The Impact of Electromyostimulation on Strength, Recovery, and Performance in Soccer Athletes: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
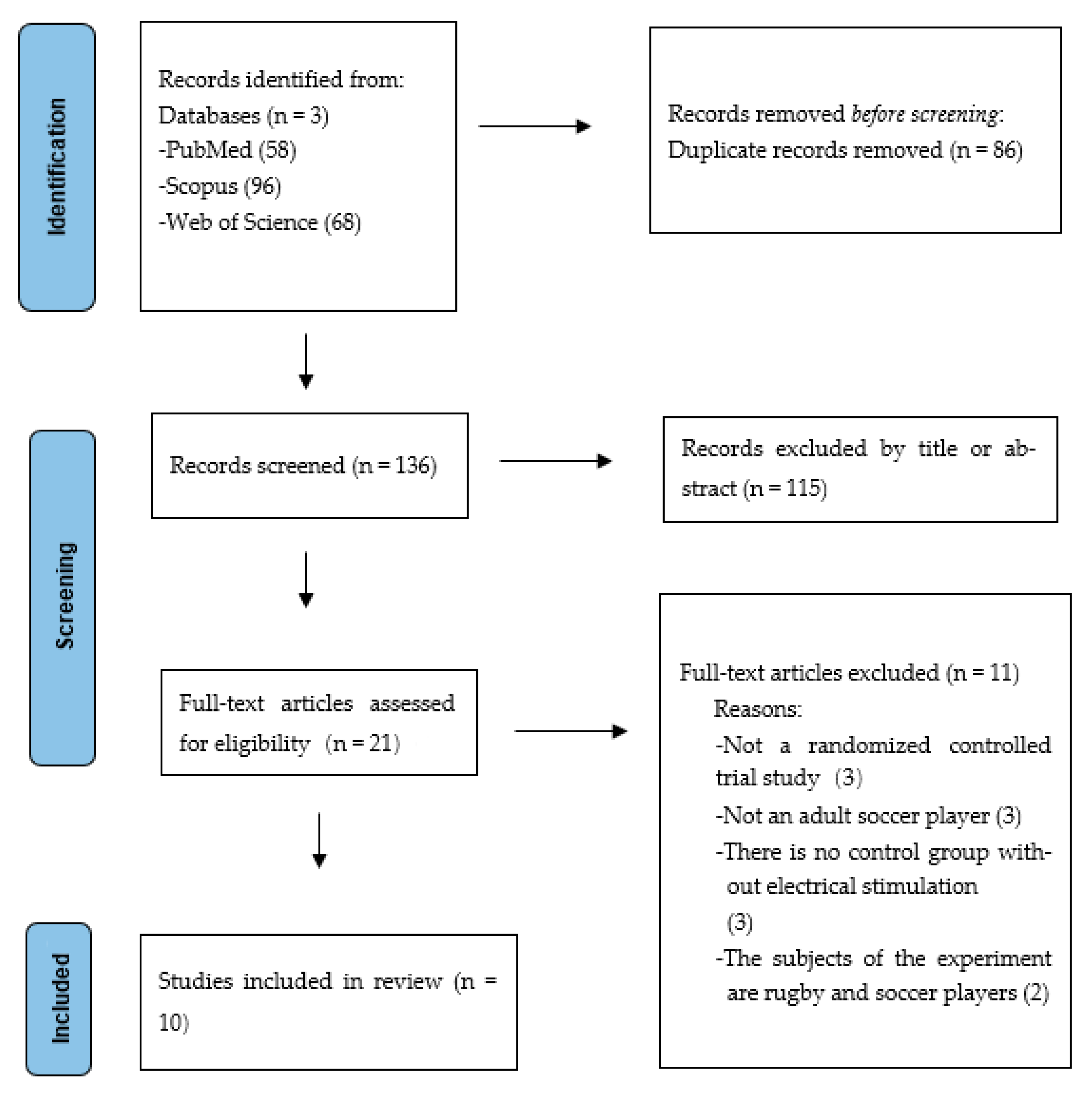
2.1. The Literature Search and Selection of Studies
2.2. Data Extraction
2.3. Quality Review
2.4. Data Analysis
3. Results
3.1. Included Studies and Study Characteristics
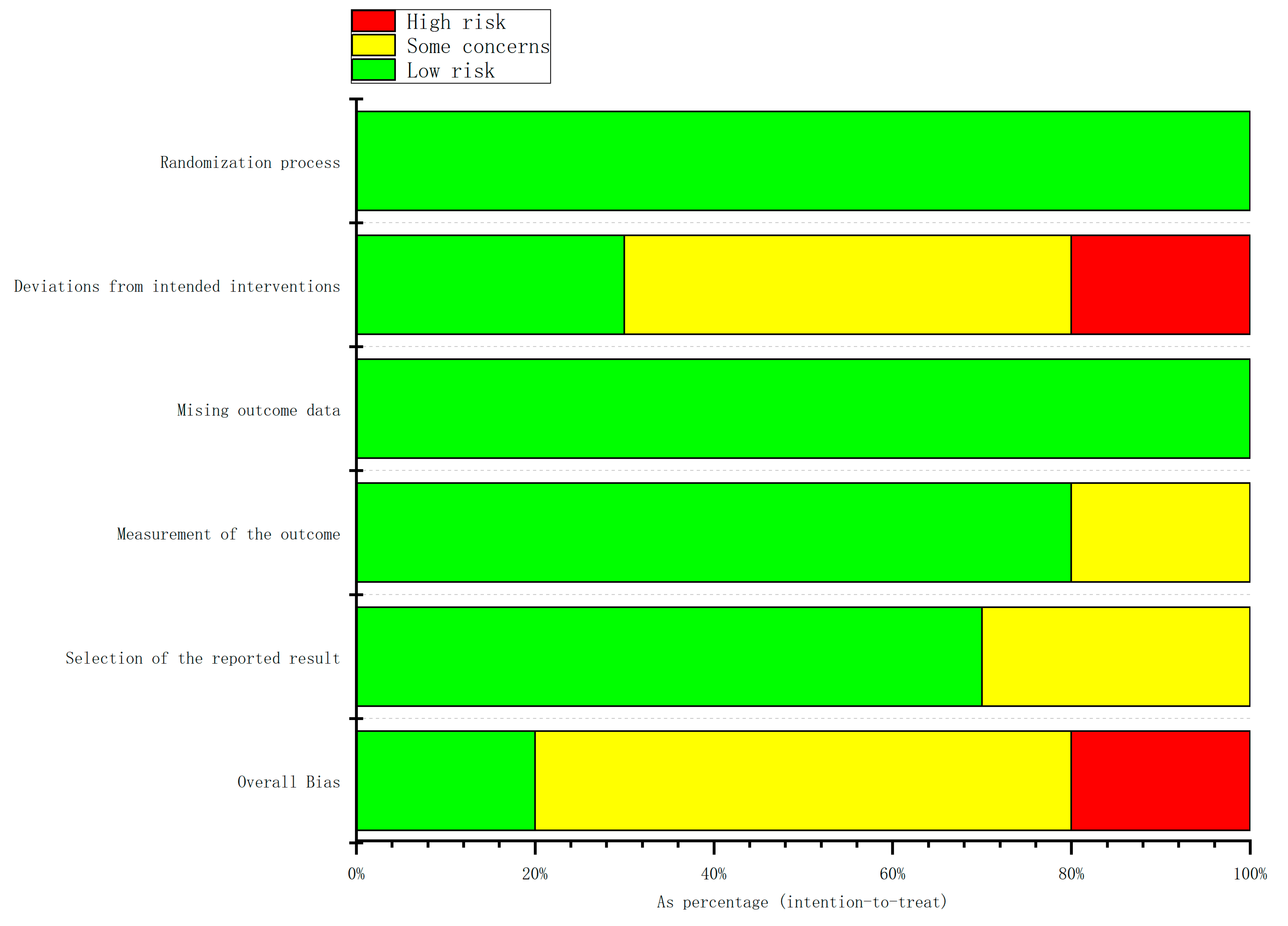
3.2. Risk of Bias
4. Discussion
4.1. The Effects of EMS on Athletic Performance
4.2. The Effects of EMS on Sports Injury Recovery
4.3. Risk Factors and Adverse Reactions Associated with EMS Application
4.4. Methodological Quality
5. Strengths of Our Study
6. Limitations and Future Directions
7. Safety Considerations
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Di Salvo, V.; Baron, R.; González-Haro, C.; Gormasz, C.; Pigozzi, F.; Bachl, N. Sprinting Analysis of Elite Soccer Players during European Champions League and UEFA Cup Matches. J. Sports Sci. 2010, 28, 1489–1494. [Google Scholar] [CrossRef]
- Wang, Y.; Zhou, Z.; Gao, Z.; Gu, Y. Comparative Effectiveness of Multi-Component, Exercise-Based Interventions for Preventing Soccer-Related Musculoskeletal Injuries: A Systematic Review and Meta-Analysis. Healthcare 2025, 13, 765. [Google Scholar] [CrossRef] [PubMed]
- Van Beijsterveldt, A.M.C.; Stubbe, J.H.; Schmikli, S.L.; Van De Port, I.G.L.; Backx, F.J.G. Differences in Injury Risk and Characteristics between Dutch Amateur and Professional Soccer Players. J. Sci. Med. Sport 2015, 18, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Fok, J.R.; Van Mechelen, W. Electrical Stimulation and Muscle Strength Gains in Healthy Adults: A Systematic Review. J. Strength Cond. Res. 2023, 37, 938–950. [Google Scholar] [CrossRef]
- Hultman, E.; Sjöholm, H.; Jäderholm-Ek, I.; Krynicki, J. Evaluation of Methods for Electrical Stimulation of Human Skeletal Muscle in Situ. Pflug. Arch. 1983, 398, 139–141. [Google Scholar] [CrossRef]
- Balke, M.; Teschler, M.; Schäfer, H.; Pape, P.; Mooren, F.C.; Schmitz, B. Therapeutic Potential of Electromyostimulation (EMS) in Critically Ill Patients—A Systematic Review. Front. Physiol. 2022, 13, 865437. [Google Scholar] [CrossRef]
- Barberi, L.; Scicchitano, B.M.; Musarò, A. Molecular and Cellular Mechanisms of Muscle Aging and Sarcopenia and Effects of Electrical Stimulation in Seniors. Eur. J. Transl. Myol. 2015, 25, 231. [Google Scholar] [CrossRef]
- Reischl, S.; Ziebart, C.; MacDermid, J.C.; Grewal, R.; Schabrun, S.M.; Trejos, A.L. Application of Neuromuscular Electrical Stimulation during Immobilization of Extremities for Musculoskeletal Conditions: A Scoping Review. J. Bodyw. Mov. Ther. 2024, 40, 1555–1560. [Google Scholar] [CrossRef]
- Cattagni, T.; Lepers, R.; Maffiuletti, N.A. Effects of Neuromuscular Electrical Stimulation on Contralateral Quadriceps Function. J. Electromyogr. Kinesiol. 2018, 38, 111–118. [Google Scholar] [CrossRef]
- Filipovic, A.; Kleinöder, H.; Dörmann, U.; Mester, J. Electromyostimulation—A Systematic Review of the Effects of Different Electromyostimulation Methods on Selected Strength Parameters in Trained and Elite Athletes. J. Strength Cond. Res. 2012, 26, 2600–2614. [Google Scholar] [CrossRef]
- Altarriba-Bartes, A.; Peña, J.; Vicens-Bordas, J.; Milà-Villaroel, R.; Calleja-González, J. Post-Competition Recovery Strategies in Elite Male Soccer Players. Effects on Performance: A Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0240135. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Minozzi, S.; Cinquini, M.; Gianola, S.; Gonzalez-Lorenzo, M.; Banzi, R. The Revised Cochrane Risk of Bias Tool for Randomized Trials (RoB 2) Showed Low Interrater Reliability and Challenges in Its Application. J. Clin. Epidemiol. 2020, 126, 37–44. [Google Scholar] [CrossRef]
- Billot, M.; Martin, A.; Paizis, C.; Cometti, C.; Babault, N. Effects of an Electrostimulation Training Program on Strength, Jumping, and Kicking Capacities in Soccer Players. J. Strength Cond. Res. 2010, 24, 1407–1413. [Google Scholar] [CrossRef]
- Bieuzen, F.; Pournot, H.; Roulland, R.; Hausswirth, C. Recovery After High-Intensity Intermittent Exercise in Elite Soccer Players Using VEINOPLUS Sport Technology for Blood-Flow Stimulation. J. Athl. Train. 2012, 47, 498–506. [Google Scholar] [CrossRef]
- Taradaj, J.; Halski, T.; Kucharzewski, M.; Walewicz, K.; Smykla, A.; Ozon, M.; Slupska, L.; Dymarek, R.; Ptaszkowski, K.; Rajfur, J.; et al. The Effect of NeuroMuscular Electrical Stimulation on Quadriceps Strength and Knee Function in Professional Soccer Players: Return to Sport after ACL Reconstruction. BioMed Res. Int. 2013, 2013, 802534. [Google Scholar] [CrossRef] [PubMed]
- Filipovic, A.; Grau, M.; Kleinöder, H.; Zimmer, P.; Hollmann, W.; Bloch, W. Effects of a Whole-Body Electrostimulation Program on Strength, Sprinting, Jumping, and Kicking Capacity in Elite Soccer Players. J. Sports Sci. Med. 2016, 15, 639–648. [Google Scholar] [PubMed]
- Barassi, G.; Bellomo, R.G.; Porreca, A.; Giannuzzo, G.; Giannandrea, N.; Pezzi, L.; Crudeli, M.; Visciano, C.; Saggini, R. The Use of Adaptive Neuro-Stimulation for Rebalancing Posture and Muscular Tone in a Soccer Team. J. Sports Med. Phys. Fit. 2019, 59, 1676–1683. [Google Scholar] [CrossRef] [PubMed]
- Filipovic, A.; DeMarees, M.; Grau, M.; Hollinger, A.; Seeger, B.; Schiffer, T.; Bloch, W.; Gehlert, S. Superimposed Whole-Body Electrostimulation Augments Strength Adaptations and Type II Myofiber Growth in Soccer Players During a Competitive Season. Front. Physiol. 2019, 10, 1187. [Google Scholar] [CrossRef]
- Kale, M.; Gurol, B. Effects of Electromyostimulation Training on Jumping and Muscle Strength in Football Players. PES 2019, 23, 242–248. [Google Scholar] [CrossRef]
- Hasan, S.; Kandasamy, G.; Alyahya, D.; Alonazi, A.; Jamal, A.; Iqbal, A.; Unnikrishnan, R.; Muthusamy, H. Effect of Plyometric Training and Neuromuscular Electrical Stimulation Assisted Strength Training on Muscular, Sprint, and Functional Performances in Collegiate Male Football Players. PeerJ 2022, 10, e13588. [Google Scholar] [CrossRef]
- Abdelmohsen Labib, H.S.; Abd Elsabour Sabah, H.M. Assessment of the Effects of Neuromuscular Electrical Stimulation after Anterior Cruciate Ligament Reconstruction on Quadriceps Muscle. J. Bodyw. Mov. Ther. 2024, 38, 274–280. [Google Scholar] [CrossRef]
- Fernández-Elías, V.; Naranjo-Delgado, S.; Sillero-Quintana, M.; Burgos-Postigo, S.; Fernández-Luna, Á. Effects of Adding WB-EMS to the Warm-Up on Football Players Power Performance Tests: A Crossover Study. Dtsch. Z. Sportmed. 2024, 75, 64–71. [Google Scholar] [CrossRef]
- Enoka, R.M.; Amiridis, I.G.; Duchateau, J. Electrical Stimulation of Muscle: Electrophysiology and Rehabilitation. Physiology 2020, 35, 40–56. [Google Scholar] [CrossRef] [PubMed]
- Filipovic, A.; Kleinöder, H.; Dörmann, U.; Mester, J. Electromyostimulation—A Systematic Review of the Influence of Training Regimens and Stimulation Parameters on Effectiveness in Electromyostimulation Training of Selected Strength Parameters. J. Strength Cond. Res. 2011, 25, 3218–3238. [Google Scholar] [CrossRef] [PubMed]
- Pano-Rodriguez, A.; Beltran-Garrido, J.V.; Hernández-González, V.; Reverter-Masia, J. Effects of Whole-Body ELECTROMYOSTIMULATION on Health and Performance: A Systematic Review. BMC Complement. Altern. Med. 2019, 19, 87. [Google Scholar] [CrossRef]
- Kemmler, W.; Fröhlich, M.; Eifler, C. Whole-Body Electromyostimulation: Effects, Limitations, Perspectives of an Innovative Training Method; Springer: Cham, Switzerland, 2024; ISBN 978-3-031-56709-4. [Google Scholar]
- Li, Z.; Jin, L.; Chen, Z.; Shang, Z.; Geng, Y.; Tian, S.; Dong, J. Effects of Neuromuscular Electrical Stimulation on Quadriceps Femoris Muscle Strength and Knee Joint Function in Patients After ACL Surgery: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Orthop. J. Sports Med. 2025, 13, 23259671241275071. [Google Scholar] [CrossRef]
- Porcari, J.P.; Mclean, K.P.; Foster, C.; Kernozek, T.; Crenshaw, B.; Swenson, C. Effects of Electrical Muscle Stimulation on Body Composition, Muscle Strength, and Physical Appearance. J. Strength Cond. Res. 2002, 16, 165–172. [Google Scholar]
- Konrad, K.L.; Baeyens, J.-P.; Birkenmaier, C.; Ranker, A.H.; Widmann, J.; Leukert, J.; Wenisch, L.; Kraft, E.; Jansson, V.; Wegener, B. The Effects of Whole-Body Electromyostimulation (WB-EMS) in Comparison to a Multimodal Treatment Concept in Patients with Non-Specific Chronic Back Pain—A Prospective Clinical Intervention Study. PLoS ONE 2020, 15, e0236780. [Google Scholar] [CrossRef]
- Bloeckl, J.; Raps, S.; Weineck, M.; Kob, R.; Bertsch, T.; Kemmler, W.; Schoene, D. Feasibility and Safety of Whole-Body Electromyostimulation in Frail Older People—A Pilot Trial. Front. Physiol. 2022, 13, 856681. [Google Scholar] [CrossRef]
- Von Deneen, K.M.; Alemayehu, D.G.; Khosla, A. Acute Compartment Syndrome and Rhabdomyolysis Caused by a Single Electrical Muscle Stimulation in a 46-Year-Old Female Professional Athlete With Fibromyalgia, Chronic Fatigue Syndrome, and Myofascial Disorder: A Case Report. Clin. J. Sport Med. 2024, 34, 506–508. [Google Scholar] [CrossRef]
- Fakhre, E.; Means, K.R.; Kessler, M.W.; Desale, S.; Paryavi, E.; Lincoln, A.E. The Epidemiology of Hand-to-Elbow Injuries in United States Collegiate Sports Over 10 Academic Years. Athl. Train. Sports Health Care 2020, 12, 159–166. [Google Scholar] [CrossRef]
- Volpi, P.; Bisciotti, G.N.; Chamari, K.; Cena, E.; Carimati, G.; Bragazzi, N.L. Risk Factors of Anterior Cruciate Ligament Injury in Football Players: A Systematic Review of the Literature. Muscle Ligaments Tendons J. 2019, 6, 480. [Google Scholar] [CrossRef]
- Nussbaum, E.L.; Houghton, P.; Anthony, J.; Rennie, S.; Shay, B.L.; Hoens, A.M. Neuromuscular Electrical Stimulation for Treatment of Muscle Impairment: Critical Review and Recommendations for Clinical Practice. Physiother. Can. 2017, 69, 1–76. [Google Scholar] [CrossRef] [PubMed]
- Daneshjoo, A.; Hosseini, E.; Heshmati, S.; Sahebozamani, M.; Behm, D.G. Effects of Slow Dynamic, Fast Dynamic, and Static Stretching on Recovery of Performance, Range of Motion, Balance, and Joint Position Sense in Healthy Adults. BMC Sports Sci. Med. Rehabil. 2024, 16, 167. [Google Scholar] [CrossRef] [PubMed]
- Yan, R.; Lin, G.; Peng, W.; Chen, Y.; Sun, P.; Sun, J.; Li, D. Time-Dependent Effects of Acute Stretching on Power, Balance, and Flexibility in Contemporary Dancers: A Randomized Crossover Trial. Sci. Rep. 2025, 15, 15489. [Google Scholar] [CrossRef] [PubMed]
- Mizumura, K.; Taguchi, T. Delayed Onset Muscle Soreness: Involvement of Neurotrophic Factors. J. Physiol. Sci. 2016, 66, 43–52. [Google Scholar] [CrossRef]
- Ackermann, P.W.; Juthberg, R.; Flodin, J. Unlocking the Potential of Neuromuscular Electrical Stimulation: Achieving Physical Activity Benefits for All Abilities. Front. Sports Act. Living 2024, 6, 1507402. [Google Scholar] [CrossRef]
- Kästner, A.; Braun, M.; Meyer, T. Two Cases of Rhabdomyolysis After Training with Electromyostimulation by 2 Young Male Professional Soccer Players. Clin. J. Sport Med. 2015, 25, e71–e73. [Google Scholar] [CrossRef]
- Almalty, A.R.; Hamed, S.H.; Jebril, M.Y.; Abdelnour, H.M. The Effect of Electrical Stimulation on Skin Vulnerability to Irritants. Skin Res. Technol. 2024, 30, e13591. [Google Scholar] [CrossRef]
- Kemmler, W.; Fröhlich, M.; Ludwig, O.; Eifler, C.; Von Stengel, S.; Willert, S.; Teschler, M.; Weissenfels, A.; Kleinöder, H.; Micke, F.; et al. Position Statement and Updated International Guideline for Safe and Effective Whole-Body Electromyostimulation Training-the Need for Common Sense in WB-EMS Application. Front. Physiol. 2023, 14, 1174103. [Google Scholar] [CrossRef]
- Qin, Y.; Chen, H.; Liu, X.; Wu, J.; Zhang, Y. Effects of Whole-Body Electromyostimulation Training on Upper Limb Muscles Strength and Body Composition in Moderately Trained Males: A Randomized Controlled Study. Front. Public Health 2022, 10, 982062. [Google Scholar] [CrossRef]
- Álvarez-Barrio, L.; Rodríguez-Pérez, V.; Calvo-Lobo, C.; Leirós-Rodríguez, R.; Alba-Pérez, E.; López-Rodríguez, A.F. Immediate Effects of Whole-Body versus Local Dynamic Electrostimulation of the Abdominal Muscles in Healthy People Assessed by Ultrasound: A Randomized Controlled Trial. Biology 2023, 12, 454. [Google Scholar] [CrossRef] [PubMed]
- Wiecha, S.; Cieśliński, I.; Wiśniowski, P.; Cieśliński, M.; Pawliczek, W.; Posadzki, P.; Prill, R.; Zając, J.; Płaszewski, M. Physical Therapies for Delayed-Onset Muscle Soreness: An Umbrella and Mapping Systematic Review with Meta-Meta-Analysis. Sports Med. 2025, 55, 1183–1212. [Google Scholar] [CrossRef] [PubMed]
- Pascale, B.; Steele, C.; Attipoe, S.; O’Connor, F.G.; Deuster, P.A. Dietary Supplements: Knowledge and Adverse Event Reporting Among American Medical Society for Sports Medicine Physicians. Clin. J. Sport Med. 2016, 26, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Ayorinde, A.A.; Williams, I.; Mannion, R.; Song, F.; Skrybant, M.; Lilford, R.J.; Chen, Y.-F. Assessment of Publication Bias and Outcome Reporting Bias in Systematic Reviews of Health Services and Delivery Research: A Meta-Epidemiological Study. PLoS ONE 2020, 15, e0227580. [Google Scholar] [CrossRef]
- Hróbjartsson, A.; Emanuelsson, F.; Skou Thomsen, A.S.; Hilden, J.; Brorson, S. Bias Due to Lack of Patient Blinding in Clinical Trials. A Systematic Review of Trials Randomizing Patients to Blind and Nonblind Sub-Studies. Int. J. Epidemiol. 2014, 43, 1272–1283. [Google Scholar] [CrossRef]
- Monaghan, T.F.; Agudelo, C.W.; Rahman, S.N.; Wein, A.J.; Lazar, J.M.; Everaert, K.; Dmochowski, R.R. Blinding in Clinical Trials: Seeing the Big Picture. Medicina 2021, 57, 647. [Google Scholar] [CrossRef]
- Page, M.J.; Higgins, J.P.T.; Clayton, G.; Sterne, J.A.C.; Hróbjartsson, A.; Savović, J. Empirical Evidence of Study Design Biases in Randomized Trials: Systematic Review of Meta-Epidemiological Studies. PLoS ONE 2016, 11, e0159267. [Google Scholar] [CrossRef]
- Hannah, R.; Minshull, C.; Buckthorpe, M.W.; Folland, J.P. Explosive Neuromuscular Performance of Males versus Females. Exp. Physiol. 2012, 97, 618–629. [Google Scholar] [CrossRef]
- Seyri, K.M.; Maffiuletti, N.A. Effect of Electromyostimulation Training on Muscle Strength and Sports Performance. Strength Cond. J. 2011, 33, 70–75. [Google Scholar] [CrossRef]
- Kemmler, W.; Weissenfels, A.; Willert, S.; Shojaa, M.; Von Stengel, S.; Filipovic, A.; Kleinöder, H.; Berger, J.; Fröhlich, M. Efficacy and Safety of Low Frequency Whole-Body Electromyostimulation (WB-EMS) to Improve Health-Related Outcomes in Non-Athletic Adults. A Systematic Review. Front. Physiol. 2018, 9, 573. [Google Scholar] [CrossRef]
| Study | Participants (Sex) | Physical Characteristics | Level | Study Design | Results |
|---|---|---|---|---|---|
| Billot et al., 2010 [14] | 20 males | Electrostimulated group (n = 10; age 20.1 ± 2.1 years; height 1.76 ± 0.06 m; mass 69.5 ± 7.4 kg); comparison group (n = 10; age 21.7 ± 3.4 years; height 1.80 ± 0.05 m; mass 70.7 ± 11.0 kg). | Regional | Two groups maintained two weekly soccer training sessions and one match (5 h total). The EMS group additionally underwent 5 weeks of EMS training. | After 3 weeks of EMS training, isometric (p < 0.01) and eccentric knee extension torque (p < 0.01) and ball speed without run-up increased (p < 0.05). After 5 weeks of EMS training, eccentric, isometric, and concentric torques, along with ball speed, significantly improved (p < 0.001). |
| Bieuzen et al., 2012 [15] | 26 males | Age = 25.6 ± 5.7 years; height = 1.77 ± 0.8 m; mass = 75.0 ± 12.2 kg. | Professional | The athletes were divided into two groups, performed an intermittent fatiguing exercise, and then underwent a 1-h recovery period. The electrical stimulation group received 20 min of electrical stimulation during the recovery phase. | The group that received electrical stimulation exhibited enhanced performance in the 30-second all-out test (p = 0.03). |
| Taradaj et al., 2013 [16] | 80 males | / | Professional | All athletes participated in a structured exercise program three times per week for one month. Additionally, participants in Group A received NMES on both the right and left quadriceps muscles. | NMES significantly improved quadriceps strength and muscle circumference compared to the control group, on both the operated and non-operated sides (p < 0.05). |
| Filipovic et al., 2016 [17] | 22 males | EMS group (n = 12; age 24.9 ± 3.6 years; height 1.84 ± 0.05 m; mass 80.6 ± 9.2 kg), comparison group (n = 10; age 26.4 ± 3.2 years; height 1.82 ± 0.07 m; mass 78.3 ± 9.3 kg). | Professional | Experimental Group: Jump training + WB-EMS. Comparison Group: Jump training only. | EMS training significantly increased the one-legged maximal strength on the leg press machine (p = 0.001) and improved linear sprint performance (p = 0.039), sprint with direction changes (p = 0.024), vertical jump performance (p = 0.021), and kicking velocity (p < 0.001). |
| Barassi et al., 2019 [18] | 20 males | Age: 25.5 ± 10.6 years. | Semi-professional | The treatment group (TR) showed a significant increase in muscular tone (p < 0.05) but also an increase in stiffness and a decrease in elasticity. The TR group exhibited notable postural improvements (p < 0.05), whereas the control group (NTR) experienced postural deterioration. | |
| Filipovic et al., 2019 [19] | 28 males | / | Regional | EMS Group: n = 10: WB-EMS + 3 × 10 squat jumps + soccer training (7 weeks). Jump Training Group: n = 10: squat jumps + soccer training (no EMS). Control Group: n = 8: only regular soccer training. | EMS training significantly improved maximal strength in leg press (p = 0.009) and leg curl (p = 0.026), along with a significant increase in Type II muscle fiber diameter (p = 0.023). |
| Kale and Gurol, 2019 [20] | 23 males | Age: 18–24 years. | Competitive | Experimental Group: n = 10: regular training + EMS. Control Group: n = 13: regular training only. Study duration: 6 weeks. | Significant strength increases in the control group across all angular velocities (60°/s, 180°/s, 300°/s), particularly in both dominant and non-dominant legs (p < 0.05). |
| Hasan et al., 2022 [21] | 60 males | NMES group (n = 30; age 22.20 ± 1.83 years; height 1.65 ± 0.01 m; mass 63.33 ± 2.99 kg), sham NMES group (n = 30; age 22.07 ± 1.80 years; height 1.66 ± 0.02 m; mass 65.20 ± 2.30 kg). | Collegiate | NMES Group (n = 30): NMES-guided strength training + plyometric training. Sham NMES group (n = 30): Sham NMES-guided strength training + plyometric training. | NMES significantly improved strength (STN) (p < 0.001) and sprint performance (ST) (p = 0.002) compared to controls. |
| Labib and Sabah, 2024 [22] | 50 males | NMES group (n = 25; age 24.16 ± 4.34 years; height 1.79 ± 0.07 m; mass 63.24 ± 3.62 kg), comparison group (n = 25; age 25.32 ± 3.68 years; height 1.77 ± 0.06 m; mass 63.80 ± 3.48 kg). | / | NMES Group (n = 25): NMES + standard rehabilitation program. Comparison Group (n = 25): Standard rehabilitation program. | NMES significantly improved functional outcomes compared to the control group at both 12 and 16 weeks post-rehabilitation (p < 0.001). |
| Fernández-Elías et al., 2024 [23] | 12 males | Age 21.75 ± 1.86 years; height 1.79 ± 0.06 m; mass 71.58 ± 6.86 kg. | Semi-professional | WB-EMS Group (n = 12): WB-EMS + FIFA11 + warm-up protocol. Comparison Group (n = 12): FIFA11 + warm-up protocol. | Left popliteal Tsk was significantly lower after WB-EMS warm-up compared to NO WB-EMS (p < 0.05, ES: ηp2 = 0.62). Capillary blood lactate significantly increased only in the NO WB-EMS trial (p < 0.05). The 20 m sprint time was significantly faster (0.2 s improvement) after WB-EMS warm-up compared to NO WB-EMS (p < 0.05). |
| Study | Training Period | Training Frequency | EMS Context | Stimulation Site | Impulse Width (μs) | Stimulation Frequency (Hz) | Impulse Intensity (mA) | On Time (on, s) | Interval (off, s) |
|---|---|---|---|---|---|---|---|---|---|
| Billot et al., 2010 [14] | 5 weeks | 3 sessions per week | In-season training | Vastus medialis and vastus lateralis | 400 | 100 | 60–120 | 3 | 17 |
| Bieuzen et al., 2012 [15] | 1 h recovery after fatiguing exercise | 1 session | Recovery after intermittent fatigue exercise | Medial-central part of the calf (bilateral placement) | 240 | 1 (first 5 min), 1.25 (next 5 min), 1.5 (next 5 min), 1.75 (final 5 min) | Adjustable (minimum threshold set to visible, comfortable contraction) | / | / |
| Taradaj et al., 2013 [16] | 1 month | 3 sessions per week | Post-ACL reconstruction rehabilitation | Both quadriceps | 1000 | 50 | 55–67 (mean = 58.89) | 10 | 50 |
| Filipovic et al., 2016 [17] | 14 weeks | 2 sessions per week | In-season training | Chest, back, abdominal muscles, glutes, thigh muscles, and calves | 350 | 80 | Individually adjusted using Borg scale (80–90%) | 4 s per jump | 10 s (duty cycle ~28%) |
| Barassi et al., 2019 [18] | 4 weeks | 4 sessions per week | In-season training | Whole body (via dermatomeral and metameric pathways) | / | 15–350 | Modulated based on tissue | 10 min per program, 20 min total per session | / |
| Filipovic et al., 2019 [19] | 7 weeks | 3 sessions per week | Preseason training | Chest, upper and lower back, latissimus, abdominals, glutes, thighs, calves | 350 | 80 | 0–120 mA, adjusted for each muscle group using Borg RPE scale (16–19, “hard to very hard”) | 4 s per squat jump (2 s eccentric, 1 s isometric, 0.1 s concentric, 1 s landing/stabilization) | 10 s rest (duty cycle ~28%) |
| Kale and Gurol, 2019 [20] | 6 weeks | 3 sessions per week | In-season training | Vastus medialis, vastus lateralis, and rectus femoris | 400 | 100 | Increased until muscle contraction was initiated (individually adjusted) | 10 | 3 |
| Hasan et al., 2022 [21] | 8 weeks | 3 sessions per week | In-season training | Femoral nerve and quadriceps femoris | 2500 | 75 | Max tolerated | 5 | 8 |
| Labib and Sabah, 2024 [22] | 6 weeks | 6 sessions per week | Post-ACL reconstruction rehabilitation | Rectus femoris and vastus lateralis | 2500 | 75 | Adjusted per individual | 10 | 50 |
| Fernández-Elías et al., 2024 [23] | 1 session (per trial) | The two experimental sessions were separated by one week | Preseason | Upper body (chest, upper back, lower back, abs), lower body (glutes, thighs, hamstrings, calves) | 350 | 20 | Adjusted per individual | / | / |
| Randomization Process | Deviations from Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall | |
|---|---|---|---|---|---|---|
| Billot et al., 2010 [14] | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Bieuzen et al., 2012 [15] | Low risk | Low risk | Low risk | Some concerns | Some concerns | Some concerns |
| Taradaj et al., 2013 [16] | Low risk | High risk | Low risk | Low risk | Some concerns | High risk |
| Filipovic et al., 2016 [17] | Low risk | Some concerns | Low risk | Low risk | Some concerns | Some concerns |
| Barassi et al., 2019 [18] | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Filipovic et al., 2019 [19] | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Kale and Gurol, 2019 [20] | Low risk | Some concerns | Low risk | Some concerns | Low risk | Some concerns |
| Hasan et al., 2022 [21] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Labib and Sabah, 2024 [22] | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Fernández-Elías et al., 2024 [23] | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shu, M.-Y.; Oh, H.S.; Jo, Y.-J.; Eom, S.-H.; Liang, J.; Jung, S.M.; Kim, K.-W.; Jung, J.-H.; Ma, C.W.; Kim, C.-H. The Impact of Electromyostimulation on Strength, Recovery, and Performance in Soccer Athletes: A Systematic Review. Appl. Sci. 2025, 15, 7950. https://doi.org/10.3390/app15147950
Shu M-Y, Oh HS, Jo Y-J, Eom S-H, Liang J, Jung SM, Kim K-W, Jung J-H, Ma CW, Kim C-H. The Impact of Electromyostimulation on Strength, Recovery, and Performance in Soccer Athletes: A Systematic Review. Applied Sciences. 2025; 15(14):7950. https://doi.org/10.3390/app15147950
Chicago/Turabian StyleShu, Meng-Yuan, Hyoung Suk Oh, Young-Jin Jo, Seon-Ho Eom, Jian Liang, Sang Mok Jung, Ki-Wan Kim, Joo-Ha Jung, Chae Woo Ma, and Chul-Hyun Kim. 2025. "The Impact of Electromyostimulation on Strength, Recovery, and Performance in Soccer Athletes: A Systematic Review" Applied Sciences 15, no. 14: 7950. https://doi.org/10.3390/app15147950
APA StyleShu, M.-Y., Oh, H. S., Jo, Y.-J., Eom, S.-H., Liang, J., Jung, S. M., Kim, K.-W., Jung, J.-H., Ma, C. W., & Kim, C.-H. (2025). The Impact of Electromyostimulation on Strength, Recovery, and Performance in Soccer Athletes: A Systematic Review. Applied Sciences, 15(14), 7950. https://doi.org/10.3390/app15147950







