1. Introduction
Basketball is an intermittent and dynamic team sport that combines multidirectional explosive movements such as accelerations, jumps, sprints, and decelerations, and rapid change-of-direction (COD) actions, together with complex technical and tactical actions [
1]. During games, players perform approximately 115 high-intensity actions, placing significant biomechanical, neuromuscular, and physiological demands on the body [
2]. Acceleration and deceleration generate high levels of mechanical stress and require elevated rates of force development and neural activation, particularly when executed at maximal intensity [
3]. These physical demands increase the risk of lower extremity injuries, especially in professional basketball, where game intensity often exceeds that observed at amateur levels [
4]. Advances in monitoring technologies, such as local positioning systems (LPS) and accelerometers, have provided detailed insights into the physical demands of basketball by accurately quantifying high-intensity actions during games [
5]. These advancements underscore the importance of designing targeted strength and conditioning programs to mitigate mechanical stress, enhance athletic performance, and reduce injury risk [
5].
Injury prevention programs in basketball have prioritized reducing the high incidence of ankle injuries, which account for up to 30% of all injuries reported in court-based sports, including basketball, volleyball, and handball [
6]. Key risk factors include a history of previous ankle injuries, inadequate neuromuscular control, and biomechanical instability—often exacerbated by poor proprioception or delayed muscle responses [
6]. Evidence shows that proprioceptive and neuromuscular intervention programs significantly reduce the incidence of lateral ankle sprains by improving joint stability and motor control [
7]. Exercises such as hopping drills and dynamic stability tasks have been shown to induce neuromuscular adaptations, enabling quicker and more controlled movements during high-intensity actions [
8]. Furthermore, these interventions are essential not only for preventing recurrent acute injuries but also for mitigating chronic ankle instability, a common consequence of poorly rehabilitated or untreated sprains [
6] which can impair COD performance during high-intensity multidirectional actions.
Beyond injury prevention, ankle function is also essential for performance in high-demand movements such as COD actions [
8]. The ability to execute rapid COD movements is fundamental for basketball players, as these movements are frequently required during both offensive and defensive actions [
9]. Several studies have indicated that ankle joint properties, including stiffness, may influence performance in such actions due to their association with improved movement efficiency and reduced injury risk [
10,
11]. Moreover, research has focused on the relationship between plantar flexion strength and ankle stability during COD movements, underscoring the importance of incorporating stiffness-related parameters into intervention programs [
12].
Isometric training has gained recognition as an effective modality for promoting neuromuscular adaptations and optimizing force production without excessive joint displacement [
13,
14]. This training approach aligns well with the mechanical demands imposed by accelerations, decelerations, and COD movements, which frequently occur during basketball games [
5]. Additionally, isometric exercises targeting the ankle joint, such as plantar flexion and inversion holds, have been shown to enhance joint stability and reduce the risk of lateral ankle sprains, one of the most prevalent injuries in the sport [
8].
However, recent evidence highlights that the specific characteristics of isometric protocols, such as intensity, duration, muscle length, and intent, determine the nature of the resulting adaptations [
13,
14]. Sustained isometric contractions performed at moderate to high intensities (e.g., 70–75% MVC) for prolonged durations have been associated with increases in maximal strength and muscle hypertrophy [
14], whereas ballistic or high-intent contractions appear more effective in enhancing neural drive and rate of force development (RFD) [
13,
14]. Despite this differentiation, most interventions rely on isolated applications of either sustained or ballistic modalities [
13,
14]. This fragmentation may limit the scope of adaptation: sustained contractions enhance force steadiness but may lack transferability to dynamic movements [
14], while ballistic protocols optimize RFD but might not sufficiently improve joint-specific stability required for injury prevention [
13].
The rationale for combining both modalities lies in addressing these limitations and capitalizing on their complementary effects. As shown in the systematic reviews by Oranchuk et al. [
13] and Lum & Barbosa [
14], each strategy activates distinct neuromuscular pathways. However, their integration within a single training protocol remains largely unexplored in elite sport contexts. Given the high incidence of ankle injuries and the limited transfer of isolated training modalities to sport-specific actions, a dual-modality intervention may offer a more ecologically valid and performance-relevant strategy for professional basketball players.
Building upon this theoretical framework, the present study aimed to examine the effects of a season-long, combined isometric intervention program on ankle dorsiflexion and COD performance. Functional outcomes were assessed using the Lunge Test and the L-Test, validated tools for evaluating ankle mobility and multidirectional COD performance, respectively. We hypothesized that integrating both sustained and ballistic isometric modalities would elicit neuromuscular adaptations associated with improvements in dorsiflexion and COD performance, thereby contributing to enhanced performance in basketball.
2. Materials and Methods
2.1. Participants
Fourteen male professional basketball players [age: 25.60 ± 3.86 years; height: 1.97 ± 0.07 m; body mass: 94.82 ± 10.17 kg; BMI: 24.40 ± 1.42 kg/m2] from a French second-division basketball team (ProB) participated in this study during the 2023–2024 season. The sample size was estimated using G*Power software (version 3.1.9.4, Franz, Universität Kiel, Germany) as a proxy for the Friedman test. Since G*Power does not directly support non-parametric tests, a repeated-measures within-subjects ANOVA model was used to approximate the required sample size. The calculation assumed a large effect size of 0.40, an alpha level of 0.05, and a statistical power of 0.80, yielding a minimum required sample size of 13 participants.
All participants had a documented history of ankle sprains but were injury-free at the time of testing and able to maintain their regular training and competition schedules. Ankle sprain history was verified through team medical records and preseason physical screenings conducted by the club’s medical staff. Eligibility criteria excluded individuals with a history of ankle surgeries, injections (e.g., platelet-rich plasma or analgesics), smoking habits, cardiovascular disorders, or the use of steroids or performance-enhancing supplements within three months prior to the study.
The study adhered to the principles of the Declaration of Helsinki and received ethical approval from the European University of Madrid (code: 3103202314923) and the Boulazac Basket Dordogne club.
2.2. Study Design and Setting
This study employed a convenience sampling approach, utilizing the full availability of the team roster. It was designed as a longitudinal experimental study and involved assessments at three fixed time points during the 2023–2024 season:
- (1)
pre-intervention, on 4 August at 10:00 A.M.;
- (2)
mid-intervention, on 4 December at 10:00 A.M.; and
- (3)
post-intervention, on 30 April at 10:00 A.M.
Data collection took place in a gymnasium with a parquet floor to replicate game-like conditions. Throughout the study period, players maintained their regular training and competition routines under the supervision of the team’s coaching staff. The study objectives, potential benefits, and risks were explained in detail to all participants before obtaining written informed consent.
2.3. Intervention Program
The intervention program consisted of two components: force-steady sustained running postures and additional isometric exercises performed in the gym. It was integrated into the players’ regular training routines and supervised by the team’s strength and conditioning coach to ensure proper execution and compliance. To control training intensity, 80% of each athlete’s Maximum Voluntary Contraction (MVC) was individually determined using a calibrated handheld dynamometer (Commander Echo, JTech Medical, Midvale, UT, USA). During a familiarization session, MVC was measured as athletes performed three maximal isometric contractions in the same joint positions that were later used in the intervention. For this assessment, athletes stood in the propulsion phase position (front knee flexed at ~30° and rear ankle dorsiflexed at 90°) against a padded wall, as described in
Section 2.3.1. The highest value recorded was used to calculate the 80% threshold. During wall-based isometric exercises, force output could not be directly measured. Therefore, the strength and conditioning coach provided intermittent verbal cues based on each athlete’s previously collected MVC data, and offered continuous visual feedback via a tablet-based display (iPad, Apple Inc., Cupertino, CA, USA) connected to the handheld dynamometer, showing the force output relative to the target 80% MVC. This allowed athletes to adjust their effort and maintain proper posture and alignment throughout each contraction. Throughout the training period, verbal instructions and occasional real-time feedback were used to support players in maintaining consistent effort across sessions.
During the intervention period, players continued with their standard team training and competition routines with no major modifications. The weekly schedule included five on-court training sessions (90–120 min each) and one official game per week, in accordance with the team’s competitive calendar. Training content was supervised and planned by the coaching and strength and conditioning staff, following a structured periodization plan that did not include new components aimed at ankle mobility or change-of-direction performance beyond the study intervention. No additional prevention programs, resistance training blocks, or individual conditioning plans were implemented during this time. While external load quantification tools (e.g., GPS or RPE logs) were not employed, the team maintained a consistent training structure that remained aligned with in-season demands.
2.3.1. Force-Steady Sustained Running Postures
Although the force-steady sustained running postures were performed against a padded wall, despite some degree of surface compliance, the exercises were designed and executed to minimize joint displacement and promote static muscle action. Players were instructed to hold fixed sprint-specific positions while applying force against the wall at approximately 80% of their individualized MVC. No visible joint displacement was observed during the effort phases, and real-time verbal cues were provided to maintain posture consistency. While the mechanical environment cannot be considered perfectly rigid, the contraction type reflects functional isometric loading commonly applied in sports performance contexts, emphasizing postural control, neuromuscular activation, and joint-angle specific force production.
Three force-steady sustained running postures replicating key phases of sprint mechanics were performed against a wall with elastic resistance (
Figure 1):
- (i)
Propulsion phase (A): the front knee (right leg) was flexed at ~30°, the rear leg slightly flexed at the knee with the ankle dorsiflexed at 90°, the torso inclined slightly forward from the hips (~10–15°), the head aligned with the spine, the gaze forward, and the arms positioned in a running stance.
- (ii)
Mid-acceleration phase (B): the front knee (right leg) was flexed at approximately 45°, the rear leg exhibited triple extension (hip, knee, and ankle) with the heel lifted, the torso leaned slightly forward, the head remained aligned with the spine, and the arms were positioned reciprocally as in running motion
- (iii)
Full-extension phase (C): the front knee (right leg) was fully extended and rear ankle dorsiflexed at 90°, the rear leg fully extended at the hip and knee, the torso upright with minimal forward lean, the head aligned with the spine, and arms aligned in sprint posture.
Each posture was held for 15 to 20 s at 80% of the MVC, with 12 repetitions per set and 3 sets per session. Ninety-second rest intervals were provided between sets to minimize fatigue.
Figure 1.
Force-steady sustained running postures simulating key phases sprint mechanics: (A) propulsion phase, (B) mid-acceleration phase, and (C) full-extension phase. All postures were performed with the right leg as the front leg.
Figure 1.
Force-steady sustained running postures simulating key phases sprint mechanics: (A) propulsion phase, (B) mid-acceleration phase, and (C) full-extension phase. All postures were performed with the right leg as the front leg.
2.3.2. Gym-Based Isometric Exercises
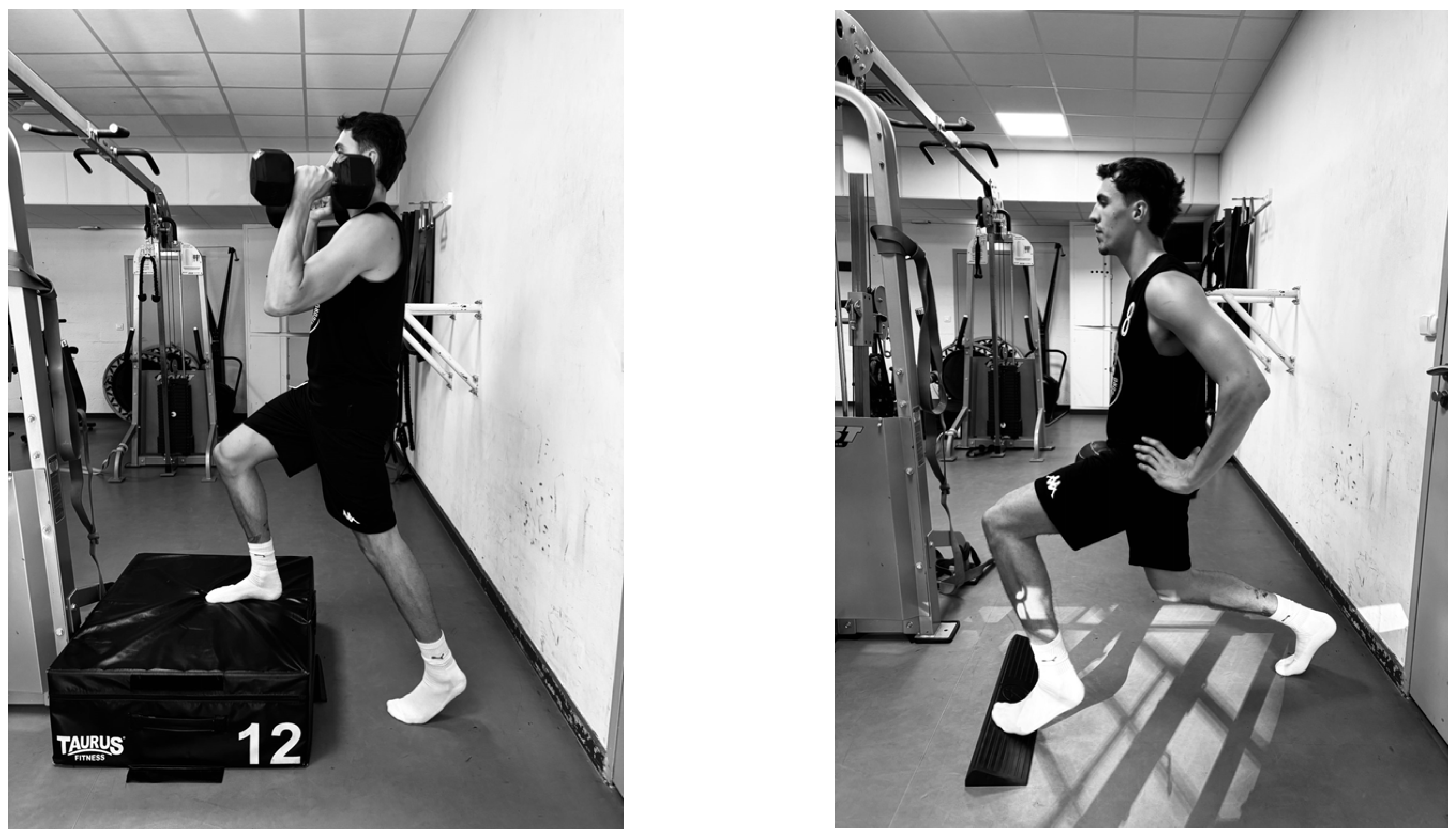
Two additional isometric exercises were included to reinforce lower-body strength and enhance ankle control, supporting joint stability and performance during multi-directional movements (
Figure 2):
- (i)
Elevated hold with external load: performed unilaterally on a 12-in (~30.5 cm) padded plyometric box (Taurus; Fitshop GmbH, Schleswig, Germany), with the stance foot fully planted on the box (heel down) and the contralateral foot maintaining forefoot contact with the floor (heel unsupported). Athletes maintained an isometric contraction while holding dumbbells (mean load = 14 ± 3 kg per hand) in the front-rack position. They were instructed to keep the trunk upright, gaze forward, and avoid compensatory movements at the hips or spine.
- (ii)
Split squat isometric hold: executed with the front foot on an inclined wedge (~10 cm at the highest edge), with the rear knee flexed slightly beyond 90° and the pelvis in a neutral position, while maintaining an upright trunk posture. The exercise was performed without external load and without pushing against any fixed surface. Athletes were instructed to aim for a balanced weight distribution between both legs and to avoid excessive anterior translation of the front knee beyond the toes.
Each exercise was performed for sets of 30 s isometric holds at approximately 75–80% of MVC, with 60 s of rest between sets. Progressive load adjustments were made incrementally, increasing dumbbell weight by an average of ~8% every 4 weeks, progressing from ~75% to 80% of MVC by the final training block. These exercises were incorporated twice per week.
Figure 2.
Gym-based isometric exercises.
Figure 2.
Gym-based isometric exercises.
2.4. Data Collection Protocol
The effects of the intervention program were evaluated using two validated tests designed to assess both performance outcomes and injury-related metrics: the Lunge Test, which measured ankle dorsiflexion range of motion, and the L-Test, which evaluated agility through high-speed change-of-direction performance. The Lunge Test has demonstrated strong concurrent validity with motion capture systems, supporting its use as a reliable and practical tool for assessing ankle mobility and its potential association with injury risk in basketball players [
15]. Similarly, the L-Test has shown high correlations with established agility assessments, such as the T-Test and the Illinois Agility Test, confirming its validity for evaluating change-of-direction ability [
16]. Before each testing session, participants completed a standardized 15 min warm-up consisting of foam rolling, joint mobility exercises, and dynamic muscle activation drills.
2.4.1. Lunge Test
For the Lunge Test, participants positioned one foot close to a wall and leaned forward while keeping the heel in contact with the floor, ensuring the knee contacted the wall. Ankle dorsiflexion range of motion was measured using a digital goniometer (Commander Echo; JTECH Medical, Midvale, UT, USA), with the best of three trials recorded for each leg. All trials were performed consecutively during the same session under standardized conditions.
2.4.2. L-Test
The L-Test of Functional Mobility was used to assess multidirectional COD performance. Following standardized procedures described in the previous literature [
17] three cones were arranged in an “L” shape: the first cone was placed 3 m in front of an armless chair, and the second cone was positioned 7 m to the right of the first. At the start signal, participants stood up from the chair, walked 3 m, made a 90° turn, walked 7 m, performed a 180° turn, retraced the patch, made another 90° turn, and returned to sit down on the chair. The total walking distance was 20 m including (sit-to-stand and stand-to-sit) and four changes in direction. Standardized instructions were provided, followed by a demonstration of the test. Participants completed one practice trial before timed attempts. Trials were considered deviated from the designated course, failed to execute the required direction changes, or did not sit fully back in the chair upon completion. Performance time was recorded using a dual-beam photocell timing system (Witty Gate, Microgate, Bolzano, Italy) placed at the start/finish line. Timing started when the participant broke the beam immediately after rising from the chair and stopped upon return to the seated position. The best performance time from three valid trials in each change-of-direction side (leftwards and rightwards) was used for analysis. All tests were performed consecutively in a single session under identical conditions, with a minimum rest interval of 2 min between trials to minimize fatigue.
2.5. Data Analysis
Statistical analyses were performed using JASP software (version 0.18.3; JASP Team, University of Amsterdam, Amsterdam, The Netherlands). Given the small sample size (
n = 14), nonparametric tests were chosen, as they are more robust to violations of normality and the presence of outliers. To compare injury frequencies between the 2022–2023 and 2023–2024 seasons, the Wilcoxon signed-rank test was used. To evaluate the effects of the intervention program across the three time points (pre-, mid-, and post-intervention), Friedman’s test was applied to the Lunge Test and L-Test results. Effect sizes for Friedman’s test were calculated using Kendall’s W, interpreted as small (0.01), moderate (0.06), and large (0.14) [
18]. When significant effects were observed, post hoc pairwise comparisons with Bonferroni correction were conducted to control for Type I error. Measurement reproducibility was assessed through the calculation of the SEM, SRD, and CV%, providing insights into the reliability, precision, and consistency of the Lunge Test and L-Test scores. In addition, a linear mixed model was applied to complement the repeated-measures analysis, accounting for the within-subject correlation structure of the data. This model included fixed effects for time (Pre-, Mid-, Post-intervention), leg (left vs. right), and their interaction, with participant ID modeled as a random effect. The model was further adjusted for individual injury frequencies reported throughout the season, in order to control for potential confounding effects. Finally, percentage changes between time points (pre–mid, mid–post, and pre–post) were calculated for both tests to aid data visualization and provide a clearer understanding of relative performance changes over the intervention period. Statistical significance was set at
p < 0.05 for all tests.
3. Results
Table 1 summarizes the results of the Lunge Test and L-Test, showing significant improvements in ankle mobility and COD performance across the pre-, mid-, and post-intervention assessments in both legs
The linear mixed model analysis revealed significant main effects of time on L-Test COD performance, with statistically significant improvements observed at both mid- (
p < 0.001) and post-intervention (
p = 0.016) compared to pre-intervention. In contrast, the effect of time on the Lunge Test did not reach statistical significance (
p = 0.081 at mid-intervention;
p = 0.820 at post-intervention). No significant main effects were found for leg or for the time × leg interaction in either test. Detailed parameter estimates are presented in
Table 2.
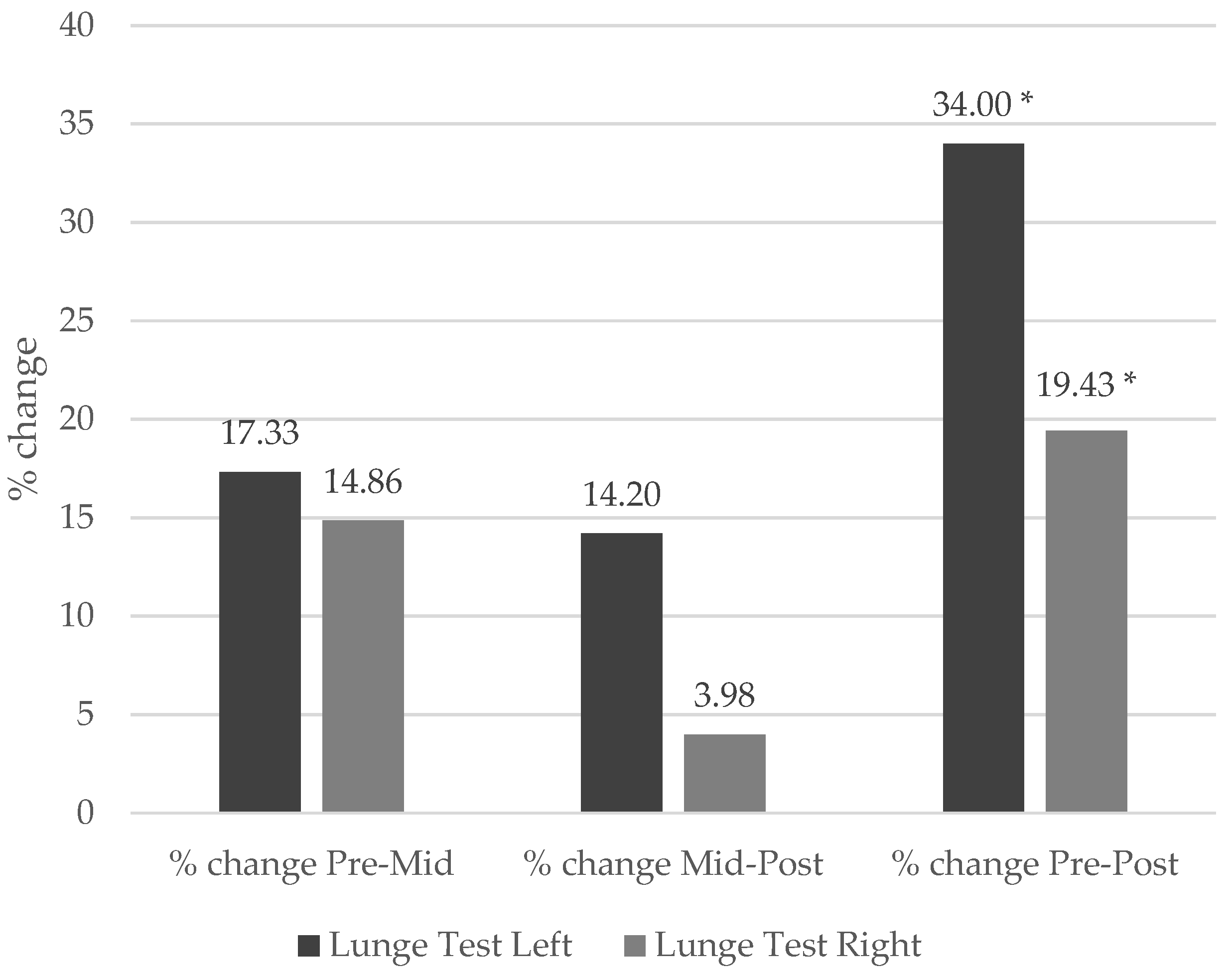
In the Lunge Test, significant improvements were observed in both legs (
Figure 3). For the left leg, there was a statistically significant difference (χ
2(
2) = 6.35,
p = 0.042, Kendall’s W = 0.31), indicating a moderate effect size according to Kendall s W. Post hoc comparisons indicated significant improvements between the pre- and post-intervention moments (Mean Difference [MD] = −2.55 cm, CI95% [−4.65, −0.45], r = 0.73,
p = 0.015). Similarly, in the right leg, significant differences were found (χ
2(
2) = 9.29,
p = 0.010, Kendall’s W = 0.47), suggesting a moderate-to-large effect size, with improvements between the pre- and post-intervention moments (MD = −1.70 cm, CI95% [−3.06, −0.34], r = 0.74,
p = 0.012).
Figure 3 illustrates the percentage change in Lunge Test performance over time. No statistically significant differences were detected between legs at any assessment time point (all
p > 0.05), suggesting that the intervention had balanced effects on ankle dorsiflexion range of motion in both legs.
The reproducibility analysis demonstrated adequate reliability of the Lunge Test. For the left leg, the SEM was 0.75 cm, the SRD was 2.07 cm, and the CV% was 30.05%. For the right leg, the SEM was 0.42 cm, the SRD was 1.15 cm, and the CV% was 13.79%. These demonstrate the consistency and precision of the measurements.
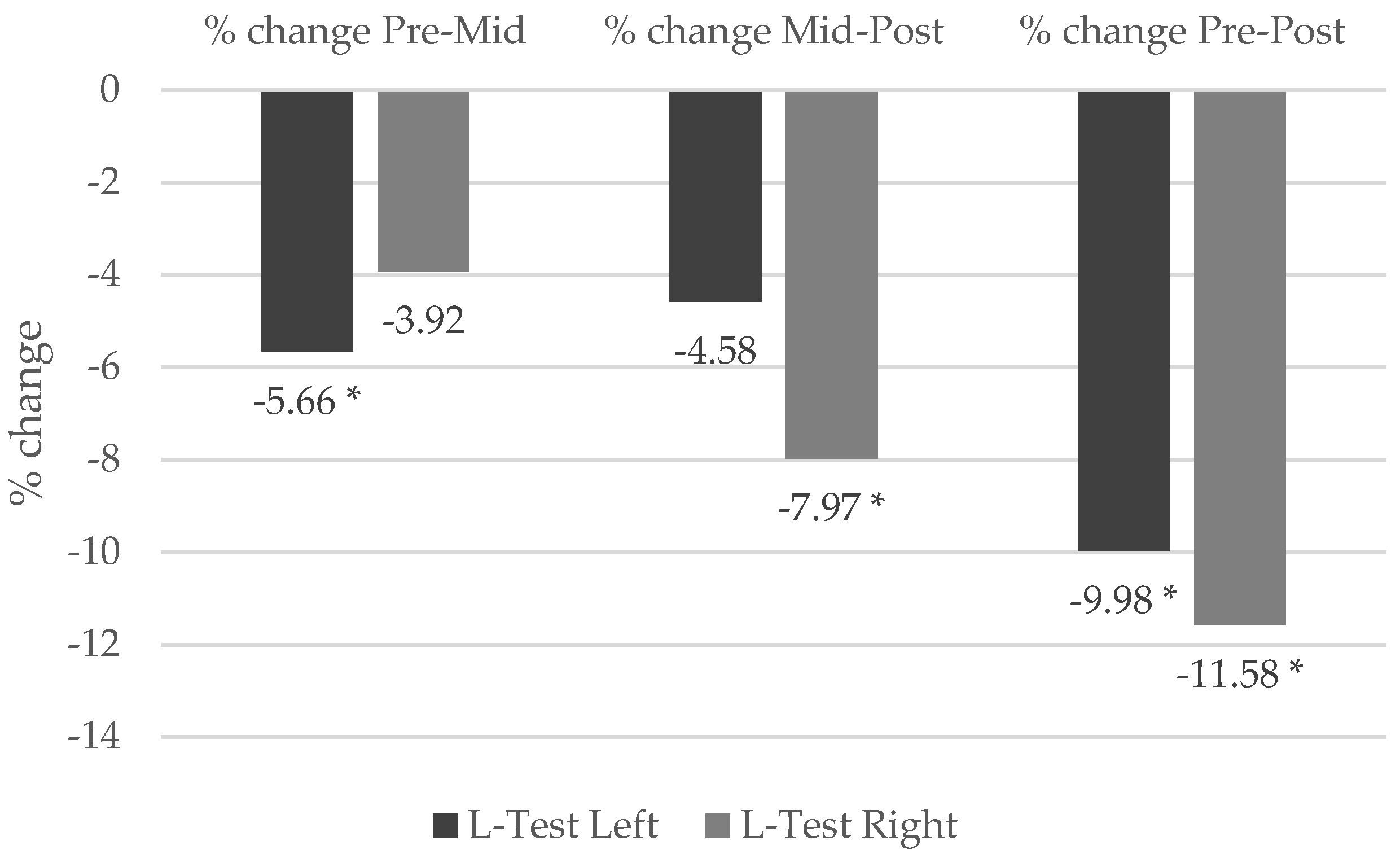
In the L-Test, a significant difference was observed for the leftwards COD (χ2(2) = 14.60, p < 0.001, Kendall’s W = 0.73), indicating a large effect size. Post hoc comparisons indicated significant improvements between the pre- and mid-intervention moments (MD = 0.33 s, CI95% [0.08, 0.59], r = 0.75, p = 0.009), as well as between the pre- and post-intervention moments (MD = 0.59 s, CI95% [0.33, 0.85], r = 0.89, p < 0.001). Similarly, in the rightward COD, significant differences were found (χ2(2) = 16.80, p < 0.001, Kendall’s W = 0.84), suggesting a large effect size. Post hoc analysis revealed improvements between the pre- and post-intervention moments (MD = 0.68 s, CI95% [0.44, 0.92], r = 0.93, p <.001) as well as between the mid- and post-intervention moments (MD = 0.45 s, CI95% [0.21, 0.69], r = 0.85, p < 0.001).
No statistically significant differences were detected between COD sides at any assessment time point (all
p > 0.05), suggesting that intervention produced balanced effects in both COD sides, with no evident performance asymmetries.
Figure 4 illustrates the percentage change in L-Test performance over time, showing progressive improvements, particularly between pre- and post-intervention assessments, with consistent gains in both COD sides.
The reproducibility analysis demonstrated excellent reliability of the L-Test. For the leftwards COD, the SEM was 0.15 s, the SRD was 0.41 s, and the CV% was 5.95%. For the rightward COD, the SEM was 0.16 s, the SRD was 0.45 s, and the CV% was 6.60%. These findings support the use of the L-Test as a reliable tool for assessing COD performance over time.
4. Discussion
The main finding of this study indicates that isometric training significantly improved ankle joint mobility, as measured by the Lunge Test, and enhanced COD performance, as reflected by reduced L-Test completion times. Furthermore, the use of linear mixed models, adjusted for injury history, confirmed the statistical significance of these improvements over time, thereby reinforcing the robustness of the observed effects. These improvements are particularly relevant in basketball, where the ability to accelerate, decelerate, and explosively change direction is critical to performance and has a direct impact on game success [
19].
Lunge Test results revealed significant improvements in ankle dorsiflexion, a key determinant of both athletic performance and injury prevention. Increased dorsiflexion reduces the risk of sprains during falls and landings [
20]. Hoch et al. [
21] demonstrated that limited dorsiflexion is associated with a greater injury risk due to altered landing mechanics. Similarly, Naderifar et al. [
6] emphasized the value of neuromuscular control exercises in enhancing postural stability and dynamic ankle function, which aligns with the dorsiflexion improvements observed in our participants. In contrast, alternative methods such as proprioceptive or balance training have not consistently shown positive changes in the dorsiflexion range of motion [
22]. Oranchuk et al. [
13] further supported these findings by demonstrating that isometric training at long muscle lengths (LMLs) enhances muscle function via increased mechanical tension and metabolite accumulation, mechanisms that may underline the improvements observed in our results. These physiological responses may explain the ability of isometric training to elicit greater neuromuscular activation and motor control, thereby improving ankle function during high-demand tasks such as rapid COD movements in basketball. However, it is important to note that increased dorsiflexion range of motion is not inherently beneficial in all contexts [
20,
21]. While limited dorsiflexion has been linked to altered landing mechanics and elevated injury risk, excessive mobility could potentially compromise joint stability, particularly in individuals with underlying laxity or poor neuromuscular control [
20,
21]. Therefore, dorsiflexion gains should be interpreted in conjunction with functional performance assessments to ensure that joint integrity is not adversely affected.
The L-Test, which evaluates COD performance, showed significant improvements in execution times, indicating enhanced performance. Although the isometric training was conducted in force-steady sustained running postures, its potential influence on running technique or motor control remains speculative in the absence of baseline assessments. Nevertheless, improvements in joint control and postural stability might have contributed indirectly to better movement efficiency during COD movements [
23]. Similarly, studies such as Naderifar et al. [
6] have emphasized the role of neuromuscular exercises in enhancing balance symmetry and motor control, factors that are critical for high-speed movements in sports like basketball. These findings align with previous research, suggesting that isometric training, when combined with ballistic exercises, enhances neuromuscular activation and rapid force production [
13]. Moreover, Forster et al. [
24] reported that combining isometric protocols with sprint and plyometric training further enhances COD performance. This capacity to perform repeated high-intensity actions, such as sprints and rapid COD movements, is essential in elite basketball, where COD agility and joint mobility are critical for meeting these demands [
25]. Therefore, improving these abilities through targeted isometric and neuromuscular training may offer functional benefits that translate into enhanced in-game performance [
26].
Beyond its preventive value, the isometric training protocol demonstrated measurable performance enhancements, particularly in COD performance and joint mobility, both of which are essential for optimizing movement efficiency in basketball-specific actions [
25]. These findings are in line with Naderifar et al. [
6], who reported that neuromuscular and isometric interventions enhance motor control and balance symmetry, facilitating rapid COD movements. These improvements contribute not only to competitive performance but also to reducing injury risk. In fact, our findings revealed a reduction in both mild and severe injuries, aligning with previous studies that highlight the protective role of isometric strengthening against ankle sprains [
27]. Thus, this study underscores the dual benefit of such training approaches in simultaneously improving athletic performance and supporting injury prevention strategies [
28,
29].
The absence of statistically significant differences in the Lunge Test between legs and in the L-Test between COD sides across all assessment points suggests that the isometric training protocol produced balanced effects, suggesting minimal performance asymmetries. This symmetry aligns with findings from previous studies reporting uniform improvements following bilateral and directional training interventions, in which structured protocols yielded balanced neuromuscular adaptations across limbs and COD sides [
30]. Similarly, Minoonejad et al. [
8] emphasized the role of neuromuscular exercises in restoring bilateral balance symmetry and improving postural control, critical factors in reducing the risk of recurrent ankle injuries. This lack of asymmetry is particularly relevant, as prior research has linked performance imbalances to an increased risk of injury and reduced athletic efficiency [
30]. The specificity of the isometric training protocol, which equally targeted both legs and COD sides, likely contributed to this uniform adaptation. However, percentage improvements in the Lunge Test differed between limbs, with greater gains observed in the left leg (14–34%) compared to the right (4–20%).
These asymmetric responses may reflect pre-existing differences in joint mobility, flexibility, or neuromuscular coordination. Unlike the L-Test, which involves bilateral coordination, the Lunge Test isolates unilateral performance, potentially amplifying inter-limb variability. Comparable patterns have been observed in team sports athletes, particularly in tasks such as lung or jump, where baseline asymmetries influence the magnitude of adaptation [
31].
This study presents several limitations. First of all, the absence of a control group limits the ability to isolate the specific effects of the isometric intervention program from those of concurrent in-season training activities. As participants were professional athletes who maintained their regular competitive routines, it is possible that other training stimuli contributed to the observed improvements. Although this design reflects the ecological conditions of elite sport, it potentially limits the internal validity of the findings. Additionally, variability in injury history and baseline fitness levels may have influenced individual responses, potentially introducing further variability into the outcomes. Nevertheless, measurement reproducibility was supported by low SEM, SRD, and CV% values for both the Lunge Test and the L-Test, confirming the precision and reliability of the outcome measures.
Another important methodological limitation pertains to the second gym-based isometric exercise (elevated hold with external load), in which the degree of heel elevation was not strictly controlled. Variations in heel height may have affected ankle stability, potentially influencing agility outcomes in the L-Test. Additionally, the use of wall-based exercises with elastic resistance represents a key limitation, as force generation occurred against a non-rigid surface. Although the exercises were intended as isometric contractions at approximately 80% MVC, the compliance of the wall and elastic setup resulted in quasi-isometric contractions. This likely reduced the precision of force steadiness and introduced variability in neuromuscular responses [
32]. Despite the provision of real-time verbal feedback and individualized targets, these conditions may have altered both the mechanical demands and the corresponding adaptive responses. Moreover, although trunk stabilization likely contributed to improvements in both L-Test performance and isometric exercise execution, core strength was not directly assessed in this study. As a result, the extent to which gains in COD ability were mediated by adaptations in trunk musculature remains unclear. Future research should address these limitations by incorporating control groups, monitoring overall training loads, rigorously controlling biomechanical parameters (e.g., heel elevation), using rigid measurement setups (e.g., force plates or dynamometers), and assessing core strength to better elucidate the mechanisms underlying performance improvements associated with isometric training.