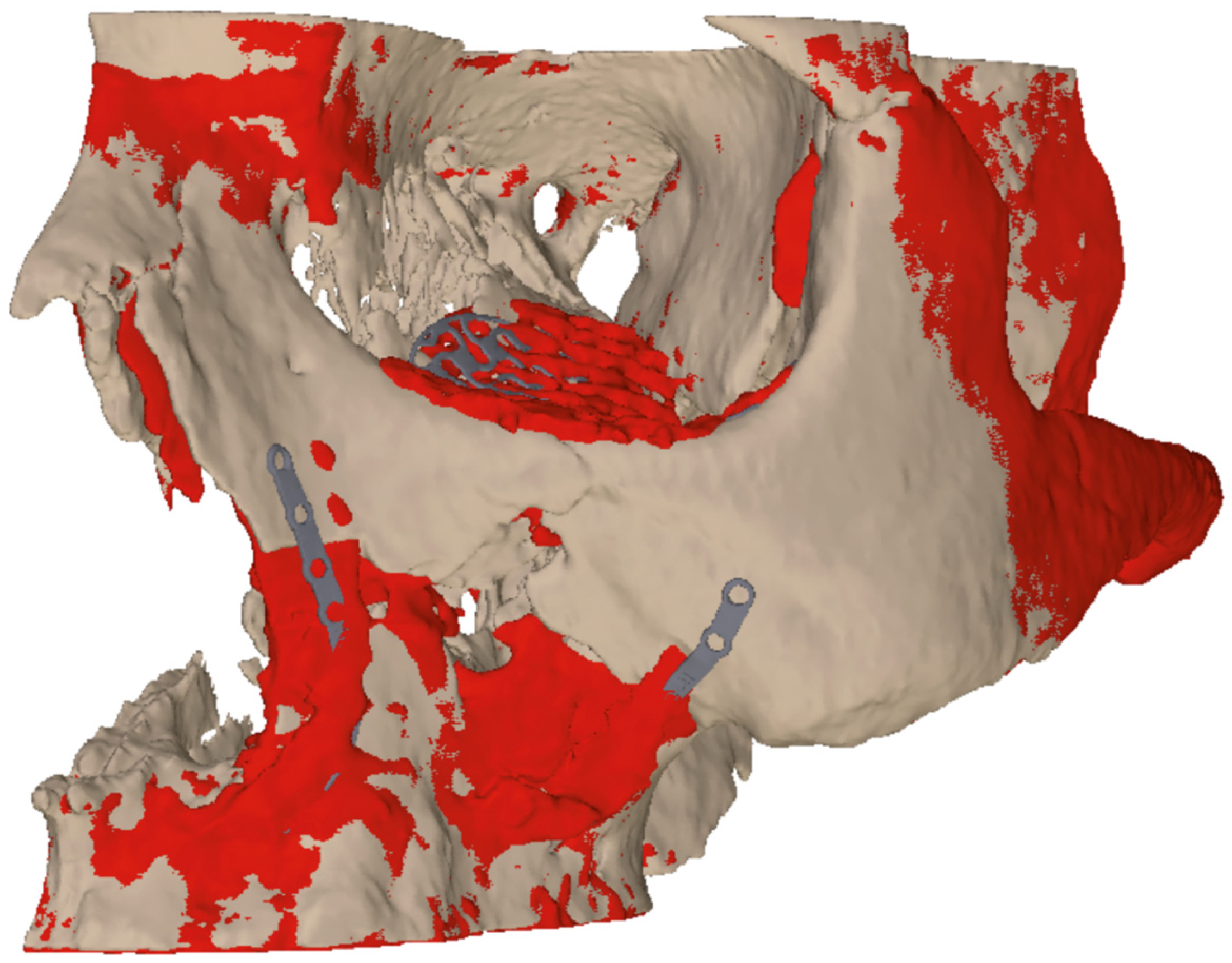
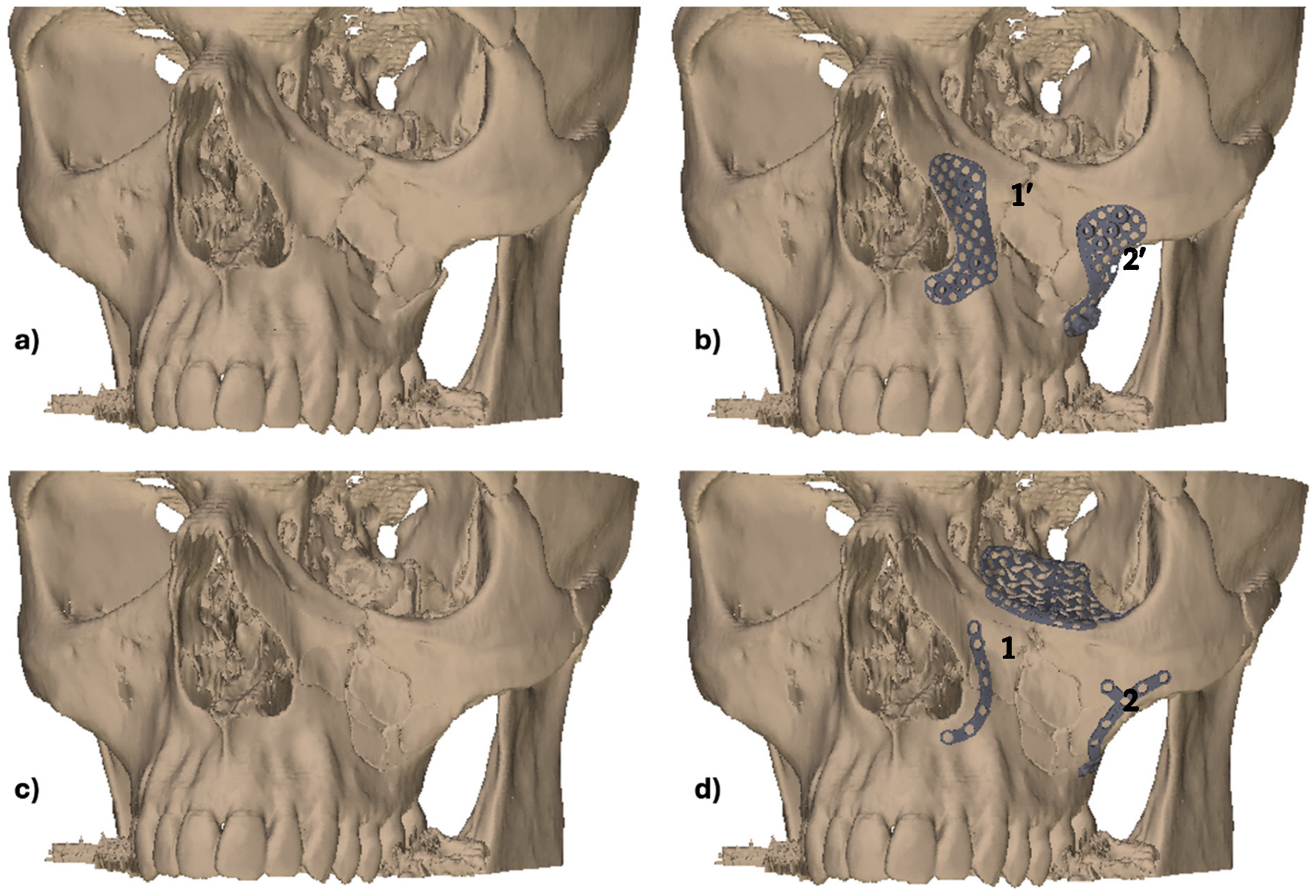
In the initial case, the intraoperative fit of the CAD/CAM-designed guides and implants in the midface was found to be optimal. The additional orbital rim implant enabled highly accurate reconstruction of the orbital frame, and the “one-position-fits-only” design of the orbital implant facilitated precise placement on the dorsal aspect of the orbital rim plate. The precise alignment between the two implants was found to be a distinct advantage in achieving an anatomically correct and functionally stable reconstruction.
However, the case also highlighted challenges in the early stages of implementation. The close and repeated collaborations between surgeons and medical engineers were necessary but difficult to coordinate due to time constraints. Although orbital reconstruction has now become relatively routine for experienced engineers, the importance of collaborative planning remains paramount, particularly in complex trauma cases. In this instance, the development and revision of multiple design proposals was necessary due to unanticipated intraoperative challenges. Notably, the enoral approach was insufficiently considered in the design phase, resulting in technical difficulties during the insertion of drills into the guide, especially for cranial drill holes in the zygomatic and paranasal areas. Furthermore, the drill sleeves exhibited inadequate continuity for the corresponding drill, resulting in minor titanium abrasion. Additionally, the penetrability of the implants for osteosynthesis screws necessitated intraoperative adjustments.
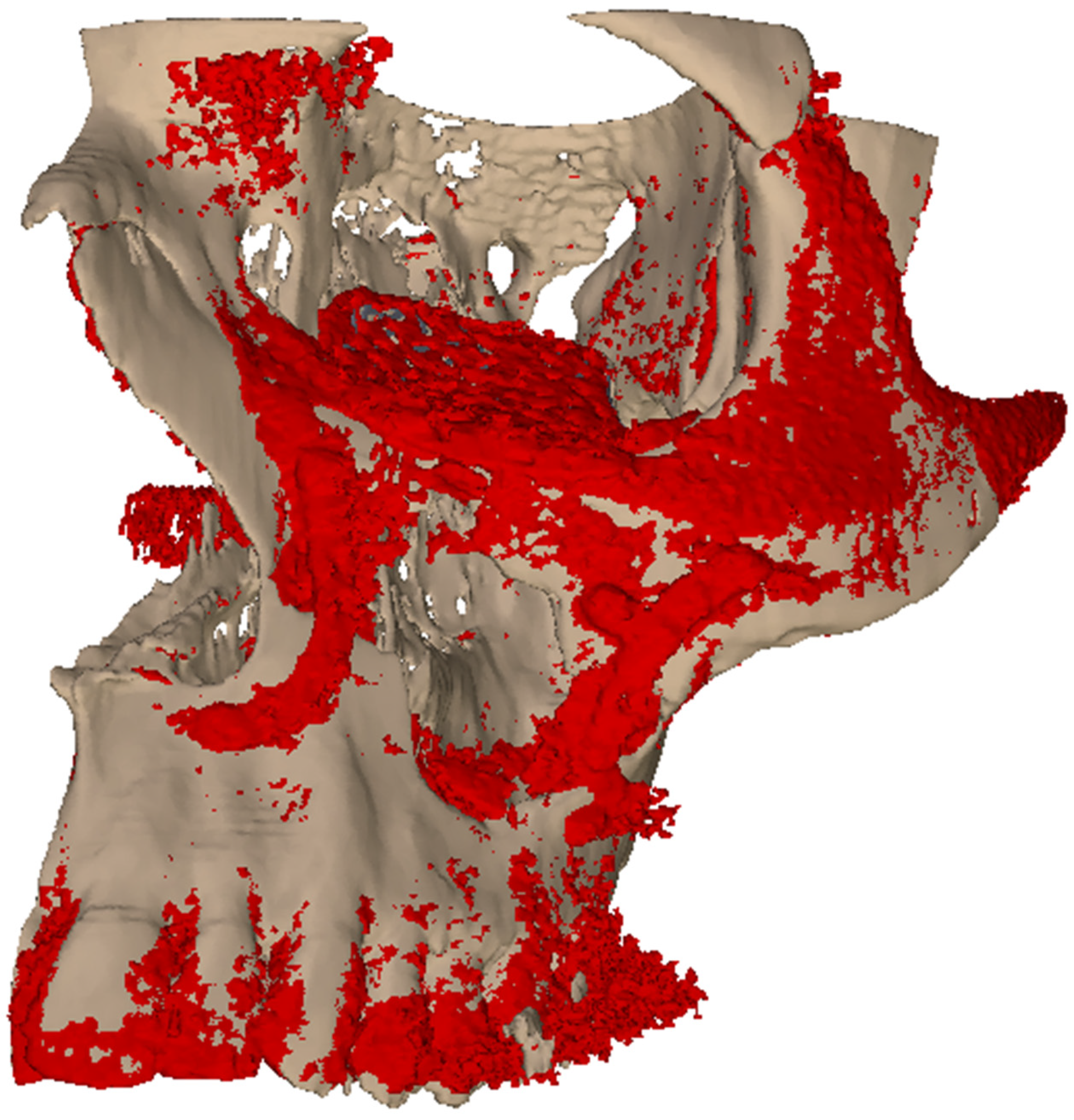
The insights gained from this inaugural experience served as a foundation for the subsequent approach to the second case. The insights and feedback from prior planning processes were leveraged to significantly streamline digital bone repositioning and implant design. The open and constructive collaboration between the surgical and engineering teams resulted in rapid production, with surgical guides and implants being delivered within just five days. Intraoperatively, the components could be applied without complications, and the planned repositioning was achieved with a precise implant fit. In this instance, the drilling templates and screw holes demonstrated optimal consistency, reflecting tangible improvements in design and manufacturing workflows.
However, a high degree of mobility in the zygomatic body during the surgical approach and fracture exposure did pose some challenges to the positioning of the surgical guides, particularly in comparison to more stable areas such as the paranasal region. This finding serves to underscore the expectation that in cases involving smaller or more mobile bone fragments, deviations from the planned position may be more likely—an issue that is less prominent in orthognathic procedures on non-osteotomized jaws. Notwithstanding these challenges, the insertion and pre-drilling procedures were successfully executed. The orbital rim plate was instrumental in correcting minor inaccuracies in the orbital frame region. Of course, it would be possible to combine the infraorbital plate with orbital implant. However, from our perspective we believe that it is beneficial to split this off for higher precision of the entire reconstruction.
The analysis presented here demonstrates the potential of CAD/CAM technology to achieve reliable, anatomically accurate, and functional reconstructions of complex midfacial fractures. Of particular note is the necessity of effective and timely interdisciplinary communication. A well-coordinated team approach, particularly during the design and planning phase, can prevent time-consuming revisions and optimize surgical outcomes. The sharing of original drills and screws with the implant manufacturer for inspection and certification was also a key step toward seamless integration of surgical requirements into the production process.
The ongoing refinement of CAD/CAM workflows, informed by real-world clinical experience, is resulting in reduced planning and production times, as well as enhanced surgical outcomes. Consequently, the method is gaining traction in clinical practice, with additional cases already in preparation. These developments affirm the value of digital, patient-specific reconstruction in modern maxillofacial trauma care.
4.2. General Discussion
The integration of CAD/CAM technology in primary midfacial reconstruction represents a beneficial advance in the field of oral and maxillofacial surgery, particularly regarding the precise repositioning of fractures. Conventional techniques frequently necessitate the surgeon’s intraoperative assessment and manual realignment of fractures, a process that is not only time-consuming but also susceptible to inaccuracies. Such inaccuracies can result in complications, including malocclusion, enophthalmos and facial asymmetry, which can necessitate complicated revision procedures and re-osteotomies. In contrast, our approach utilizing CAD/CAM technology permits meticulous preoperative planning, thereby facilitating the creation of surgical guides that enable the precise and reproducible repositioning of fractures, which could contribute to future improvements in this field.
Perhaps the most transformative aspect of our method is the ability to digitally reposition fractures before the surgical procedure commences. This digital process entails the creation of a virtual model of the patient’s skull, thereby enabling the surgeon to manipulate the fractured segments to their optimal anatomical positions. Once the optimal alignment is determined, CAD/CAM technology is used to create customized surgical guides that are customized to the patient’s particular anatomy. These guides are produced with such precision that they guarantee the bones can be repositioned during surgery in a manner that aligns them with the configuration depicted in the digital model. This “one position fits only” design represents a significant advancement over traditional methods, where the final positioning frequently relies on the surgeon’s visual and tactile assessment during the operation.
This digital repositioning offers notable advantages over conventional care. Firstly, it ensures that the fractures are aligned in the most anatomically correct position, thereby reducing the risk of post-surgical complications. The precision of the CAD/CAM surgical guides eliminates the need for guesswork associated with traditional fracture fixation, thereby ensuring more consistent and reliable outcomes. Furthermore, this approach has the potential to significantly reduce the surgical time. In the standard care approach, a significant portion of the operative time is dedicated to achieving proper alignment of the fracture segments, which often necessitates multiple adjustments. The pre-planned digital alignment enables more expeditious and efficacious surgical procedures, as the surgeon can promptly position the fracture segments using the guides, obviating the necessity for extensive intraoperative corrections.
Moreover, the enhanced precision afforded by the CAD/CAM guides diminishes the probability of requiring subsequent corrective surgeries. In the context of conventional methodologies, it is not uncommon for postoperative imaging to reveal suboptimal fracture alignment, thereby necessitating further interventions. The capacity of our method to achieve the correct alignment on the first attempt serves to minimize these risks, thereby facilitating a more expedient recovery process and enhancing long-term outcomes for patients. The combination with intraoperative 3D imaging continues to be of particular value here.
The true landmark in this field is the way CAD/CAM guides transform the approach of surgeons to fracture repositioning. In contrast to the reliance on intraoperative adjustments, which can be imprecise and subjective, our method provides a pre-determined, scientifically grounded approach to fracture alignment. This results in not only improved functional and aesthetic outcomes but also a more predictable and streamlined surgical process.
The present report is limited by the very small sample size of only two cases, which restricts the strength of the conclusions that can be drawn. Although both cases demonstrated precise anatomical restoration and technical feasibility, the evidence level remains low, and results cannot be generalized to the wider patient population. Further studies including larger case series and ideally controlled trials are necessary to assess reproducibility, cost-effectiveness, and long-term outcomes. Until such evidence is available, the presented workflow should be regarded as a proof-of-concept approach rather than a broadly established clinical standard.
The primary objective of this feasibility study was to assess the outcomes, which was primarily achieved through a descriptive analysis. The focus of this analysis was on intraoperative handling, implant fit, and congruence between the virtual plan and postoperative imaging. The utilisation of standardised postoperative functional or aesthetic measures (e.g., diplopia testing, exophthalmometry, or validated patient-reported outcome questionnaires) was not systematically recorded. Nevertheless, both patients underwent routine follow-up examinations, during which no subjective complaints (e.g., diplopia, sensory disturbances, discomfort) or clinical abnormalities were noted. While this provides preliminary reassurance, the lack of standardised functional and aesthetic outcome measures represents a limitation of the present report. Future studies with larger cohorts should systematically compare this digital workflow to standard approaches in terms of operative time, complication rates, revision surgery, and long-term functional outcomes.
While the feasibility of CAD/CAM-guided fracture management has been demonstrated in the present cases, its widespread implementation in emergency trauma care is still limited by cost and resource availability. The fabrication of patient-specific implants and guides necessitates specialised infrastructure, collaboration with engineering partners, and additional preoperative planning time. The present study has identified a number of factors that are currently resulting in higher treatment costs when compared to conventional methods. Furthermore, these factors may not be available in all trauma centres, particularly in cases of urgent intervention. However, with ongoing improvements in production speed, cost reduction through streamlined workflows, and increasing availability of in-house or regional manufacturing facilities, broader accessibility is expected in the near future.
Further developments may offer more sophisticated and artificial intelligence supported digital planning tools that permit even finer adjustments to the fracture alignment, as well as the integration of real-time feedback during surgery to further enhance precision.