Trueness of Implant Positioning Using Intraoral Scanning and Dental Photogrammetry for Full-Arch Implant-Supported Rehabilitations: An In Vitro Study
Abstract
1. Introduction
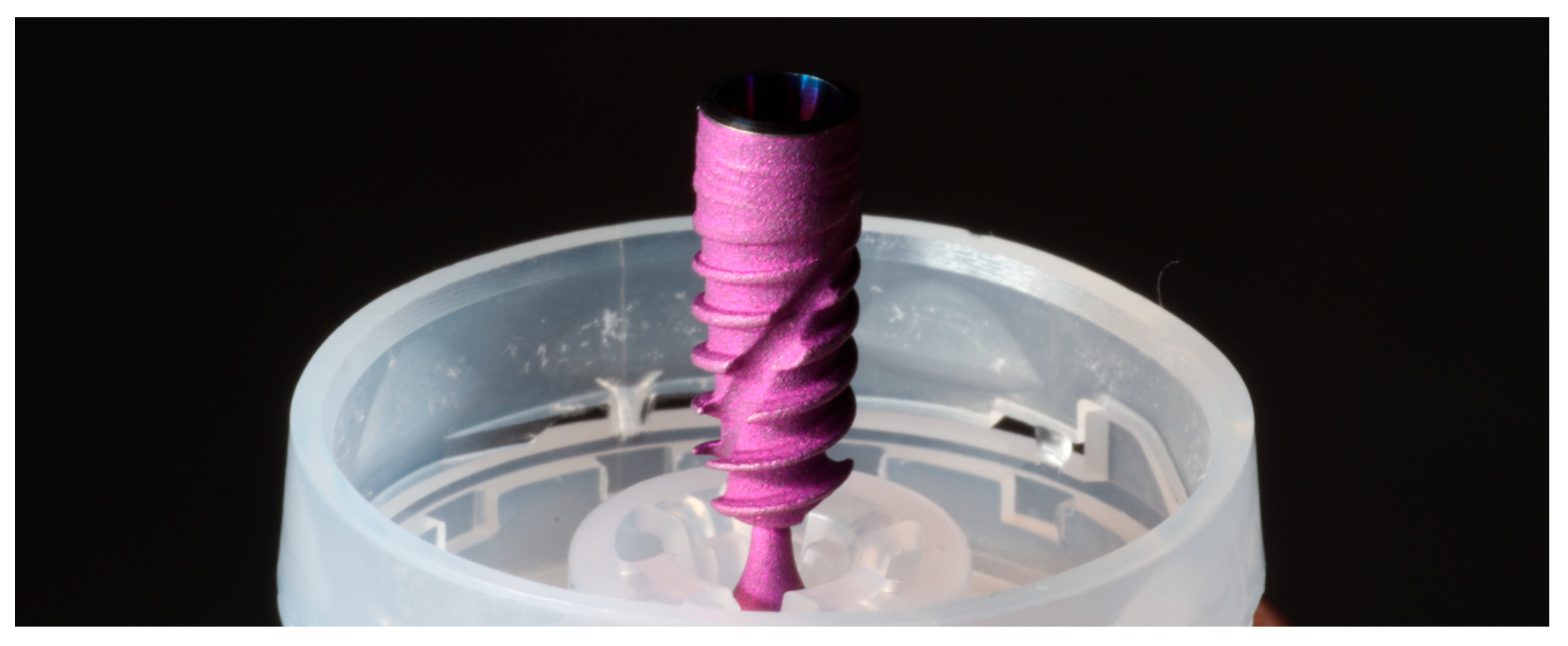
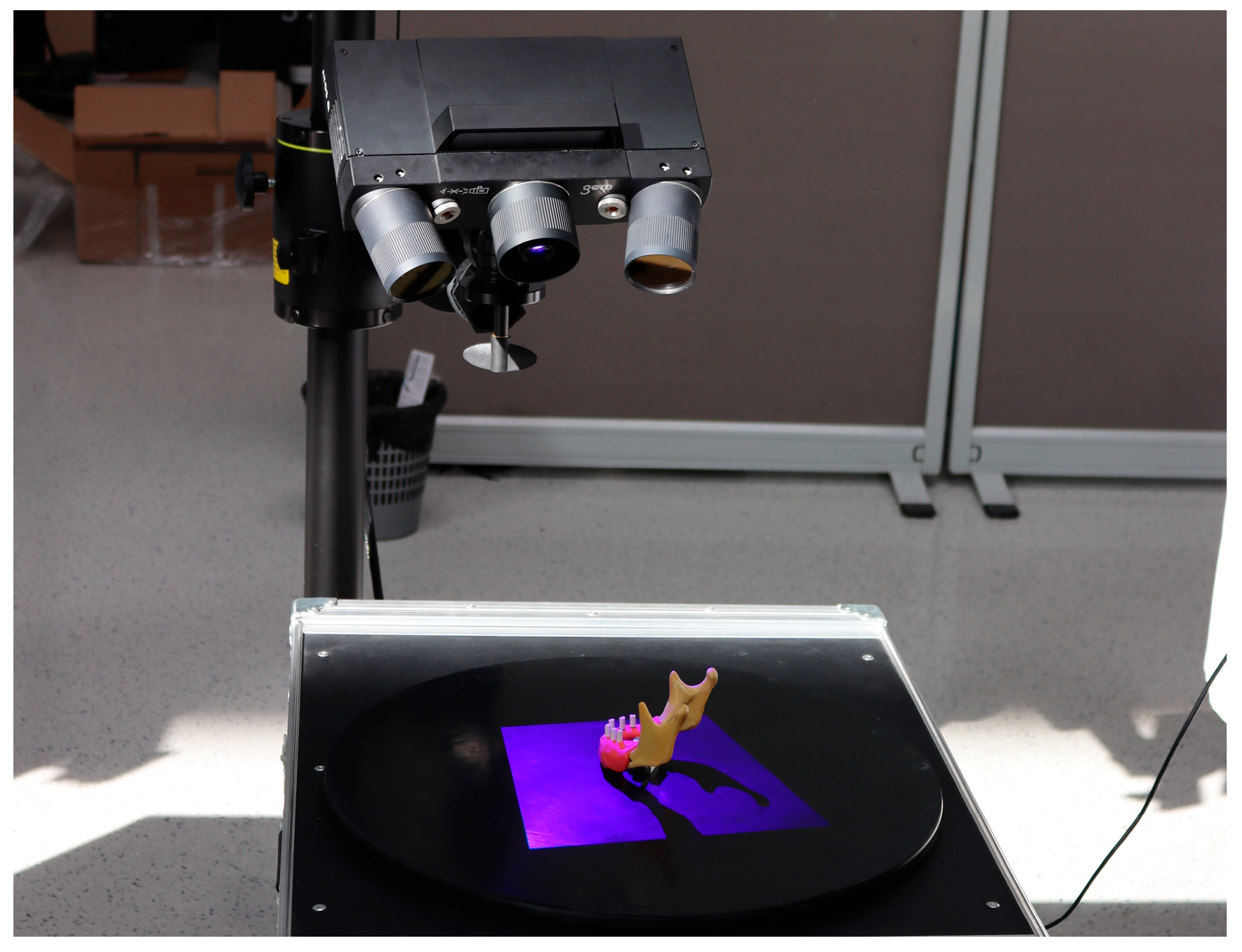
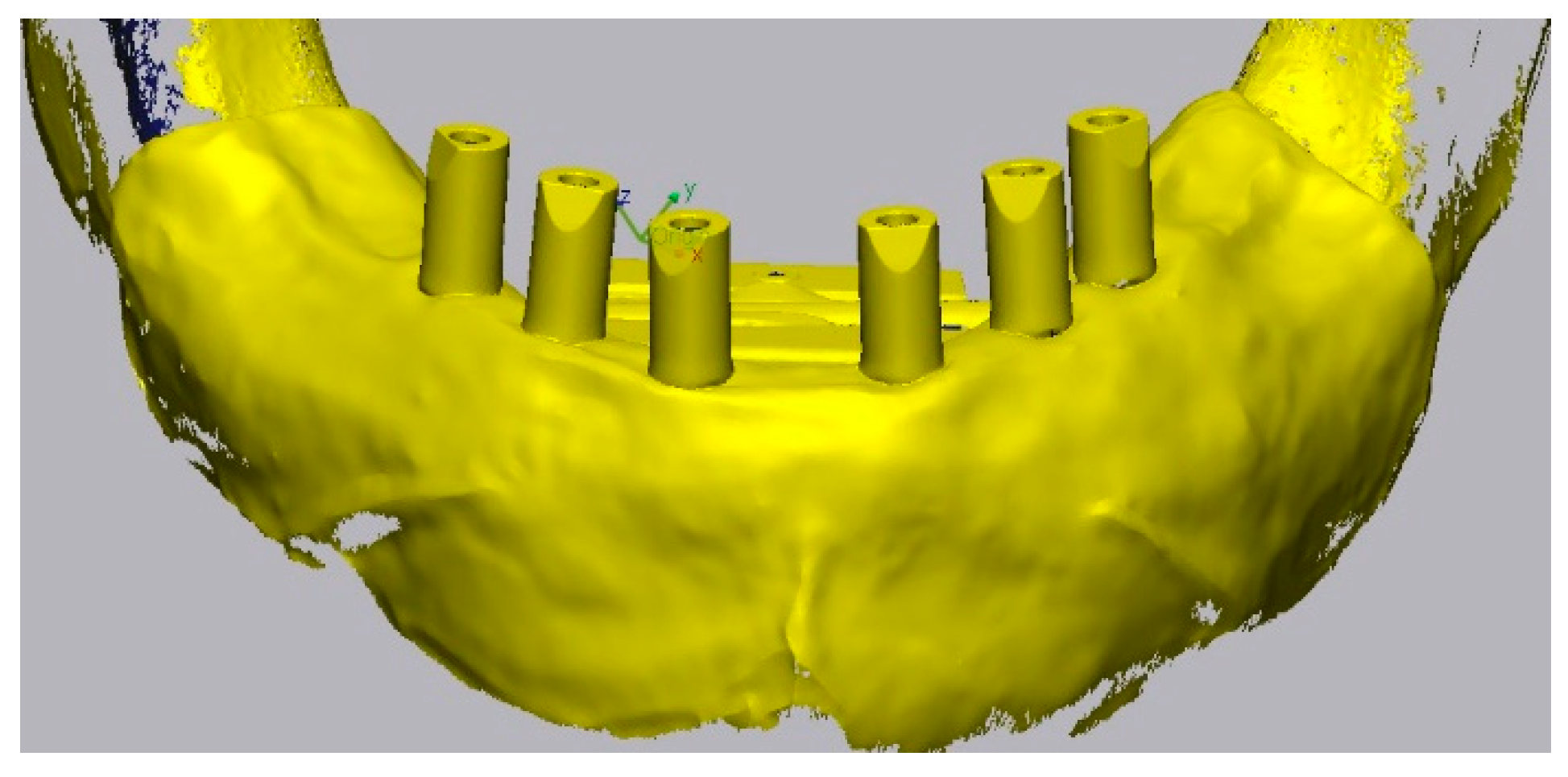
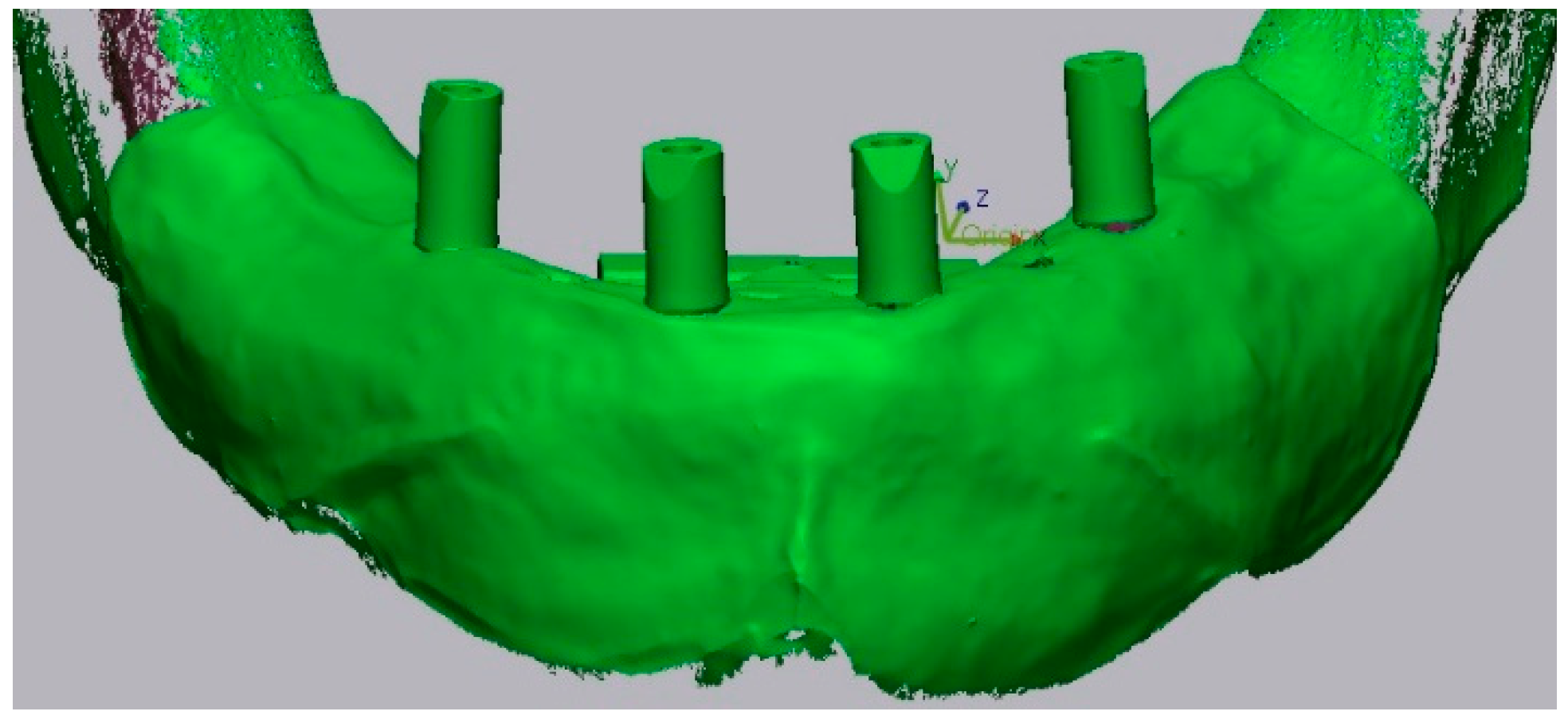
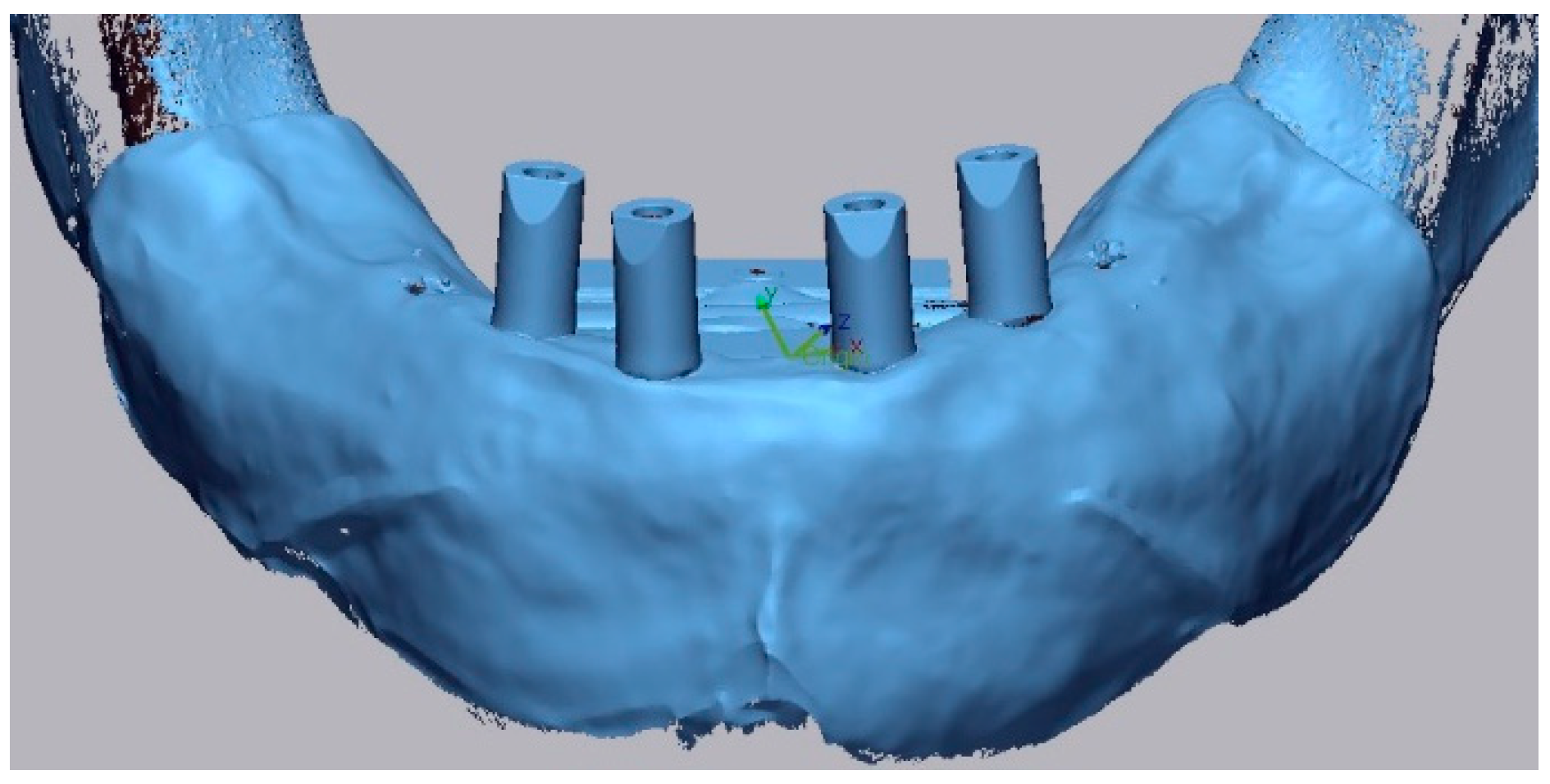
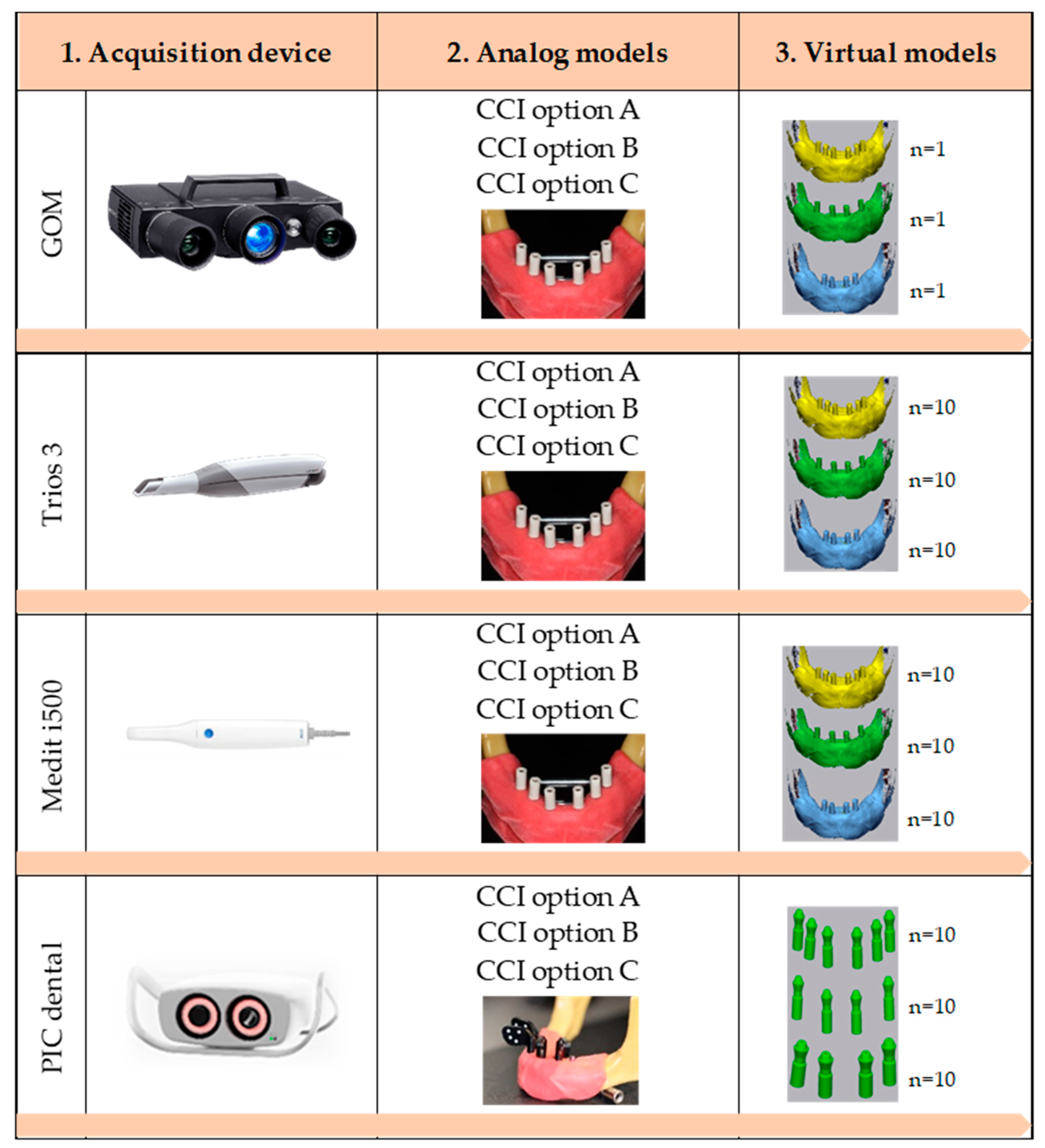
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amin, S.; Weber, H.P.; Finkelman, M.; El Rafie, K.; Kudara, Y.; Papaspyridakos, P. Digital vs. Conventional Full-Arch Implant Impressions: A Comparative Study. Clin. Oral Implants Res. 2017, 28, 1360–1367. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Liu, Y.; Huang, B.; Zhang, C.; Chen, Z.; Li, Z. Improved Scanning Accuracy with Newly Designed Scan Bodies: An in Vitro Study Comparing Digital versus Conventional Impression Techniques for Complete-arch Implant Rehabilitation. Clin. Oral Implants Res. 2020, 31, 625–633. [Google Scholar] [CrossRef] [PubMed]
- D’Ambrosio, F.; Giordano, F.; Sangiovanni, G.; Di Palo, M.P.; Amato, M. Conventional versus Digital Dental Impression Techniques: What Is the Future? An Umbrella Review. Prosthesis 2023, 5, 851–875. [Google Scholar] [CrossRef]
- Pozzi, A.; Agliardi, E.; Lio, F.; Nagy, K.; Nardi, A.; Arcuri, L. Accuracy of Intraoral Optical Scan versus Stereophotogrammetry for Complete-Arch Digital Implant Impression: An in Vitro Study. J. Prosthodont. Res. 2023, 68, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Jivănescu, A.; Bara, A.; Faur, A.-B.; Rotar, R.N. Is There a Significant Difference in Accuracy of Four Intraoral Scanners for Short-Span Fixed Dental Prosthesis? A Comparative In Vitro Study. Appl. Sci. 2021, 11, 8280. [Google Scholar] [CrossRef]
- Ma, B.; Yue, X.; Sun, Y.; Peng, L.; Geng, W. Accuracy of Photogrammetry, Intraoral Scanning, and Conventional Impression Techniques for Complete-Arch Implant Rehabilitation: An in Vitro Comparative Study. BMC Oral Health 2021, 21, 636. [Google Scholar] [CrossRef] [PubMed]
- Aswani, K.; Wankhade, S.; Khalikar, A.; Deogade, S. Accuracy of an Intraoral Digital Impression: A Review. J. Indian Prosthodont. Soc. 2020, 20, 27. [Google Scholar] [CrossRef] [PubMed]
- Imburgia, M.; Logozzo, S.; Hauschild, U.; Veronesi, G.; Mangano, C.; Mangano, F.G. Accuracy of Four Intraoral Scanners in Oral Implantology: A Comparative in Vitro Study. BMC Oral Health 2017, 17, 92. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Gandolfi, A.; Luongo, G.; Logozzo, S. Intraoral Scanners in Dentistry: A Review of the Current Literature. BMC Oral Health 2017, 17, 149. [Google Scholar] [CrossRef] [PubMed]
- Papaspyridakos, P.; Chen, C.-J.; Gallucci, G.O.; Doukoudakis, A.; Weber, H.-P.; Chronopoulos, V. Accuracy of Implant Impressions for Partially and Completely Edentulous Patients: A Systematic Review. Int. J. Oral Maxillofac. Implants 2014, 29, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T.; Lie, A. Accuracy of Implant-Supported Prostheses in the Edentulous Jaw: Analysis of Precision of Fit between Cast Gold-Alloy Frameworks and Master Casts by Means of a Three-Dimensional Photogrammetric Technique. Clin. Oral Implants Res. 1995, 6, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Jemt, T.; Hjalmarsson, L. In Vitro Measurements of Precision of Fit of Implant-Supported Frameworks. A Comparison between “Virtual” and “Physical” Assessments of Fit Using Two Different Techniques of Measurements. Clin. Implant Dent. Relat. Res. 2012, 14, e175–e182. [Google Scholar] [CrossRef] [PubMed]
- Michelinakis, G.; Apostolakis, D.; Kamposiora, P.; Papavasiliou, G.; Özcan, M. The Direct Digital Workflow in Fixed Implant Prosthodontics: A Narrative Review. BMC Oral Health 2021, 21, 37. [Google Scholar] [CrossRef] [PubMed]
- Sahin, S.; Cehreli, M.C. The Significance of Passive Framework Fit in Implant Prosthodontics: Current Status. Implant Dent. 2001, 10, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Oh, T.-J.; Misch, C.E.; Wang, H.-L. Occlusal Considerations in Implant Therapy: Clinical Guidelines with Biomechanical Rationale. Clin. Oral Implants Res. 2005, 16, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Knechtle, N.; Wiedemeier, D.; Mehl, A.; Ender, A. Accuracy of Digital Complete-Arch, Multi-Implant Scans Made in the Edentulous Jaw with Gingival Movement Simulation: An in Vitro Study. J. Prosthet. Dent. 2022, 128, 468–478. [Google Scholar] [CrossRef] [PubMed]
- Di Fiore, A.; Meneghello, R.; Graiff, L.; Savio, G.; Vigolo, P.; Monaco, C.; Stellini, E. Full Arch Digital Scanning Systems Performances for Implant-Supported Fixed Dental Prostheses: A Comparative Study of 8 Intraoral Scanners. J. Prosthodont. Res. 2019, 63, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Revell, G.; Simon, B.; Mennito, A.; Evans, Z.P.; Renne, W.; Ludlow, M.; Vág, J. Evaluation of Complete-Arch Implant Scanning with 5 Different Intraoral Scanners in Terms of Trueness and Operator Experience. J. Prosthet. Dent. 2022, 128, 632–638. [Google Scholar] [CrossRef] [PubMed]
- Rutkūnas, V.; Gečiauskaitė, A.; Jegelevičius, D.; Vaitiekūnas, M. Accuracy of Digital Implant Impressions with Intraoral Scanners. A Systematic Review. Eur. J. Oral Implantol. 2017, 10 (Suppl. 1), 101–120. [Google Scholar] [PubMed]
- Imburgia, M.; Kois, J.; Marino, E.; Lerner, H.; Mangano, F.G. Continuous Scan Strategy (CSS): A Novel Technique to Improve the Accuracy of Intraoral Digital Impressions. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Arcuri, L.; Pozzi, A.; Lio, F.; Rompen, E.; Zechner, W.; Nardi, A. Influence of Implant Scanbody Material, Position and Operator on the Accuracy of Digital Impression for Complete-Arch: A Randomized in Vitro Trial. J. Prosthodont. Res. 2020, 64, 128–136. [Google Scholar] [CrossRef] [PubMed]
- ISO 5725-1:2023; Accuracy (Trueness and Precision) of Measurement Methods and results—Part 1: General Principles and Definitions. ISO: Geneva, Switzerland, 2023.
- Sanda, M.; Miyoshi, K.; Baba, K. Trueness and Precision of Digital Implant Impressions by Intraoral Scanners: A Literature Review. Int. J. Implant Dent. 2021, 7, 97. [Google Scholar] [CrossRef] [PubMed]
- Sampaio-Fernandes, M.A.; Pinto, R.; Almeida, P.R.; Sampaio-Fernandes, M.M.; Marques, D.; Figueiral, M.H. Accuracy of Extraoral Digital Impressions with Multi-Unit Implants. Appl. Sci. 2023, 13, 8769. [Google Scholar] [CrossRef]
- Kihara, H.; Hatakeyama, W.; Komine, F.; Takafuji, K.; Takahashi, T.; Yokota, J.; Oriso, K.; Kondo, H. Accuracy and Practicality of Intraoral Scanner in Dentistry: A Literature Review. J. Prosthodont. Res. 2020, 64, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Polo, M.; Gómez-Polo, C.; Del Río, J.; Ortega, R. Stereophotogrammetric Impression Making for Polyoxymethylene, Milled Immediate Partial Fixed Dental Prostheses. J. Prosthet. Dent. 2018, 119, 506–510. [Google Scholar] [CrossRef] [PubMed]
- Hussein, M.O. Photogrammetry Technology in Implant Dentistry: A Systematic Review. J. Prosthet. Dent. 2023, 130, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Lin, X.; Yue, X.; Geng, W. Accuracy of 2 Direct Digital Scanning Techniques—Intraoral Scanning and Stereophotogrammetry—For Complete Arch Implant-Supported Fixed Prostheses: A Prospective Study. J. Prosthet. Dent. 2023, 130, 564–572. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, J.C.; Sampaio-Fernandes, M.A.; Oliveira, S.J.; Malheiro, R.; Sampaio-Fernandes, J.C.; Figueiral, M.H. Precision of Photogrammetry and Intraoral Scanning in Full-Arch Implant Rehabilitation: An In Vitro Comparative Study. Appl. Sci. 2025, 15, 1388. [Google Scholar] [CrossRef]
- Revilla-León, M.; Att, W.; Özcan, M.; Rubenstein, J. Comparison of Conventional, Photogrammetry, and Intraoral Scanning Accuracy of Complete-Arch Implant Impression Procedures Evaluated with a Coordinate Measuring Machine. J. Prosthet. Dent. 2021, 125, 470–478. [Google Scholar] [CrossRef]
- Caramês, J. A Comprehensive Classification to Full Arch Implant Rehabilitation. Rev. Port. Estomatol. Med. Dentária Cir. Maxilofac. 2019, 60, 175–188. [Google Scholar] [CrossRef]
- Amornvit, P.; Rokaya, D.; Peampring, C.; Sanohkan, S. Confocal 3D Optical Intraoral Scanners and Comparison of Image Capturing Accuracy. Comput. Mater. Contin. 2020, 66, 303–314. [Google Scholar] [CrossRef]
- Cakmak, G.; Marques, V.R.; Donmez, M.B.; Lu, W.-E.; Abou-Ayash, S.; Yilmaz, B. Comparison of Measured Deviations in Digital Implant Scans Depending on Software and Operator. J. Dent. 2022, 122, 104154. [Google Scholar] [CrossRef] [PubMed]
- Bud, E.S.; Bocanet, V.I.; Muntean, M.H.; Vlasa, A.; Păcurar, M.; Zetu, I.N.; Soporan, B.I.; Bud, A. Extra-Oral Three-Dimensional (3D) Scanning Evaluation of Three Different Impression Materials—An In Vitro Study. Polymers 2022, 14, 3678. [Google Scholar] [CrossRef] [PubMed]
- Sampaio-Fernandes, M.A.F.; Pinto, R.; Sampaio-Fernandes, M.M.; Carlos, J.; Marques, D.; Figueiral, M.H. Accuracy of Silicone Impressions and Stone Models Using Two Laboratory Scanners: A 3D Evaluation. Int. J. Prosthodont. 2024, 37, e10–e24. [Google Scholar] [CrossRef] [PubMed]
- Wulfman, C.; Naveau, A.; Rignon-Bret, C. Digital Scanning for Complete-Arch Implant-Supported Restorations: A Systematic Review. J. Prosthet. Dent. 2020, 124, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Kanjanasavitree, P.; Thammajaruk, P.; Guazzato, M. Comparison of Different Artificial Landmarks and Scanning Patterns on the Complete-Arch Implant Intraoral Digital Scans. J. Dent. 2022, 125, 104266. [Google Scholar] [CrossRef] [PubMed]
- Rivara, F.; Lumetti, S.; Calciolari, E.; Toffoli, A.; Forlani, G.; Manfredi, E. Photogrammetric Method to Measure the Discrepancy between Clinical and Software-Designed Positions of Implants. J. Prosthet. Dent. 2016, 115, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Sicilia, E.; Lagreca, G.; Papaspyridakos, P.; Finkelman, M.; Cobo, J.; Att, W.; Revilla-León, M. Effect of Supramucosal Height of a Scan Body and Implant Angulation on the Accuracy of Intraoral Scanning: An In Vitro Study. J. Prosthet. Dent. 2024, 131, 1126–1134. [Google Scholar] [CrossRef] [PubMed]
- Lyu, M.; Di, P.; Lin, Y.; Jiang, X. Accuracy of Impressions for Multiple Implants: A Comparative Study of Digital and Conventional Techniques. J. Prosthet. Dent. 2022, 128, 1017–1023. [Google Scholar] [CrossRef] [PubMed]
- Ender, A.; Mehl, A. Accuracy of Complete-Arch Dental Impressions: A New Method of Measuring Trueness and Precision. J. Prosthet. Dent. 2013, 109, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Flügge, T.V.; Schlager, S.; Nelson, K.; Nahles, S.; Metzger, M.C. Precision of Intraoral Digital Dental Impressions with ITero and Extraoral Digitization with the ITero and a Model Scanner. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Tohme, H.; Lawand, G.; Chmielewska, M.; Makhzoume, J. Comparison between Stereophotogrammetric, Digital, and Conventional Impression Techniques in Implant-Supported Fixed Complete Arch Prostheses: An in Vitro Study. J. Prosthet. Dent. 2023, 129, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Taylor, T.D. Prosthodontic Problems and Limitations Associated with Osseointegration. J. Prosthet. Dent. 1998, 79, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Kallus, T.; Bessing, C. Loose Gold Screws Frequently Occur in Full-Arch Fixed Prostheses Supported by Osseointegrated Implants after 5 Years. Int. J. Oral Maxillofac. Implants 1994, 9, 169–178. [Google Scholar] [PubMed]
- Papaspyridakos, P.; Hirayama, H.; Chen, C.; Ho, C.; Chronopoulos, V.; Weber, H. Full-arch Implant Fixed Prostheses: A Comparative Study on the Effect of Connection Type and Impression Technique on Accuracy of Fit. Clin. Oral Implants Res. 2016, 27, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Chochlidakis, K.; Papaspyridakos, P.; Tsigarida, A.; Romeo, D.; Chen, Y.; Natto, Z.; Ercoli, C. Digital Versus Conventional Full-Arch Implant Impressions: A Prospective Study on 16 Edentulous Maxillae. J. Prosthodont. 2020, 29, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, R.M.; Yilmaz, B. Intraoral Scan Bodies in Implant Dentistry: A Systematic Review. J. Prosthet. Dent. 2018, 120, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Yilmaz, H.; Treviño, A.; Kökat, A.M.; Yilmaz, B. The Effect of Scanner Type and Scan Body Position on the Accuracy of Complete-arch Digital Implant Scans. Clin. Implant Dent. Relat. Res. 2020, 22, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Bohner, L.; Gamba, D.D.; Hanisch, M.; Marcio, B.S.; Tortamano Neto, P.; Laganá, D.C.; Sesma, N. Accuracy of Digital Technologies for the Scanning of Facial, Skeletal, and Intraoral Tissues: A Systematic Review. J. Prosthet. Dent. 2019, 121, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Yilmaz, H.; Treviño Santos, A.; Kökat, A.M.; Yilmaz, B. Effect of Scanner Type and Scan Body Location on the Accuracy of Mandibular Complete-Arch Digital Implant Scans: An In Vitro Study. J. Prosthodont. 2022, 31, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Mizumoto, R.M.; Alp, G.; Özcan, M.; Yilmaz, B. The Effect of Scanning the Palate and Scan Body Position on the Accuracy of Complete-arch Implant Scans. Clin. Implant Dent. Relat. Res. 2019, 21, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.-H.; Park, J.-M.; Kim, M.; Heo, S.-J.; Myung, J.-Y. Comparison of Digital Intraoral Scanner Reproducibility and Image Trueness Considering Repetitive Experience. J. Prosthet. Dent. 2018, 119, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Zotti, F.; Rosolin, L.; Bersani, M.; Poscolere, A.; Pappalardo, D.; Zerman, N. Digital Dental Models: Is Photogrammetry an Alternative to Dental Extraoral and Intraoral Scanners? Dent. J. 2022, 10, 24. [Google Scholar] [CrossRef] [PubMed]
- Pascadopoli, M.; Zampetti, P.; Nardi, M.G.; Pellegrini, M.; Scribante, A. Smartphone Applications in Dentistry: A Scoping Review. Dent. J. 2023, 11, 243. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yang, J.Y.; Liu, H.K.; Yu, P.; Jiang, X.J.; Liu, R.J. Co-Mask R-CNN: Collaborative Learning-Based Method for Tooth Instance Segmentation. J. Clin. Pediatr. Dent. 2024, 48, 161. [Google Scholar] [CrossRef] [PubMed]
| Scanner | Number and Position of Implants | Group |
|---|---|---|
| 3Shape Trios 3 IOS | 6 (CCI Option A) | TA |
| 4 (CCI Option B) | TB | |
| 4 (CCI Option C) | TC | |
| Medit i500 | 6 (CCI Option A) | MA |
| 4 (CCI Option B) | MB | |
| 4 (CCI Option C) | MC | |
| PIC Dental Photogrammetry | 6 (CCI Option A) | PA |
| 4 (CCI Option B) | PB | |
| 4 (CCI Option C) | PC |
| Scanner | Number and Position of Implants | Group | RMS (µm) Median | IQR | N | Intra-Group p-Values | |
|---|---|---|---|---|---|---|---|
| IO 3Shape Trios 3 | 6 (CCI A) | TA | 29.55 | 27.85; 29.73 | 10 | a | <0.001 |
| 4 (CCI B) | TB | 58.80 | 45.78; 63.38 | 10 | a | ||
| 4 (CCI C) | TC | 18.75 | 17.95; 20.75 | 10 | |||
| IO Medit i500 | 6 (CCI A) | MA | 33.95 | 32.10; 37.20 | 10 | <0.001 | |
| 4 (CCI B) | MB | 24.45 | 20.48; 25.70 | 10 | b | ||
| 4 (CCI C) | MC | 13.65 | 11.90; 15.60 | 10 | b | ||
| Photogrammetry PIC Dental | 6 (CCI A) | PA | 53.55 | 53.03; 53.95 | 10 | c | <0.001 |
| 4 (CCI B) | PB | 49.45 | 45.38; 51.38 | 10 | c,d | ||
| 4 (CCI C) | PC | 43.70 | 43.38; 45.88 | 10 | d | ||
| Number and Position of Implants | RMS (µm) Median | IQR | N | p | |
|---|---|---|---|---|---|
| 6 (CCI A) | 34.20 | 29.70; 53.15 | 30 | a | <0.001 |
| 4 (CCI B) | 45.75 | 24.58; 57.05 | 30 | a | |
| 4 (CCI C) | 19.00 | 15.58; 43.40 | 30 | ||
| Device | RMS (µm) Median | IQR | N | p |
|---|---|---|---|---|
| IO 3Shape Trios 3 | 29.20 | 20.13; 51.50 | 30 | <0.001 |
| IO Medit i500 | 24.45 | 14.45; 32.63 | 30 | |
| Photogrammetry PIC Dental | 49.45 | 44.13; 53.30 | 30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faria, J.C.; Sampaio-Fernandes, M.A.; Oliveira, S.J.; Malheiro, R.; Sampaio-Fernandes, J.C.; Figueiral, M.H. Trueness of Implant Positioning Using Intraoral Scanning and Dental Photogrammetry for Full-Arch Implant-Supported Rehabilitations: An In Vitro Study. Appl. Sci. 2025, 15, 8016. https://doi.org/10.3390/app15148016
Faria JC, Sampaio-Fernandes MA, Oliveira SJ, Malheiro R, Sampaio-Fernandes JC, Figueiral MH. Trueness of Implant Positioning Using Intraoral Scanning and Dental Photogrammetry for Full-Arch Implant-Supported Rehabilitations: An In Vitro Study. Applied Sciences. 2025; 15(14):8016. https://doi.org/10.3390/app15148016
Chicago/Turabian StyleFaria, João Carlos, Manuel António Sampaio-Fernandes, Susana João Oliveira, Rodrigo Malheiro, João Carlos Sampaio-Fernandes, and Maria Helena Figueiral. 2025. "Trueness of Implant Positioning Using Intraoral Scanning and Dental Photogrammetry for Full-Arch Implant-Supported Rehabilitations: An In Vitro Study" Applied Sciences 15, no. 14: 8016. https://doi.org/10.3390/app15148016
APA StyleFaria, J. C., Sampaio-Fernandes, M. A., Oliveira, S. J., Malheiro, R., Sampaio-Fernandes, J. C., & Figueiral, M. H. (2025). Trueness of Implant Positioning Using Intraoral Scanning and Dental Photogrammetry for Full-Arch Implant-Supported Rehabilitations: An In Vitro Study. Applied Sciences, 15(14), 8016. https://doi.org/10.3390/app15148016






