Prosthetic Devices for Adaptative Sport in Pediatrics: A Narrative Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection Process
2.4. Data Extraction Synthesis
3. Results
3.1. Nature of Pediatric Limb Deficiencies and Impacts in Prosthetic Use: Congenital and Acquired Amputations
3.2. Prosthetics in Children
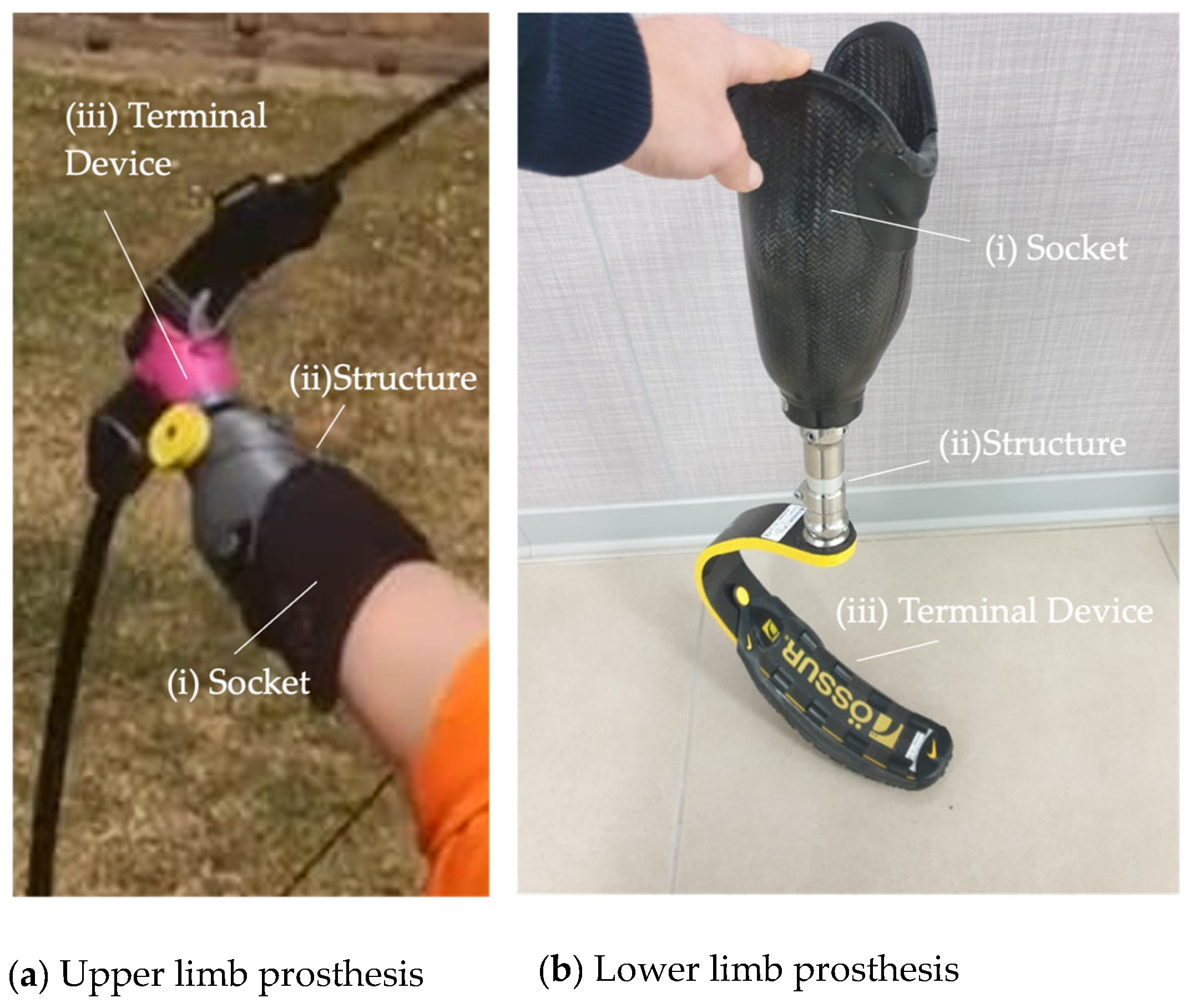
3.2.1. Nomenclature of Prosthetic Devices
3.2.2. Current Barriers in the Field of Pediatric Prosthetics
Functionality of the Device
Prosthetic Comfort
Economic Barriers
3.3. Timing of Prosthetic Fit
3.4. Activity-Specific Prostheses
3.4.1. Upper-Limb Prostheses
Commercially Available Prosthetic Terminal Devices
Classification of Activities
3.4.2. Lower-Limb Prostheses
Amputation Levels and Prosthetic Implications
Above Knee Amputation
Below Knee (or Transtibial) Amputation
Foot Amputation
Running-Specific Prostheses (RSPs) and Alternative Solutions
3.5. Current Role of Myoelectric Devices and Innovative Methods
4. Discussion
4.1. Activity-Specific Prostheses: Current Landscape and Conflict Findings
- Multifactorial Determinants of Prosthetic Use
- Capacity vs. Performance: Real-World Use
4.2. Gaps in Pediatric Activity-Specific Prosthetic Design
4.2.1. Adult-to-Pediatric Design Limitation
4.2.2. Gaps in Pediatric-Specific Biomechanical Research
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Borne, A.; Porter, A.; Recicar, J.; Maxson, T.; Montgomery, C. Pediatric Traumatic Amputations in the United States: A 5-Year Review. J. Pediatr. Orthop. 2017, 37, e104–e107. [Google Scholar] [CrossRef] [PubMed]
- Louer, C.R.; Scott-Wyard, P.; Hernandez, R.; Vergun, A.D. Principles of Amputation Surgery, Prosthetics, and Rehabilitation in Children. J. Am. Acad. Orthop. Surg. 2021, 29, E702–E713. [Google Scholar] [CrossRef]
- Milteer, R.M.; Ginsburg, K.R.; Council on Communications and Media Committee on Psychosocial Aspects of Child and Family Health; Mulligan, D.A.; Ameenuddin, N.; Brown, A.; Christakis, D.A.; Cross, C.; Falik, H.L.; Hill, D.L.; et al. The importance of play in promoting healthy child development and maintaining strong parent-child bond: Focus on children in poverty. Pediatrics 2012, 129, e204–e213. [Google Scholar] [CrossRef]
- Kanas, J.A.L.; Holowka, M. Adaptive upper extremity prostheses for recreation and play. J. Pediatr. Rehabil. Med. 2009, 2, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, B.S.; Lamy, M.; Cameron, D.; Artero, L.; Ramdial, S.; Leineweber, M.; Andrysek, J. Factors impacting participation in sports for children with limb absence: A qualitative study. Disabil. Rehabil. 2018, 40, 1393–1400. [Google Scholar] [CrossRef] [PubMed]
- Hadj-Moussa, F.; Zahid, H.B.; Wright, F.V.; Kelland, K.; Andrysek, J. ‘It’s more than just a running leg’: A qualitative study of running-specific prosthesis use by children and youth with lower limb absence. Disabil. Rehabil. 2022, 44, 7190–7198. [Google Scholar] [CrossRef] [PubMed]
- Agnew, S.; Geil, M.D.; Gharai, M.H. Dynamic Stiffness of Pediatric Prostheses During Rapid Loading. J. Prosthet. Orthot. 2020, 32, 245–250. [Google Scholar] [CrossRef]
- McQuerry, J.; Gammon, L.; Carpiaux, A.; Talwalkar, V.; Iwinski, H.; Walker, J.; Jacobs, C.A.; Muchow, R. Effect of Amputation Level on Quality of Life and Subjective Function in Children. J. Pediatr. Orthop. 2019, 39, e524–e530. [Google Scholar] [CrossRef]
- Westberry, D.E. State of the Art: Amputation and Prosthetics. J. Pediatr. Orthop. 2017, 37, S22–S25. [Google Scholar] [CrossRef]
- Griffet, J. Amputation and prosthesis fitting in paediatric patients. Orthop. Traumatol. Surg. Res. 2016, 102, S161–S175. [Google Scholar] [CrossRef]
- Kopová, B.; Bakeš, M.; Čížek, M.; Horký, A.; Dvořák, J.; Ráž, K.; Chval, Z. Development and Production of a Children’s Upper-Limb Cycling Adapter Using 3D Printing. Materials 2024, 17, 4731. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.L.; Coburn, T.R.; Cottle, W.; Burke, C.; Talwalkar, V.R. Recreational Terminal Devices for Children With Upper Extremity Amputations. J. Pediatr. Orthop. 2008, 28, 271–273. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.J.; Cummings, D.R.; Welling, R.I.; Kaleta, M.K.; Koenig, K.D.; Laine, J.C.; Morgan, S.J. Current Concept Review Essentials of Pediatric Prosthetics. J. Pediatr. Orthop. Soc. N. Am. 2020, 2, 168. [Google Scholar] [CrossRef]
- Day, H.J.B. The ISO/ISPO classification of congenital limb deficiency. J. Prosthet. Orthot. Int. 1991, 15, 67–69. [Google Scholar] [CrossRef]
- Yiİĝiİter, K.; Ülger, Ö.; Şener, G.; Akdoğan, S.; Erbahçeci, F.; Bayar, K. Demography and function of children with limb loss. Prosthet. Orthot. Int. 2005, 29, 131–138. [Google Scholar] [CrossRef]
- Seelman, K.D.; Seelman, K.D. The World Health Organization/World Bank’s first World Report on Disability. Int. J. Telerehabil. 2011, 3, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Krajbich, J.I. Lower-limb deficiencies and amputations in children. J. Am. Acad. Orthop. Surg. 1998, 6, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Cordella, F.; Ciancio, A.L.; Sacchetti, R.; Davalli, A.; Cutti, A.G.; Guglielmelli, E.; Zollo, L. Literature review on needs of upper limb prosthesis users. Front. Neurosci. 2016, 10, 209. [Google Scholar] [CrossRef]
- Trent, L.; Intintoli, M.; Prigge, P.; Bollinger, C.; Walters, L.S.; Conyers, D.; Miguelez, J.; Ryan, T. A narrative review: Current upper limb prosthetic options and design. Disabil. Rehabil. Assist. Technol. 2020, 15, 604–613. [Google Scholar] [CrossRef]
- Egermann, M.; Kasten, P.; Thomsen, M.; Thomsen, M. Myoelectric hand prostheses in very young children. Int. Orthop. 2009, 33, 1101–1105. [Google Scholar] [CrossRef]
- Battraw, M.A.; Fitzgerald, J.; Joiner, W.M.; James, M.A.; Bagley, A.M.; Schofield, J.S. A review of upper limb pediatric prostheses and perspectives on future advancements. J. Prosthet. Orthot. Int. 2022, 46, 267–273. [Google Scholar] [CrossRef] [PubMed]
- James, M.A.; Bagley, A.M.; Brasington, K.; Lutz, C.; Mcconnell, S.; Molitor, F. Impact of Prostheses on Function and Quality of Life for Children with Unilateral Congenital Below-the-Elbow Deficiency. J. Bone Joint Surg. Am. 2006, 88, 2356–2365. [Google Scholar] [CrossRef] [PubMed]
- Davids, J.R.; Wagner, L.V.; Meyer, L.C.; Blackhurst, D.W. Prosthetic Management of Children with Unilateral Congenital Below-Elbow Deficiency. J. Bone Joint Surg. Am. 2006, 88, 1294–1300. [Google Scholar] [CrossRef]
- Manocchio, N.; Gaudenzi, M.; Tofani, M.; Ljoka, C.; Imeshtari, A.; Giordani, L.; Della Bella, G.; Foti, C. Functional Impact of Early Prosthetic Implantation in Children with Upper Limb Agenesis or Amputation. Appl. Sci. 2024, 14, 7259. [Google Scholar] [CrossRef]
- Meurs, M.; Maathuis, C.G.B.; Lucas, C.; Hadders-Algra, M.; van der Sluis, C.K. Prescription of the first prosthesis and later use in children with congenital unilateral upper limb deficiency: A systematic review. Prosthet. Orthot. Int. 2006, 30, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Geil, M.D.; Safaeepour, Z.; Giavedoni, B.; Coulter, C.P. Walking kinematics in young children with limb loss using early versus traditional prosthetic knee prescription protocols. PLoS ONE 2020, 15, e0231401. [Google Scholar] [CrossRef]
- Hadj-Moussa, F.; Ngan, C.C.; Andrysek, J. Biomechanical factors affecting individuals with lower limb amputations running using running-specific prostheses: A systematic review. Gait Posture 2022, 92, 83–95. [Google Scholar] [CrossRef]
- Medina-Coello, P.; Salvador-Domínguez, B.; Badesa, F.J.; Rodríguez Corral, J.M.; Plastrotmann, H.; Morgado-Estévez, A. Anthropomorphic Robotic Hand Prosthesis Developed for Children. Biomimetics 2024, 9, 401. [Google Scholar] [CrossRef] [PubMed]
- Zuniga, J.; Katsavelis, D.; Peck, J.; Stollberg, J.; Petrykowski, M.; Carson, A.; Fernandez, C. Cyborg beast: A low-cost 3d-printed prosthetic hand for children with upper-limb differences. BMC Res. Notes 2015, 8, 10. [Google Scholar] [CrossRef]
- Patralekh, M.K.; Mohanta, S.; Lal, H. Role of 3D printing in sports and prosthetics. In Additive Manufacturing Materials and Technology; Elsevier: Amsterdam, The Netherlands, 2024; pp. 341–357. [Google Scholar] [CrossRef]
- Stucki Rauch, A.; Cieza, A.; Stucki, G. How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur. J. Phys. Rehabil. Med. 2008, 44, 329–342. [Google Scholar]
- Tofani, M.; Mustari, M.; Tiozzo, E.; Dall’oGlio, I.; Morelli, D.; Gawronski, O.; Salata, M.; Cantonetti, L.; Castelli, E.; Di Lallo, D.; et al. The development of the International Classification of Functioning, Disability and Health for Child and Youth (ICF-CY) Core Sets: A systematic review. Disabil. Rehabil. 2023, 45, 3951–3960. [Google Scholar] [CrossRef]
- Della Bella, G.; Santecchia, L.; Luttazi, P.; Mariani, G.; Pochiero, L.; Lacopo, A.; Delia, C.; Tofani, M. The Use of ABILHAND-Kids in Children with Unilateral Congenital Below-Elbow Deficiencies and Acquired Amputation: An Italian Cross-Sectional Study. Children 2024, 11, 988. [Google Scholar] [CrossRef] [PubMed]
- Santecchia, L.; Della Bella, G.; Caspi, F.; Luttazi, P.; Pochiero, L.; Taffoni, F.; Mariani, G.; Gaudenzi, M.; Valente, D.; Tofani, M. Child Amputee Prosthetics Project-Prosthesis Satisfaction Inventory (CAPP-PSI): Validation of Italian Version in Children with Upper Limb Amputation. Children 2025, 12, 130. [Google Scholar] [CrossRef]
- Tiele, A.; Soni-Sadar, S.; Rowbottom, J.; Patel, S.; Mathewson, E.; Pearson, S.; Hutchins, D.; Head, J.; Hutchins, S. Design and development of a novel upper-limb cycling prosthesis. Bioengineering 2017, 4, 89. [Google Scholar] [CrossRef]
- Oudenhoven, L.M.; Boes, J.M.; Hak, L.; Faber, G.S.; Houdijk, H. Regulation of step frequency in transtibial amputee endurance athletes using a running-specific prosthesis. J. Biomech. 2017, 51, 42–48. [Google Scholar] [CrossRef]
- Shultz, A.H.; Lawson, B.E.; Goldfarb, M.; Goldfarb, M. Running with a powered knee and ankle prosthesis. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 403–412. [Google Scholar] [CrossRef]
- Guzelbulut, C.; Suzuki, K.; Shimono, S.; Hobara, H. Shape Optimization of Running Specific Prosthesis Based on Force-Displacement Characteristics. In Proceedings of the 13th Conference of the International Sports Engineering Association, Basel, Switzerland, 22–26 June 2020; Volume 49, p. 7. [Google Scholar] [CrossRef]
- Dyer, B.; Dyer, B. Development of high performance parasport prosthetic limbs: A proposed framework and case study. Assist. Technol. 2020, 32, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Dyer, B.; Glithro, R.; Batley, A.; Batley, A. The design of an upper arm prosthesis utilising 3D printing conceived for the 2020 Tokyo paralympic games: A technical note. J. Rehabil. Assist. Technol. Eng. 2022, 9, 20556683221113309. [Google Scholar] [CrossRef] [PubMed]
- Dyer, B.; Woolley, H.; Woolley, H. Development of a high-performance transtibial cycling-specific prosthesis for the London 2012 Paralympic Games. Prosthet. Orthot. Int. 2017, 41, 498–502. [Google Scholar] [CrossRef]
- Dyer, B.; Disley, B.X.; Disley, B.X. The aerodynamic impact of a range of prostheses designs when cycling with a trans-tibial amputation. Disabil. Rehabil. Assist. Technol. 2020, 15, 577–581. [Google Scholar] [CrossRef]
- Dyer, B.T.; Deans, S.A.; Deans, S.A. Swimming with limb absence: A systematic review. J. Rehabil. Assist. Technol. Eng. 2017, 4, 2055668317725451. [Google Scholar] [CrossRef] [PubMed]
- Beck, O.N.; Taboga, P.; Grabowski, A.M.; Grabowski, A.M. Characterizing the Mechanical Properties of Running-Specific Prostheses. PLoS ONE 2016, 11, e0168298. [Google Scholar] [CrossRef]
- Rahnama, L.; Soulis, K.; Geil, M.D.; Geil, M.D. A review of evidence on mechanical properties of running specific prostheses and their relationship with running performance. Front. Rehabil. Sci. 2024, 5, 1402114. [Google Scholar] [CrossRef] [PubMed]
- Allen, S.P.; Diaz, G.B.; Grabowski, A.M.; Grabowski, A.M. The Effect of Unequal Crank Arm Lengths and Cycling-Specific Prostheses for Recreational Riders with a Transtibial Amputation. Med. Sci. Sports Exerc. 2024, 56, 1976–1987. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, T.; Oreste, A.; Hutnick, G.; Chory, A.; Chehata, V.; Seldin, J.; Gallo, M.D.; Bloom, O. A Pilot Study Testing a Novel 3D Printed Amphibious Lower Limb Prosthesis in a Recreational Pool Setting. PMR 2020, 12, 783–793. [Google Scholar] [CrossRef]
- Molino, J.; Rodriguez, M.; Cárdenas, M. Design of a cost-effective swimming prosthesis for transtibial amputee patients. Gente Clave 2022, 6, 9–22. [Google Scholar]
- De Luigi, A.J.; Cooper, R.A. Adaptive sports technology and biomechanics: Prosthetics. PMR 2014, 6, S40–S57. [Google Scholar] [CrossRef]
- Willwacher, S.; Funken, J.; Heinrich, K.; Müller, R.; Hobara, H.; Grabowski, A.M.; Brüggemann, G.-P.; Potthast, W. Elite long jumpers with below the knee prostheses approach the board slower, but take-off more effectively than non-amputee athletes. Sci. Rep. 2017, 7, 16058. [Google Scholar] [CrossRef]
- Grabowski, A.M.; McGowan, C.P.; McDermott, W.J.; Beale, M.T.; Kram, R.; Herr, H.M. Running-specific prostheses limit ground-force during sprinting. Biol. Lett. 2010, 6, 201–204. [Google Scholar] [CrossRef]
- Rigney, S.M.; Simmons, A.; Kark, L.; Kark, L. Mechanical characterization and comparison of energy storage and return prostheses. Med. Eng. Phys. 2017, 41, 90–96. [Google Scholar] [CrossRef]
- Eshraghi, A.; Safaeepour, Z.; Geil, M.D.; Andrysek, J. Walking and balance in children and adolescents with lower-limb amputation: A review of literature. Clin. Biomech. 2018, 59, 181–198. [Google Scholar] [CrossRef] [PubMed]
- Taboga, P.; Grabowski, A.M. Axial and torsional stiffness of pediatric prosthetic feet. Clin. Biomech. 2017, 42, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Herbaut, A.; Chavet, P.; Roux, M.; Guéguen, N.; Gillet, C.; Barbier, F.; Simoneau-Buessinger, E. The influence of shoe drop on the kinematics and kinetics of children tennis players. Eur. J. Sport. Sci. 2016, 16, 1121–1129. [Google Scholar] [CrossRef] [PubMed]



| Search Strings | Last Search Date |
|---|---|
| (prosthes* OR device) AND children AND sports | 20 March 2025 |
| (“pediatric prostheses”) AND sports | 20 March 2025 |
| “Prostheses AND (“recreational activities”) AND children” | 20 March 2025 |
| “Prostheses AND sports AND children” | 20 March 2025 |
| “Auxiliary AND sports AND children” | 20 March 2025 |
| (“acquired amputation” OR congenital amputation” OR “congenital limb deficiency”) AND (“sports participation”) | 20 May 2025 |
| Prostheses AND sports AND children AND “3D printing” AND “additive manufacturing”) | 20 May 2025 |
| Prosthetic AND (hand OR leg OR foot OR feet OR limb) AND children AND (sports OR “recreational activities” OR running OR swimming OR bicycle OR “table tennis”) | 22 May 2025 |
| (Prostheses OR prosthetics) AND (children OR pediatric) AND limb AND (sports OR “recreational activities” OR running OR swimming OR bicycle OR) | 22 May 2025 |
| (prosthesis OR prostheses OR device) AND amputation AND deficiency AND (sports OR “recreational activities” OR running) AND (children OR pediatric) AND limb | 22 May 2025 |
| “Artificial Limbs” [MAJR] AND children | 22 May 2025 |
| Type of Prostheses | Study (Author, Year) | Type of Article | Study Design/Scope | Population (N, Age) or Method | Sport(s) | Type of Amputation | Prosthetic Device | Outcome Measures Covered | Key Findings/Conclusions | Exposed Limitations/Gaps | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Etiology | Laterality | Level of Amputation | ||||||||||
| Lower limb | Hadj-Moussa et al., 2022 [6] | O.R.A | Qualitative cross-sectional study | Children and youth (8 participants [8–20 y.o.]). | Running (track, field, cross-country), basketball, gym | Congenital, acquired | Unilateral (n = 5), bilateral (n = 3) | Knee (n = 1), transtibial (n = 6), ankle (n = 1) | RSPs | Impact of RSP in sport and physical activity participation. Benefits and limitations of their use compared to DUPs. | Advantages of RSPs include jumping. Limitations involve running and jogging at different speeds and long periods of time. | Financial barriers. Limited studies that approach RSPs. |
| Agnew et al., 2020 [7] | O.A | Innovative Study | Mechanical testing methods for simulation. | NR | NR | NR | NR | College Park: Truper, Ossur: Cheetah Junior, Flex-Foot Junior, Vari-Flex Junior. | Simulation of single-leg drop-landing with four pediatric prosthetic feet from two heights and two contact orientations. | All prosthetic feet were stiffer for flatfoot. The Ceetah was the least sensitive to foot angle, while the Flex-Foot Junior and Truper showed the greatest values of stiffness for flatfoot. Individual feet showed different stiffness, but differences were not significant of height changes. | The four prosthetic feet had different intrinsic functionalities when applied in sports contexts. Prosthetic feet are often the result of re-dimensioned adult prostheses. | |
| McQuerry et al., 2019 [8] | O.A | Qualitative cross-sectional study | Infants, children, and adolescents [96 participants (0–21 y.o.)]. | NR | Congenital (n = 78), acquired (n = 18) | Unilateral (n = 84), bilateral (n = 12) | Transfemoral (n = 9) Knee (n = 27), Transtibial (n = 21), Ankle (n = 39) | Defined as low-end or high-end, based on L-code. | Subjective perception of function based on amputation level using PODCI scores. | Better sport/physical functioning scores for ankle-level compared to knee-level amputation. Congenital and acquired amputees showed similar outcomes. Bilateral knee amputees had significantly worse outcomes in transfers of sport/physical functioning compared to ULA. | Limited data comparing functionality for different levels of amputation, specially for causes other than osteosarcoma. | |
| Westberry 2017 [9] | N.R | State of the art (1983–2015) | Children. | Running and swimming mentioned | NR | NR | _ † | _† | Residual limb deformities and prosthetic management. Fabrication and performance of these devices. | Importance of an adequate residual limb. Fitting of initiates with a simple device and follows a gradual transition. | Financial demands during lifespan suppose a limit. Molding and manufacturing should use CAD/CAM systems. | |
| Griffet, 2016 [10] | N.R | Literature Overview (1998–2011) | Infants, children, and adolescents. | Multi-sport | Congenital, acquired | NR | Hip, femur, tibia, foot | C-leg Ottobock, Genium leg Ottobock, commercially available sport-specific TDs. | Amputation surgery, fitting of prosthetic devices, performance, and rehabilitation. | Adaptation of a prosthesis requires a disciplinary team, periodic evaluations, imaging, and GA. Specific evaluation for ASPs. | Lack of literature on the psychological impact of amputation. Fitting of prostheses in children adapts to their growth. Difference in performance between feet and below-knee prostheses. | |
| Upper limb | Kopova’ et al., 2024 [11] | O.A | Innovative study | Children (3 participants [4–5 y.o.]). | Cycling | NR | NR | _ † | Innovative device. | Design and implementation of a low-cost upper-limb cycling adapter for young children with a 360º rotation around arm axis. | Use of FDM and MJF as the 3DP technique. Bicycle adapter consists of a rotational eight-tooth mechanism and a grasping end. Flexion and pronation enabled. Nanomaterials as a future proposal. | FDM presented quality limitations. Testing and evaluation performed without the wrist mechanism. |
| Kanas et al., 2009 [4] | N.R | Literature Overview (1998–2009) | Children. | Multi-sport | NR | NR | _ † | TRS-manufactured ASPs. | Technical and functional aspects of activity-specific TDs for children in a variety of sports and activities. | TD choice must consider different aspects. Classification of ASPs. Prescription of these devices requires reaching certain milestones. Type of prosthetic components and their use. | Issues reported on the cost of the ASP, age and size of the user, and its use in certain activities. Reported lack of documentation of TDs and their designs. | |
| Walker et al., 2008 [12] | O.A | Qualitative cross-sectional study | Children (11 participants [4–16 y.o.]). | Multi-sport | Congenital (n = 10), Traumatic (n = 1) | Unilateral (n = 10), bilateral (n = 1). Unilateral prosthetization only. | Proximal third of the forearm (n = 4), middle third of the forearm (n = 3), wrist (n = 2), hand (n = 2) | Commercially available ASPs (TRS-manufactured and others). | Successful users evaluation through a chart review and patient survey. | TDs for weight-lifting and violin-playing adaptations were reported as being beneficial to the user’s performance. Age differences between successful and unsuccessful users. Effect of level of amputation on reported success. Relevance of the use of one or two limbs in bimanual activities on the outcome. | Lack of sensorial input and feedback in current ULPs can affect outcomes in certain activities. | |
| Both upper and lower limbs | Louer et al., 2021 [2] | N.R | Literature Overview (1975–2020) | Children. | NR | Traumatic | Unilateral and bilateral | _ † | _ † | Surgical principles in pediatric amputation, recovery timeline. Pain/complaints of prosthetic fits and possible causes. Timing of prosthetic use in ULA and LLA in pediatric congenital deficiencies. | Importance of quality amputation in growing children. Factors impacting adaptation of the prostheses and timing of prosthetic introduction for DUPs and ASPs. | A prosthesis lasts a child 12–18 months. Surgical approaches and prosthetization are limited to the growing characteristics of the pediatric patient. |
| Hall et al., 2020 [13] | N.R | Current Concept Review (1972–2020) | Infants, children, and adolescents. | NR | NR | Unilateral and bilateral | _ † | _ † | Timing and future function of prosthetic devices. Prosthetic options and terminology. | Requirements for proper prosthetic use and timing of its fitting. Characteristics of the residual limb needed for an adequate prosthetization. | ASPs are not considered “medically necessary” and are not covered by insurance. | |
| Ahmed et al., 2018 [5] | O.A | Qualitative study | Children and adolescents [11 participants (6–14 y.o.)] and parents. | Multi-sports | Congenital (n = 11) | NR | Upper deficiencies: elbow (n = 1), trans-radial (n = 3), Hand (n = 2) Lower deficiencies: transtibial (n = 4), transfemoral (n = 1) | _ † | Interviews with children with and without parents. Functionality, capabilities, stigma and social environment, interest for sport, and investment involved. | Variability in reported functionality of the prosthetic device. | Cost of ASPs. Sampling bias mentioned as a possible limitation. Lack of comparative studies between children who do not engage in sport activities and does who do. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vila, C.B.; Stella, G.; Pauciulo, F.; Tofani, M.; Delia, C.; Canzano, L.; Luttazi, P.; Cerretani, C.; Della Bella, G. Prosthetic Devices for Adaptative Sport in Pediatrics: A Narrative Review. Appl. Sci. 2025, 15, 9652. https://doi.org/10.3390/app15179652
Vila CB, Stella G, Pauciulo F, Tofani M, Delia C, Canzano L, Luttazi P, Cerretani C, Della Bella G. Prosthetic Devices for Adaptative Sport in Pediatrics: A Narrative Review. Applied Sciences. 2025; 15(17):9652. https://doi.org/10.3390/app15179652
Chicago/Turabian StyleVila, Clàudia Bigas, Giulia Stella, Federica Pauciulo, Marco Tofani, Caterina Delia, Loredana Canzano, Paola Luttazi, Cecilia Cerretani, and Gessica Della Bella. 2025. "Prosthetic Devices for Adaptative Sport in Pediatrics: A Narrative Review" Applied Sciences 15, no. 17: 9652. https://doi.org/10.3390/app15179652
APA StyleVila, C. B., Stella, G., Pauciulo, F., Tofani, M., Delia, C., Canzano, L., Luttazi, P., Cerretani, C., & Della Bella, G. (2025). Prosthetic Devices for Adaptative Sport in Pediatrics: A Narrative Review. Applied Sciences, 15(17), 9652. https://doi.org/10.3390/app15179652






