Where You Place, How You Load: A Scoping Review of the Determinants of Orthodontic Mini-Implant Success
Abstract
1. Introduction
2. Methods
2.1. Search Strategy and Eligibility Criteria
2.2. Database Search and Terms
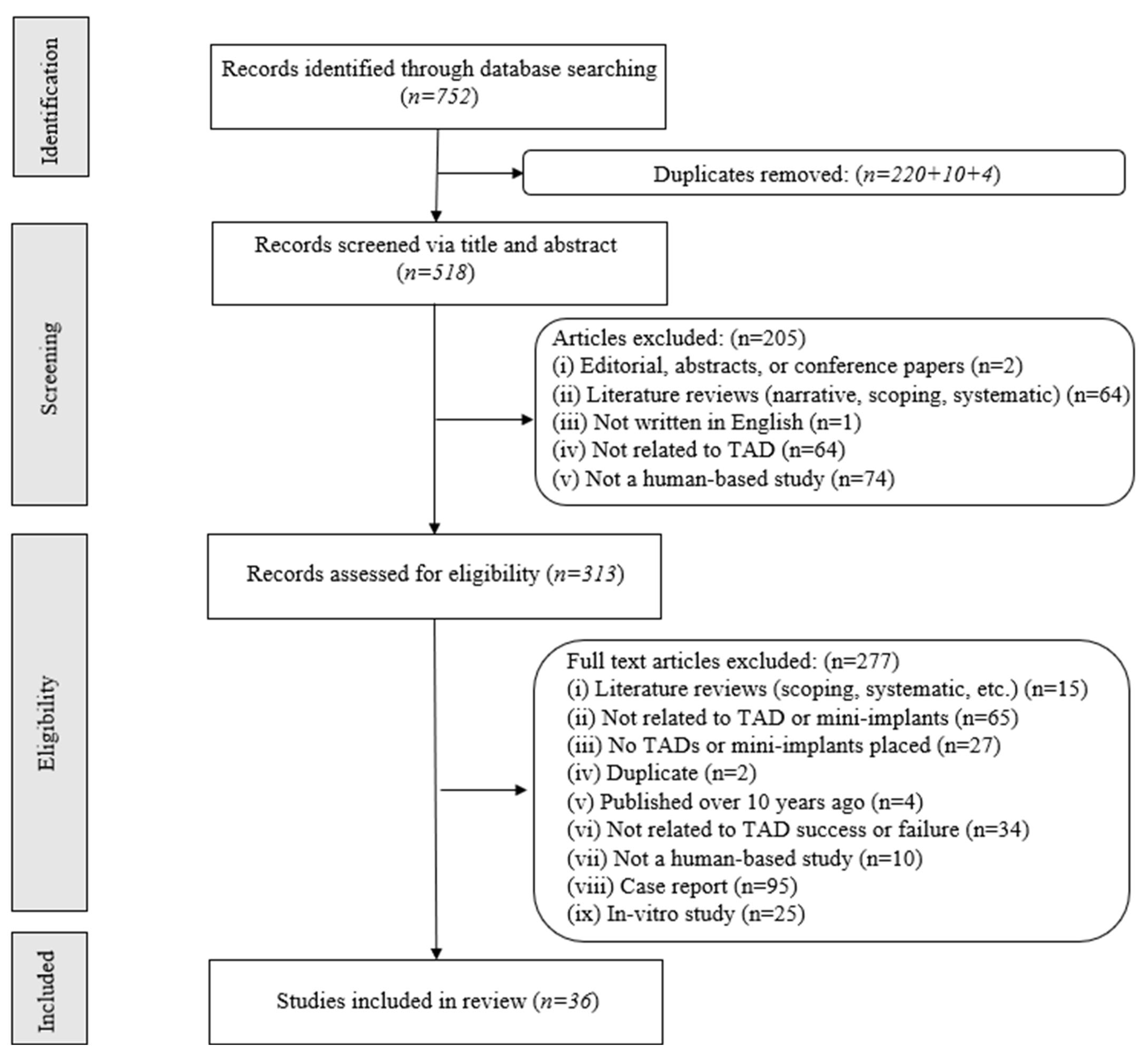
2.3. Selection Process
2.4. Quality Assurance and Synthesis
3. Results
3.1. Article Selection
3.2. Study Designs
3.3. Factors Leading to MI/TAD Success
| Authors | Type of Orthodontic Movement | Placement Location | Success Factors |
|---|---|---|---|
| Abu et al. (2023) [30] | Numerous orthodontic tooth movements | Alveolar Ridge | Mini-implants were more likely to be successful with an increased length. Success rate increased when two mini-implants were splinted together. |
| Ağlarcı et al. (2016) [36] | Protrusion (maxillary & mandibular incisors) and Protraction of maxilla | Between mandibular lateral and canine teeth and maxillary second premolar and first molar. | Poor oral hygiene increased the rate of failure |
| Aly et al. (2018) [35] | Intrusion (molar) Retraction, Distalization (molar) | Maxillary and mandibular arches | The higher age group (>20 years), good oral hygiene, and immediate loading had a higher success rate |
| Arqub et al. (2021) [31] | Distalization, expansion, intrusion, or protraction | palatal mini-implants- paramedian or sutural, anteroposterior location (mesial to canine, canine to the second premolar, or distal to the second premolar) and buccal mini-implants (interradicular, infrazygomatic, or buccal shelf) | Palatal Implants: Lowest survival rate when used for and posterior segment protraction had the highest survival rate. Buccal Implants: Lower survival rate in males and when treating class III malocclusion. Treating class II malocclusion had the highest survival rate. Location—palatal shelf had the highest survival rate and the buccal shelf had the lowest survival rate |
| Azeem et al. (2019) [42] | Numerous orthodontic tooth movements | Maxillary tuberosity | Mini-implants placed by an operator with little experience was more likely to fail |
| Azeem et al. (2019) [29] | Uprighting (molar) | Placed in the buccal retromolar area, at the distobuccal surface of the second molars, between the anterior border of the mandibular ramus and the temporal crest | Mini-implants placed on the right side and when there was inflammation had a higher failure rate |
| Bearn & Alharbi (2015) [28] | Numerous orthodontic tooth movements | Various locations | Mini-implants were more successful when placed in the maxilla compared to the mandible and by clinicians with more experience |
| Bratu et al. (2014) [43] | Numerous orthodontic tooth movements | Various locations | Sandblasting and acid etching increased mini-implant success rate |
| Bungau et al. (2022) [27] | Intrusion (molar & incisor) and uprighting (molar) | Buccal maxillary area, the infrazygomatic region, palatal area, buccal mandibular area and lingual area | Mini-implants placed in the palatal region were more successful than when placed in the buccal mandibular region. The highest rejection rate occurred within the first month of placement. |
| Garg & Gupta (2015) [26] | Retraction (anterior teeth) | Second premolar and first molar (zygomatic buttress) in maxilla and mandible | More mobility observed on the right side than left side and when placed between the second premolar and first molar compared the first premolar and second premolar. Presence of inflammation decreased success. |
| Gurdan & Szalma (2018) [25] | Intrusion, distalization, uprighting | Various locations | Screw mobility was the most common in buccal placement and when used for intrusion. Inflammation due to poor oral hygiene decreased success rate |
| Haddad & Saadeh (2019) [24] | Numerous orthodontic tooth movements | Canines and first premolars, first and second premolars, second premolars and permanent first molars, or between first and second permanent molars | Success rate increased with increasing age, when placed between premolars or premolar and first molar, and with increasing DC distance |
| He et al. (2023) [41] | Distalization | Infrazygomatic crest | Success rate increases with increasing implant height |
| Hourfar et al. (2017) [39] | Protraction (molar) and distalization (molar) | Buccal premolar region on the maxilla and mandible or anterior palate | Patients between 6–20 years of age had a lower failure rate than patients over 30 years old. Individually placed mini-implants had lower success rates than dually placed mini-implants |
| Jia et al. (2018) [23] | Distalization | Infrazygomatic crest | Thickness of the cortical bone increased the success rate and inflammation decreased success |
| Kim et al. (2016) [44] | Numerous orthodontic tooth movements | Buccal alveolar bone in posterior regions | Failure rate can increase with the frequency of mini-implant reinsertions after failure. Sex, age, and arch may have no correlation with primary or recurrent OMI failure. |
| Lai & Chen (2014) [22] | Numerous orthodontic tooth movements | Various locations | Diameter and length, sex, age, and malocclusion type did not show any statistically significant difference in success rates. Success rate was reduced when placed in the jaw or lingually, inflammation, and applying force at two weeks. |
| Melo et al. (2016) [21] | Numerous orthodontic tooth movements | Various locations | No difference in loss of stability with age, sex, craniofacial pattern or smoking habit. Shorter mini-implants were more likely to fail than longer ones and mandibular mini-implants had a lower stability. |
| Migliorati et al. (2016) [20] | Retraction, intrusion, and extrusion | Maxillary and mandibular arches | Mandibular arch was more stable and delayed loading more stable |
| Migliorati et al. (2020) [45] | Distalization, intrusion, extrusion, mesialization | Maxillary and mandibular arches | No significant differences in success among the gender of the patients, age, miniscrew location (maxilla or mandible), miniscrew position (palatal/lingual or vestibular), baseline torque values and groups |
| Moeini et al. (2023) [19] | Retrusion and distalization (molar) | Buccal side of first molars | Higher failure rate in mandible, time of loading had no influence, infection present in failed MI, younger patients had higher probability of failure in the mandible, young females had highest failure rate |
| Mommaerts et al. (2014) [38] | Proclination, intrusion, uprighting molars | Maxillary and mandibular arches | Age, gender, time of loading, and location did not influence failure rate. Mini-implants were more likely to fail in female patients and in younger patients |
| Motoyoshi et al. (2016) [18] | Retraction (anterior teeth) | Maxillary buccal alveolar bone between second pre-molar and first molar | More likely to fail if in contact with the root |
| Nienkemper et al. (2014) [40] | Distalization (molars) | Maxillary and mandibular arches | Longer mini-implants were more likely to not fail |
| Nienkemper et al. (2020) [34] | Sagittal molar movement | Median of anterior palate | Stability decreased with decreased oral health. Sex had no impact on success rate |
| Nienkemper et al. (2020) [17] | Sagittal molar movement | Median of anterior palate | Length of mini-implant, age, sex, vertical bone height did not affect failure rate |
| Ravi et al. (2023) [46] | Retraction (maxillary & mandibular anterior teeth) | Various locations | Surface treatment using sandblasting and acid etching may improve the secondary stability of self-drilling orthodontic mini-implants. |
| Sarul et al. (2022) [33] | Distalization (anterior teeth) | Mandibular buccal shelf | Larger screws had a higher success rate. Inflammation decreased success rate |
| Shaikh et al. (2021) [16] | Distalization (maxillary molars) and intrusion (maxillary anterior teeth) | Between first and second molars | Bone density and volume increase success rate |
| Slabkovskaya et al. (2021) [47] | Intrusion (maxillary molars) | Between first and second molars | Age and gender had no effect on success rate |
| Sreenivasagan et al. (2021) [15] | Numerous orthodontic tooth movements | Anterior interradicular, buccal shelf, infrazygomatic, palatal, midline, posterior maxilla, and posterior mandible | Success rate increased with self-tapping, in maxilla, in the maxilla, and with sandblasting and etching. Poor home care, inflammation, and excessive load decreased success rate. |
| Sreenivasagan et al. (2021) [14] | Numerous orthodontic tooth movements | Anterior interradicular, buccal shelf, infrazygomatic, palatal, midline, posterior maxilla, and posterior mandible | Buccal shelf implants had the highest torque. Failure was due to implant breakage during insertion and soft tissue inflammation |
| Uribe et al. (2015) [13] | Numerous orthodontic tooth movements | Infrazygomatic crest | Age, gender, size of mini-implant, type of movement, oral hygiene, operator experience, and pilot hole was not a predictor of mini-implant success |
| Vicioni-Marques et al. (2022) [32] | Numerous orthodontic tooth movements | Maxillary and mandibular arches | Adequate clinical procedure, precise placement, and lack of inflammation increase success of mini-implant |
| Yao et al. (2015) [37] | Numerous orthodontic tooth movements | Maxillary and mandibular arches | Sex, malocclusion type, bone density, inflammation had no effect on failure. Patients over 35 years and immediate loading were more likely to be successful |
| Yi Lin et al. (2015) [12] | Numerous orthodontic tooth movements | Maxillary and mandibular arches and palate | No patient related factors affected success rate, but the longer mini-screw and average mandibular plane angle patients had higher success rates |
3.4. Type of Orthodontic Movement/ Indications for TADs/Mis
3.5. Host-Related and Biomechanical Moderators
3.6. Outcome Definitions and Follow-Up Heterogeneity
4. Discussion
4.1. Additional Patient and Procedural Considerations
4.2. Limitations
4.3. Implications for Clinical Practice
4.4. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mizrahi, E. The use of miniscrews in orthodontics: A review of selected clinical applications. Prim. Dent. J. 2016, 5, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Leo, M.; Cerroni, L.; Pasquantonio, G.; Condò, S.G.; Condò, R. Temporary anchorage devices (TADs) in orthodontics: Review of the factors that influence the clinical success rate of the mini-implants. Clin. Ther. 2016, 167, e70–e77. [Google Scholar] [CrossRef]
- Umalkar, S.S.; Jadhav, V.V.; Paul, P.; Reche, A. Modern anchorage systems in orthodontics. Cureus 2022, 14, e31476. [Google Scholar] [CrossRef] [PubMed]
- Dalstra, M.; Cattaneo, P.; Melsen, B. Load transfer of miniscrews for orthodontic anchorage. Orthodontics 2004, 1, 53–62. [Google Scholar]
- Creekmore, T.D.; Eklund, M.K. The possibility of skeletal anchorage. J. Clin. Orthod. 1983, 17, 266–269. [Google Scholar]
- Uzuner, F.; Işık Aslan, B. Miniscrew Applications in Orthodontics; InTech: London, UK, 2015. [Google Scholar] [CrossRef]
- Kuroda, S.; Sugawara, Y.; Deguchi, T.; Kyung, H.M.; Takano-Yamamoto, T. Clinical use of miniscrew implants as orthodontic anchorage: Success rates and postoperative discomfort. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 9–15. [Google Scholar] [CrossRef]
- Ahuja, K.P.; Jadhav, V.V.; Paul, P.; John, H.A.; Dakhale, R. Anterior en masse retraction in orthodontics. Cureus 2023, 15, e43194. [Google Scholar] [CrossRef]
- Umeh, O.D.; Offojebe, U.L.; Isiekwe, I.G.; Utomi, I.; daCosta, O. Survival analysis of temporary anchorage devices: A retrospective analysis in a Nigerian orthodontic patient population. J. Orthod. Sci. 2023, 12, 45. [Google Scholar] [CrossRef]
- Veroniki, A.A.; Hutton, B.; Stevens, A.; McKenzie, J.E.; Page, M.J.; Moher, D.; McGowan, J.; Straus, S.E.; Li, T.; Munn, Z.; et al. Update to the PRISMA guidelines for network meta-analyses and scoping reviews and development of guidelines for rapid reviews: A scoping review protocol. JBI Evid. Synth. 2025, 23, 517–526. [Google Scholar] [CrossRef]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Implement. 2021, 19, 3–10. [Google Scholar] [CrossRef]
- Song, Y.L.; Yow, M.; Chew, M.T.; Foong, K.W.C.; Wong, H.C. A study of success rate of miniscrew implants as temporary anchorage devices in Singapore. Int. J. Dent. 2015, 2015, 294670. [Google Scholar] [CrossRef]
- Uribe, F.; Mehr, R.; Mathur, A.; Janakiraman, N.; Allareddy, V. Failure rates of mini-implants placed in the infrazygomatic region. Prog. Orthod. 2015, 16, 31. [Google Scholar] [CrossRef]
- Sreenivasagan, S.; Subramanian, A.K.; Nivethigaa, B. Assessment of insertion torque of mini-implant and its correlation with primary stability and pain levels in orthodontic patients. J. Contemp. Dent. Pract. 2021, 22, 84–88. [Google Scholar] [PubMed]
- Sreenivasagan, S.; Subramanian, A.K.; Rengalakshmi, S. Prevalence and cause of mini-implant failure encountered by orthodontic residents. J. Long-Term Eff. Med. Implants 2021, 31, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, A.; Jamdar, A.F.; Galgali, S.A.; Patil, S.; Patel, I.; Hemagiriyappa, M.S. Efficacy of infrazygomatic crest implants for full-arch distalization of maxilla and reduction of gummy smile in class II malocclusion. J. Contemp. Dent. Pract. 2021, 22, 1135–1143. [Google Scholar]
- Nienkemper, M.; Willmann, J.H.; Becker, K.; Drescher, D. RFA measurements of survival midpalatal orthodontic mini-implants in comparison to initial healing period. Prog. Orthod. 2020, 21, 5. [Google Scholar] [CrossRef] [PubMed]
- Motoyoshi, M.; Uchida, Y.; Inaba, M.; Ejima, K.; Honda, K.; Shimizu, N. Are assessments of damping capacity and placement torque useful in estimating root proximity of orthodontic anchor screws? Am. J. Orthod. Dentofac. Orthop. 2016, 150, 124–129. [Google Scholar] [CrossRef]
- Moeini, N.; Sabri, H.; Galindo-Fernandez, P.; Mirmohamadsadeghi, H.; Valian, N.K. Periodontal status following orthodontic mini-screw insertion: A prospective clinical split-mouth study. Clin. Exp. Dent. Res. 2023, 9, 596–605. [Google Scholar] [CrossRef]
- Migliorati, M.; Drago, S.; Gallo, F.; Amorfini, L.; Dalessandri, D.; Calzolari, C.; Benedicenti, S.; Silvestrini-Biavati, A. Immediate versus delayed loading: Comparison of primary stability loss after miniscrew placement in orthodontic patients-a single-centre blinded randomized clinical trial. Eur. J. Orthod. 2016, 38, 652–659. [Google Scholar] [CrossRef]
- Melo, A.C.; Andrighetto, A.R.; Hirt, S.D.; Bongiolo, A.L.; Silva, S.U.; Silva, M.A. Risk factors associated with the failure of miniscrews—A ten-year cross sectional study. Braz. Oral Res. 2016, 30, e124. [Google Scholar] [CrossRef]
- Lai, T.-T.; Chen, M.-H. Factors affecting the clinical success of orthodontic anchorage: Experience with 266 temporary anchorage devices. J. Dent. Sci. 2014, 9, 49–55. [Google Scholar] [CrossRef][Green Version]
- Jia, X.; Chen, X.; Huang, X. Influence of orthodontic mini-implant penetration of the maxillary sinus in the infrazygomatic crest region. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Haddad, R.; Saadeh, M. Distance to alveolar crestal bone: A critical factor in the success of orthodontic mini-implants. Prog. Orthod. 2019, 20, 19. [Google Scholar] [CrossRef] [PubMed]
- Szalma, J.; Gurdan, Z. Evaluation of the success and complication rates of self-drilling orthodontic mini-implants. Niger. J. Clin. Pract. 2018, 21, 546. [Google Scholar] [CrossRef]
- Garg, K.K.; Gupta, M. Assessment of stability of orthodontic mini-implants under orthodontic loading: A computed tomography study. Indian J. Dent. Res. 2015, 26, 237–243. [Google Scholar] [CrossRef]
- Bungău, T.C.; Vaida, L.L.; Moca, A.E.; Ciavoi, G.; Iurcov, R.; Romanul, I.M.; Buhaș, C.L. Mini-implant rejection rate in teenage patients depending on insertion site: A retrospective study. J. Clin. Med. 2022, 11, 5331. [Google Scholar] [CrossRef]
- Bearn, D.R.; Alharbi, F. British orthodontic society national audit of temporary anchorage devices (TADs): Report of the first thousand TADs placed. J. Orthod. 2015, 42, 214–219. [Google Scholar] [CrossRef]
- Azeem, M.; Saleem, M.M.; Liaquat, A.; Ul Haq, A.; Ul Hamid, W.; Masood, M. Failure rates of mini-implants inserted in the retromolar area. Int. Orthod. 2019, 17, 53–59. [Google Scholar] [CrossRef]
- Abu Arqub, S.; Greene, R.; Greene, S.; Laing, K.; Kuo, C.-L.; Godoy, L.D.C.; Uribe, F. Ridge mini-implants, a versatile biomechanical anchorage device whose success is significantly enhanced by splinting: A clinical report. Prog. Orthod. 2023, 24, 27. [Google Scholar] [CrossRef]
- Arqub, S.A.; Gandhi, V.; Mehta, S.; Palo, L.; Upadhyay, M.; Yadav, S. Survival estimates and risk factors for failure of palatal and buccal mini-implants. Article. Angle Orthod. 2021, 91, 756–763. [Google Scholar] [CrossRef]
- Vicioni-Marques, F.; Pimentel, D.J.B.; Matsumoto, M.A.N.; Stuani, M.B.S.; Romano, F.L. Orthodontic mini-implants: Clinical and peri-implant evaluation. J. World Fed. Orthod. 2022, 11, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Sarul, M.; Lis, J.; Park, H.S.; Rumin, K. Evidence-based selection of orthodontic miniscrews, increasing their success rate in the mandibular buccal shelf. A randomized, prospective clinical trial. BMC Oral Health 2022, 22, 414. [Google Scholar] [CrossRef] [PubMed]
- Nienkemper, M.; Willmann, J.H.; Drescher, D. Long-term stability behavior of paramedian palatal mini-implants: A repeated cross-sectional study. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Aly, S.A.; Alyan, D.; Fayed, M.S.; Alhammadi, M.S.; Mostafa, Y.A. Success rates and factors associated with failure of temporary anchorage devices: A prospective clinical trial. J. Investig. Clin. Dent. 2018, 9, e12331. [Google Scholar] [CrossRef]
- Ağlarcı, C.; Esenlik, E.; Fındık, Y. Comparison of short-term effects between face mask and skeletal anchorage therapy with intermaxillary elastics in patients with maxillary retrognathia. Eur. J. Orthod. 2016, 38, 313–323. [Google Scholar] [CrossRef]
- Yao, C.C.; Chang, H.H.; Chang, J.Z.; Lai, H.H.; Lu, S.C.; Chen, Y.J. Revisiting the stability of mini-implants used for orthodontic anchorage. J. Formos. Med. Assoc. 2015, 114, 1122–1128. [Google Scholar] [CrossRef]
- Mommaerts, M.Y.; Nols, V.; De Pauw, G. Long-term prospective study of an orthodontic bone anchor. Int. J. Oral Maxillofac. Implants 2014, 29, 419–426. [Google Scholar] [CrossRef]
- Hourfar, J.; Bister, D.; Kanavakis, G.; Lisson, J.A.; Ludwig, B. Influence of interradicular and palatal placement of orthodontic mini-implants on the success (survival) rate. Head Face Med. 2017, 13, 14. [Google Scholar] [CrossRef]
- Nienkemper, M.; Wilmes, B.; Pauls, A.; Yamaguchi, S.; Ludwig, B.; Drescher, D. Treatment efficiency of mini-implant-borne distalization depending on age and second-molar eruption. J. Orofac. Orthop. 2014, 75, 118–132. [Google Scholar] [CrossRef]
- He, Y.; Liu, J.; Huang, R.; Chen, X.; Jia, X.; Zeng, N.; Fan, X.; Huang, X. Clinical analysis of successful insertion of orthodontic mini-implants in infrazygomatic crest. BMC Oral Health 2023, 23, 348. [Google Scholar] [CrossRef]
- Azeem, M.; Haq, A.U.; Awaisi, Z.H.; Saleem, M.M.; Tahir, M.W.; Liaquat, A. Failure rates of miniscrews inserted in the maxillary tuberosity. Dent. Press J. Orthod. 2019, 24, 46–51. [Google Scholar] [CrossRef]
- Bratu, D.C.; Popa, G.; Petrescu, H.P.; Karancsi, O.L.; Bratu, E.A.; Babeș, V. Influence of chemically-modified implant surfaces on the stability of orthodontic mini-implants. Rev. Chim. 2014, 65, 1222–1225. [Google Scholar]
- Kim, J.W.; Lee, N.K.; Sim, H.Y.; Yun, P.Y.; Lee, J.H. Failure of orthodontic mini-implants by patient age, sex, and arch; number of primary insertions; and frequency of reinsertions after failure: An analysis of the implant failure rate and patient failure rate. Int. J. Periodontics Restor. Dent. 2016, 36, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Migliorati, M.; Drago, S.; Amorfini, L.; Nucera, R.; Silvestrini-Biavati, A. Maximum insertion torque loss after miniscrew placement in orthodontic patients: A randomized controlled trial. Orthod. Craniofacial Res. 2021, 24, 386–395. [Google Scholar] [CrossRef]
- Ravi, J.; Duraisamy, S.; Rajaram, K.; Kannan, R.; Arumugam, E. Survival rate and stability of surface-treated and non-surface-treated orthodontic mini-implants: A randomized clinical trial. Dent. Press J. Orthod. 2023, 28, e2321345. [Google Scholar] [CrossRef]
- Slabkovskaya, A.; Divnich, A.; Abramova, M.; Slabkovsky, R.; Alimova, A.; Lukina, G. Clinical and radiographic changes following orthodontic intrusion of overerupted maxillary molars with two mini-implants. Georgian Med. News 2021, 318, 50–56. [Google Scholar]
- Kuroda, T. Evidence-based individualized orthodontic treatment: The future of orthodontics? J. World Fed. Orthod. 2020, 9, 139–145. [Google Scholar] [CrossRef]
- Yu, W.-P.; Tsai, M.-T.; Yu, J.-H.; Huang, H.-L.; Hsu, J.-T. Bone quality affects stability of orthodontic miniscrews. Sci. Rep. 2022, 12, 2849. [Google Scholar] [CrossRef]
- Tarigan, S.H.P.; Sufarnap, E.; Bahirrah, S. The orthodontic mini-implants failures based on patient outcomes: Systematic review. Eur. J. Dent. 2024, 18, 417–429. [Google Scholar] [CrossRef]
- Tian, Y. A review on factors related to patient comfort experience in hospitals. J. Health Popul. Nutr. 2023, 42, 125. [Google Scholar] [CrossRef]
- Huang, Y.C.; Huang, Y.C.; Ding, S.J. Primary stability of implant placement and loading related to dental implant materials and designs: A literature review. J. Dent. Sci. 2023, 18, 1467–1476. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Databases and Search Date | Search Strategy & Filters | Results |
|---|---|---|
| Dentistry & Oral Sciences Source (EBSCOhost) https://web.p.ebscohost.com/ehost/search/advanced?vid=0&sid=cb491755-8714-4139-8948-384b93edcb90%40redis (accessed on 13 September 2023) | (((“Orthodontics”) OR (“Orthodontics, Corrective”) OR (“Corrective Orthodontics”) OR (“Orthodontics, Interceptive”) OR (“Interceptive Orthodontics”)) AND ((“men”) OR (“women”) OR (“patient”) OR (“female”) OR (“male”) OR (“subjects”) OR (“adult”) OR (“human”))) AND TI ((“Mini implants”) OR (“mini-implants”) OR (“orthodontic mini implants”) OR (“orthodontic mini-implants”) OR (“temporary anchorage device”)) OR AB ((“Mini implants”) OR (“mini-implants”) OR (“orthodontic mini implants”) OR (“orthodontic mini-implants”) OR (“temporary anchorage device”)) Filters: 2013–2023 & English | 125 |
| Ovid Medline https://ovidsp.dc2.ovid.com/ovid-new-a/ovidweb.cgi (accessed on 13 September 2023) | ((Orthodontics or Orthodontics, Corrective or Corrective Orthodontics or Orthodontics, Interceptive or Interceptive Orthodontics) and (men or women or patient or female or male or subjects or adult or human)).af. and (Mini implants or mini-implants or orthodontic mini implants or orthodontic mini-implants or temporary anchorage device).ab. and (Mini implants or mini-implants or orthodontic mini implants or orthodontic mini-implants or temporary anchorage device).ti. Filters: 2013–2023 | 58 |
| PubMed https://pubmed.ncbi.nlm.nih.gov/?otool=nvujrolib (accessed on 13 September 2023) | (“Orthodontics” [Mesh] OR “Orthodontics, Corrective” [Mesh] OR “Orthodontics, Interceptive” [Mesh]) AND (“Mini implants” [tiab] OR “mini-implants” [tiab] OR “orthodontic mini implants” [tiab] OR “orthodontic mini-implants” [tiab] OR “temporary anchorage device” [tiab]) Filters: Human, English, & 2013–2023 | 284 |
| Scopus https://www.scopus.com/search/form.uri?display=basic#basic (accessed on 13 September 2023) | (TITLE-ABS-KEY (((“Orthodontics”) OR (“Orthodontics, Corrective”) OR (“Corrective Orthodontics”) OR (“Orthodontics, Interceptive”) OR (“Interceptive Orthodontics”)) AND ((“Mini implants”) OR (“mini-implants”) OR (“orthodontic mini implants”) OR (“orthodontic mini-implants”) OR (“temporary anchorage device”))) AND ALL (((“men”) OR (“women”) OR (“patient”) OR (“female”) OR (“male”) OR (“subjects”) OR (“adult”) OR (“human”))) AND NOT ALL ((“animal models”))) AND (LIMIT-TO (SUBJAREA, “DENT”)) AND (LIMIT-TO (LANGUAGE, “English”)) AND (LIMIT-TO (EXACTKEYWORD, “Human”) OR LIMIT-TO (EXACTKEYWORD, “Humans”) OR LIMIT-TO (EXACTKEYWORD, “Orthodontic Anchorage Procedures”)) Filters: Human, English, & 2013–2023 | 155 |
| Web of Science https://www.webofscience.com/wos/woscc/basic-search (accessed on 13 September 2023) | ALL = ((“Orthodontics”) OR (“Orthodontics, Corrective”) OR (“Corrective Orthodontics”) OR (“Orthodontics, Interceptive”) OR (“Interceptive Orthodontics”)) AND TS = ((“Mini implants”) OR (“mini-implants”) OR (“orthodontic mini implants”) OR (“orthodontic mini-implants”) OR (“temporary anchorage device”)) AND ALL = ((“men”) OR (“women”) OR (“patient”) OR (“female”) OR (“male”) OR (“subjects”) OR (“adult”) OR (“human”)) NOT ALL = ((“animal models”)) Filters: Human, English, & 2013–2023 | 130 |
| Study Design | Count (%) |
|---|---|
| Retrospective | 11 (30.6%) |
| Retrospective Cohort | 4 (11.1%) |
| Cohort | 3 (8.3%) |
| Prospective | 3 (8.3%) |
| Cross-sectional | 2 (5.6%) |
| Longitudinal | 2 (5.6%) |
| Prospective Clinical Trial | 2 (5.6%) |
| Randomized Clinical Trial | 3 (8.3%) |
| Retrospective Cross-sectional | 2 (5.6%) |
| Case–control | 1 (2.8%) |
| Longitudinal Prospective | 1 (2.8%) |
| Prospective Cohort | 1 (2.8%) |
| Randomized Case–control | 1 (2.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gardner, J.D.; Ha, A.; Lee, S.; Mohajeri, A.; Schwartz, C.; Hung, M. Where You Place, How You Load: A Scoping Review of the Determinants of Orthodontic Mini-Implant Success. Appl. Sci. 2025, 15, 9673. https://doi.org/10.3390/app15179673
Gardner JD, Ha A, Lee S, Mohajeri A, Schwartz C, Hung M. Where You Place, How You Load: A Scoping Review of the Determinants of Orthodontic Mini-Implant Success. Applied Sciences. 2025; 15(17):9673. https://doi.org/10.3390/app15179673
Chicago/Turabian StyleGardner, Jacob Daniel, Ambrose Ha, Samantha Lee, Amir Mohajeri, Connor Schwartz, and Man Hung. 2025. "Where You Place, How You Load: A Scoping Review of the Determinants of Orthodontic Mini-Implant Success" Applied Sciences 15, no. 17: 9673. https://doi.org/10.3390/app15179673
APA StyleGardner, J. D., Ha, A., Lee, S., Mohajeri, A., Schwartz, C., & Hung, M. (2025). Where You Place, How You Load: A Scoping Review of the Determinants of Orthodontic Mini-Implant Success. Applied Sciences, 15(17), 9673. https://doi.org/10.3390/app15179673








