Abstract
Background: Between 2014 and 2024, Poland underwent a significant digital transformation in its healthcare sector, evolving from isolated initiatives to a cohesive national eHealth ecosystem. This review examines the development, clinical significance, and research trends in telemedicine in Poland, providing comparative insights from 1995 to 2015 and assessing the impact of the COVID-19 pandemic. Methods: A narrative review was conducted using the PubMed, Scopus, EMBASE, and Web of Science databases to identify peer-reviewed articles published between January 2014 and December 2024. A total of 1012 records were identified, and 212 articles were included after applying predefined inclusion criteria. These articles were categorized by medical specialty, study type, COVID-19 relevance, and clinical versus nonclinical focus. Gray literature and policy reports were examined only to provide a context for the findings. Results: Ninety-six publications were included in the clinical studies. The most common specialties are cardiology, psychiatry, geriatrics, general practice, and rehabilitation. In earlier years, survey-based and observational designs were predominant, whereas later years saw an increase in interventional trials and studies enabled by Artificial Intelligence (AI). The COVID-19 pandemic has had a significant impact on research activity, accelerating the adoption of digital technologies in previously underrepresented fields, such as pulmonology and palliative care, as well as in the routine use of modern Internet communication technologies for daily patient–doctor interactions. Discussion: Advancements in digital health (including eHealth and telemedicine) in Poland have been driven by policy reforms, technological advancements, and epidemiological events, such as COVID-19. Various fields have evolved from feasibility studies to clinical trials, and emerging specialties have focused on user experience and implementation. However, the adoption of AI and its interoperability remains underdeveloped, primarily because of regulatory and reimbursement challenges. Conclusions: Poland has made significant strides in institutionalizing digital health; however, ongoing innovation necessitates regulatory alignment, strategic funding, and enhanced collaboration between academia and industry. As the country aligns with the European Union (EU) initiatives, such as the European Health Data Space, it has the potential to lead to regional integration in digital health.
1. Introduction
Digital health encompasses various technologies, including artificial intelligence (AI) in healthcare, telemedicine, eHealth, big data analytics, and connected devices, which are transforming the way care is delivered, making it more efficient, personalized, and accessible [1,2]. It also encompasses AI, wearable devices, and mobile health (mHealth). The digital transformation of healthcare has profoundly altered the delivery, access, and management of services across Europe [3,4]. Telemedicine is defined as the use of communications networks for delivering healthcare services and medical education from one geographic location to another, designed to overcome issues like uneven resource distribution and accessibility barriers [5,6,7]. It typically involves real-time, two-way communication between a patient and a healthcare provider for clinical purposes, such as consultation, diagnosis, and treatment [8]. Telemedicine refers more specifically to the provision of healthcare services at a distance, including diagnosis, treatment, prevention, and health education, through the use of telecommunication technologies [9,10,11]. It involves recent, rather real-time, or rarely asynchronous interactions [12] between healthcare professionals and patients (or between professionals). It is recognized in Poland as a regulated form of medical service.
Both definitions by the European Commission’s eHealth framework and proposed earlier by the Polish Telemedicine Society, which adds medical professional liability to the definition of real telemedicine [13], are followed. eHealth is defined as ‘the use of information and communication technologies locally and at a distance’ to support and enhance healthcare, public health, and health education [14,15]. Digital health transformation reshapes how health services are delivered, public health is protected, and chronic disease is managed and prevented [16,17].
In Poland, telemedicine and eHealth have played a central role in this shift, driving a decade-long evolution toward more accessible, efficient, and patient-centered care [18,19,20]. Between 2014 and 2024, Poland transitioned from fragmented digital health initiatives to a nationally coordinated eHealth (digital health) ecosystem [19,20,21]. This system integrates teleconsultations, remote monitoring, telerehabilitation, Electronic health records (EHRs), electronic prescriptions (e-prescriptions), mobile applications, and artificial intelligence (AI) tools for healthcare delivery [20,22]. This progress was propelled by a combination of policy, technological, and epidemiological factors. Telemedicine refers to the delivery of healthcare services at a distance using information and communication technology (ICT) [8,11,23]. eHealth encompasses broader digital health solutions including EHRs and decision-support systems [15,24,25]. The definitions used align with those of the WHO and European Commission (e.g., eHealth Action Plan 2012–2020). However, the definition of telemedicine proposed by the Polish Telemedicine Society before 2000 also addresses medical professional liability, which primarily distinguishes it from other forms of digital health [26]. This has recently been recognized by the EU [27]. Initially, telemedicine efforts in Poland led by academic centers or innovative clinicians lacked systemic integration [19,22,28]. The digitization of healthcare in Poland has thus far been not only technological but also regulatory. A breakthrough occurred in December 2015, when formal regulations enabling the use of telemedicine services were introduced into Polish law [18]. These changes are crucial for further development and institutionalization of digital health services. A pivotal transformation occurred with the legalization of teleconsultations, followed by the implementation of mandatory e-prescriptions, alongside e-referrals and the Internet Patient Account (IKP) [29,30,31,32]. These developments were facilitated by structural funding from the Ministry of Health (MH), National Health Fund (NFZ), and European Union (EU) structural funding [18,22,33]. Digital health initiatives were initially confined to academic experimentation and institutional solutions. However, by the mid-2010s, the formal legalization of teleconsultations and the establishment of nationwide platforms laid the foundation for a cohesive digital health infrastructure supported by EU funding and domestic policy frameworks [18]. The COVID-19 pandemic has accelerated the adoption of digital tools and telemedicine in primary and specialist care, demonstrating the adaptability of the Polish health system and highlighting challenges in interoperability, access, digital literacy, and regulations [34,35,36,37]. The pandemic spurred widespread adoption of telehealth across various clinical domains, with notable growth in psychiatry [38], cardiology [39], geriatrics [40], and rehabilitation [41], including increased use of mobile health applications [42,43,44,45,46] and AI-assisted diagnostics [47]. Healthcare stakeholders respond to scaling services and establishing standards for remote care.
This study aimed to analyze telemedicine and eHealth research in Poland from 2014 to 2024 by exploring thematic trends, clinical relevance, and digital health initiatives across various medical specialties. By comparing this period with 1995–2015 [28], this study assesses the maturity of Poland’s digital health ecosystem and identifies key challenges and opportunities. It examines thematic trends and clinical relevance, situating the country’s progress within a broader European context. This study seeks to synthesize trends, research areas, and the involvement of specialists across diverse medical fields where telemedicine and eHealth solutions have been implemented in Poland during the specified period. It identifies the enablers, barriers, and opportunities for regional leadership in digital health innovation.
2. Materials and Methods
A comprehensive and structured literature search was conducted using four major databases: PubMed, EMBASE, Scopus, and Web of Science.
2.1. Search Strategy and Data Sources
The search terms included combinations of “telemedicine,” “eHealth,” “digital health,” AND “Poland,” using Boolean operators (AND, OR). The search was limited to English-language publications. The initial query identified 1012 records, of which 852 were published between 2014 and 2024. After restricting the results to this timeframe and conducting deduplication and relevance screening, a final dataset comprising 212 peer-reviewed publications was selected for in-depth review. Duplicates were removed using EndNote’s deduplication function, followed by manual screening to ensure accuracy.
Based on the number of articles on specific specializations and fields, the most frequently represented ones (four or more articles from a given specialization) were selected, and field-specific comments were added. For comparison, the remaining articles (three or fewer articles) were analyzed and described collectively with references to Supplementary Table S1. To enrich the dataset and provide a policy context, the national context was considered based on gray literature, national reports, and strategic policy documents using targeted searches in the Semantic Scholar database, digital archives of the MH, NFZ, and Center of eHealth (formerly Central Center for Information and Health Systems (CSIOZ), and selected European health repositories. However, these studies were excluded from analysis.
2.2. Inclusion and Exclusion Criteria
Studies were eligible for inclusion if they met the following criteria:
- Centered in Poland, with a focus on telemedicine, eHealth, and digital health.
- The peer-reviewed articles focused on the implementation, evaluation, and development of the field.
- Reported on empirical data, pilot project results, implementation outcomes, and health policy evaluations.
- Provided insights into clinical outcomes, patient satisfaction, technological development, or institutional adoption.
- Clinical studies, pilot programs, policy evaluations, and health technology assessments.
The exclusion criteria were as follows:
- The studies were conducted entirely outside of Poland.
- Technical or engineering reports with no clinical or policy relevance.
- Editorials, conference-only publications, opinion pieces, or articles lacking empirical or methodological content.
- Studies unrelated to the Polish healthcare system.
- Purely technical articles lacking clinical or health system relevance.
2.3. Data Extraction and Classification
Two independent reviewers screened titles and abstracts to ensure their relevance. Disagreements were resolved through discussions or third-party arbitration. Full-text articles were assessed for study type, clinical focus, and relevance to the national health transformation. The extracted metadata are as follows:
- Journal and publication year.
- Study type (e.g., trial, review, survey, cross-sectional).
- Medical specialty (e.g., psychiatry, cardiology, and geriatrics).
- Intervention type (e.g., teleconsultation, AI diagnostics, mHealth).
- Clinical versus non-clinical categories.
- COVID-19 relationship (if applicable).
Conflicts in the data extraction were resolved by consensus or adjudication by a third reviewer. Descriptive statistics and thematic coding were used to identify specific trends, temporal shifts, and the impact of significant policy changes or events such as the COVID-19 pandemic. Visualizations were created to depict trends in publication frequency, specialty engagement, and evolution of study types.
Regardless of the structure of the narrative review studies, the PRISMA flowchart (Figure 1) was developed to emphasize compliance with the rigorous research methodology.
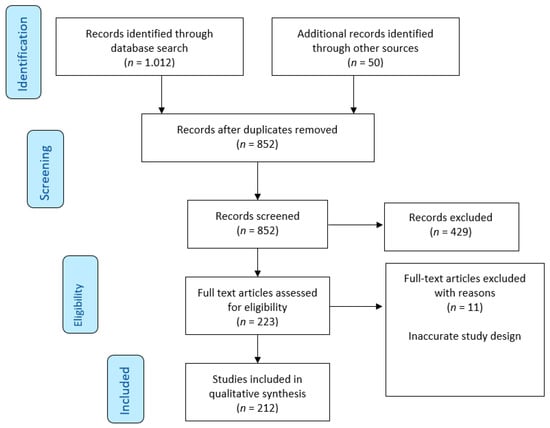
Figure 1.
The PRISMA flow diagram summarizes the flow of records through the study selection process for narrative review of telemedicine and eHealth in Poland (2014–2024).
3. Results
Of the 1012 records identified, 256 met all eligibility criteria. Of these, 212 studies were classified as either clinical (n = 96) or nonclinical (n = 116). The number of telemedicine and eHealth publications has grown steadily over the past decade, with significant increases observed during the COVID-19 pandemic (2020–2022). The analysis of temporal trends and themes (captured by thematic codes) examined the evolution of telemedicine and eHealth in Poland across three phases: (1) the Pre-Pandemic Foundations Phase (2014–2019), (2) the Pandemic Catalyst Phase (2020–2022), and (3) the Post-Pandemic Maturation Phase (2023–2024).
In the first phase (2014–2019), Polish law formally recognized and accepted telemedicine in December 2015, and e-prescriptions, e-referrals, and online patient accounts (IKP) were gradually implemented [23,24]. The initial clinical focus during this period was on psychiatry, cardiology, and dermatology. In the second phase (2020–2022), teleconsultations will be mandatorily implemented, accounting for up to 80% of primary care visits and 79% of specialist visits. In this phase, e-prescriptions became mandatory, with 67% of users accessing them independently. The scope of the national pilot programs for remote monitoring, including heart failure and geriatrics, has expanded. The third phase (2023–2024) witnessed the implementation of AI-based diagnostics in cardiology [48] and mental health as well as the emergence of cross-sector partnerships, including collaborations with the space industry and EU agencies. A strategic focus is placed on digital skills, interoperability, and sustainability.
3.1. Distribution by Medical Specialties
The most frequently studied medical specialties were psychiatry (n = 35), cardiology (n = 25), geriatrics (n = 22), general practice (n = 21), and rehabilitation (n = 18). The emerging fields were assumed to have the lowest number of studies that had not been scientifically explored in the previous period. These fields include oncology, neurology, dermatology, and diabetes. Psychiatry and geriatrics had the highest proportion of nonclinical research, whereas cardiology and rehabilitation were more heavily represented in clinical investigations.
3.2. Study Types
Surveys and questionnaire-based research (n = 78) dominated the dataset, particularly for the newly engaged specialties. Reviews accounted for 64 studies, which are often used to map the early to moderately advanced stages of adoption. Clinical trials and interventional studies (n = 37) were focused on cardiology, geriatrics, and rehabilitation. The standards for mental health and chronic diseases were based on cross-sectional and observational designs (n = 49).
3.3. Impact of COVID-19
Approximately 25% of the included studies were related to COVID-19, either in design or context. In certain specialties, including infectious diseases, pulmonology, and geriatrics, COVID-19 has catalyzed the implementation of telemedicine and the initiation of studies. Notably, in fields such as palliative care and rehabilitation, the only research output identified during that decade was related to COVID-19.
3.4. Clinical vs. Non-Clinical Studies by Specialty
Clinical studies were predominantly conducted in the cardiology (80%), rehabilitation (78%), and general practice (67%) settings. Nonclinical dominance was observed in the domains of psychiatry, geriatrics, and public health.
3.5. Research Aims and Maturity Assessment
Studies in telemedically advanced specialties such as cardiology and rehabilitation have emphasized outcome measurement, integration into care pathways, and the implementation of AI. In contrast, studies on less mature specialties have focused on feasibility, user perception, and platform usability. These differences reflect the varying stages of telemedicine and eHealth maturity across different specialties.
3.6. Trends over Time
Between 2014 and 2016, the publication volume was limited and predominantly nonclinical. From 2017 onward, thematic diversification increased, with growing contributions from geriatrics, psychiatry, and cardiology. The COVID-19 pandemic marked a sharp inflection point, after which implementation-focused research gained prominence. Post-pandemic years have witnessed a gradual return to strategic evaluation and interoperability studies. Figure 2 presents the trend analysis of telemedicine and eHealth publications in Poland from 2014 to 2024.
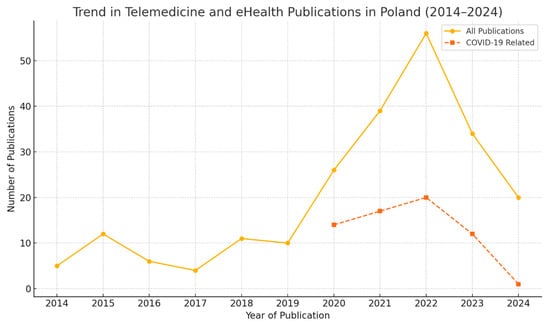
Figure 2.
Trend analysis of telemedicine and eHealth publications in Poland from 2014 to 2024.
There has been a steady increase in the number of publications since 2015, which is aligned with the formal legal implementation of telemedicine. COVID-19-related publications experienced a notable surge starting in 2020 and peaking in 2021 and 2022, reflecting the pandemic’s catalytic effect on research.
The comparison of two periods: 1995–2015 and 2014–2024 shows changes in the number of publications on telemedicine and eHealth by specialization (Figure 3).
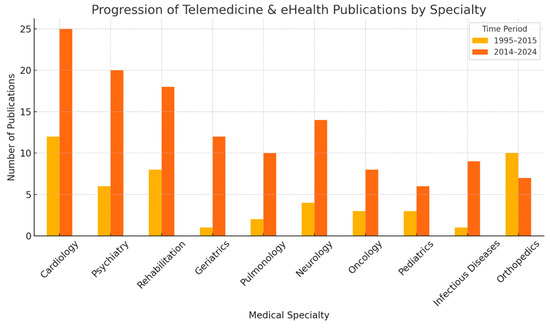
Figure 3.
Changes in the number of publications on telemedicine and eHealth by specialization, comparison of two periods: 1995–2015 and 2014–2024. Significant progress has been noted in cardiology, psychiatry, and rehabilitation, where the number of scientific publications has increased significantly. Geriatrics, pulmonology, and infectious diseases were almost absent before 2015; however, after 2015, they became very active, especially under the influence of the COVID-19 pandemic. Orthopedics, although very active, have seen relatively little growth in the last decade.
An analysis of progress in telemedicine and eHealth has shown that, between 2014 and 2024, these solutions have evolved from niche innovations to integral parts of national healthcare systems. The COVID-19 pandemic has significantly accelerated these changes, highlighting the shortcomings of traditional healthcare delivery methods, and accelerating the implementation of remote services. Such interdisciplinary bridges connect and integrate the expanding digital infrastructure in healthcare in Poland, ensuring the flow of data, funding, and innovation between sectors, while protecting patients’ needs, rights, coverage, and accountability.
3.7. Detailed Analysis of Developments in Selected Specialties
In accordance with the described methodology, the most prevalent disciplines were thoroughly analyzed and discussed, with field-specific comments included. The remaining specialties, which had three or fewer articles, were collectively analyzed and described, with references provided in Supplementary Table S1.
3.7.1. Telecardiology
Over the past decade, telecardiology in Poland has evolved significantly, transitioning from feasibility studies to clinical trials, particularly for the management of heart failure. During the early phase from 2014 to 2016, prospective studies established the safety of home-based cardiac telerehabilitation [49,50,51,52,53,54]. This initial focus on telemedicine laid the groundwork for structured programs [52]. Between 2019 and 2021, studies validated portable electrocardiogram (ECG) devices against standard 12-lead ECG [39,55]. The COVID-19 pandemic accelerated the adoption of telecardiology [56], while also highlighting its limitations [57]. An app was introduced to manage atrial fibrillation [43], and trials assessed the impact of hybrid telerehabilitation on heart failure patients [58,59,60,61,62,63]. Selected trials developed interventions aimed at reducing hospitalizations [64], whereas studies examined teleconsultations [39,65,66]. A cost-effectiveness analysis evaluated hybrid telerehabilitation [67]. Reviews have analyzed telemedicine in cardiology and the impact of digital technologies [68,69,70,71,72], and AI applications have also been reviewed [73]. Natural language processing (NLP) algorithms have been developed to extract data from EHRs [74], and remote heart monitoring via VPG from drones has been explored [75]. Patient perspectives on telemedicine have also been evaluated [76,77]. Trials have assessed post-myocardial interventions [78,79,80], and studies have supported the safety of telerehabilitation after acute myocardial infarction [81], demonstrating benefits for heart failure etiology [82]. Telemonitoring in cardiac resynchronization therapy has also been evaluated [83]. Overall, during the study period, Polish telecardiology advanced from telerehabilitation studies to comprehensive remote monitoring systems bolstered by clinical evidence and technological advancements.
3.7.2. Teledermatology
The evolution of teledermatology demonstrates the integration of virtual tools accelerated by COVID-19, encompassing diagnosis, management, and patient care. Initially, Reflectance confocal microscopy with cloud-based telemedicine was assessed for dermatological consultations [84]. During COVID-19 (2020–2022), the pandemic has accelerated the adoption of teledermatology through virtual conferences [85]. Research has explored COVID-19’s impact on atopic dermatitiss [86] and its efficacy in skin cancer screening [87]. Reviews have evaluated melanoma management through teledermatology [88], while the role of mobile teledermoscopy in skin cancer management has been analyzed [89]. Surveys have shown a growing acceptance of AI and telemedicine among dermatologists [90], and studies have reported positive patient experiences during COVID-19 restrictions [91]. The role of teledermatology in managing sexually transmitted infections was examined during the pandemic [92]. Early teledermatology used advanced diagnostics for remote consultation [87,92,93]. COVID-19 has expanded teledermatology into clinical care and education, particularly in skin cancer screening. Mobile teledermoscopy [89] and virtual conferences [85] have become essential remote tools. Healthcare professionals are increasingly accepting of AI and telemedicine. Teledermatology has proven to be effective for chronic conditions and patient access during social distancing. Its expansion to sexually transmitted infections has broadened in scope. The reviews have highlighted the benefits and limitations of these approaches.
3.7.3. eHealth Development
The evolution of eHealth in Poland encompasses user acceptance, digital literacy, telemedicine solutions, and inequities, reflecting the pandemic and demographic challenges. Studies have examined internet usage and eHealth literacy among elderly populations [94,95]. An 8-item eHealth literacy scale validation enabled reliable measurements [96]. Research has explored eHealth acceptance among patients with chronic diseases [97] and machine translation of telemedicine data [98]. Studies have assessed user satisfaction during COVID-19 [99,100], while surveys have examined demographic factors affecting older adults’ engagement [101]. Geographic disparities were analyzed using the Theil Index [102]. Research has examined telemedicine for individuals with intellectual disabilities [103] and eHealth service use factors in Central and Eastern Europe [104]. The Polish eHEALS validation supported literacy measurement [105]. A virtual patient collection blueprint enhances clinical reasoning [106]. Studies have analyzed pandemic-driven eHealth usage [107,108] and digital health definitions [109]. Advanced analytics has been evaluated in omics research [110]. Studies have established adoption hurdles and validated literacy assessment tools. COVID-19 has accelerated adoption, while research has addressed inequities and vulnerable groups through inclusive design.
3.7.4. Emergency Medicine Telemedicine Development
Research on telemedicine in Poland has focused on collaborative efforts, technology-enhanced training, telemonitoring, and pandemic reviews to enhance emergency care delivery. Early initiatives have improved cross-border cooperation in emergency medical services (EMS) through regional coordination [111]. Telemedicine interventions have been piloted to improve the quality of cardiopulmonary resuscitation (CPR) among healthcare providers. A randomized trial showed promising results in augmenting resuscitation skills [112], whereas a pilot study evaluated telemedicine tools in simulated cardiac arrest scenarios [113]. Research on prehospital electrocardiogram (ECG) teletransmission has improved transport logistics and hospital admissions [114]. The COVID-19 pandemic prompted a review of telemedicine in emergency medicine, covering prehospital, in-hospital, and remote consultations [115]. Emergency medicine telemedicine initially focused on harmonizing cross-border EMS systems. Telemedicine platforms enhance emergency skill training and clinical competencies. ECG teletransmission expedited patient triage and cardiac care. This pandemic has accelerated the adoption of telemedicine in emergency medicine. Polish emergency telemedicine research emphasizes clinical applications rather than large trials or technological development.
3.7.5. Telemedicine and Digital Health Development in Laryngology (ENT)
Telemedicine in ENT is gaining traction in Poland, focusing on remote screening, mobile applications, and adaptation to the pandemic. A telemedicine model for hearing screening in children developed in Poland was adopted in Tajikistan, demonstrating the feasibility of remote auditory testing [116]. The COVID-19 pandemic prompted clinical recommendations for otolaryngologists regarding high-risk procedures [117] and guidelines for managing patients while preventing infections [118]. Surveys assessed the impact of the pandemic on the Newborn Hearing Screening Program in Poland [119]. Research has evaluated a mobile application for tinnitus sound therapy, showing therapeutic potential through telehealth platforms [120]. A multicenter study investigated COVID-19’s impact on head and neck cancer progression, addressing emergency airway management and telemedicine in acute care [121]. Trends in ENT telemedicine indicate that remote pediatric screening is among the earliest applications. This pandemic has influenced ENT practices and requires infection control guidelines. Service disruptions affect newborn hearing screening, highlighting the need for remote solutions. Digital therapeutics through mobile apps shows promise for patient support. Telemedicine remains vital in acute and oncological ENT care, with data showing delayed cancer diagnosis due to the pandemic. The integration of telemedicine reflects technological adoption and pandemic adaptation, while maintaining the quality of care.
3.7.6. Telemedicine in Gerontology
Advancements in this field highlight Poland’s efforts to promote telehealth adoption among older adults and healthcare transformations during COVID-19. The study “Patient Perspectives and Telemedicine Accessibility” (2017) examined Polish patients’ views on telemedicine, uncovering insights into senior barriers [122]. “The Impact of the COVID-19 Pandemic on Older Adults” assessed healthcare service utilization among the elderly during the pandemic [40]. The 2022 study “Clinical Telerehabilitation in Specific Geriatric Conditions” showcased telerehabilitation for managing pelvic girdle pain in geriatric contexts [123]. “Pilot Telemedicine Projects for Frailty and Malnutrition” described an initiative for geriatric patients with frailty syndrome [124]. Research on Polish telemedicine in gerontology is in its early stages with a focus on patient acceptance. Although telerehabilitation addresses specific geriatric issues, further clinical studies are needed.
3.7.7. Telemedicine and Digital Health Development in Medical Practice
In this field, telemedicine and digital health have grown significantly owing to COVID-19, focusing on teleconsultations, digital skills, and legal frameworks. Early studies from 2017 to 2020 explored the potential of teleconsultation in Polish healthcare [125]. Legal analyses have reviewed telemedicine according to European standards [18]. National surveys have examined public interest in electronic health records (EHRs) [126]. Trials have evaluated remote monitoring of cardiac patients [127]. Studies have assessed the impact of teleconsultation on GP-patient communication [31,32] and healthcare professionals’ acceptance [29,128]. Research has examined physicians’ digital skills [129] and analyzed hospitals’ telemedicine monitoring [93,130]. Reviews evaluated patient satisfaction and digital health frameworks [131,132,133]. Studies have assessed legal barriers [22] and analyzed reimbursement models [134]. Research has examined GP telehealth adoption [29] and telemedicine uptake factors [135]. Projects have tested telemedicine for chronic diseases [136] and long-COVID [130]. Studies have compared rural telemedicine across Europe [137] and Generation Z’s teleconsultation satisfaction [138]. COVID-19 has accelerated telemedicine adoption, with studies showing positive attitudes and a need for digital literacy. Research has emphasized digital skills and regulatory clarity as enablers. Telemonitoring for chronic conditions has become part of routine care, and cross-border projects inform Polish telemedicine through European benchmarking.
3.7.8. mHealth Development and Research in Poland
In Poland, mHealth focuses on patient-centered mobile apps, wearables, informatics, and behavioral engagement. This study included clinical research, algorithm development, and mobile health technology surveys. Early and Clinical Usability Studies (2019–2021) explored Polish citizens’ attitudes toward mHealth and evaluated app usability for venous thromboembolic diseases [139,140]. Research has examined cardiovascular and pre-frailty risks using wearable data during the COVID-19 lockdown [141]. Attitudinal assessments (2020–2021) have investigated telemedical features for older adults, physicians’ views on rhythm-monitoring devices, and integration challenges [142,143]. Innovative Informatics (2022–2024) explored personalizing mHealth and developing algorithms for behavioral incentivization through rewards [144,145]. Studies have explored the impact of gamification and developed machine-learning models for estimating cognitive load using smartwatch data [146]. Early research established public attitudes and needs, whereas clinical studies validated apps and wearables for remote monitoring. Despite integration challenges, professional acceptance of wearables is increasing. Recent focus on personalization and engagement shows the field’s maturation through adaptive algorithms and gamification. The field remains exploratory, emphasizing development and feasibility, and further clinical validation is needed.
3.7.9. Telerehabilitation
In Poland, rehabilitation has seen significant growth in telerehabilitation technologies for neurological and musculoskeletal conditions accelerated by COVID-19. During Early Development (2016–2018), efforts focused on hand telerehabilitation systems for post-stroke patients using computer vision [147] and mobile applications for monitoring activities [148]. During the pandemic (2021–2023), telerehabilitation programs for Duchenne muscular dystrophy (DMD) proved feasible [149,150], with surveys exploring respiratory telerehabilitation for DMD patients [149,150]. Reviews of multiple sclerosis rehabilitation have highlighted the role of telemedicine while emphasizing clinical validation needs [151]. Studies have compared patient satisfaction between telerehabilitation and traditional therapies [152]. Recent Advances (2022–2024) include meta-analyses of cognitive telerehabilitation effectiveness [153] and evidence-based guidelines for Physical and Rehabilitation Medicine [154]. This field has progressed from feasibility studies to clinical evaluations, particularly in neurological rehabilitation. Research shows telerehabilitation’s effectiveness for stroke, DMD, MS, and cognitive impairment. The pandemic has accelerated its implementation when in-person care is limited. Studies indicate that telerehabilitation matches traditional methods in terms of patient acceptance. Despite these positive findings, additional large-scale trials are needed to refine the protocols and verify long-term outcomes.
3.7.10. Telemedicine and eHealth in Nursing
The research explores eHealth literacy among nursing students and has outlined the requirements for telemedical systems in home monitoring, particularly in rural areas with limited care access [155]. Surveys have examined nurses’ views on eHealth and patient empowerment through digital solutions, noting the value of eHealth despite implementation barriers [156]. Research has studied nursing students’ clinical education during COVID-19, advocating tele-education integration into curricula [157]. Cross-sectional studies have evaluated eHealth literacy among nursing students in Poland and Sweden, showing varying yet positive literacy trends in digital healthcare [158]. Nursing research has evolved from a system design to workforce needs and education. The COVID-19 pandemic has accelerated the use of remote learning in nursing education. eHealth literacy among students remains vital for telemedicine in patient care, highlighting the need to prepare nurses for digital healthcare.
3.7.11. Teleophthalmology
Teleophthalmology indicates a growing interest in remote eye care, particularly for diabetic retinopathy, with AI and telemedicine enhancing access to and diagnostics. Studies have evaluated diabetic retinopathy patients’ attitudes towards telemedicine, showing positive reception of remote management [159]. Surveys of visually impaired patients demonstrated acceptance of telemedicine, highlighting the need for disability-specific adaptations [160]. An algorithm for detecting hard exudates in retinal images demonstrated the feasibility of automated screening [161]. Reviews examining AI’s role of AI in diabetic retinopathy screening indicate its potential to improve accuracy and reduce specialist workload [162]. The analyses confirmed that home/remote optical coherence tomography (OCT) devices provide accurate retinal imaging outside clinics. Literature reviews have shown teleophthalmology’s potential to expand eye care access in underserved populations through remote monitoring [163]. In Poland, teleophthalmology combines AI algorithms with home-based OCT to enhance the diagnostics. While customization remains crucial, patients show positive attitudes towards telemedicine. AI and teleophthalmology improve screening while reducing the specialist burden. Although some studies were clinical, others were survey-based, indicating a need for validation in Poland.
3.7.12. Telemedicine and Digital Health Development in Locomotor System
The evolution of telemedicine in Orthopedics and trauma in Poland has driven the evaluation of pandemic-induced teleconsultation adoption and post-surgical care, particularly after total hip arthroplasty (THA) [164]. Research has focused on 3D telediagnostic screening for scoliosis and postural disorders [165]. A web survey examined “red flags” for serious low back pain among Internet users, highlighting the need for tele-triage [166]. During COVID-19 (2021–2023), studies have focused on orthopedic teleconsultations, documenting diagnoses, and effectiveness [167,168]. Surveys have explored surgeons’ methods for assessing fracture healing [169]. Literature reviews have proposed telemedicine-based postsurgical care models for THA recovery [170]. Systematic reviews have identified technologies for postsagittal THA care [171]. Early telemedicine focused on diagnostic screening and patient self-reporting. The pandemic has accelerated the adoption of teleconsultation, proving its effectiveness. Research has emphasized post-hospital telemedicine care, including rehabilitation monitoring, for THA patients. Future efforts should enhance organizational frameworks and patient outcomes through telemedicine.
3.7.13. Telemedicine in Pediatrics
The evolution of telemedicine in pediatrics has accelerated owing to COVID-19, focusing on the remote management of complex diseases, impact assessments, and cross-border collaborations. Clinical Case Reports and Treatment Advances (2024) have highlighted the treatment of infantile hemangioma with β-blockers via telemedicine, demonstrating the feasibility of managing complex conditions remotely [172]. The pandemic’s impact on pediatric healthcare and service adaptation (2020–2022) examined COVID-19’s effects on pediatric hospital activities, emphasizing disruptions and strategies for resuming services [173]. The focus was on pediatric epilepsy and asthma, assessing clinical changes and satisfaction with telemedicine [174,175]. Reviews have addressed pediatric hepatitis C management during pandemics [176]. Surveys have documented telemedicine use among pediatric providers, offering insights into acceptance and barriers [177]. Telemedicine Network Development (2023–2024) reported a cross-border network for pediatric hematology and oncology, emphasizing specialist access [178]. Studies have evaluated healthcare providers’ and patients’ perspectives on teleconsultations in Poland [179]. COVID-19 has accelerated the adoption of telemedicine in pediatric care, particularly in chronic conditions. Telemedicine has proven effective for managing complicated pediatric cases. Surveys have shown a growing acceptance among providers and patients while identifying challenges. Cross-border collaborations demonstrate the expanding scope of specialized care. The field has evolved from pandemic-driven adoption to sustainable models supported by evidence and feedback.
3.7.14. Telepsychiatry
Psychiatry has been instrumental in introducing telemedicine in Poland, with research encompassing telepsychiatric compliance studies, clinical trials, mental health interventions during COVID-19, mobile app support for addictions, and studies on cyberchondria related to health literacy. Foundational studies on Early Telepsychiatry Adoption and Compliance (2015–2019) concentrated on enhancing compliance in patients with paranoid schizophrenia through telemedicine systems [180]. A trial involving the MONEO platform with paranoid schizophrenia patients demonstrated the feasibility of remote monitoring [181]. Surveys have evaluated patient and psychiatrist attitudes towards telepsychiatry and identified levels of acceptance [182]. Commentaries have underscored the role of psychiatry in telemedicine, highlighting opportunities in mental healthcare [183]. The Expansion to Broader Mental Health Interventions and Tools (2017–2022) reviewed telemedicine interventions during COVID-19, summarizing the challenges of telepsychiatry delivery [184]. A pictogram-based tool was developed for individuals with communication impairments [185]. Mobile health applications have been evaluated to aid recovery from alcohol use disorders [186]. Reviews have identified strategies for occupational e-mental health interventions [187]. Studies have examined the mental health effects of COVID-19 on pregnant women [188]. Recent Cross-Sectional and Interventional Studies (2024) have explored cyberchondria and its connection with health literacy and eHealth literacy [189]. Sociodemographic factors have been linked to eHealth tool usage patterns among psychiatric populations [190]. A study comparing the Geriatric Depression Scale-30 assessments conducted face-to-face and telephone interviews [191]. Interviews analyzed user experiences with mobile apps for alcohol-use disorders [186]. Overall, psychiatry has become one of the leading specializations in Poland in terms of telemedicine integration, especially for serious mental illnesses. Clinical trials have demonstrated the efficacy of telepsychiatric platforms, alongside innovations in digital therapeutics. The scope of research has expanded owing to COVID-19, with studies focusing on digital behaviors and mental health. Tools have been developed to address communication impairments, and telepsychiatry has been extended to geriatric and occupational health.
3.7.15. Telemedicine in Pulmonology
In Poland, telemedicine research and practice in pulmonology have concentrated on chronic respiratory diseases, particularly chronic obstructive pulmonary disease (COPD) and sleep-related breathing disorders, such as obstructive sleep apnea (OSA). This field encompasses telehealth projects, telemonitoring for exacerbations, and evaluation of innovative technologies, including virtual reality (VR). A pilot study assessed daily telemonitoring to predict acute exacerbations (ECOPD) and demonstrated the feasibility of providing early warning signs to prevent hospitalization [192]. A recent pilot project (2022–2023) implemented telemedical solutions for managing COPD in senior populations in Wrocław and the Lower Silesian Voivodeship, offering insights into telehealth strategies for older adults with COPD [193]. A narrative review explored telehealth and VR applications in COPD management during COVID-19, highlighting VR’s role of VR in pulmonary rehabilitation alongside telemedicine approaches [194]. A questionnaire-based study assessed OSA management across Europe, revealing an increased adoption of telemedicine approaches including remote diagnostics and therapy monitoring [195]. COPD management remains central to pulmonology telemedicine research in Poland, with telemonitoring showing promise for early detection of exacerbations. The integration of telehealth with innovative technologies has enhanced pulmonary rehabilitation. Regional pilot projects provide evidence for scaling telemedical care models for older adults with respiratory disease. European studies on OSA management have demonstrated that the increasing adoption of telemedicine is applicable in Polish practice. The field combines practical pilots and reviews, indicating growth while highlighting opportunities for larger implementations.
3.7.16. Telemedicine in Urology
The advancement of telemedicine in urology, accelerated by COVID-19, has integrated remote solutions with a focus on clinical guidelines, practical impact, and future directions. Guidelines for online consultations in uro-oncology have been established to optimize remote care delivery while maintaining quality [196]. A review assessed the impact of the pandemic on urological practices and offered recommendations for adapting to new healthcare realities [197]. Research has identified key barriers to telemedicine implementation, such as technological limitations and reimbursement issues [198,199], while examining patient perceptions revealed positive attitudes towards convenience but concerns about care quality. A recent review evaluated the evolution of telemedicine in urology and proposed enhancing teleurology through AI, remote monitoring, and personalized care models [200]. The pandemic has catalyzed telemedicine adoption in urology, prompting guideline development and practice changes. Research highlights implementation challenges while showing positive patient attitudes towards teleurology accessibility. Recent analyses have suggested incorporating digital technologies to improve outcomes, although more empirical studies are needed to evaluate the impact of telemedicine on urological outcomes in Poland and beyond.
3.7.17. Telemedicine in Other Specialties
Telemedicine is being increasingly adopted across various medical specialties in Poland. However, fields such as artificial intelligence, allergology, bariatrics, dentistry, diabetes, hematology, laboratory medicine, maritime and tropical medicine, medical education, nephrology, neurosurgery, obesity, obstetrics/gynecology, oncology, pharmacy, prenatal care, preventive medicine, radiology, rheumatology, surgery, telemedicine/eHealth, and digital twins remain underrepresented in academic literature. Initial investigations, often in the form of surveys, reviews, or pilot studies, have indicated the development of telemedicine applications. The COVID-19 pandemic has heightened interest, prompting research on its impact on service delivery and patient perceptions, particularly in bariatrics, diabetes, obesity, and prenatal care. Patient satisfaction surveys are common in nephrology, hematology, and dentistry. Clinical studies are exploring technologies, such as artificial intelligence in voice technology, mobile nutrition applications, and virtual patients in medical education. Specialized services include telemedical assistance in maritime and tropical medicine for mass casualties. Some specialties such as orthopedics, urology, and rheumatology integrate telemedicine with traditional care. In summary, telemedicine in Poland is expanding, with cardiology, emergency medicine, and psychiatry exhibiting mature research, whereas other fields remain in the pilot phase. The pandemic has stimulated interest in telemedical solutions for the continuity of care, with satisfaction surveys indicating a need for acceptance. Technological studies suggest ongoing innovation, although implementation lags behind that of more established fields.
4. Discussion
4.1. Evolution of Digital Health in Poland
Based on the analyses conducted, we can conclude that, over the last decade, a mature digital health ecosystem (eHealth and telemedicine) has been established in Poland (Figure 4). Compared to the previous decade, it has undergone a significant transformation influenced by political reforms, technological innovations, the digitization of healthcare, and the growing involvement of stakeholders. This ecosystem comprises five main areas: (1) clinical care and telemedicine; (2) public health and health policy; (3) technological infrastructure; (4) patient and community engagement; and (5) research and innovation (Table 1).
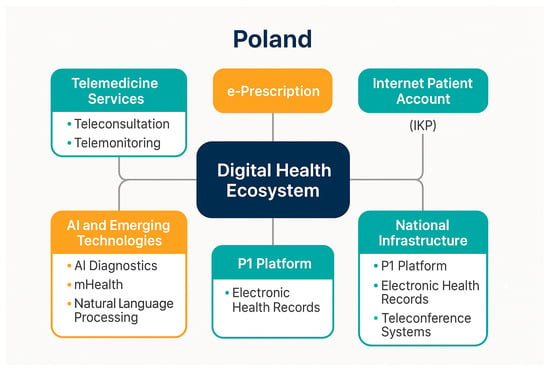
Figure 4.
eHealth Ecosystem Overview (Poland, 2014–2024).

Table 1.
Domains and key players in the eHealth ecosystem in Poland (2014–2024).
Table 1 presents descriptions of the domains and key players in the Polish eHealth ecosystem (2014–2024).
In Poland, telemedicine and eHealth transitioned from niche innovations to integral components of the national healthcare system between 2014 and 2024 [18,19]. The COVID-19 pandemic has significantly accelerated these transformations by highlighting the deficiencies in traditional healthcare delivery and expediting the adoption of remote services [35,100,107,131,137,201,202].
Poland is actively engaged in the development of telemedicine and eHealth. Since the early 21st century, substantial investments have been made and executed in line with the global dynamics of the telemedicine market, leading to the development and implementation of innovative telemedicine technologies. Notably, these investments were partially funded by the Polish public sector, specifically the MFZ and Mandatory Health Care Fund [18,19]. The potential benefits of telemedicine technologies are widely acknowledged and particularly evident in healthcare systems, society, and individual patients [203].
Telemedicine and eHealth represent robust and rapidly evolving medical sectors with the shared objective of enhancing healthcare and supporting the management and control of infectious and non-communicable diseases [7,8]. The global interest in these sectors is evident among governments and stakeholders. According to a recent report on eHealth status in the World Health Organization (WHO) European Region (from 2012), 41 of 53 countries had an eHealth strategy or policy in place by 2012 [104,204,205].
Numerous Polish projects and initiatives have explored various methodologies in telemedicine and eHealth and introduced classifications that incorporate diverse perspectives on commitment and environmental considerations [35,43,74,124,136,193,206,207,208]. Solutions in this field must encompass a wide range, including individual noninvasive telemonitoring, elements of space technology, comprehensive software for managing medical entities, and the development of virtual patients representing thousands of different diseases, thereby enhancing the educational process for students and medical personnel. Furthermore, systems facilitating real-time consultations, teleconferencing tools, advanced specialized equipment, robots, and other specialists are being developed. These systems utilize artificial intelligence in high-ranking simulation modes such as laboratories, telesurgery in high-precision operating modes, remote rehabilitation through computer games, and other intellectual and entertainment activities controlled by feedback from telemonitoring [19,22,108,209].
The evolution of telemedicine and eHealth in Poland is characterized by diverse projects and initiatives, highlighting key areas of commitment to systemic transformation through the enhancement of online and broadband health services. Notably, attention is directed towards further development and planned European Union financing for 2020–2026, alongside the requirements for comprehensive strategic investment plans utilizing funds from the National eHealth/Telemedicine Program [19,20,22].
Telemedicine and eHealth have emerged as transformative forces in global healthcare delivery for countries in Central and Eastern Europe, such as Poland [16,22,31]. The past decade has been marked by digital acceleration driven by evolving ICT technologies and urgent demands posed by the COVID-19 pandemic [22,35,203]. Before this period, digital health in Poland was in its infancy, characterized by sporadic implementation and limited legal support [28]. However, since 2015, strategic investments and regulatory reforms have spurred growth [22,35], positioning Poland as a regional innovator.
The scope and trajectory of telemedicine and eHealth development in Poland from 2014 to 2024 demonstrate the integration of national health platforms, telemonitoring systems, artificial intelligence-based tools, and mobile applications while assessing barriers and enabling factors in policy, practice, and public perception. The analyzed material contributes to understanding how a medium-sized European healthcare system can transition towards nationwide adoption and digital maturity.
Poland’s eHealth ecosystem encompasses formal and informal legal, strategic, and institutional mechanisms that facilitate cooperation and data exchange among key stakeholders, including government administration, healthcare providers, technology developers, patients, and research institutions. Based on the analyzed studies (2014–2024), several aspects of links with digital health strategies can be identified, including the national eHealth strategy and the P1 project, which involves a central platform enabling the provision of services such as e-prescriptions, e-referrals, and online patient accounts (IKP). Legislation on telemedicine enacted in 2015 provides a legal basis for remote consultation, digital documentation, and reimbursement. Regulations from the MH and NFZ define the scope of reimbursable telehealth services, including coding and eligibility criteria for service providers. An essential element is the regulation of data management and privacy, including standards compliant with the GDPR, which affects how personal and health data are collected, processed, and shared; a national interoperability framework aimed at standardizing data exchange between hospitals, clinics, and IT providers; consent protocols for data access via IKP and mobile apps; reimbursement and financing mechanisms; systems for the reimbursement of telehealth services by the NFZ, introduced or expanded during the COVID-19 pandemic; public–private financing programs, including support for AI tools, mHealth, and pilot implementations; and EU structural funds used for infrastructure and innovation.
Before COVID-19, telemedicine reimbursement by Poland’s NFZ was inconsistent. Though teleconsultations were legally recognized after the 2015 Act on Medical Activity amendment, the reimbursement framework remained limited, with services mostly restricted to pilot projects or regional initiatives [19,35]. The lack of standardized tariffs discouraged widespread adoption. COVID-19 has led to rapid institutionalization of telemedicine reimbursement. In March 2020, full reimbursement for teleconsultations in primary care and selected specialties was authorized with fees equivalent to those for in-person visits. E-prescriptions and e-referrals became mandatory, facilitating remote care workflows, while new codes were introduced for COVID-related telemedicine [35]. Regulatory changes granted telemedicine visits equal legal status. Post-COVID, while emergency measures were reduced, telemedicine reimbursement remained integral to routine care, particularly in primary care (POZ), specialist services, and chronic care management. However, a comprehensive long-term reimbursement policy has not yet been adopted, depending on local interpretations. Unlike Germany and France, Poland lacks quality-based payments for telemedicine metrics and reimbursements for AI-based diagnostics or mHealth tools. In the EU context, Poland followed similar trends, where Germany implemented Digitale-Versorgung-Gesetz (DVG) for digital app reimbursement [210,211], France maintained teleconsultation reimbursement post-COVID [212], and Nordic countries incorporated telehealth in chronic disease management [213,214].
Digital spaces also include cross-sector cooperation agreements, such as public–private partnerships (PPPs) between tech startups, academic centers, and hospitals; research grants carried out in collaboration between academia and industry, contributing to the promotion of innovation in artificial intelligence, wearable technology, and remote monitoring tools; space sector alliances covering, among other things, the use of telemetry in extreme conditions; and marine medicine. The professional standards and guidelines established by specialist medical and scientific associations that provide ethical and procedural frameworks must play a key role in implementing telemedicine services. Training and certification policies for healthcare professionals using telemedicine tools are crucial.
Over the last decade, Poland’s digital health evolution has demonstrated how a mid-income European country can harness legal reforms, policy momentum, and innovation to modernize its healthcare system [20]. Before 2014, telemedicine in Poland was primarily confined to conceptual or small-scale pilot projects, with minimal national coordination [28,215]. The period from 1995 to 2015 was characterized by specialties such as cardiology, pathology, orthopedics, and medical imaging, with research primarily focusing on technological feasibility rather than clinical outcomes.
In contrast, the 2014–2024 decade brought about a profound shift. The legalization of teleconsultations in 2015, implementation of mandatory e-prescriptions in 2020, and introduction of electronic referrals in 2018 established a functional policy framework. These regulatory milestones coincided with the development of the core infrastructure, including the P1 platform and IKP, which enabled the delivery of scalable digital services. The COVID-19 pandemic has further accelerated digital adoption, resulting in a significant increase in publication volumes, particularly between 2020 and 2022 [35]. Over the past decade, Poland has transitioned from fragmented and experimental telemedicine efforts to establishing coordinated, legally sanctioned, and partially interoperable eHealth ecosystems. Key drivers include top-down legal reforms, EU-supported infrastructure development, increased professional acceptance, and disruptive but catalytic influence of the COVID-19 pandemic.
Legislative decisions mandating e-prescriptions, e-referrals, and the rollout of the IKP were the most visible accelerators of systemic change. These milestones have enabled large-scale adoption by integrating digital tools into clinical workflows, reimbursement frameworks, and patient engagement strategies. While centralizing key services, the national digitization strategy laid the groundwork for expanded data sharing, user authentication, and remote service delivery, which became critical during the pandemic.
Notably, COVID-19 has accelerated the digitization of healthcare delivery and significantly reshaped the specialty landscape. Fields with minimal or no prior engagement in telemedicine, such as geriatrics, pulmonology, infectious diseases, and palliative care, saw rapid adoption of digital tools. In some cases, such as palliative medicine and respiratory care, COVID-related studies constituted the only publications on digital health, suggesting that the pandemic served as a trigger for digital innovation in those domains.
Simultaneously, mature specialties such as cardiology and rehabilitation have transitioned from feasibility studies to rigorous clinical trials and outcome-based evaluations. Notably, over 50% of cardiology-related articles involve patient-level data, with several evaluating the use of remote monitoring and telerehabilitation in chronic disease management. The digital footprints of mental health, psychiatry, and neurology have expanded their digital footprints through mHealth applications, AI-supported diagnostics, and video consultations, reflecting both clinical necessity and increased societal demand.
Conversely, traditional strongholds in digital health research from the pre-2015 period, such as pathology, orthopedics, and technical imaging, showed a relative regression in research activity. Despite advances in teleradiology infrastructure, the number of specialty-specific publications has decreased, possibly due to integration into broader health IT systems or shifting research funding priorities.
Artificial intelligence (AI) is an area of significant development. Although still emerging, AI applications in Poland’s healthcare system, particularly in cardiology, oncology, and geriatrics, include natural language processing (NLP) for electronic health records (EHRs), image recognition in radiology, and AI-assisted cognitive assessments [216]. However, its integration into the clinical workflow remains limited. Regulatory ambiguity, lack of reimbursement models, and insufficient clinician training/impeding their widespread implementation.
This regulatory lag is particularly evident compared to countries such as Germany, which has legislated digital therapeutics (DiGAs) [217], or Estonia [218], which operates under a fully digitalized, blockchain-secured health infrastructure [219,220]. Poland’s strength lies in its centralized platforms and capacity for rapid policy execution. However, its weakness is the slow translation of innovation into everyday clinical practice and limited long-term evaluation of digital interventions.
Furthermore, the distribution of study types underscores the advanced maturity of digital health research. Survey-based studies were predominant in emerging specialties and during the initial phases of the pandemic, whereas trials and longitudinal studies were more common in established fields, such as cardiology, psychiatry, and rehabilitation. This trend reflects both the readiness of infrastructure and the presence of established academic-industry collaborations, which have been instrumental in broadening the scope of research. Poland’s alignment with the European Health Data Space (EHDS) presents a critical opportunity to address the remaining challenges in interoperability, ethical governance, and cross-border data sharing [221,222]. Achieving success in this subsequent phase will necessitate technological advancements, enhanced regulatory clarity, inclusion of AI in strategic planning, and proactive engagement with patients and professionals to ensure trust and adoption. The period from 2014 to 2024 marked an accelerated transition from experimentation to institutionalization within the Polish digital health sector. The capacity to scale digital infrastructure and mobilize various sectors during a crisis has become evident from a national perspective. However, sustaining this trajectory in the coming decade will require greater emphasis on the interoperability, regulation of new technologies, strategic financing, and synergies between academia and industry. Identifying and supporting specializations that remain underrepresented, but could significantly benefit from tailored digital interventions, is crucial. Drawing on insights from previous research, a thirty-year outlook for the development of telemedicine and eHealth in Poland was delineated. The results of this study reflect both the historical progress and significant shifts in priorities, opportunities, and system integration over the past decade. Recent years have witnessed significant thematic diversification, demonstrating the expansion of the scope and increased maturity of telemedicine and eHealth in Poland. Psychiatry, pulmonology, rehabilitation, and neurology have emerged as key areas of development, reflecting the adaptation of Polish medicine to promote solutions to address the burden of chronic diseases and undertaking strategic public health initiatives. The importance of previously developed areas, such as orthopedics and pathology, has declined, not due to a loss of significance, but rather due to a shift from opportunistic applications to strategically driven development. Instead, their representation has decreased because of their heightened interest in other specialties.
There has been a notable increase in clinical research encompassing projects, trials, and implementations, with over 60% of studies incorporating patient data and structured clinical protocols. This trend underscores the advancement and specialization of clinical research. The number and sophistication of research projects is particularly evident in the fields of cardiology, geriatrics, and mental health. The application of artificial intelligence and telemonitoring tools in cardiology, along with video consultations in psychiatry and dermatology, highlights the progression from general tools to solutions tailored to specific specialties. The COVID-19 pandemic has served a pivotal moment by acting as a systemic catalyst. The volume of publications on telemedicine and eHealth surged between 2020 and 2022, aligning with the national guidelines on teleconsultation and e-prescriptions. The swift deployment of digital infrastructure bolstered by EU funds and changes in national policy has facilitated the integration of telemedicine into routine healthcare. However, this transformation has exposed structural deficiencies such as disparities in access to digital technologies, varying levels of health literacy, and inconsistent implementation of technologies across regions and professional groups. Compared to the pre-2014 scenario, characterized by localized pilot projects and minimal institutional coordination, the Polish digital health system has undergone substantial transformation, allowing for an assessment of regional maturity. The establishment of national platforms (e.g., e-prescriptions, e-referrals, IKP), innovative projects executed under public–private partnerships, and a formalized legal framework have enabled Poland to attain a medium level of eHealth maturity in Europe. Estonia remains a regional leader because of its fully integrated electronic medical records and blockchain-secured systems [220,223]. Germany has pioneered regulations for artificial intelligence and digital therapies [224,225], and Poland has surpassed countries such as Hungary, Romania, and Bulgaria in terms of telemedicine infrastructure and utilization.
Poland’s eHealth integration and governance ecosystem encompasses interdisciplinary and interconnected domains, public administration, healthcare providers, patients, technology developers, and research institutions linked by digital platforms and policy bridges. These bridges include a national eHealth strategy, GDPR-based regulatory updates, and a P1 health information infrastructure. Key areas of convergence include reimbursement reforms, digital skill initiatives, and cross-sector research collaborations. A visual model of the ecosystem reflects the interdependencies and direction of influence between these actors.
The path towards sustainable innovation requires the institutionalization of telemedicine in reimbursement systems, prioritizing digital integration, and introducing mandatory interoperability between platforms. Developing training programs for healthcare professionals, particularly those aimed at bridging the digital skill gap among older doctors, is essential. Training in this area must be included in the curriculum of medical universities in the clinical sciences section, as students are familiar with clinical examination methods and have a basic understanding of disease diagnosis and treatment. Ethical oversight mechanisms should be strengthened to address concerns about AI implementation of artificial intelligence, clinical data safety, and data management.
Poland’s participation in EU initiatives such as the European Health Data Space (EHDS) should be used to increase interoperability and support joint innovation. Furthermore, integrating space technologies, wearable devices, and NLP tools into national projects demonstrates Poland’s potential to become a regional leader in applied digital health innovations.
Despite this progress, the integration of telemedicine remains uneven across different specialties and geographical regions. Disparities in access to digital technologies persist between urban and rural areas, and many digital tools remain in the pilot phase or are used only to a limited extent. Therefore, overcoming the remaining barriers and research gaps is necessary to ensure sustainable scaling, implementation of a scientific framework, and long-term research of the results.
Specializations, such as orthopedics and pathology, despite their historical contribution to early pilot telemedicine studies in Poland, did not show significant progress in the use of digital technologies in Polish healthcare between 2014 and 2024. This stagnation may be due to infrastructure limitations, limited reimbursement frameworks, and lower perception of the feasibility of remote diagnostics in these specialties. In the current period of the global expansion of AI-assisted image analysis and tele-imaging platforms, targeted national initiatives could accelerate their integration into routine orthopedic examinations and pathological processes. AI-based radiological interpretation tools could enhance musculoskeletal diagnostics and digital pathology systems could facilitate centralized expert consultations, which would be particularly beneficial for regions with limited access to services in these specialized fields. While cardiology, psychiatry, and neurology have maintained high levels of telemedicine use, their future maturity will depend on the structured integration of artificial intelligence, particularly in a changing regulatory environment shaped by the EU’s Artificial Intelligence Act and the future European Health Data Space (EHDS) [226]. Ensuring the ethical implementation of artificial intelligence requires transparent validation of algorithms, physician training, and integration with existing clinical pathways while minimizing the widening of the digital divide. The limited use of artificial intelligence observed in the dataset highlights the current stage of digital transformation in healthcare in Poland. While national eHealth strategies focus on teleconsultations and electronic prescriptions, the integration of advanced digital therapies, real-time clinical decision support, and AI-based diagnostic systems remains in its infancy. Cross-sector collaboration involving academic institutions, technology start-ups, and health policymakers could fill this gap by supporting innovation sandboxes and pilot programs aligned with EU digital health priorities. Finally, as specializations such as rehabilitation, geriatrics, and pulmonology have gained popularity in telehealth applications, a systematic framework is needed to assess their clinical effectiveness, cost-effectiveness, and patient satisfaction.
As emphasized in recent frameworks [227], evaluating telemedicine effectiveness should address patient safety, diagnostic precision, equity, and patient-reported outcomes. Incorporating such multidimensional evaluation frameworks into national monitoring strategies may enhance accountability and service quality
The assessments obtained should ensure that telemedicine not only increases access, but also improves health outcomes, which is a key objective for Poland’s pursuit of digital maturity in health, comparable to leaders such as Estonia and Germany.
4.2. Limitations
This review had several limitations that warrant consideration. The search was confined to English language publications, excluding significant research published in Polish, particularly in national journals, conference proceedings, and institutional reports. Given that local pilot projects and regional innovations have played a role in the implementation of telemedicine and eHealth in Poland, this language restriction may have overlooked critical contributions. Only peer-reviewed and structured literature indexed in major international databases (PubMed, Scopus, EMBASE, and Web of Science) were included. This approach may underestimate the extent of telemedicine and eHealth development in Poland, especially considering the dynamic contributions of gray literature, unindexed national initiatives, and real-world implementation reports that have not been formally published. It is also important to acknowledge that authors often submit articles to high-impact journals when they believe their work has achieved a significant level of scientific maturity, prompting them to undergo a peer-review process. Although efforts were made to ensure accuracy, some records contained limited metadata or ambiguous methodological descriptors, which may have introduced minor classification errors, particularly in distinguishing between clinical and nonclinical studies or assigning studies to specific medical fields when interdisciplinary overlaps occur. This review encompassed various study designs, populations, and digital tools. Although a narrative synthesis approach accounts for this variability, it limits the ability to conduct meta-analyses or to generate summary effect estimates for outcomes, effectiveness, and adoption rates. Studies were classified as “COVID-19-related” based on the presence of keywords and a review of the full article. This may have led to an underestimation of indirect pandemic-related effects, such as changes in healthcare delivery models or accelerated digitization due to crisis-induced changes in healthcare system behavior. Although this study attempted to assess the maturity of telemedicine adoption across specialties, based on trends in research objectives, types of technologies, and integration, a more formalized maturity framework is required to verify these impressions and enable comparisons with international standards for digital healthcare. Future research should focus on methodologies and real-world outcome measures to complement and deepen our understanding of the digital health transformation in Poland.
Another limitation of this study was the potential bias in the misclassification of medical specialties assigned to individual publications. Given that many telemedicine and eHealth interventions are multidisciplinary and often overlap (e.g., rehabilitation studies in neurology or geriatrics and cardiology studies involving respiratory assessment), assigning them to a single specialty may oversimplify their scope. While necessary for quantitative trend analysis, this classification approach may not reflect the actual extent of telemedicine integration in related medical fields.
The lessons learned from the study of peer-reviewed articles on telemedicine and eHealth in Poland, published between 2014 and 2024, highlight the most significant achievements in the field of telemedicine and eHealth in Poland during that period. Telemedicine has been successfully used to treat patients with many chronic diseases including Duchenne muscular dystrophy, intellectual disability, and chronic heart failure. The technology implemented ensured continuity of care for elderly patients during the COVID-19 pandemic despite limited social contact and access to in-person services for improving psychosocial and mental health. Numerous studies have reported enhanced psychosocial outcomes in patients using telepsychiatry, mobile apps, and digital monitoring tools. Virtual reality (VR) and telemedicine have emerged as promising methods for rehabilitation and treatment of neurodevelopmental disorders. Visual tools and wearable devices have been shown to improve post-hospital care, particularly in orthopedic and cardiac rehabilitation, and offer potential for technology-enabled care coordination. The effective use of telemedicine depends on the appropriateness of the technology and the quality of the digital communication infrastructure. Health literacy, user experience, demographic data, and trust in digital technologies significantly impacted patient satisfaction and continued use of telemedicine. Particular attention should be paid to the increasing popularity of telemedicine among older adults and digitally excluded individuals. Some studies have focused on computational tools for analyzing large health datasets, highlighting the growing role of data science in eHealth, which has contributed significantly to scientific and technical advancements in Polish medicine. Although less common, methodological advances have highlighted the interdisciplinary nature of digital health research.
5. Conclusions
An analysis of peer-reviewed material allowed us to present the course of digital transformation and the development of telemedicine and eHealth in Poland, where healthcare has evolved from isolated telemedicine initiatives to a national eHealth ecosystem driven by regulatory, technological, and public health changes. This evolution has been facilitated by legislative reforms, infrastructure investments, and the pandemic, all of which have increased teleconsultations, e-prescriptions, and digital tools in clinical practice. Research on digitization, telemedicine, and eHealth has matured in cardiology, psychiatry, geriatrics, and rehabilitation, with new applications emerging in pulmonology and pediatrics. However, fields that were active ten years ago, such as orthopedics and pathology, have not seen similar development and remain underrepresented in publications. Investments in artificial intelligence (AI), digital infrastructure, and political support are essential for the integration of digital health in all areas of medicine. Studies have demonstrated increased acceptance among patients and providers while highlighting challenges such as regulatory uncertainty, limited reimbursement frameworks, and interoperability gaps, particularly for AI technologies. Despite progress, development depends on regulatory harmonization, sustainable financing, professional training, and collaboration among the government, academia, industry, and patient communities. By aligning with European initiatives such as the European Health Data Space, Poland can become a leader in regional digital healthcare integration, providing reforms that support interoperability, data security, and equitable access.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app15168793/s1, Table S1: The supplementary table summarizes the final selection of papers for analysis in the narrative review.
Author Contributions
Conceptualization, W.M.G.; Methodology, W.M.G., T.C., A.W., R.D., K.W., and S.W.; Validation, W.M.G., T.C., A.W., R.D., K.W., and S.W.; Formal analysis, W.M.G., T.C., A.W., R.D., K.W., and S.W.; Investigation, W.M.G., T.C., A.W., R.D., K.W., and S.W.; Resources, W.M.G., and K.W.; Data curation, W.M.G., T.C., and A.W.; Writing—original draft preparation, W.M.G., T.C., A.W., and S.W.; Writing—review and editing, W.M.G., and A.W.; Visualization, W.M.G., T.C., A.W., R.D., K.W., and S.W.; Supervision, W.M.G., and S.W.; Project administration, W.M.G., T.C., A.W., R.D., K.W., and S.W.; APC funding acquisition, K.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Yeung, A.W.K.; Torkamani, A.; Butte, A.J.; Glicksberg, B.S.; Schuller, B.; Rodriguez, B.; Ting, D.S.W.; Bates, D.; Schaden, E.; Peng, H.; et al. The promise of digital healthcare technologies. Front. Public Health 2023, 11, 1196596. [Google Scholar] [CrossRef]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef]
- Fonda, F.; Galazzi, A.; Chiappinotto, S.; Justi, L.; Frydensberg, M.S.; Boesen, R.L.; Macur, M.; Reig, E.A.; Espaulella, E.R.; Palese, A. Healthcare System Digital Transformation across Four European Countries: A Multiple-Case Study. Healthcare 2023, 12, 16. [Google Scholar] [CrossRef]
- Galazzi, A.; Fonda, F.; Chiappinotto, S.; Justi, L.; Sønderskov Frydensberg, M.; Lehmann Boesen, R.; Macur, M.; de San Pedro, M.; Reixach Espaulella, E.; Palese, A. Recommendations to promote the digital healthcare transformation in the clinical practice: Findings from an international consensus development method. BMC Health Serv. Res. 2025, 25, 929. [Google Scholar] [CrossRef]
- Sood, S.; Mbarika, V.; Jugoo, S.; Dookhy, R.; Doarn, C.R.; Prakash, N.; Merrell, R.C. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed. J. eHealth 2007, 13, 573–590. [Google Scholar] [CrossRef]
- Gao, J.; Fan, C.; Chen, B.; Fan, Z.; Li, L.; Wang, L.; Ma, Q.; He, X.; Zhai, Y.; Zhao, J. Telemedicine Is Becoming an Increasingly Popular Way to Resolve the Unequal Distribution of Healthcare Resources: Evidence from China. Front. Public Health 2022, 10, 916303. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Williams, K.; Bohls, J.; Shamsi, W. Telemedicine and health policy: A systematic review. Health Policy Technol. 2021, 10, 209–229. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Anawade, P.A.; Sharma, D.; Gahane, S. A Comprehensive Review on Exploring the Impact of Telemedicine on Healthcare Accessibility. Cureus 2024, 16, e55996. [Google Scholar] [CrossRef]
- Alenoghena, C.O.; Ohize, H.O.; Adejo, A.O.; Onumanyi, A.J.; Ohihoin, E.E.; Balarabe, A.I.; Okoh, S.A.; Kolo, E.; Alenoghena, B. Telemedicine: A Survey of Telecommunication Technologies, Developments, and Challenges. J. Sens. Actuator Netw. 2023, 12, 20. [Google Scholar] [CrossRef]
- Stoltzfus, M.; Kaur, A.; Chawla, A.; Gupta, V.; Anamika, F.N.U.; Jain, R. The role of telemedicine in healthcare: An overview and update. Egypt. J. Intern. Med. 2023, 35, 49. [Google Scholar] [CrossRef]
- Culmer, N.; Smith, T.B.; Stager, C.; Wright, A.; Fickel, A.; Tan, J.; Clark, C.T.; Meyer, H.; Grimm, K. Asynchronous Telemedicine: A Systematic Literature Review. Telemed. Rep. 2023, 4, 366–386. [Google Scholar] [CrossRef]
- Glinkowski, W. Advances in International Telemedicine and Ehealth. Around the World, 1st ed.; Medipage Ltd.: Warszawa, Poland, 2006; Volume 1, p. 171. [Google Scholar]
- Oh, H.; Rizo, C.; Enkin, M.; Jadad, A. What is eHealth (3): A systematic review of published definitions. J. Med. Internet Res. 2005, 7, e1. [Google Scholar] [CrossRef] [PubMed]
- da Fonseca, M.H.; Kovaleski, F.; Picinin, C.T.; Pedroso, B.; Rubbo, P. EHealth Practices and Technologies: A Systematic Review from 2014 to 2019. Healthcare 2021, 9, 1192. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2023: OECD Indicators; OECD Publishing: Paris, France, 2023. [Google Scholar]
- Directorate-General for Health and Food Safety (European Commission). Opinion on Assessing the Impact of Digital Transformation of Health Services; Publications Office of the European Union: Luxembourg, 2019. [Google Scholar]
- Flaga-Gieruszyńska, K.; Kożybska, M.; Osman, T.; Radlińska, I.; Zabielska, P.; Karakiewicz-Krawczyk, K.; Jurczak, A.; Karakiewicz, B. Telemedicine services in the work of a doctor, dentist, nurse and midwife—Analysis of legal regulations in Poland and the possibility of their implementation on the example of selected European countries. Ann. Agric. Environ. Med. 2020, 27, 680–688. [Google Scholar] [CrossRef]
- Pochrzęst-Motyczyńska, A.; Pinkas, J.; Religioni, U.; Ostrowski, J. Development of telemedicine in Poland—Organizational, ethical and communication challenges. Ann. Agric. Environ. Med. 2025, 32, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Latif, F. Implementation and Progress of Telemedicine in Poland: Comparative Analysis with EU Member States. Annales Univ. Mariae Curie-Skłodowska Sect. H Oeconomia 2025, 59, 18. [Google Scholar] [CrossRef]
- Livieri, G.; Mangina, E.; Protopapadakis, E.D.; Panayiotou, A.G. The gaps and challenges in digital health technology use as perceived by patients: A scoping review and narrative meta-synthesis. Front. Digit. Health 2025, 7, 1474956. [Google Scholar] [CrossRef]
- Furlepa, K.; Tenderenda, A.; Kozłowski, R.; Marczak, M.; Wierzba, W.; Śliwczyński, A. Recommendations for the Development of Telemedicine in Poland Based on the Analysis of Barriers and Selected Telemedicine Solutions. Int. J. Environ. Res. Public Health 2022, 19, 1221. [Google Scholar] [CrossRef] [PubMed]
- NEJM Catalyst. What Is Telehealth? Catal. Carryover 2018, 4. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0268 (accessed on 4 August 2025).
- Thomsen, T.; Esbensen, B.A.; Hetland, M.L.; Aadahl, M. Motivational Counseling and Text Message Reminders: For Reduction of Daily Sitting Time and Promotion of Everyday Physical Activity in People with Rheumatoid Arthritis. Rheum. Dis. Clin. N. Am. 2019, 45, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Białczyk, A.; Leśniak, G.; Nadolny, F.; Mrowiec, J.; Otałęga, A. Exploring digital health horizons: A narrative review of eHealth innovations in Poland, Spain, Romania and Estonia. Prospect. Pharm. Sci. 2024, 22, 32–37. [Google Scholar] [CrossRef]
- Bente, B.E.; Van Dongen, A.; Verdaasdonk, R.; van Gemert-Pijnen, L. eHealth implementation in Europe: A scoping review on legal, ethical, financial, and technological aspects. Front. Digit. Health 2024, 6, 1332707. [Google Scholar] [CrossRef]
- Raposo, V.L. Telemedicine: The legal framework (or the lack of it) in Europe. GMS Health Technol. Assess. 2016, 12, Doc03. [Google Scholar]
- Glinkowski, W.M.; Karlińska, M.; Karliński, M.; Krupiński, E.A. Telemedicine and eHealth in Poland from 1995 to 2015. Adv. Clin. Exp. Med. 2018, 27, 277–282. [Google Scholar] [CrossRef]
- Walczak, R.; Kludacz-Alessandri, M.; Hawrysz, L. Use of Telemedicine Technology among General Practitioners during COVID-19: A Modified Technology Acceptance Model Study in Poland. Int. J. Environ. Res. Public Health 2022, 19, 10937. [Google Scholar] [CrossRef] [PubMed]
- Kruszyńska-Fischbach, A.; Sysko-Romańczuk, S.; Rafalik, M.; Walczak, R.; Kludacz-Alessandri, M. Organizational E-Readiness for the Digital Transformation of Primary Healthcare Providers during the COVID-19 Pandemic in Poland. J. Clin. Med. 2021, 11, 133. [Google Scholar] [CrossRef] [PubMed]
- Kludacz-Alessandri, M.; Hawrysz, L.; Korneta, P.; Gierszewska, G.; Pomaranik, W.; Walczak, R. The impact of medical teleconsultations on general practitioner-patient communication during COVID-19: A case study from Poland. PLoS ONE 2021, 16, e0254960. [Google Scholar] [CrossRef]
- Kludacz-Alessandri, M.; Walczak, R.; Hawrysz, L.; Korneta, P. The Quality of Medical Care in the Conditions of the COVID-19 Pandemic, with Particular Emphasis on the Access to Primary Healthcare and the Effectiveness of Treatment in Poland. J. Clin. Med. 2021, 10, 3502. [Google Scholar] [CrossRef]
- Frost, D.; Mahmud, M.; Kaiser, M.S.; Musoke, D.; Henry, P.; Islam, S. Innovative approaches to strengthening health systems in low- and middle-income countries: Current models, developments, and challenges. Health Policy Technol. 2021, 10, 100567. [Google Scholar] [CrossRef]
- Golinelli, D.; Boetto, E.; Carullo, G.; Nuzzolese, A.G.; Landini, M.P.; Fantini, M.P. Adoption of Digital Technologies in Health Care During the COVID-19 Pandemic: Systematic Review of Early Scientific Literature. J. Med. Internet Res. 2020, 22, e22280. [Google Scholar] [CrossRef] [PubMed]
- Furlepa, K.; Śliwczyński, A.; Kamecka, K.; Kozłowski, R.; Gołębiak, I.; Cichońska-Rzeźnicka, D.; Marczak, M.; Glinkowski, W.M. The COVID-19 Pandemic as an Impulse for the Development of Telemedicine in Primary Care in Poland. J. Pers. Med. 2022, 12, 1165. [Google Scholar] [CrossRef]
- Omboni, S.; Padwal, R.S.; Alessa, T.; Benczúr, B.; Green, B.B.; Hubbard, I.; Kario, K.; Khan, N.A.; Konradi, A.; Logan, A.G.; et al. The worldwide impact of telemedicine during COVID-19: Current evidence and recommendations for the future. Connect. Health 2022, 1, 7–35. [Google Scholar] [CrossRef] [PubMed]
- Shaver, J. The State of Telehealth Before and After the COVID-19 Pandemic. Prim. Care 2022, 49, 517–530. [Google Scholar] [CrossRef]
- Kalin, M.L.; Garlow, S.J.; Thertus, K.; Peterson, M.J. Rapid Implementation of Telehealth in Hospital Psychiatry in Response to COVID-19. Am. J. Psychiatry 2020, 177, 636–637. [Google Scholar] [CrossRef]
- Kołtowski, Ł.; Krzowski, B.; Boszko, M.; Paskudzka, D.; Peller, M.; Lodziński, P.; Balsam, P.; Grabowski, M.; Kochman, J.; Opolski, G. Cardiological teleconsultation in the coronavirus disease 2019 era: Patient’s and physician’s perspective. Kardiol. Pol. 2021, 79, 76–78. [Google Scholar] [CrossRef]
- Agrawal, S.; Makuch, S.; Dróżdż, M.; Strzelec, B.; Sobieszczańska, M.; Mazur, G. The Impact of the COVID-19 Emergency on Life Activities and Delivery of Healthcare Services in the Elderly Population. J. Clin. Med. 2021, 10, 4089. [Google Scholar] [CrossRef]
- Seron, P.; Oliveros, M.J.; Gutierrez-Arias, R.; Fuentes-Aspe, R.; Torres-Castro, R.C.; Merino-Osorio, C.; Nahuelhual, P.; Inostroza, J.; Jalil, Y.; Solano, R.; et al. Effectiveness of Telerehabilitation in Physical Therapy: A Rapid Overview. Phys. Ther. 2021, 101, pzab053. [Google Scholar] [CrossRef] [PubMed]
- Lan, X.; Yu, H.; Cui, L. Application of Telemedicine in COVID-19: A Bibliometric Analysis. Front. Public Health 2022, 10, 908756. [Google Scholar] [CrossRef]
- Gawałko, M.; Duncker, D.; Manninger, M.; van der Velden, R.M.J.; Hermans, A.N.L.; Verhaert, D.V.M.; Pison, L.; Pisters, R.; Hemels, M.; Sultan, A.; et al. The European TeleCheck-AF project on remote app-based management of atrial fibrillation during the COVID-19 pandemic: Centre and patient experiences. Europace 2021, 23, 1003–1015. [Google Scholar] [CrossRef]
- Krzowski, B.; Peller, M.; Boszko, M.; Hoffman, P.; Żurawska, N.; Jaruga, K.; Skoczylas, K.; Osak, G.; Kołtowski, Ł.; Grabowski, M.; et al. Mobile app and digital system for patients after myocardial infarction (afterAMI): Study protocol for a randomized controlled trial. Trials 2022, 23, 522. [Google Scholar] [CrossRef]
- Davalbhakta, S.; Advani, S.; Kumar, S.; Agarwal, V.; Bhoyar, S.; Fedirko, E.; Misra, D.P.; Goel, A.; Gupta, L.; Agarwal, V. A Systematic Review of Smartphone Applications Available for Corona Virus Disease 2019 (COVID19) and the Assessment of their Quality Using the Mobile Application Rating Scale (MARS). J. Med. Syst. 2020, 44, 164. [Google Scholar] [CrossRef]
- Więckowska-Rusek, K.; Danel, J.; Deja, G. The usefulness of the nutrition apps in self-control of diabetes mellitus—The review of literature and own experience. Pediatr. Endocrinol. Diabetes Metab. 2022, 28, 75–80. [Google Scholar] [CrossRef]
- Chaturvedi, U.; Chauhan, S.B.; Singh, I. The impact of artificial intelligence on remote healthcare: Enhancing patient engagement, connectivity, and overcoming challenges. Intell. Pharm. 2025, in press. [Google Scholar] [CrossRef]
- Leclercq, C.; Witt, H.; Hindricks, G.; Katra, R.P.; Albert, D.; Belliger, A.; Cowie, M.R.; Deneke, T.; Friedman, P.; Haschemi, M.; et al. Wearables, telemedicine, and artificial intelligence in arrhythmias and heart failure: Proceedings of the European Society of Cardiology Cardiovascular Round Table. Europace 2022, 24, 1372–1383. [Google Scholar] [CrossRef]
- Piotrowicz, E.; Korzeniowska-Kubacka, I.; Chrapowicka, A.; Wolszakiewicz, J.; Dobraszkiewicz-Wasilewska, B.; Batogowski, M.; Piotrowski, W.; Piotrowicz, R. Feasibility of home-based cardiac telerehabilitation: Results of TeleInterMed study. Cardiol. J. 2014, 21, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Piotrowicz, E.; Orzechowski, P.; Chrapowicka, A.; Piotrowicz, R. How Should We Advise Heart Failure Patients on Exercise and What Should We Tell Them? Curr. Heart Fail Rep. 2014, 11, 274–280. [Google Scholar] [CrossRef]
- Piotrowicz, E.; Stepnowska, M.; Leszczynska-Iwanicka, K.; Piotrowska, D.; Kowalska, M.; Tylka, J.; Piotrowski, W.; Piotrowicz, R. Quality of life in heart failure patients undergoing home-based telerehabilitation versus outpatient rehabilitation—A randomized controlled study. Eur. J. Cardiovasc. Nurs. 2015, 14, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Piotrowicz, E.; Pencina, M.; Piotrowski, W.; Banach, M.; Piotrowicz, R. Influence of exercise training on T-wave alternans assessed during exercise test in heart failure patients. Int. J. Cardiol. 2014, 174, 747–749. [Google Scholar] [CrossRef] [PubMed]
- Piotrowicz, R.; Grabowski, M.; Balsam, P.; Kołtowski, Ł.; Kozierkiewicz, A.; Zajdel, J.; Piotrowicz, E.; Kowalski, O.; Mitkowski, P.; Kaźmierczak, J.; et al. [“Baltic Declaration”—Telemedicine and mHealth as support for clinical processes in cardiology. The opinion of the Committee of Informatics and Telemedicine of the Polish Society of Cardiology and Telemedicine Clinical Sciences Committee of the PAS]. Kardiol. Pol. 2015, 73, 575–584. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Piotrowicz, E.; Zieliński, T.; Bodalski, R.; Rywik, T.; Dobraszkiewicz-Wasilewska, B.; Sobieszczańska-Małek, M.; Stepnowska, M.; Przybylski, A.; Browarek, A.; Szumowski, Ł.; et al. Home-based telemonitored Nordic walking training is well accepted, safe, effective and has high adherence among heart failure patients, including those with cardiovascular implantable electronic devices: A randomised controlled study. Eur. J. Prev. Cardiol. 2015, 22, 1368–1377. [Google Scholar] [CrossRef] [PubMed]
- Piotrowicz, E.; Piepoli, M.F.; Jaarsma, T.; Lambrinou, E.; Coats, A.J.; Schmid, J.P.; Corrà, U.; Agostoni, P.; Dickstein, K.; Seferović, P.M.; et al. Telerehabilitation in heart failure patients: The evidence and the pitfalls. Int. J. Cardiol. 2016, 220, 408–413. [Google Scholar] [CrossRef]
- Krzowski, B.; Skoczylas, K.; Osak, G.; Żurawska, N.; Peller, M.; Kołtowski, Ł.; Zych, A.; Główczyńska, R.; Lodziński, P.; Grabowski, M.; et al. Kardia Mobile and ISTEL HR applicability in clinical practice: A comparison of Kardia Mobile, ISTEL HR, and standard 12-lead electrocardiogram records in 98 consecutive patients of a tertiary cardiovascular care centre. Eur. Heart J. Digit. Health 2021, 2, 467–476. [Google Scholar] [CrossRef]
- Świerad, M.; Dyrbuś, K.; Szkodziński, J.; Zembala, M.O.; Kalarus, Z.; Gąsior, M. Telehealth visits in a tertiary cardiovascular center as a response of the healthcare system to the severe acute respiratory syndrome coronavirus 2 pandemic in Poland. Pol. Arch. Intern Med. 2020, 130, 700–703. [Google Scholar]
- Sabiniewicz, A.; Lubocka, P.; Sabiniewicz, R. Case Report: Right Heart Failure Mistaken for Obesity—A Fault of Telemedicine. Front. Pediatr. 2022, 10, 856911. [Google Scholar] [CrossRef]
- Główczyńska, R.; Piotrowicz, E.; Szalewska, D.; Piotrowicz, R.; Kowalik, I.; Pencina, M.J.; Zaręba, W.; Banach, M.; Orzechowski, P.; Pluta, S.; et al. Effects of hybrid comprehensive telerehabilitation on cardiopulmonary capacity in heart failure patients depending on diabetes mellitus: Subanalysis of the TELEREH-HF randomized clinical trial. Cardiovasc. Diabetol. 2021, 20, 106. [Google Scholar] [CrossRef]
- Piotrowicz, R.; Krzesiński, P.; Balsam, P.; Piotrowicz, E.; Kempa, M.; Lewicka, E.; Główczyńska, R.; Grabowski, M.; Kołtowski, Ł.; Peller, M.; et al. Telemedicine solutions in cardiology: A joint expert opinion by the Information Technology and Telemedicine Committee of the Polish Cardiac Society, the Section of Noninvasive Electrocardiology and Telemedicine of the Polish Cardiac Society, and the Clinical Research Committee of the Polish Academy of Sciences (short version, 2021). Kardiol. Pol. (Pol. Heart J.) 2021, 79, 227–241. [Google Scholar]
- Piotrowicz, E.; Orzechowski, P.; Kowalik, I.; Zaręba, W.; Pencina, M.; Komar, E.; Opolski, G.; Banach, M.; Pluta, S.; Główczyńska, R.; et al. Predictors of proarrhythmic effect in heart failure patients after 9-week hybrid comprehensive telerehabilitation and their influence on cardiovascular mortality in long-term follow-up: Subanalysis of the TELEREH-HF randomized clinical trial. J. Electrocardiol. 2022, 75, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Piotrowicz, E.; Mierzyńska, A.; Jaworska, I.; Opolski, G.; Banach, M.; Zaręba, W.; Kowalik, I.; Pencina, M.; Orzechowski, P.; Szalewska, D.; et al. Relationship between physical capacity and depression in heart failure patients undergoing hybrid comprehensive telerehabilitation vs. usual care: Subanalysis from the TELEREH-HF Randomized Clinical Trial. Eur. J. Cardiovasc. Nurs. 2022, 21, 568–577. [Google Scholar] [CrossRef] [PubMed]
- Piotrowicz, E. eHealth for maintenance cardiovascular rehabilitation-current status and future challenges. Eur. J. Prev. Cardiol. 2023, 30, 1632–1633. [Google Scholar] [CrossRef]
- Piotrowicz, E.; Pencina, M.; Kowalik, I.; Orzechowski, P.; Banach, M.; Glowczynska, R.; Zareba, W.; Opolski, G.; Szalewska, D.; Pluta, S.; et al. Predictors of long-term prognosis based on clinical status and measurements obtained in heart failure patients after 9-week hybrid comprehensive telerehabilitation: A subanalysis of the TELEREH-HF randomized clinical trial. Kardiol. Pol. 2023, 81, 726–736. [Google Scholar] [CrossRef]
- Krzesiński, P.; Siebert, J.; Jankowska, E.A.; Banasiak, W.; Piotrowicz, K.; Stańczyk, A.; Galas, A.; Walczak, A.; Murawski, P.; Chrom, P.; et al. Rationale and design of the AMULET study: A new Model of telemedical care in patients with heart failure. ESC Heart Fail. 2021, 8, 2569–2579. [Google Scholar] [CrossRef]
- Paskudzka, D.; Kołodzińska, A.; Cacko, A.; Stolarz, P.; Łyżwiński, Ł.; Opolski, G.; Grabowski, M. Telephone follow-up of patients with cardiovascular implantable electronic devices during the coronavirus disease 2019 pandemic: Early results. Kardiol. Pol. 2020, 78, 725–731. [Google Scholar] [CrossRef]
- Orzechowski, P.; Piotrowicz, R.; Zaręba, W.; Główczyńska, R.; Szalewska, D.; Pluta, S.; Irzmański, R.; Kalarus, Z.; Banach, M.; Opolski, G.; et al. Assessment of ECG during hybrid comprehensive telerehabilitation in heart failure patients-Subanalysis of the Telerehabilitation in Heart Failure Patients (TELEREH-HF) randomized clinical trial. Ann. Noninvasive Electrocardiol. 2021, 26, e12887. [Google Scholar] [CrossRef]
- Niewada, M.; Tabor, B.; Piotrowicz, E.; Piotrowicz, R.; Opolski, G.; Banach, M.; Jakubczyk, M. Cost-effectiveness of telerehabilitation in patients with heart failure in Poland: An analysis based on the results of Telerehabilitation in the Heart Failure Patients (TELEREH-HF) randomized clinical trial. Kardiol. Pol. 2021, 79, 510–516. [Google Scholar] [CrossRef]
- Kędzierski, K.; Radziejewska, J.; Sławuta, A.; Wawrzyńska, M.; Arkowski, J. Telemedicine in Cardiology: Modern Technologies to Improve Cardiovascular Patients’ Outcomes—A Narrative Review. Medicina 2022, 58, 210. [Google Scholar] [CrossRef] [PubMed]
- Sokolski, M.; Kalużna-Oleksy, M.; Tycińska, A.; Jankowska, E.A. Telemedicine in Heart Failure in the COVID-19 and Post-Pandemic Era: What Have We Learned? Biomedicines 2023, 11, 2222. [Google Scholar] [CrossRef] [PubMed]
- Kotalczyk, A.; Imberti, J.F.; Lip, G.Y.H.; Wright, D.J. Telemedical Monitoring Based on Implantable Devices-the Evolution Beyond the CardioMEMS™ Technology. Curr. Heart Fail. Rep. 2022, 19, 7–14. [Google Scholar] [CrossRef]
- Milewski, K.; Balsam, P.; Kachel, M.; Sitek, B.; Kolarczyk-Haczyk, A.; Skoczyński, S.; Hirnle, P.; Gawałko, M.; Kołtowski, Ł.; Główczynska, R.; et al. Actual status and future directions of cardiac telerehabilitation. Cardiol. J. 2023, 30, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Uchmanowicz, I.; Wleklik, M.; Foster, M.; Olchowska-Kotala, A.; Vellone, E.; Kaluzna-Oleksy, M.; Szczepanowski, R.; Uchmanowicz, B.; Reczuch, K.; Jankowska, E.A. Digital health and modern technologies applied in patients with heart failure: Can we support patients’ psychosocial well-being? Front. Psychol. 2022, 13, 940088. [Google Scholar] [CrossRef]
- Rudnicka, Z.; Pręgowska, A.; Glądys, K.; Perkins, M.; Proniewska, K. Advancements in artificial intelligence-driven techniques for interventional cardiology. Cardiol. J. 2024, 31, 321–341. [Google Scholar] [CrossRef]
- Maciejewski, C.; Ozierański, K.; Barwiołek, A.; Basza, M.; Bożym, A.; Ciurla, M.; Janusz Krajsman, M.; Maciejewska, M.; Lodziński, P.; Opolski, G.; et al. AssistMED project: Transforming cardiology cohort characterisation from electronic health records through natural language processing—Algorithm design, preliminary results, and field prospects. Int. J. Med. Inform. 2024, 185, 105380. [Google Scholar] [CrossRef]
- Pająk, A.; Przybyło, J.; Augustyniak, P. Touchless Heart Rate Monitoring from an Unmanned Aerial Vehicle Using Videoplethysmography. Sensors 2023, 23, 7297. [Google Scholar] [CrossRef] [PubMed]
- Kalańska-Łukasik, B.; Gładyś, A.; Jadczyk, T.; Gruz-Kwapisz, M.; Wojakowski, W.; Kowalska, M. Readiness for Telemedical Services in Patients with Cardiovascular Diseases: Cross-sectional Study. JMIR Form Res. 2022, 6, e33769. [Google Scholar] [CrossRef]
- Paskudzka, D.; Januszkiewicz, Ł.; Załuska, R.; Kołodzińska, A.; Łyżwiński, Ł.; Grabowski, M. Patients with Cardiovascular Implantable Electronic Devices in the Era of COVID-19 and Their Response to Telemedical Solutions. Medicina 2022, 58, 160. [Google Scholar] [CrossRef]
- Krzowski, B.; Boszko, M.; Peller, M.; Hoffman, P.; Żurawska, N.; Skoczylas, K.; Osak, G.; Kołtowski, Ł.; Grabowski, M.; Opolski, G.; et al. Mobile App and Digital System for Patients after Myocardial Infarction (afterAMI): Results from a Randomized Trial. J. Clin. Med. 2023, 12, 2886. [Google Scholar] [CrossRef]
- Krzowski, B.; Boszko, M.; Peller, M.; Hoffman, P.; Żurawska, N.; Skoczylas, K.; Osak, G.; Kołtowski, Ł.; Grabowski, M.; Opolski, G.; et al. Mobile application and digital system for patients after myocardial infarction: Early results from a randomized trial. Pol. Arch. Intern. Med. 2023, 133, 16452. [Google Scholar] [PubMed]
- Wańczura, P.; Aebisher, D.; Wiśniowski, M.; Kos, M.; Bukowski, H.; Hołownia-Voloskova, M.; Przybylski, A. Telemedical Intervention and Its Effect on Quality of Life in Chronic Heart Failure Patients: The Results from the Telemedicine and eHealth Solution Pilot Program. J. Clin. Med. 2024, 13, 2604. [Google Scholar] [CrossRef] [PubMed]
- Orzechowski, P.; Kowalik, I.; Piotrowicz, E. Feasibility of hybrid telerehabilitation as a component of the Managed Care after Acute Myocardial Infarction (MC-AMI) program in a 12-month follow-up: Experience from a single center. Pol. Arch. Intern. Med. 2023, 133, 16456. [Google Scholar] [PubMed]
- Szalewska, D.; Główczyńska, R.; Piotrowicz, R.; Kowalik, I.; Pencina, M.J.; Opolski, G.; Zaręba, W.; Banach, M.; Orzechowski, P.; Pluta, S.; et al. An aetiology-based subanalysis of the Telerehabilitation in Heart Failure Patients (TELEREH-HF) trial. ESC Heart Fail. 2021, 8, 1263–1273. [Google Scholar] [CrossRef]
- Wita, M.; Orszulak, M.; Szydło, K.; Wróbel, W.; Filipecki, A.; Simionescu, K.; Sanecki, K.; Uchwat, U.; Wybraniec, M.; Tabor, Z.; et al. The usefulness of telemedicine devices in patients with severe heart failure with an implanted cardiac resynchronization therapy system during two years of observation. Kardiol. Pol. 2022, 80, 41–48. [Google Scholar] [CrossRef]
- Łudzik, J.; Witkowski, A.M.; Roterman-Konieczna, I. New telemedicine techniques in dermatology—Evaluation with reflectance confocal microscopy via cloud-based platform. Folia Med. Cracov. 2016, 56, 21–29. [Google Scholar] [PubMed]
- Goldust, M.; Shivakumar, S.; Kroumpouzos, G.; Murrell, D.F.; Rudnicka, L.; Jafferany, M.; Navarini, A.A. Virtual conferences of dermatology during the COVID-19 pandemic. Dermatol. Ther. 2020, 33, e13774. [Google Scholar] [CrossRef]
- Sieniawska, J.; Lesiak, A.; Ciążyński, K.; Narbutt, J.; Ciążyńska, M. Impact of the COVID-19 Pandemic on Atopic Dermatitis Patients. Int. J. Environ. Res. Public Health 2022, 19, 1734. [Google Scholar] [CrossRef]
- Ziętek, M.; Nowacki, M.; Wierzbicki, J.; Matkowski, R.; Maciejczyk, A.; Czajkowski, R.; Pawlak-Adamska, E. The report and analysis concerning the usefulness of basic telemedicine tools in the skin cancer diagnostic screening process during COVID-19 pandemics. Postep. Dermatol. Alergol. 2022, 39, 189–194. [Google Scholar] [CrossRef]
- Pala, P.; Bergler-Czop, B.S.; Gwiżdż, J.M. Teledermatology: Idea, benefits and risks of modern age—A systematic review based on melanoma. Postep. Dermatol. Alergol. 2020, 37, 159–167. [Google Scholar] [CrossRef]
- Lee, C.; Witkowski, A.; Żychowska, M.; Ludzik, J. The role of mobile teledermoscopy in skin cancer triage and management during the COVID-19 pandemic. Indian J. Dermatol. Venereol. Leprol. 2023, 89, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Patrzyk, S.; Bielecki, W.; Woźniacka, A. A study of attitudes among Polish dermatologists and dermatology trainees regarding modern technologies in medicine. Postep. Dermatol Alergol 2022, 39, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Gierek, M.; Kitala, D.; Łabuś, W.; Glik, J.; Szyluk, K.; Pietrauszka, K.; Bergler-Czop, B.; Niemiec, P. The Impact of Telemedicine on Patients with Hidradenitis Suppurativa in the COVID-19 Era. Healthcare 2023, 11, 1453. [Google Scholar] [CrossRef]
- Woźna, J.; Stępka, J.; Bałoniak, A.; Żaba, R. Teledermatology in the diagnosis and treatment of sexually transmitted infections: A narrative review. Postep. Dermatol. Alergol. 2024, 41, 1–8. [Google Scholar] [CrossRef]
- Stepaniuk, A.; Pawlukianiec, C.; Krawiel, M.; Lewoc, M.; Baran, A.; Flisiak, I. Great hopes or disappointment—A survey-based study on patients’ and doctors’ perception of telemedicine during the COVID-19 pandemic in Poland. Postep. Dermatol. Alergol. 2022, 39, 384–391. [Google Scholar] [CrossRef]
- Bujnowska-Fedak, M.M.; Pirogowicz, I. Support for eHealth services among elderly primary care patients. Telemed. J. eHealth 2014, 20, 696–704. [Google Scholar] [CrossRef]
- Bujnowska-Fedak, M.M. Trends in the use of the Internet for health purposes in Poland. BMC Public Health 2015, 15, 194. [Google Scholar] [CrossRef] [PubMed]
- Duplaga, M.; Sobecka, K.; Wójcik, S. The Reliability and Validity of the Telephone-Based and Online Polish eHealth Literacy Scale Based on Two Nationally Representative Samples. Int. J. Environ. Res. Public Health 2019, 16, 3216. [Google Scholar] [CrossRef] [PubMed]
- Duplaga, M. A cross-sectional study assessing determinants of the attitude to the introduction of eHealth services among patients suffering from chronic conditions. BMC Med. Inform. Decis. Mak. 2015, 15, 33. [Google Scholar] [CrossRef]
- Wołk, K.; Marasek, K.; Glinkowski, W. Telemedicine as a special case of machine translation. Comput. Med. Imaging Graph. 2015, 46 Pt 2, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Duplaga, M.; Turosz, N. User satisfaction and the readiness-to-use eHealth applications in the future in Polish society in the early phase of the COVID-19 pandemic: A cross-sectional study. Int. J. Med. Inform. 2022, 168, 104904. [Google Scholar] [CrossRef]
- Duplaga, M. A Nationwide Natural Experiment of eHealth Implementation during the COVID-19 Pandemic in Poland: User Satisfaction and the Ease-of-Use of Remote Physician’s Visits. Int. J. Environ. Res. Public Health 2022, 19, 8338. [Google Scholar] [CrossRef]
- Rój, J. What Determines the Acceptance and Use of eHealth by Older Adults in Poland? Int. J. Environ. Res. Public Health 2022, 19, 15643. [Google Scholar] [CrossRef]
- Rój, J. Inequity in the Access to eHealth and Its Decomposition Case of Poland. Int. J. Environ. Res. Public Health 2022, 19, 2340. [Google Scholar] [CrossRef]
- Krysta, K.; Romańczyk, M.; Diefenbacher, A.; Krzystanek, M. Telemedicine Treatment and Care for Patients with Intellectual Disability. Int. J. Environ. Res. Public Health 2021, 18, 1746. [Google Scholar] [CrossRef]
- Ćwiklicki, M.; Schiavone, F.; Klich, J.; Pilch, K. Antecedents of use of eHealth services in Central Eastern Europe: A qualitative comparative analysis. BMC Health Serv. Res. 2020, 20, 171. [Google Scholar] [CrossRef]
- Burzyńska, J.; Rękas, M.; Januszewicz, P. Evaluating the Psychometric Properties of the eHealth Literacy Scale (eHEALS) among Polish Social Media Users. Int. J. Environ. Res. Public Health 2022, 19, 4067. [Google Scholar] [CrossRef]
- Mayer, A.; Da Silva Domingues, V.; Hege, I.; Kononowicz, A.A.; Larrosa, M.; Martínez-Jarreta, B.; Rodriguez-Molina, D.; Sousa-Pinto, B.; Sudacka, M.; Morin, L. Planning a Collection of Virtual Patients to Train Clinical Reasoning: A Blueprint Representative of the European Population. Int. J. Environ. Res. Public Health 2022, 19, 6175. [Google Scholar] [CrossRef] [PubMed]
- Jankowiak, M.; Rój, J. The eHealth usage during COVID-19 pandemic 2020 year-Case of Poland. PLoS ONE 2023, 18, e0290502. [Google Scholar] [CrossRef] [PubMed]
- Płaciszewski, K.; Wierzba, W.; Ostrowski, J.; Pinkas, J.; Jankowski, M. Factors associated with the use of public eHealth services in Poland—A 2022 nationwide cross-sectional survey. Ann. Agric. Environ. Med. 2023, 30, 127–134. [Google Scholar] [CrossRef]
- Burrell, A.; Zrubka, Z.; Champion, A.; Zah, V.; Vinuesa, L.; Holtorf, A.P.; Di Bidino, R.; Earla, J.R.; Entwistle, J.; Boltyenkov, A.T.; et al. How Useful Are Digital Health Terms for Outcomes Research? An ISPOR Special Interest Group Report. Value Health 2022, 25, 1469–1479. [Google Scholar] [CrossRef]
- Wróbel, S.; Turek, C.; Stępień, E.; Piwowar, M. Data integration through canonical correlation analysis and its application to OMICs research. J. Biomed. Inform. 2024, 151, 104575. [Google Scholar] [CrossRef] [PubMed]
- Ucinski, T.; Dolata, G.; Hełminiak, R.; Fischer, L.; Fleßa, S.; Brehmer, B.; Viert, A.; Grundmann, V.; Rehberg, S.; Krügel, K.; et al. Integrating cross-border emergency medicine systems: Securing future preclinical medical workforce for remote medical services. Best Pract. Res. Clin. Anaesthesiol. 2018, 32, 39–46. [Google Scholar] [CrossRef]
- Więch, P.; Muster, M.; Bazaliński, D.; Kucaba, G.; Sałacińska, I.; Januszewicz, P.; Wołoszczuk-Gębicka, B. A pilot, prospective, randomized trial to evaluate the influence of telemedicine training on the CPR quality provided by the nurses. Am. J. Emerg. Med. 2018, 36, 1913–1914. [Google Scholar] [CrossRef]
- Więch, P.; Sałacińska, I.; Muster, M.; Bazaliński, D.; Kucaba, G.; Fąfara, A.; Przybek-Mita, J.; Januszewicz, P. Use of Selected Telemedicine Tools in Monitoring Quality of In-Hospital Cardiopulmonary Resuscitation: A Prospective Observational Pilot Simulation Study. Med. Sci. Monit. 2019, 25, 2520–2526. [Google Scholar] [CrossRef]
- Sowizdraniuk, J.; Smereka, J.; Ladny, J.R.; Kaserer, A.; Palimonka, K.; Ruetzler, K.; Skierczynska, A.; Szarpak, L. ECG pre-hospital teletransmission by emergency teams staffed with an emergency physician and paramedics and its impact on transportation and hospital admission. Medicine 2019, 98, e16636. [Google Scholar] [CrossRef]
- Witkowska-Zimny, M.; Nieradko-Iwanicka, B. Telemedicine in Emergency Medicine in the COVID-19 Pandemic-Experiences and Prospects—A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 8216. [Google Scholar] [CrossRef]
- Skarzyński, P.H.; Świerniak, W.; Piłka, A.; Skarżynska, M.B.; Włodarczyk, A.W.; Kholmatov, D.; Makhamadiev, A.; Hatzopoulos, S. A Hearing Screening Program for Children in Primary Schools in Tajikistan: A Telemedicine Model. Med. Sci. Monit. 2016, 22, 2424–2430. [Google Scholar] [CrossRef] [PubMed]
- Krajewska Wojciechowska, J.; Krajewski, W.; Zub, K.; Zatoński, T. Review of practical recommendations for otolaryngologists and head and neck surgeons during the COVID-19 pandemic. Auris Nasus Larynx 2020, 47, 544–558. [Google Scholar] [CrossRef] [PubMed]
- Obrębski, J.; Skorek, P.; Tretiakow, D.; Narożny, W.; Skorek, A. [Patient in the otolaryngology office in the time of the COVID-19 pandemic in the light of current recommendations, legal regulations and authors’ own experience]. Med. Pract. 2021, 72, 327–334. [Google Scholar] [CrossRef]
- Greczka, G.; Dąbrowski, P.; Zych, M.; Szyfter, W.; Wierzbicka, M. The impact of the COVID 19 pandemic on the functioning of the Universal Newborn Hearing Screening Program in Poland. Otolaryngol. Pol. 2022, 76, 1–5. [Google Scholar] [CrossRef]
- Kutyba, J.J.; Jędrzejczak, W.W.; Gos, E.; Raj-Koziak, D.; Skarzynski, P.H. Chronic Tinnitus and the Positive Effects of Sound Treatment via a Smartphone App: Mixed-Design Study. JMIR Mhealth Uhealth 2022, 10, e33543. [Google Scholar] [CrossRef] [PubMed]
- Pietruszewska, W.; Burduk, P.; Rosiak, O.; Podlawska, P.; Zakrzewski, B.; Barańska, M.; Kowalczyk, M.; Piątkowski, J.; Śmigielski, G.; Solarz, P.; et al. Impact of COVID-19 on Head and Neck Cancer Advancement Measured by Increasing Numbers of Urgent Dyspnea Cases-What Could Be Improved in the Event of Subsequent Pandemics? J. Clin. Med. 2022, 11, 6385. [Google Scholar] [CrossRef]
- Buliński, L.; Błachnio, A. Health in old age, and patients’ approaches to telemedicine in Poland. Ann. Agric. Environ. Med. 2017, 24, 322–328. [Google Scholar] [CrossRef]
- Starzec-Proserpio, M.; Vandyken, C. Telerehabilitation for persistent Pelvic Girdle Pain within a biopsychosocial framework—A case report. Physiother. Theory Pract. 2023, 39, 2251–2261. [Google Scholar] [CrossRef]
- Jankowska-Polańska, B.; Kałuska, M.; Mazurek, T.; Badura, A.; Lisiewicz-Jakubaszko, J.; Tomasiewicz, B.; Tański, W. The Framework of the Pilot Project for Testing a Telemedicine Model in the Field of Geriatrics—Health Challenges and Justification of the Project Implementation. Pol. Merkur. Lek. 2023, 51, 665–673. [Google Scholar] [CrossRef]
- Paszkowska, M. [Medical teleconsultation in the polish healthcare system]. Wiad Lek. 2019, 72, 1343–1349. [Google Scholar] [CrossRef]
- Bujnowska-Fedak, M.M.; Wysoczański, Ł. Access to an Electronic Health Record: A Polish National Survey. Int. J. Environ. Res. Public Health 2020, 17, 6165. [Google Scholar] [CrossRef]
- Tajstra, M.; Sokal, A.; Gwóźdź, A.; Wilczek, M.; Gacek, A.; Wojciechowski, K.; Gadula-Gacek, E.; Adamowicz-Czoch, E.; Chłosta-Niepiekło, K.; Milewski, K.; et al. REmote SUpervision to Decrease HospitaLization RaTe. Unified and integrated platform for data collected from devices manufactured by different companies: Design and rationale of the RESULT study. Ann. Noninvasive Electrocardiol. 2017, 22, e12418. [Google Scholar] [CrossRef] [PubMed]
- Grata-Borkowska, U.; Sobieski, M.; Drobnik, J.; Fabich, E.; Bujnowska-Fedak, M.M. Perception and Attitude toward Teleconsultations among Different Healthcare Professionals in the Era of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 11532. [Google Scholar] [CrossRef] [PubMed]
- Burzyńska, J.; Bartosiewicz, A.; Januszewicz, P. Dr. Google: Physicians-The Web-Patients Triangle: Digital Skills and Attitudes towards eHealth Solutions among Physicians in South Eastern Poland—A Cross-Sectional Study in a Pre-COVID-19 Era. Int. J. Environ. Res. Public Health 2023, 20, 978. [Google Scholar] [CrossRef] [PubMed]
- Romaszko-Wojtowicz, A.; Maksymowicz, S.; Jarynowski, A.; Jaśkiewicz, Ł.; Czekaj, Ł.; Doboszyńska, A. Telemonitoring in Long-COVID Patients-Preliminary Findings. Int. J. Environ. Res. Public Health 2022, 19, 5268. [Google Scholar] [CrossRef]
- Pogorzelska, K.; Chlabicz, S. Patient Satisfaction with Telemedicine during the COVID-19 Pandemic—A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 6113. [Google Scholar] [CrossRef]
- Praus, F.; Krzowski, B.; Walther, T.; Gratzke, C.; Balsam, P.; Miernik, A.; Pohlmann, P.F. Smartphone Apps for Managing Antithrombotic Therapy: Scoping Literature Review. JMIR Cardio 2022, 6, e29481. [Google Scholar] [CrossRef]
- Kolasa, K.; Kozinski, G. How to Value Digital Health Interventions? A Systematic Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 2119. [Google Scholar] [CrossRef]
- van Kessel, R.; Srivastava, D.; Kyriopoulos, I.; Monti, G.; Novillo-Ortiz, D.; Milman, R.; Zhang-Czabanowski, W.W.; Nasi, G.; Stern, A.D.; Wharton, G.; et al. Digital Health Reimbursement Strategies of 8 European Countries and Israel: Scoping Review and Policy Mapping. JMIR Mhealth Uhealth 2023, 11, e49003. [Google Scholar] [CrossRef]
- Duplaga, M. Predictors of the Use of Physician’s Televisits During the COVID-19 Pandemic in Poland. Stud. Health Technol. Inform. 2024, 310, 1106–1110. [Google Scholar]
- Tański, W.; Stapkiewicz, A.; Szalonka, A.; Głuszczyk-Ferenc, B.; Tomasiewicz, B.; Jankowska-Polańska, B. The Framework of the Pilot Project for Testing a Telemedicine Model in the Field of Chronic Diseases—Health Challenges and Justification of the Project Implementation. Pol. Merkur Lekarski 2023, 51, 674–681. [Google Scholar] [CrossRef]
- Petrazzuoli, F.; Gokdemir, O.; Antonopoulou, M.; Blahova, B.; Mrduljaš-Đujić, N.; Dumitra, G.; Falanga, R.; Ferreira, M.; Gintere, S.; Hatipoglu, S.; et al. Patient consultations during SARS-CoV-2 pandemic: A mixed-method cross-sectional study in 16 European countries. Rural Remote Health 2022, 22, 7196. [Google Scholar] [CrossRef]
- Frankowska, A.; Szymkowiak, M.; Walkowiak, D. Teleconsultations Quality During the COVID-19 Pandemic in Poland in the Opinions of Generation Z Adults. Telemed. J. eHealth 2022, 28, 1843–1851. [Google Scholar] [CrossRef]
- Waligóra, J.; Bujnowska-Fedak, M.M. Online Health Technologies and Mobile Devices: Attitudes, Needs, and Future. Adv. Exp. Med. Biol. 2019, 1153, 19–29. [Google Scholar]
- Merks, P.; Religioni, U.; Arciszewska, K.; Pankiewicz, W.; Jaguszewski, M.; Vaillancourt, R. Usability testing and satisfaction of “The Patient Access”: A mobile health application for patients with venous thromboembolic disease. A pilot study. Cardiol. J. 2020, 27, 891–893. [Google Scholar] [CrossRef]
- Kańtoch, E.; Kańtoch, A. Cardiovascular and Pre-Frailty Risk Assessment During Shelter-In-Place Measures Based on Multimodal Biomarkers Collected from Smart Telemedical Wearables. J. Clin. Med. 2021, 10, 1997. [Google Scholar] [CrossRef]
- Kańtoch, E.; Kańtoch, A. What Features and Functions Are Desired in Telemedical Services Targeted at Polish Older Adults Delivered by Wearable Medical Devices?—Pre-COVID-19 Flashback. Sensors 2020, 20, 5181. [Google Scholar] [CrossRef]
- Manninger, M.; Zweiker, D.; Svennberg, E.; Chatzikyriakou, S.; Pavlovic, N.; Zaman, J.A.B.; Kircanski, B.; Lenarczyk, R.; Vanduynhoven, P.; Kosiuk, J.; et al. Current perspectives on wearable rhythm recordings for clinical decision-making: The wEHRAbles 2 survey. Europace 2021, 23, 1106–1113. [Google Scholar] [CrossRef]
- Ammenwerth, E.; Wilk, S.; Huang, Z. Personalization in mHealth: Innovative informatics methods to improve patient experience and health outcome. J. Biomed. Inform. 2022, 133, 104143. [Google Scholar] [CrossRef]
- Peleg, M.; Veggiotti, N.; Sacchi, L.; Wilk, S. How can we reward you? A compliance and reward ontology (CaRO) for eliciting quantitative reward rules for engagement in mHealth app and healthy behaviors. J. Biomed. Inform. 2024, 154, 104655. [Google Scholar] [CrossRef]
- Grzeszczyk, M.K.; Adamczyk, P.; Marek, S.; Pręcikowski, R.; Kuś, M.; Lelujko, M.P.; Blanco, R.; Trzciński, T.; Sitek, A.; Malawski, M.; et al. Can gamification reduce the burden of self-reporting in mHealth applications? A feasibility study using machine learning from smartwatch data to estimate cognitive load. AMIA Annu. Symp. Proc. 2023, 2023, 389–396. [Google Scholar] [PubMed]
- Staszuk, A.; Wiatrak, B.; Tadeusiewicz, R.; Karuga-Kuźniewska, E.; Rybak, Z. Telerehabilitation approach for patients with hand impairment. Acta Bioeng. Biomech. 2016, 18, 55–62. [Google Scholar] [PubMed]
- Saran, T.; Pedrycz, A.; Mucha, D.; Mucha, D. Follow-up monitoring of physical activity after rehabilitation by means of a mobile application: Effectiveness of measurements in different age groups. Adv. Clin. Exp. Med. 2018, 27, 1037–1044. [Google Scholar] [CrossRef] [PubMed]
- Sobierajska-Rek, A.; Mański, Ł.; Jabłońska-Brudło, J.; Śledzińska, K.; Wasilewska, E.; Szalewska, D. Respiratory Telerehabilitation of Boys and Young Men with Duchenne Muscular Dystrophy in the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 6179. [Google Scholar] [CrossRef]
- Sobierajska-Rek, A.; Mański, Ł.; Jabłońska-Brudło, J.; Śledzińska, K.; Ucińska, A.; Wierzba, J. Establishing a telerehabilitation program for patients with Duchenne muscular dystrophy in the COVID-19 pandemic. Wien. Klin. Wochenschr. 2021, 133, 344–350. [Google Scholar] [CrossRef]
- Zasadzka, E.; Trzmiel, T.; Pieczyńska, A.; Hojan, K. Modern Technologies in the Rehabilitation of Patients with Multiple Sclerosis and Their Potential Application in Times of COVID-19. Medicina 2021, 57, 549. [Google Scholar] [CrossRef]
- Cieślik, B.; Kuligowski, T.; Cacciante, L.; Kiper, P. The Impact of Personality Traits on Patient Satisfaction after Telerehabilitation: A Comparative Study of Remote and Face-to-Face Musculoskeletal Rehabilitation during COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2023, 20, 5019. [Google Scholar] [CrossRef]
- Cacciante, L.; Pietà, C.D.; Rutkowski, S.; Cieślik, B.; Szczepańska-Gieracha, J.; Agostini, M.; Kiper, P. Cognitive telerehabilitation in neurological patients: Systematic review and meta-analysis. Neurol. Sci. 2022, 43, 847–862. [Google Scholar] [CrossRef]
- Zampolini, M.; Oral, A.; Barotsis, N.; Aguiar Branco, C.; Burger, H.; Capodaglio, P.; Dincer, F.; Giustini, A.; Hu, X.; Irgens, I.; et al. Evidence-based position paper on Physical and Rehabilitation Medicine (PRM) professional practice on telerehabilitation. The European PRM position (UEMS PRM Section). Eur. J. Phys. Rehabil. Med. 2024, 60, 165–181. [Google Scholar] [CrossRef]
- Maciejewski, M.; Surtel, W.; Wójcik, W.; Masiak, J.; Dzida, G.; Horoch, A. Telemedical systems for home monitoring of patients with chronic conditions in rural environment. Ann. Agric. Environ. Med. 2014, 21, 167–173. [Google Scholar]
- Duplaga, M. Searching for a Role of Nursing Personnel in Developing Landscape of Ehealth: Factors Determining Attitudes toward Key Patient Empowering Applications. PLoS ONE 2016, 11, e0153173. [Google Scholar] [CrossRef][Green Version]
- Dziurka, M.; Machul, M.; Ozdoba, P.; Obuchowska, A.; Kotowski, M.; Grzegorczyk, A.; Pydyś, A.; Dobrowolska, B. Clinical Training During the COVID-19 Pandemic: Experiences of Nursing Students and Implications for Education. Int. J. Environ. Res. Public Health 2022, 19, 6352. [Google Scholar] [CrossRef]
- Andersson, E.K.; Dallora, A.L.; Marcinowicz, L.; Stjernberg, L.; Björling, G.; Anderberg, P.; Bohman, D. Self-Reported eHealth literacy among nursing students in Sweden and Poland: The eNursEd cross-sectional multicentre study. Health Inform. J. 2023, 29, 14604582231214588. [Google Scholar] [CrossRef]
- Agrawal, S.; Strzelec, B.; Poręba, R.; Agrawal, A.; Mazur, G. Clinical Characteristics, Preventive Care and Attitude to Telemedicine Among Patients with Diabetic Retinopathy: A Cross-Sectional Study. J. Clin. Med. 2021, 10, 249. [Google Scholar] [CrossRef]
- Binder-Olibrowska, K.W.; Wrzesińska, M.A.; Godycki-Ćwirko, M. Is Telemedicine in Primary Care a Good Option for Polish Patients with Visual Impairments Outside of a Pandemic? Int. J. Environ. Res. Public Health 2022, 19, 6357. [Google Scholar] [CrossRef]
- Saeed, E.; Szymkowski, M.; Saeed, K.; Mariak, Z. An Approach to Automatic Hard Exudate Detection in Retina Color Images by a Telemedicine System Based on the d-Eye Sensor and Image Processing Algorithms. Sensors 2019, 19, 695. [Google Scholar] [CrossRef]
- Pieczynski, J.; Kuklo, P.; Grzybowski, A. The Role of Telemedicine, In-Home Testing and Artificial Intelligence to Alleviate an Increasingly Burdened Healthcare System: Diabetic Retinopathy. Ophthalmol. Ther. 2021, 10, 445–464. [Google Scholar] [CrossRef]
- Dolar-Szczasny, J.; Barańska, A.; Rejdak, R. Evaluating the Efficacy of Teleophthalmology in Delivering Ophthalmic Care to Underserved Populations: A Literature Review. J. Clin. Med. 2023, 12, 3161. [Google Scholar] [CrossRef]
- Czyzewska, A.; Glinkowski, W.M.; Walesiak, K.; Krawczak, K.; Cabaj, D.; Gorecki, A. Effects of preoperative physiotherapy in hip osteoarthritis patients awaiting total hip replacement. Arch. Med. Sci. AMS 2014, 10, 985–991. [Google Scholar] [CrossRef] [PubMed]
- Glinkowski, W.; Michoński, J.; Zukowska, A.; Glinkowska, B.; Sitnik, R.; Górecki, A. The time effectiveness of three-dimensional telediagnostic postural screening of back curvatures and scoliosis. Telemed. J. eHealth 2014, 20, 11–17. [Google Scholar] [CrossRef]
- Miekisiak, G.; Latka, D.; Sobolewski, T.; Sulewski, A.; Kubaszewski, L.; Kaczmarczyk, J. Prevalence of “red flags” among the internet user with low back pain seeking information on spinal health-a web survey. Telemed. J. eHealth 2015, 21, 120–124. [Google Scholar] [CrossRef]
- Glinkowski, W.M. Orthopedic Telemedicine Outpatient Practice Diagnoses Set during the First COVID-19 Pandemic Lockdown-Individual Observation. Int. J. Environ. Res. Public Health 2022, 19, 5418. [Google Scholar] [CrossRef] [PubMed]
- Glinkowski, W.M. Telemedicine Orthopedic Consultations Duration and Timing in Outpatient Clinical Practice During the COVID-19 Pandemic. Telemed. J. eHealth 2023, 29, 778–787. [Google Scholar] [CrossRef]
- Glinkowski, W.; Chelnokov, A.N. The orthopaedic surgeon’s clinical and experimental experience affect methods used for the fracture healing assessment (FHA)—An International Survey. Injury 2021, 52, 2205–2214. [Google Scholar] [CrossRef] [PubMed]
- Kamecka, K.; Rybarczyk-Szwajkowska, A.; Staszewska, A.; Engelseth, P.; Kozlowski, R. Process of Posthospital Care Involving Telemedicine Solutions for Patients after Total Hip Arthroplasty. Int. J. Environ. Res. Public Health 2021, 18, 10135. [Google Scholar] [CrossRef]
- Kamecka, K.; Foti, C.; Gawiński, Ł.; Matejun, M.; Rybarczyk-Szwajkowska, A.; Kiljański, M.; Krochmalski, M.; Kozłowski, R.; Marczak, M. Telemedicine Technologies Selection for the Posthospital Patient Care Process after Total Hip Arthroplasty. Int. J. Environ. Res. Public Health 2022, 19, 11521. [Google Scholar] [CrossRef]
- Bogomolets, O.; Wierzbik-Strońska, M.; Hryshchenko, R.; Bogomolets, C. Urgent Treatment of Complicated Ulcerated Infantile Hemangioma with β-Blockers via Telemedicine: A Case Report. Telemed. J. eHealth 2024, 30, 881–884. [Google Scholar] [CrossRef]
- Indolfi, G.; Stivala, M.; Lenge, M.; Diaz Naderi, R.; McIntosh, J.; Llandrich, R.C.; Gannon, J.; McGreevy, K.S.; Trapani, S.; Miettinen, P.; et al. Impact of SARS-CoV-2 Pandemic and Strategies for Resumption of Activities During the Second Wave of the Pandemic: A Report from Eight Paediatric Hospitals from the ECHO Network. Front. Public Health 2021, 9, 630168. [Google Scholar] [CrossRef] [PubMed]
- Anuszkiewicz, K.; Stogowski, P.; Zawadzka, M.; Waszak, P.; Sokolewicz, E.; Dułak, N.A.; Dzwilewski, K.; Jażdżewska, K.; Karbowiak, K.; Karlińska, D.; et al. COVID-19 pandemic influence on epilepsy course in pediatric patients. Epilepsy Behav. 2022, 129, 108581. [Google Scholar] [CrossRef]
- Papadopoulos, N.G.; Custovic, A.; Deschildre, A.; Mathioudakis, A.G.; Phipatanakul, W.; Wong, G.; Xepapadaki, P.; Agache, I.; Bacharier, L.; Bonini, M.; et al. Impact of COVID-19 on Pediatric Asthma: Practice Adjustments and Disease Burden. J. Allergy Clin. Immunol. Pract. 2020, 8, 2592–2599.e3. [Google Scholar] [CrossRef]
- Pokorska-Śpiewak, M.; Śpiewak, M. Management of hepatitis C in children and adolescents during COVID-19 pandemic. World J. Hepatol. 2020, 12, 485–492. [Google Scholar] [CrossRef]
- Reingold, S.M.; Hadjipanayis, A.; van Esso, D.; Del Torso, S.; Dornbusch, H.J.; de Guchtenaere, A.; Pancheva, R.; Mujkic, A.; Syridou, G.; Valiulis, A.; et al. COVID-19 Era Effect on Pandemic and Post-pandemic Pediatric Telemedicine Use: A Survey of the European Academy of Pediatrics Research in Ambulatory Settings Network. Front. Pediatr. 2021, 9, 713930. [Google Scholar] [CrossRef]
- Troschke, T.; Wieczorek, A.; Kulinski, K.; Ociepa, T.; Zielezinska, K.; Lode, H.N.; Urasinski, T. Pediatric Hematology and Oncology Center Integrated by Telemedicine: Experience, Challenges and First Results of a Cross Border Network. Healthcare 2023, 11, 1431. [Google Scholar] [CrossRef] [PubMed]
- Lubomski, J.; Malchrzak, W.; Babicki, M.; Kłoda, K.; Suwała, S.; Mastalerz-Migas, A. Teleconsultation as a Modern Form of Health Care Service in the Case of Poland: Assessment of Its Potential Use from the Perspective of Health Care Providers and Patients. Telemed. J. eHealth 2024, 30, 234–241. [Google Scholar] [CrossRef]
- Krzystanek, M.; Krzeszowski, D.; Jagoda, K.; Krysta, K. Long term telemedicine study of compliance in paranoid schizophrenia. Psychiatr. Danub. 2015, 27 (Suppl. S1), S266–S268. [Google Scholar] [CrossRef]
- Krzystanek, M.; Borkowski, M.; Skałacka, K.; Krysta, K. A telemedicine platform to improve clinical parameters in paranoid schizophrenia patients: Results of a one-year randomized study. Schizophr. Res. 2019, 204, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Wojtuszek, M.; Kachnic, J.; Krysta, K.; Wutke, J. Telepsychiatry in Polish patients’ and doctors’ opinion. Psychiatr. Danub. 2015, 27 (Suppl. S1), S379–S382. [Google Scholar]
- Krzystanek, M.; Borkowski, M.; Krysta, K. Psychiatry as a leader of contemporary telemedicine in Poland. Reumatologia 2018, 56, 65–66. [Google Scholar] [CrossRef]
- Rutkowska, A. Telemedicine Interventions as an Attempt to Improve the Mental Health of Populations during the COVID-19 Pandemic—A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 14945. [Google Scholar] [CrossRef]
- Wołk, K.; Wołk, A.; Marasek, K.; Glinkowski, W. Pictogram-based mobile first medical aid communicator. Procedia Comput. Sci. 2017, 121, 3–10. [Google Scholar] [CrossRef]
- Klingemann, J.; Wieczorek, Ł. Mobile application recovery support for patients with an alcohol use disorder. Acceptance, usability, and perceived helpfulness. J. Addict. Dis. 2022, 40, 559–567. [Google Scholar] [CrossRef]
- Bernard, R.M.; Toppo, C.; Raggi, A.; de Mul, M.; de Miquel, C.; Pugliese, M.T.; van der Feltz-Cornelis, C.M.; Ortiz-Tallo, A.; Salvador-Carulla, L.; Lukersmith, S.; et al. Strategies for Implementing Occupational eMental Health Interventions: Scoping Review. J. Med. Internet Res. 2022, 24, e34479. [Google Scholar] [CrossRef]
- Mazurkiewicz, D.W.; Strzelecka, J.; Piechocka, D.I. Adverse Mental Health Sequelae of COVID-19 Pandemic in the Pregnant Population and Useful Implications for Clinical Practice. J. Clin. Med. 2022, 11, 2072. [Google Scholar] [CrossRef]
- Kobryn, M.; Duplaga, M. Does Health Literacy Protect Against Cyberchondria: A Cross-Sectional Study? Telemed. J. eHealth 2024, 30, e1089–e1100. [Google Scholar] [CrossRef]
- Ochnik, D.; Cholewa-Wiktor, M.; Jakubiak, M.; Pataj, M. eHealth tools use and mental health: A cross-sectional network analysis in a representative sample. Sci. Rep. 2024, 14, 5173. [Google Scholar] [CrossRef]
- Sozański, B.; Ćwirlej-Sozańska, A.B.; Wiśniowska-Szurlej, A.; Wilmowska-Pietruszyńska, A.; Spalek, R.; de Sire, A. Geriatric Depression Scale—30 assessments: Face-to-face or telephone interviews for older people—A randomized crossover study. Ann. Agric. Environ. Med. 2024, 31, 72–77. [Google Scholar] [CrossRef]
- Miłkowska-Dymanowska, J.; Białas, A.J.; Obrębski, W.; Górski, P.; Piotrowski, W.J. A pilot study of daily telemonitoring to predict acute exacerbation in chronic obstructive pulmonary disease. Int. J. Med. Inform. 2018, 116, 46–51. [Google Scholar] [CrossRef]
- Tański, W.; Teplicki, A.; Stapkiewicz, A.; Szalonka, A.; Kulas, I.; Jankowska-Polańska, B. Challenges and opportunities in implementing telemedical solutions for COPD management in the Polish healthcare sector: A presenting own experience. Wiad Lek. 2024, 77, 1808–1817. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, S. Management Challenges in Chronic Obstructive Pulmonary Disease in the COVID-19 Pandemic: Telehealth and Virtual Reality. J. Clin. Med. 2021, 10, 1261. [Google Scholar] [CrossRef]
- Fietze, I.; Laharnar, N.; Bargiotas, P.; Basoglu, O.K.; Dogas, Z.; Drummond, M.; Fanfulla, F.; Gislason, T.; Gouveris, H.; Grote, L.; et al. Management of obstructive sleep apnea in Europe—A 10-year follow-up. Sleep Med. 2022, 97, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Sosnowski, R.; Kamecki, H.; Joniau, S.; Walz, J.; Dowling, J.; Behrendt, M.; Klaassen, Z.; Palou, J.; van Poppel, H. Uro-oncology in the era of social distancing: The principles of patient-centered online consultations during the COVID-19 pandemic. Cent. Eur. J. Urol. 2020, 73, 260–264. [Google Scholar]
- Nowak, Ł.; Krajewski, W.; Kiełb, P.; Śliwa, A.; Zdrojowy-Wełna, A.; Zdrojowy, R. COVID-19 and the urological practice: Changes and future perspectives. Cent. Eur. J. Urol. 2020, 73, 269–272. [Google Scholar]
- Naik, N.; Hameed, B.M.Z.; Nayak, S.G.; Gera, A.; Nandyal, S.R.; Shetty, D.K.; Shah, M.; Ibrahim, S.; Naik, A.; Kamath, N.; et al. Telemedicine and Telehealth in Urology-What Do the ‘Patients’ Think About It? Front. Surg. 2022, 9, 863576. [Google Scholar] [CrossRef]
- Naik, N.; Nandyal, S.R.; Nayak, S.G.; Shah, M.; Ibrahim, S.; Hameed, B.M.Z.; Patil, A.; Suresh, G.; Shetty, P.A.; Rai, B.P.; et al. Telemedicine and Telehealth in Urology: Uptake, Impact and Barriers to Clinical Adoption. Front. Surg. 2022, 9, 911206. [Google Scholar] [CrossRef]
- Symeonidis, E.N.; Veneziano, D.; Borgmann, H.; Zapała, Ł.; Zachariou, A.; Brenneis, H.; Haensel, S.M.; Haas, H.; Dimitriadis, F. Telemedicine in Urology: Where Have We Been and Where Are We Heading? Eur. Urol. Open Sci. 2023, 50, 106–112. [Google Scholar] [CrossRef]
- Ciećko, W.; Labunets, K.; Wojnarowska, M.; Bosek, D.; Skwierawska, J.; Bandurski, T.; Bandurska, E. How COVID-19 Broke the Barriers Related to the Implementation of Telecare-Patients’ Experiences with a New form of Providing Health Services in Primary Health Care. Healthcare 2023, 11, 497. [Google Scholar] [CrossRef]
- Sosnowski, R.; Kamecki, H.; Joniau, S.; Walz, J.; Klaassen, Z.; Palou, J. Introduction of Telemedicine During the COVID-19 Pandemic: A Challenge for Now, an Opportunity for the Future. Eur. Urol. 2020, 78, 820–821. [Google Scholar] [CrossRef]
- Doniec, R.J.; Piaseczna, N.J.; Szymczyk, K.A.; Jacennik, B.; Siecinski, S.; Mocny-Pachonska, K.; Duraj, K.; Cedro, T.; Tkacz, E.J.; Glinkowski, W.M. Experiences of the Telemedicine and eHealth Conferences in Poland—A Cross-National Overview of Progress in Telemedicine. Appl. Sci. 2022, 13, 587. [Google Scholar] [CrossRef]
- Melchiorre, M.G.; Papa, R.; Rijken, M.; van Ginneken, E.; Hujala, A.; Barbabella, F. eHealth in integrated care programs for people with multimorbidity in Europe: Insights from the ICARE4EU project. Health Policy 2018, 122, 53–63. [Google Scholar] [CrossRef]
- Leporatti, L.; Montefiori, M. Complex role of individual digital skills and eHealth policies in shaping health policy. Socio-Econ. Plan. Sci. 2024, 93, 101897. [Google Scholar] [CrossRef]
- Peleg, M.; Shahar, Y.; Quaglini, S.; Broens, T.; Budasu, R.; Fung, N.; Fux, A.; Garcia-Saez, G.; Goldstein, A.; Gonzalez-Ferrer, A.; et al. Assessment of a personalized and distributed patient guidance system. Int. J. Med. Inform. 2017, 101, 108–130. [Google Scholar] [CrossRef]
- Kononowicz, A.A.; Heid, J.; Donkers, J.; Hege, I.; Woodham, L.; Zary, N. Development and validation of strategies to test for interoperability of virtual patients. Stud. Health Technol. Inform. 2009, 150, 185–189. [Google Scholar]
- Krzesiński, P. Digital Health Technologies for Post-Discharge Care after Heart Failure Hospitalisation to Relieve Symptoms and Improve Clinical Outcomes. J. Clin. Med. 2023, 12, 2373. [Google Scholar] [CrossRef]
- Rödiger, H.; Busse, R.; Henschke, C. The introduction of maximum reimbursement prices for digital health applications in Germany in 2022: Current developments. Health Policy 2025, 155, 105284. [Google Scholar] [CrossRef]
- Schliess, F.; Affini Dicenzo, T.; Gaus, N.; Bourez, J.M.; Stegbauer, C.; Szecsenyi, J.; Jacobsen, M.; Müller-Wieland, D.; Kulzer, B.; Heinemann, L. The German Fast Track Toward Reimbursement of Digital Health Applications: Opportunities and Challenges for Manufacturers, Healthcare Providers, and People with Diabetes. J. Diabetes Sci. Technol. 2024, 18, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Vidal, P.; Rezanova, A. Teleconsultation cabins: A response to France’s healthcare access crisis? GeoJournal 2025, 90, 98. [Google Scholar] [CrossRef]
- Gullslett, M.K.; Ronchi, E.; Lundberg, L.; Larbi, D.; Lind, K.F.; Tayefi, M.; Ngo, P.D.; Sy, T.R.; Adib, K.; Hamilton, C. Telehealth development in the WHO European region: Results from a quantitative survey and insights from Norway. Int. J. Med. Inform. 2024, 191, 105558. [Google Scholar] [CrossRef] [PubMed]
- Asomugha, A.U.; Pakai, A. Trends and Shifts in Swedish Telemedicine Consultations During the Pre–COVID-19, COVID-19, and Post–COVID-19 Periods: Retrospective Observational Study. JMIR Form Res. 2025, 9, e60294. [Google Scholar] [CrossRef]
- Glinkowski W, K.M. Telemedicine and eHealth in Poland: A Review (Polish Telemedicine Society Perspective). Glob. Telemed. Ehealth Updates Knowl. Resour. 2013, 6, 381–384. [Google Scholar]
- Ledziński, Ł.; Grześk, G. Artificial Intelligence Technologies in Cardiology. J. Cardiovasc. Dev. Dis. 2023, 10, 202. [Google Scholar] [CrossRef]
- Goeldner, M.; Gehder, S. Digital Health Applications (DiGAs) on a Fast Track: Insights from a Data-Driven Analysis of Prescribable Digital Therapeutics in Germany from 2020 to Mid-2024. J. Med. Internet Res. 2024, 26, e59013. [Google Scholar] [CrossRef]
- Priisalu, J.; Ottis, R. Personal control of privacy and data: Estonian experience. Health Technol. 2017, 7, 441–451. [Google Scholar] [CrossRef]
- Kasyapa, M.S.B.; Vanmathi, C. Blockchain integration in healthcare: A comprehensive investigation of use cases, performance issues, and mitigation strategies. Front. Digit. Health 2024, 6, 1359858. [Google Scholar] [CrossRef]
- Soares, B.; Ferreira, A.; Veiga, P. The Benefits and Challenges of Blockchain Technology and eHealth Implementation in Estonia—A Literature Review. Appl. Med. Inform. 2023, 45, 118–131. [Google Scholar]
- Marelli, L.; Stevens, M.; Sharon, T.; Van Hoyweghen, I.; Boeckhout, M.; Colussi, I.; Degelsegger-Márquez, A.; El-Sayed, S.; Hoeyer, K.; van Kessel, R.; et al. The European health data space: Too big to succeed? Health Policy 2023, 135, 104861. [Google Scholar] [CrossRef] [PubMed]
- van Drumpt, S.; Chawla, K.; Barbereau, T.; Spagnuelo, D.; van de Burgwal, L. Secondary use under the European Health Data Space: Setting the scene and towards a research agenda on privacy-enhancing technologies. Front. Digit. Health 2025, 7, 1602101. [Google Scholar] [CrossRef] [PubMed]
- Semenzin, S.; Rozas, D.; Hassan, S. Blockchain-based application at a governmental level: Disruption or illusion? The case of Estonia. Policy Society 2022, 41, 386–401. [Google Scholar] [CrossRef]
- Baumgart, D.C.; Kvedar, J.C. Germany and Europe lead digital innovation and AI with collaborative health data use at continental level. npj Digit. Med. 2025, 8, 215. [Google Scholar] [CrossRef]
- Schmidt, L.; Pawlitzki, M.; Renard, B.Y.; Meuth, S.G.; Masanneck, L. The three-year evolution of Germany’s Digital Therapeutics reimbursement program and its path forward. npj Digit. Med. 2024, 7, 139. [Google Scholar] [CrossRef] [PubMed]
- Vardas, E.P.; Marketou, M.; Vardas, P.E. Medicine, healthcare and the AI act: Gaps, challenges and future implications. Eur Heart J. Digit. Health 2025, 6, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Molina-Nava, A.; Kapoor, Y.; Anerobi, C.; Maddukuri, H. Analyzing the Effect of Telemedicine on Domains of Quality Through Facilitators and Barriers to Adoption: Systematic Review. J. Med. Internet Res. 2023, 25, e43601. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).