1. Introduction
The development of effective healthcare strategies presents a multifaceted challenge requiring comprehensive consideration of sector-specific determinants. As both a fundamental economic driver and a social welfare mechanism, healthcare systems play a pivotal role in national development. Healthcare institutions in Colombia, however, face systemic challenges, including insufficient service coverage (23% of medical needs went unaddressed in 2022), suboptimal care quality, and operational deficiencies [
1]. These limitations are exacerbated by structural barriers—from service delivery shortcomings to administrative bottlenecks—with 33.7% of constitutional injunctions (tutelas) directly attributable to procedural delays [
2]. Such systemic inefficiencies, rooted in inadequate policy frameworks and resource mismanagement, require regional health authorities and planning institutions to implement and necessitate strategic reallocation toward high-impact health initiatives.
Within Colombia’s Meta department (29 municipalities), extractive industry royalties—mandatory payments made by companies exploiting non-renewable natural resources such as oil and minerals that are paid to the State—have historically financed critical social infrastructure [
3]. The 2020 Royalty System Reform (Law 2056) fundamentally altered resource distribution mechanisms, disproportionately affecting Meta due to local governance capacity constraints [
4]. While newly established Territorial Planning Councils have strengthened participatory budgeting [
5,
6] local health authorities and planning institutions must implement rigorous, criteria-based health investment strategies that leverage community expertise in identifying localized health priorities.
This study employs multicriteria decision analysis to optimize health project prioritization in Meta, where geographical fragmentation, infrastructure gaps, and environmental health risks disproportionately affect rural and vulnerable populations (including indigenous communities and agricultural workers). Analysis of epidemiological data by the authors reveals acute challenges: elevated preventable mortality rates, diabetes prevalence (18.7%), childhood malnutrition (12.3%), and persistent vector-borne disease threats [
7]. These interconnected issues demand an integrated analytical approach that enables the simultaneous consideration of technical, social, and spatial factors, facilitates the modeling of interdependent criteria, and supports transparent, evidence-based decisions aimed at improving equity and health outcomes in complex territorial contexts.
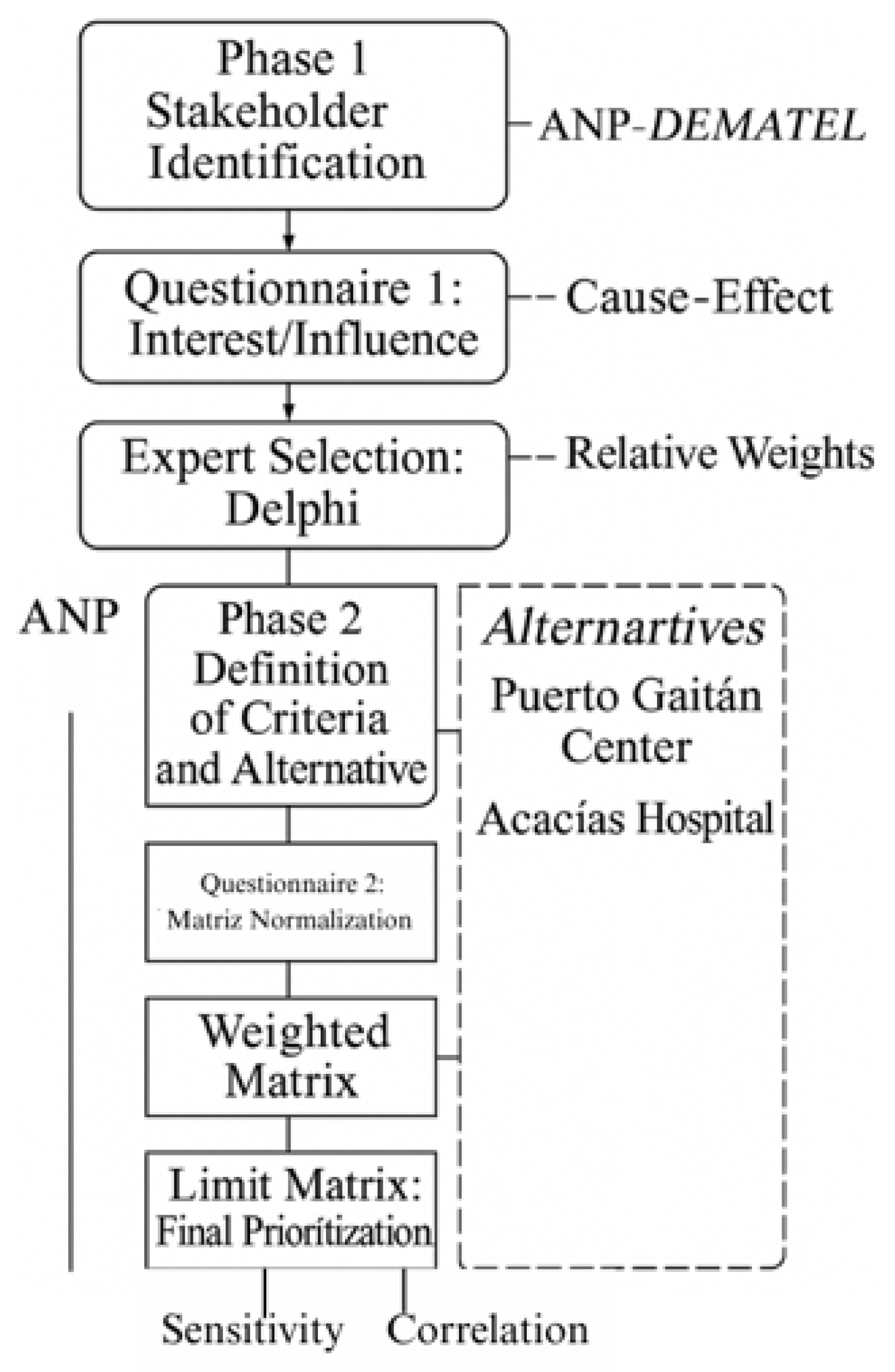
The authors adopted the ANP-DEMATEL hybrid methodology to address this complexity by (1) modeling criterion interdependencies; (2) quantifying systemic relationships, and (3) enabling evidence-based resource allocation [
8].
3. Materials and Methods
The selection of stakeholders was guided by their level of interest, motivation, and expectations regarding the issue and the broader decision-making process [
22,
23]. A stakeholder mapping exercise was conducted to identify key actors with influence over health-related decisions, ensuring balanced representation across sectors [
23,
24]. The selection criteria included experience in public health, hospital planning, and the evaluation of infrastructure and health service projects, with a minimum of five years of professional background in these areas. Experts involved in health policy formulation and regional resource allocation were also included, particularly those familiar with project prioritization methodologies (see
Figure 1).
The process began with the administration of Questionnaire 1 (
Table A1) to a group of 82 experts. The objective was to assess participants’ levels of interest and influence in health-related decision-making. Based on their responses, individuals were classified into four quadrants according to the stakeholder mapping framework: manage closely, keep informed, keep satisfied, and monitor [
25,
26].
The “Manage Closely” quadrant, comprising stakeholders with both high interest (mean score = 4.7/5) and high influence (mean score = 4.5/5), was identified as the optimal decision-making cohort according to established stakeholder management theory; however, quantitative analysis revealed only one participant met these stringent criteria (representing just 1.4% of the sample), suggesting limited direct representation of this ideal profile. Consequently, the analytical focus shifted to the “Keep Satisfied” quadrant, which contained the majority of participants
(n = 42; 58.3%) exhibiting substantial policy interest (mean = 4.2/5) coupled with moderate influence (mean = 3.1/5). This group was subsequently designated as the primary decision-making body, with
Figure 2b providing detailed demographic and professional characteristics of these key stakeholders.
3.1. Participant Identification and Data Collection
A group of key stakeholders (with a 40.3% response rate) participated in the questionnaire phase. This sampling approach aligns with the methodological literature, which emphasizes the importance of participant expertise over sample size in policy-focused research. This view is supported by Johnson et al. (2021) [
27], who found that decision quality tends to plateau beyond 25–30 qualified experts.
3.2. Definition of Criteria and Alternatives
The authors conducted a comprehensive document analysis of three key policy instruments: (1) the Territorial Health Plan (2022 revision), (2) the Departmental Development Plan (2020–2023), and (3) the most recent Health Situation Analysis (ASIS, 2021) [
28]. Through an iterative Delphi process involving five senior health policy experts from the Meta Department government (mean experience = 12.4 years), the team established a hierarchical decision framework comprising nine primary evaluation criteria (e.g., health equity improvement, resource efficiency), eighteen secondary indicators (including specific metrics like reduction in maternal mortality rates), and five concrete project alternatives. This structured approach ensured alignment between research objectives and departmental strategic priorities, with the complete criteria taxonomy and project alternatives presented in
Table 1 and
Table 2, respectively. The Delphi process achieved strong consensus (Kendall’s W = 0.82,
p < 0.01) after three rounds, indicating robust agreement among experts regarding the selected criteria and their relative importance weights [
29,
30].
3.3. Construction of the Influence Matrix Between Network Elements
The influence matrix was constructed to map the complex web of relationships within the health system decision network, following the DEMATEL methodology. Through structured expert consultations (Questionnaire 2, see Annex
Table A2 for a summarized version of the instrument), all 29 participating specialists evaluated directional influences between elements. Their responses enabled the creation of a relational map that captured four dimensions of interaction: (i) mutual influences among criteria, (ii) impacts of criteria on alternatives, (iii) feedback effects from alternatives to criteria, and (iv) interdependencies among alternatives.
This approach is consistent with DEMATEL protocols for complex system analysis, where each matrix entry quantifies the directed influence from one element to another. After two Delphi rounds, the expert panel achieved substantial agreement (Fleiss’ κ = 0.78) on a six-point scale ranging from “None” (0) to “Very High” (5), with clear operational definitions. The scale is summarized in
Table 3. The use of a 0–5 scale aligns with standard DEMATEL practice to reduce cognitive burden [
31]; although debates continue regarding optimal granularity, evidence suggests that five-point scales enhance response quality without sacrificing discriminative power [
18].
Complete documentation of individual expert judgments (E1 to E29) was maintained throughout the process. Appendix
Table A2 presents the influence matrix from Expert E1, selected for its high consistency (CR = 0.92).
Table 4 provides an illustrative submatrix that captures nuanced relationships—such as the moderate influence of water access (C.1.1) on cardiovascular health (C.2.1) and the absence of direct influence on suicide rates (C.3.1). These examples highlight the method’s ability to detect specific directional relationships often missed by traditional ranking techniques.
The resulting matrices enabled a comprehensive mapping of both direct and indirect relationships across the health system. This phase converted qualitative expert input into structured, quantifiable data, bridging theory and practical application. It also supported the identification of leverage points within the network—nodes where targeted interventions could produce disproportionately large system-wide effects. These insights are especially valuable in resource-constrained environments where strategic prioritization is essential.
As an example,
Table 4 presents the observed influence values from items C.1.1 to C.3.2 over items C.1.1 to C.3.2 for one of the experts.
3.4. Creation of the Influence Matrix Between Network Groups
The authors asked experts to evaluate the influence relationships among the different groups within the network, following the procedure previously described. This analysis enabled the construction of matrices that represent such interactions, the results of which are shown in
Table 5.
3.5. Determination of the Unweighted Matrix
The authors normalized the influence matrix in the DEMATEL method involves summing the values of the elements of the same group within each column and dividing each individual value by this sum. This procedure yields the unweighted matrix used in the ANP method, allowing a significant reduction in the number of questions posed to experts. Compared to the traditional ANP method, which requires multiple pairwise comparison matrices, this approach simplifies the process.
Table 6 shows a fragment of the normalized influence matrix.
The authors obtained the values in column C2.2 and rows C1.1 to C2.2 by summing those positions from
Table 7 and dividing each by the total. This reformulated approach simplified the calculation compared to ANP, which would have required more complex and detailed pairwise comparison evaluations.
Table 7 shows the equivalent unweighted supermatrix generated through this procedure.
The influence matrix among groups in DEMATEL is normalized by summing the values of each column in the matrix and dividing each element by this sum. The normalized matrix, derived from
Table 4, is presented in
Table 5 as the equivalent of the cluster matrix in the ANP method. This approach significantly reduced the number of questions posed to experts, as the ANP model would have required judgments across seven pairwise comparison matrices.
3.6. Determination of the Weighted Matrix
The authors constructed the weighted matrix by normalizing each column of the original influence matrix. This matrix (
Table 5), derived from the initial influence matrix (
Table 4), serves as the cluster matrix equivalent in the ANP method. This method significantly reduced the number of expert judgments, avoiding the need for seven pairwise comparison matrices. The weighted matrix of relationships between network elements is presented in
Table 8.
A key property of the weighted matrix is its column stochastic nature, where each column sums to unity. Columns not meeting this requirement were re-normalized to satisfy this condition.
3.7. Calculation of the Limit Matrix
The authors derived the limit matrix by exponentiating the weighted matrix to progressively higher powers until column convergence was achieved. The resulting identical column values (“raw values”) represent the relative influence of each network element. The final priorities were determined by normalizing these raw values for both criteria and alternatives. Appendix
Table A3 presents the complete matrices and priorities assigned by Expert E1.
The full methodological workflow—including stakeholder identification, criteria definition, and the ANP-DEMATEL prioritization process—is illustrated in
Figure 3.
4. Results
The authors applied expert-derived influence models consisting of relationship matrices and limit matrices to quantify interconnections among network elements and groups. These analytical constructs facilitated the determination of expert-specific priority assignments for system components. Additionally, stakeholders completed Questionnaire 2 (
Table A4) to evaluate both criteria importance and alternative prioritization. Analysis was performed using SuperDecisions software version number 3.2.0 [
31,
32]. The authors aggregated priorities by calculating the geometric mean of re-normalized expert judgments, following the methodological framework by Forman and Peniwati (1998) [
33], which accounts for individual judgment variability.
The consolidated outcomes are presented in
Table 9 (criteria priorities, with percentage values enabling comparative interpretation across all evaluated elements).
The comparative analysis reveals that criterion C.4.1 (8.54%) received the highest weight, highlighting its focus on reducing the proportion of the population with Unmet Basic Needs (UBNs). Its prioritization reflects its direct contribution to improving quality of life, reducing socioeconomic inequalities, and promoting food and nutritional security for vulnerable populations.
Criterion C.6.1 (8.15%), which focuses on expanding hospital capacity for emergencies and disasters, underscores the importance of preparedness for health crises. Its position reflects the emphasis on public health system resilience and responsiveness.
Similarly, criterion C.9.2 (7.59%) emphasizes financial sustainability, efficient resource allocation, and strategic planning to enhance the longevity and effectiveness of health interventions.
Criterion C.6.2 (7.55%) addresses access to basic and advanced emergency transport in rural and remote areas. Criterion C.4.2 (7.14%) targets the reduction of acute malnutrition in children under five and was prioritized for its impact on nutrition outcomes.
Other relevant criteria include C.2.2 (7.03%) for oral health, C.8.1 (6.96%) for Indigenous and rural health access, and C.3.2 (6.00%) for reducing domestic violence—underscoring the relevance of mental health and social cohesion.
Other important criteria include C.2.2 (7.03%), aimed at reducing oral health problems—a frequently overlooked determinant of general health and a key factor in preventing non-communicable diseases. Criterion C.8.1 (6.96%) promotes equitable access to healthcare services for dispersed rural and Indigenous populations, reaffirming the importance of differential approaches in health policy. Finally, criterion C.3.2 (6.00%) addresses the reduction of domestic violence, thus highlighting the relevance of mental health and social cohesion within the broader public health agenda.
This prioritization pattern demonstrates that experts placed a strong emphasis on criteria related to equity, system sustainability, access to essential services, and emergency preparedness, reflecting a multidimensional understanding of health system strengthening. It integrates technical, social, and territorial considerations to guide decision-making and optimize the overall impact of health investments [
34,
35]. The prioritization analysis identified the replacement of the healthcare center in Puerto Gaitán (A05, 29.84%) as the highest-ranked project due to its strategic role in the hospital accessibility network. As shown in
Table 10 and summarized below, the prioritized alternatives are ranked from highest to lowest based on the final group weights. The prioritized projects are listed as follows:
Project A05, prioritized with a score of 29.84%, is associated with criterion C.4.1 (reduction of Unmet Basic Needs—UBN, weighted at 8.54%) (see
Table 9), indicating a direct impact on access to basic services such as drinking water and sanitation. Its implementation would benefit over 15,000 residents in an area with a high prevalence of occupational diseases. Project A04, with a score of 22.31%, addresses the hospital capacity deficit in Acacías, where a 60% increase in hospitalization capacity is projected, along with a significant reduction in surgical waiting lists [
7].
A panel of 29 health sector experts from the Meta department employed the integrated ANP/DEMATEL methodology to evaluate priority health projects. The analysis identified the replacement of Puerto Gaitán’s healthcare center (A05) as the highest priority (29.84%), followed by the expansion of Acacías municipal hospital (A04. 20%). Other significant projects included establishing an emergency regulatory center (A03. 17.95%), implementing primary healthcare actions (A02. 16.11%), and strengthening emergency transport services in La Macarena (A01. 16.10%).
This prioritization reflects three critical health system needs: (1) infrastructure modernization in high-demand areas (A05. A04), (2) emergency response capacity building (A03), and (3) rural service accessibility improvement (A02. A01). The ANP-DEMATEL framework effectively captured the complex interdependencies between these projects, revealing how strategic investments in infrastructure (A05. A04) create foundational capacity that supports subsequent emergency system (A03) and rural service (A02. A01) enhancements.
Correlation and Compatibility Analysis
The authors analyzed variable rank relationships using both Spearman’s and Kendall’s correlation methods, identifying Kendall’s Tau-b as the primary statistical indicator due to its robustness and effectiveness with small samples and tied observations [
36]. To evaluate priority vector consistency within the AHP/ANP framework, the authors applied two validated compatibility metrics: Saaty’s S index and Garuti’s G index [
37], which applies a physical interpretation to vector inner products [
38,
39].
Table 11 presents Kendall’s Tau-b coefficients with
p-values and compares individual versus group priorities using S and G compatibility indices. This dual-metric approach supports rigorous analysis of both rank order and directional alignment.
The compatibility analysis reveals that Expert 1 (E1) is highly aligned with the group consensus, as shown by the Kendall’s Tau-b coefficient of 0.8. This concordance positions E1 as a reference point for validating group priorities and guiding expert discussions. In contrast, Expert 2 (E2) shows low compatibility (Kendall = 0.2), suggesting possible divergence in criteria interpretation or evaluative emphasis. Targeted alignment sessions could help harmonize E2′s contributions and improve overall group coherence.
Expert 4 (E4), with a negative Kendall coefficient (−0.2), reflects significant divergence; however, this difference can enrich analysis if addressed through inclusive dialogue and collaborative workshops.
The E1–E2 comparison (Kendall = 0.4) indicates low compatibility, possibly due to divergent heuristics or methodological preferences. Facilitating exchanges between these experts may help bridge conceptual gaps. Conversely, moderate compatibility between E2 and E4 (Kendall = 0.6) suggests potential complementarity and an opportunity for shared insights.
The results from the S and G indices reinforce the observed variability in expert priority vectors. These variations may stem from disciplinary or cognitive differences in evaluation; therefore, implementing consensus-building strategies such as joint reviews, shared criteria interpretation, and iterative feedback is essential to ensure methodological cohesion.
In summary, promoting leadership among highly compatible experts (e.g., E1) while actively including divergent perspectives fosters a more robust and participatory decision-making process. Such strategies reinforce analytical rigor and enhance shared ownership of prioritization outcomes.
5. Discussion
The prioritization analysis identified the replacement of the healthcare center in Puerto Gaitán (A05, 29.84%) as the highest-ranked project due to its strategic role in the hospital accessibility network. These findings underscore infrastructure improvement as a key driver of equity, aligning with approaches in Argentina, where multicriteria evaluation has guided the placement of new healthcare centers in underserved areas [
40]. In contrast, Cuba and Uruguay prioritize primary healthcare, reflecting their advanced infrastructure and focus on preventive strategies [
41]. This divergence highlights the need for prioritization frameworks to adapt to local contexts.
The proposed prioritization reflects the needs identified in the ASIS 2021 [
7] and is designed to generate tangible impacts. A05 not only addresses a historical infrastructure gap but could also reduce UBN by an estimated 25% within its coverage area. A03, related to emergency regulation, would prevent an estimated USD 2.5 million in annual losses due to avoidable incapacities, based on the regional burden of disease models presented in ASIS 2021 [
7]. A02 and A01 prioritize territories with over 50% Indigenous population and elevated maternal mortality rates, directly contributing to the reduction of rural health disparities.
Notably, decision-making criteria vary across regions and reflect not only technical and socioeconomic factors but also deeper political ideologies. In Brazil, efficiency and equity dominate healthcare planning, particularly in high-inequality settings, whereas Cuban policymakers prioritize equity over efficiency [
42]. This contrast may be explained by ideological underpinnings: Brazil’s decentralized and market-oriented governance tends to emphasize managerial efficiency, while Cuba’s centralized socialist model places equity at the core of its public health strategies. Colombia has adopted integrated ANP-DEMATEL methodologies for health sector project prioritization, though these are typically applied at the national level. By focusing on the regional level (Meta department), this article demonstrates how prioritization frameworks must be sensitive not only to territorial specificities but also to the institutional and normative context in which decisions are made.
Financial sustainability emerged as a critical consideration, raising questions about the long-term viability of proposed investments. A key debate centers on whether sustainability should focus solely on resource management or incorporate structural reforms to ensure equitable and efficient resource distribution. Sustainability must be evaluated not only economically but also through social and political lenses, necessitating broader discussions on healthcare equity and the State’s role in service provision [
43,
44].
The ANP-DEMATEL framework provided a robust structure for modeling complex interdependencies among criteria and alternatives. Grounded in Participatory Process Theory, these tools integrate diverse perspectives, fostering inclusive decision-making; however, their implementation faces challenges, including the need for decision-maker training and reliance on high-quality data. To maximize utility, technical analyses should be paired with participatory processes that enhance decision legitimacy.
Our findings correlate with the Situational Health Analysis (ASIS) of Meta, where prioritized projects (e.g., A05 and A04) address critical infrastructure gaps. Projects A02 and A01 target geographic dispersion and access barriers in rural and Indigenous communities, reinforcing the need for context-specific strategies to reduce health inequities [
45].
This article contributes to administrative discourse by demonstrating how advanced analytical methods (ANP-DEMATEL) can be combined with structured stakeholder participation to improve decision-making in decentralized health systems. Specifically, it provides a practical framework for local authorities to prioritize health investment projects in a way that balances technical criteria with social legitimacy. The article offers actionable insights for policymakers in the Meta Department, including (1) the adoption of integrated multicriteria methodologies (ANP-DEMATEL) to align technical decisions with stakeholder engagement; (2) the use of structured surveys to map interest and influence in territorial health planning; and (3) the prioritization of infrastructure and accessibility interventions as high-impact criteria in underserved contexts. In doing so, it illustrates how expert judgment and participatory processes can be integrated into formal planning tools, reinforcing transparency and institutional coordination.
Future research should explore additional decision criteria, such as financial sustainability and implementation capacity, which were not explicitly addressed in this analysis. Longitudinal studies assessing the impact of prioritized projects on health indicators are also recommended. Policymakers are encouraged to adopt collaborative and adaptive strategies that align decisions with the evolving dynamics of the health system [
46,
47]. In addition, the prioritization results were shared with participating stakeholders, reinforcing transparency and encouraging institutional appropriation of the findings.
6. Conclusions
This article employed a Multicriteria Decision-Making (MCDM) approach—integrating ANP and DEMATEL—to prioritize health projects in Meta. The replacement of Puerto Gaitán’s healthcare center (A05) was ranked highest, followed by the expansion of Acacías’ municipal hospital (A04) and the creation of an emergency regulation center. Correlation analysis revealed a strong link between hospital expansion and reduced unmet basic needs, highlighting the interplay between social determinants and healthcare infrastructure. The high consistency in expert rankings underscores the robustness of the ANP-DEMATEL model.
A relevant methodological limitation identified in this study is the partial disconnect between the highest-weighted criterion (C4.1: reduction of the population with Unmet Basic Needs) and the evaluated alternatives, which do not explicitly address it. Although the ANP-DEMATEL model captured indirect influences between criteria—thereby reflecting some of the impact of alternatives such as A05 and A04 on improving structural conditions—this lack of direct alignment between strategic objectives and proposed actions may affect the interpretation of results. It is recommended that future applications reinforce the conceptual correspondence between high-priority criteria and selected projects through an intermediate portfolio validation stage. This experience demonstrates the utility of the ANP-DEMATEL approach not only for modeling interdependencies but also for revealing potential gaps between strategic intent and the technical execution of decisions.
Sensitivity analysis confirmed the stability of results under a 10% variation in weight assignments, reinforcing the methodology’s reliability for public health planning. From a policy standpoint, integrated resource allocation—prioritizing accessibility and equity—is essential. Stakeholder inclusion enhances transparency, though a key limitation was the limited availability of some experts. We recommend replicating this approach in other Colombian regions to assess broader applicability. Further methodological refinements could combine MCDM with cost–benefit analysis and predictive modeling for healthcare infrastructure planning.
These priorities, validated through the participation of 42 institutional stakeholders and formally shared with them, provide a strategic roadmap to guide public health investment in Meta. They are expected to optimize the social return on allocated resources and reduce structural inequities in access to essential services.