Age-Related Compensatory Gait Strategies During Induced Perturbations in the Pre-Swing Gait Phase: A Kinematic and Kinetic Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
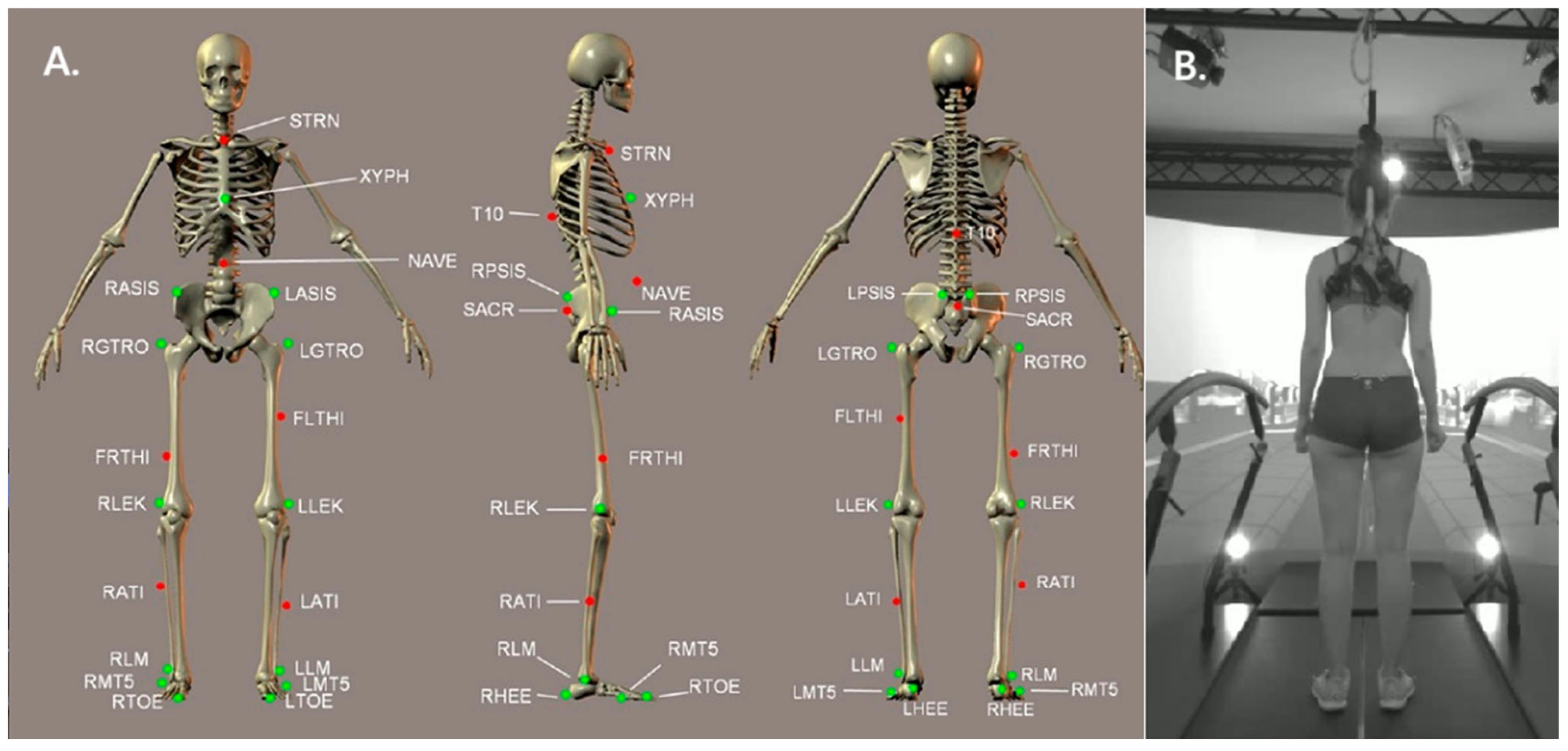
2.2. Measurement Protocol and Perturbation Specification
2.3. Parameters and Strategies Identification
2.4. Statistical Analysis
3. Results
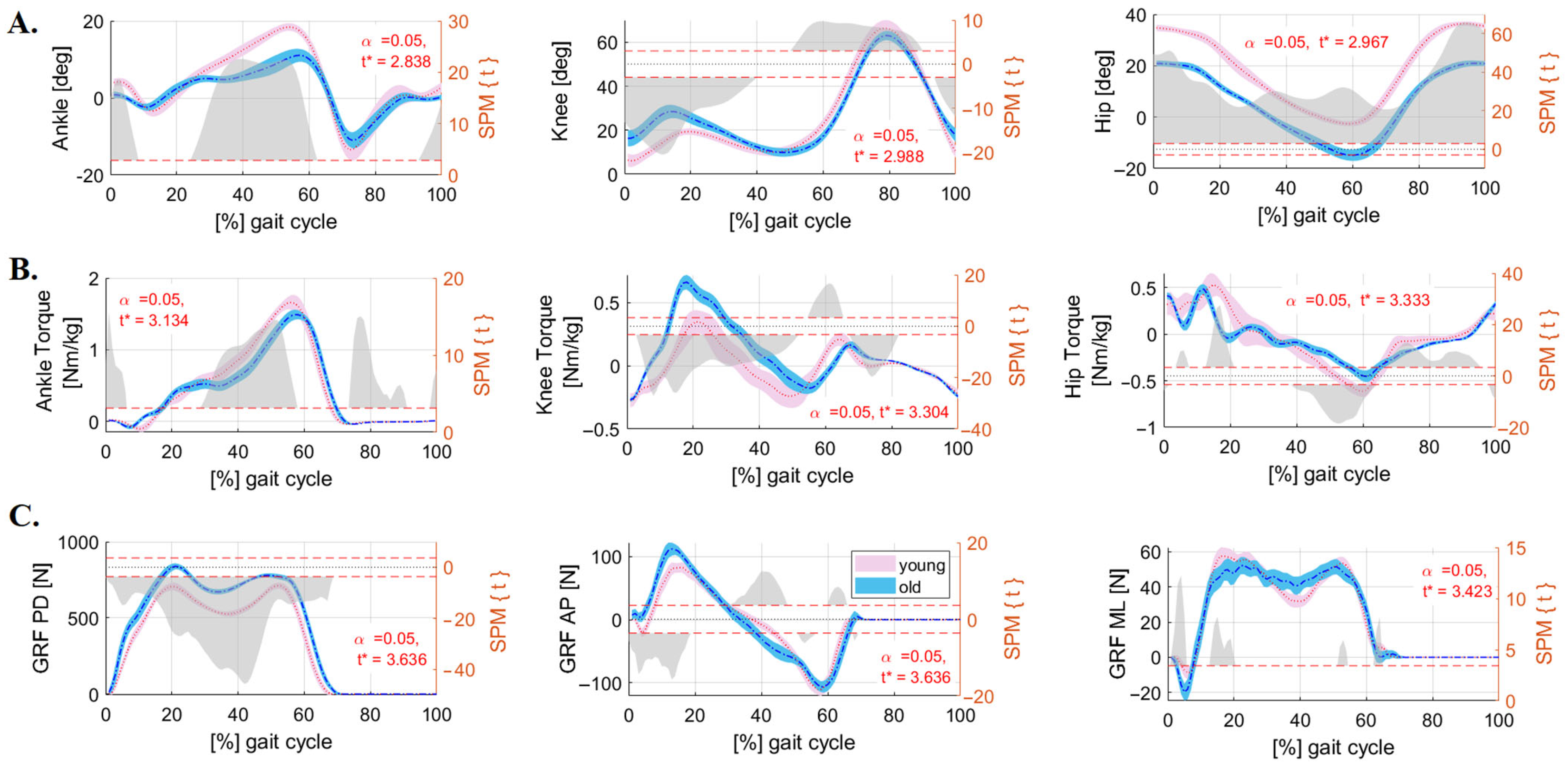
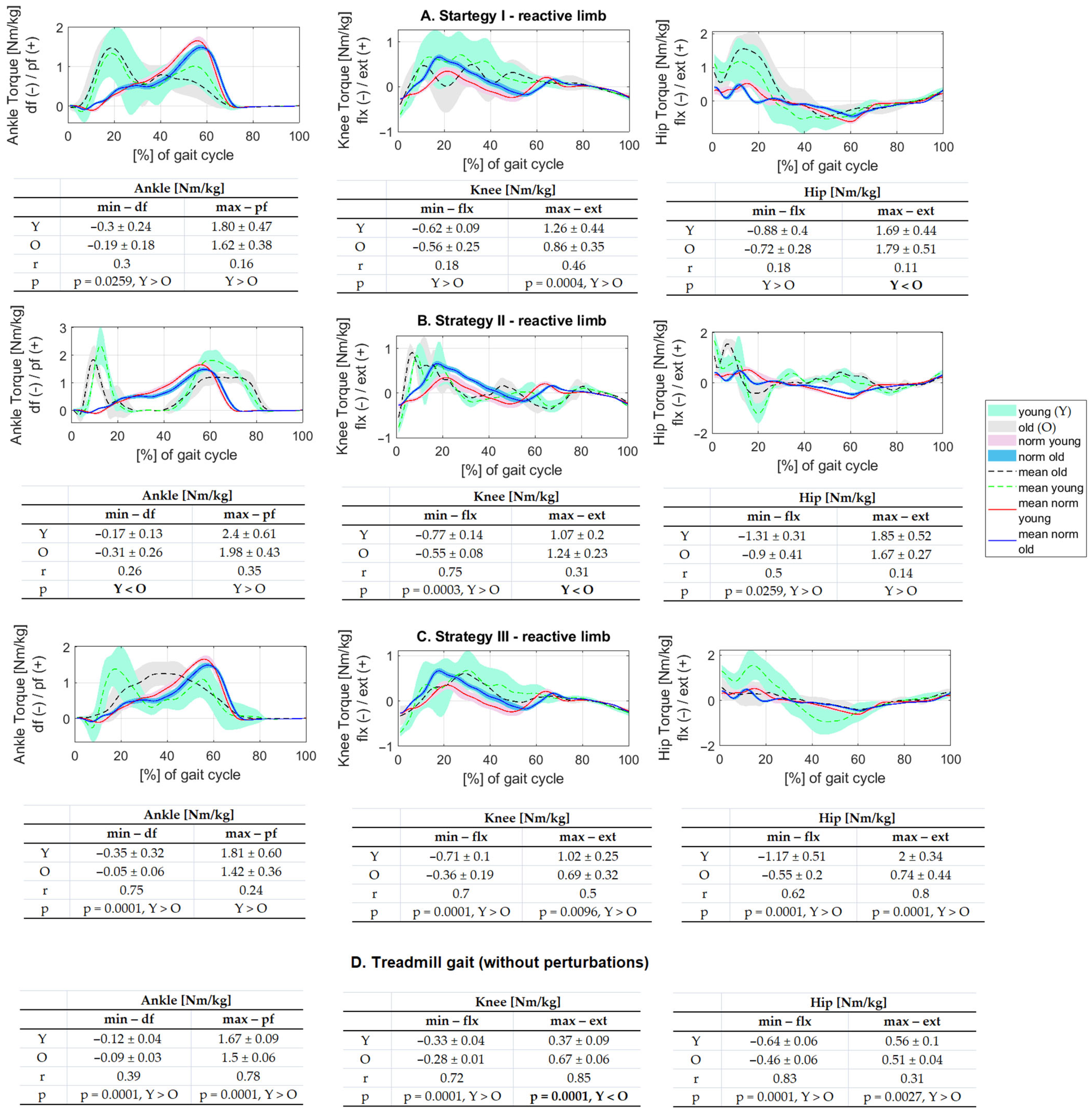
3.1. Differences Between Groups in Treadmill Gait Without Perturbations
3.2. Description of Response to Perturbation for Kinematic and Kinetic Parameters–Perturbed Limb
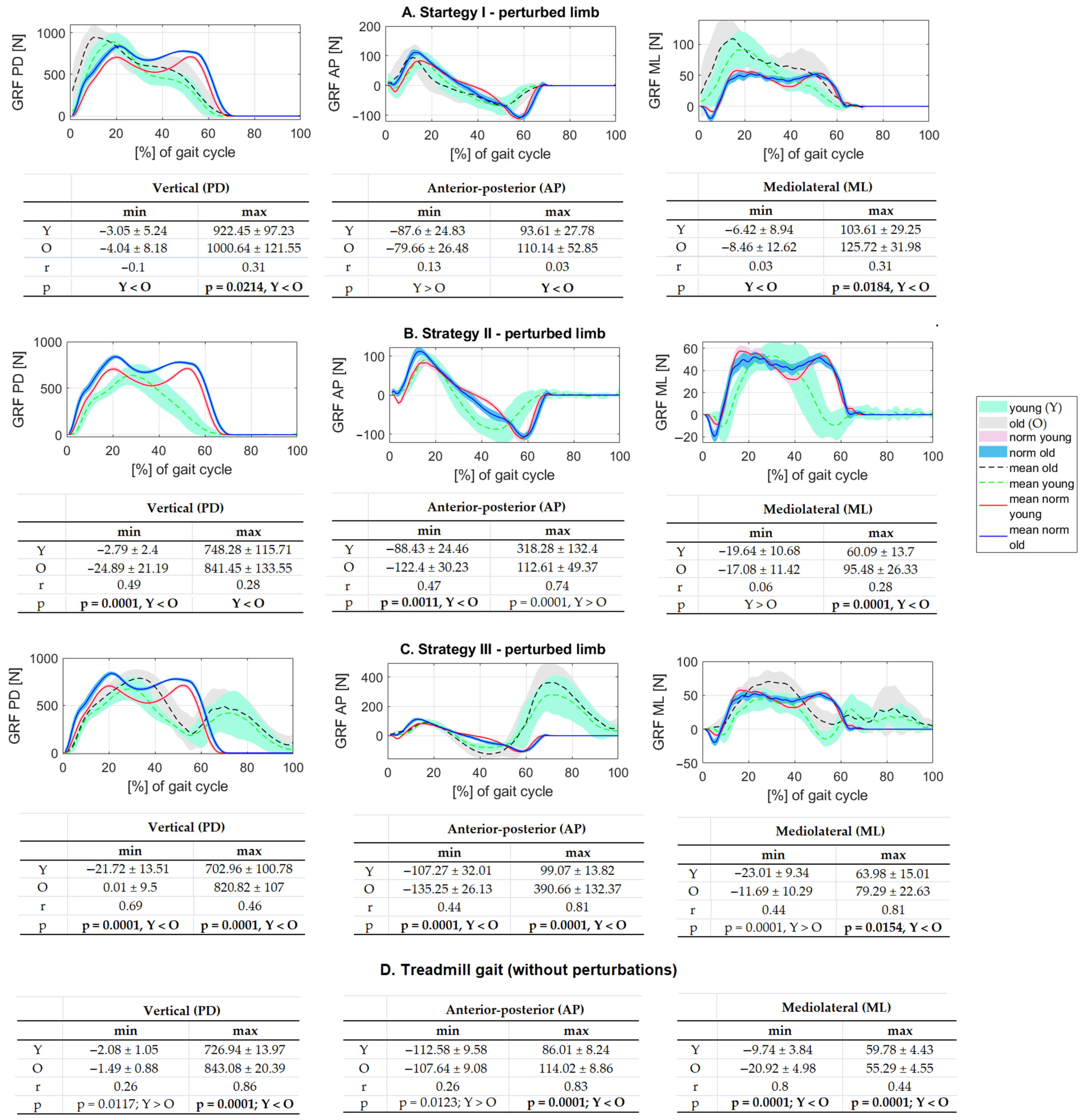
3.2.1. Ground Reaction Forces
3.2.2. Kinematic Parameters
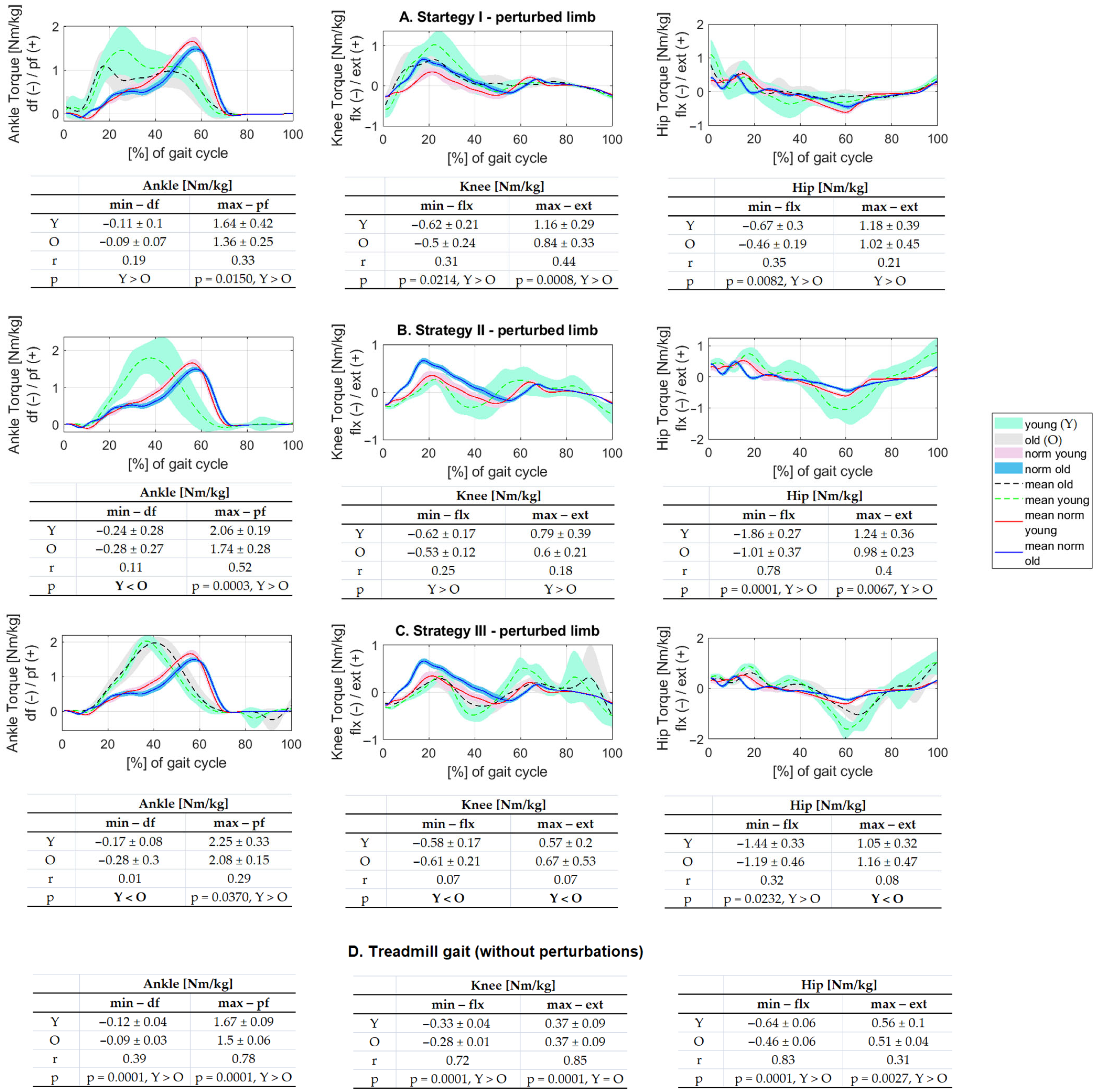
3.2.3. Kinetic Parameters
3.3. Description of Response to Perturbation for Kinematic and Kinetic Parameters–Reactive Limb
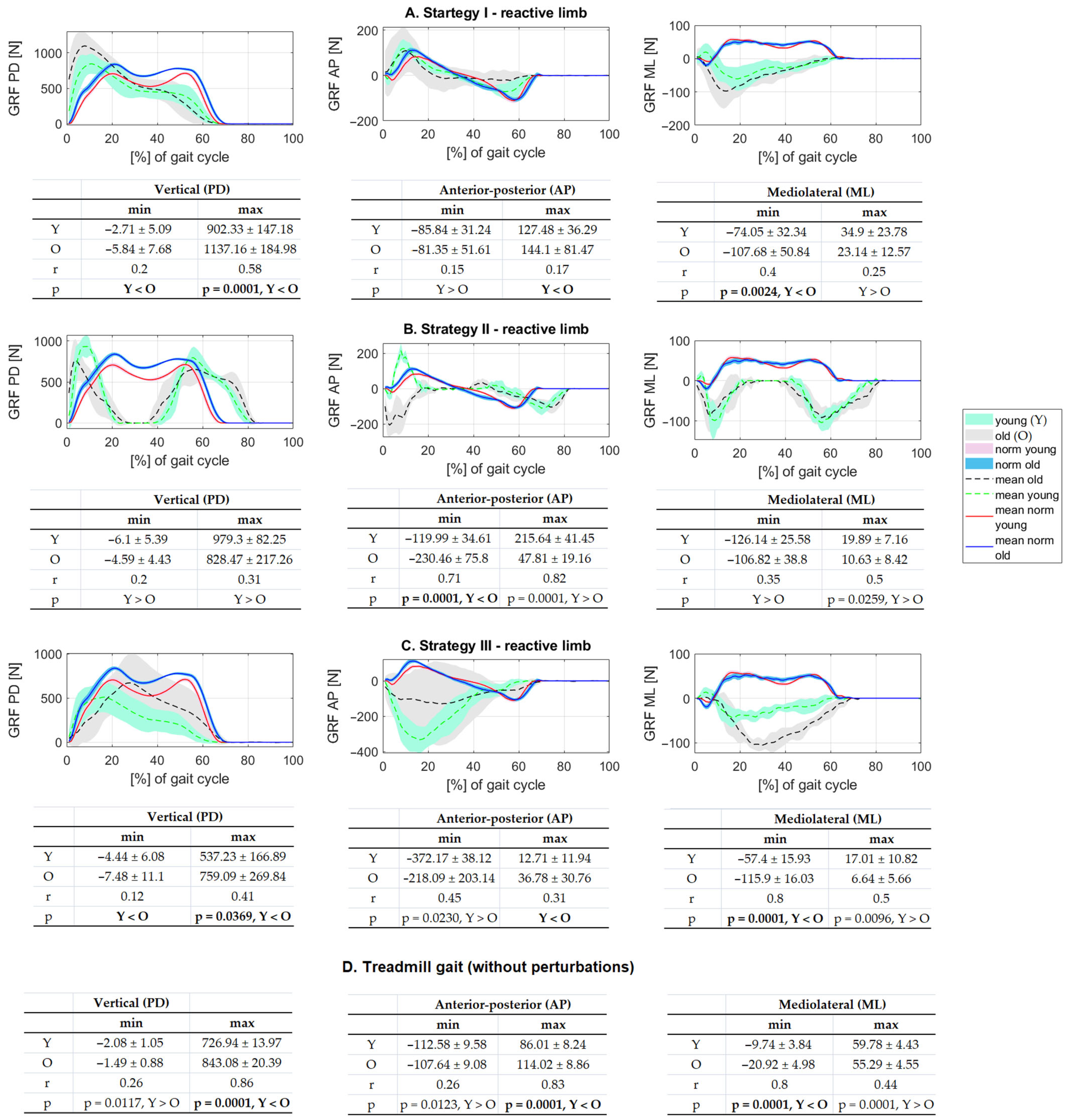
3.3.1. Ground Reaction Forces
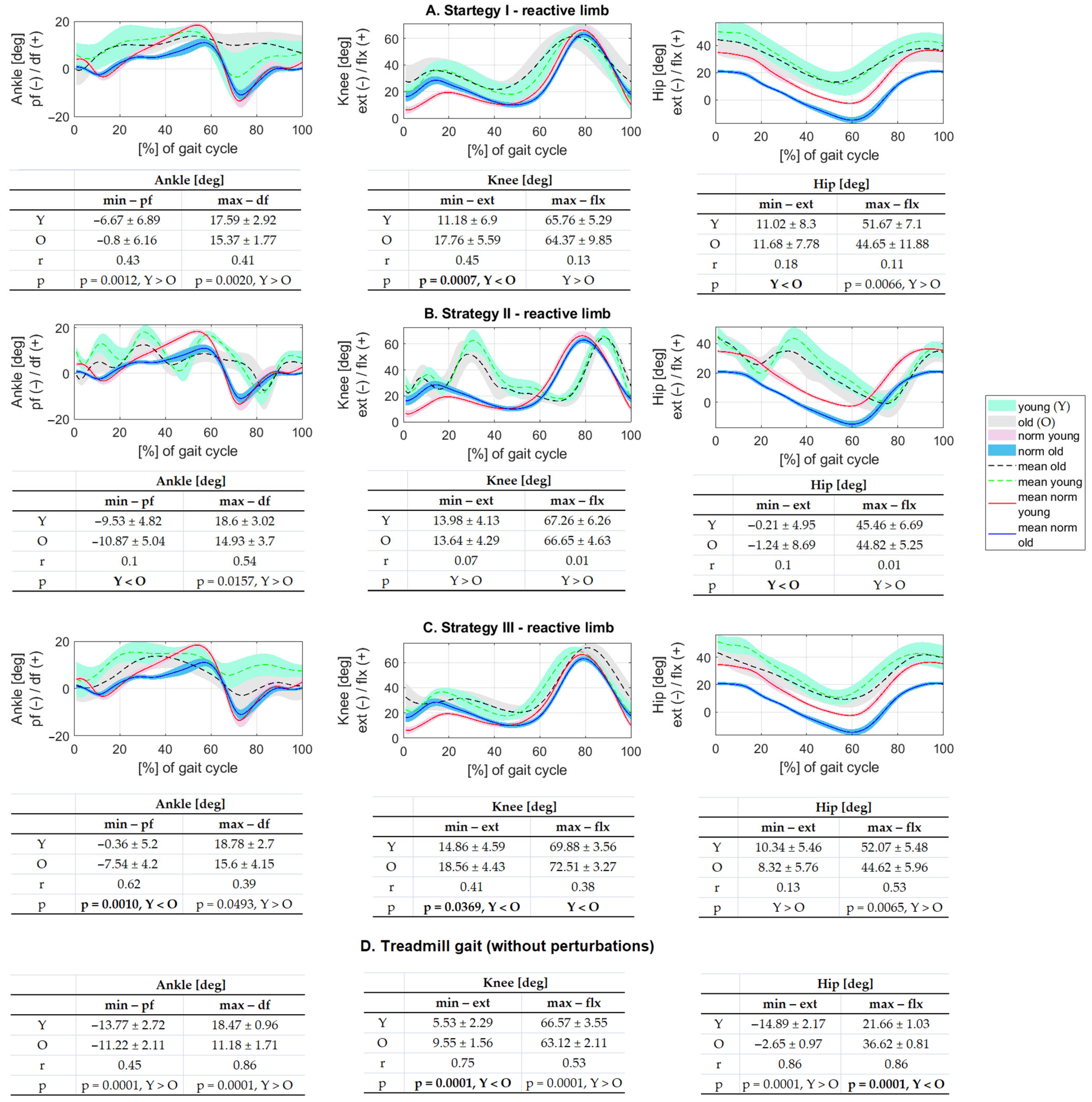
3.3.2. Kinematic Parameters
3.3.3. Kinetic Parameters
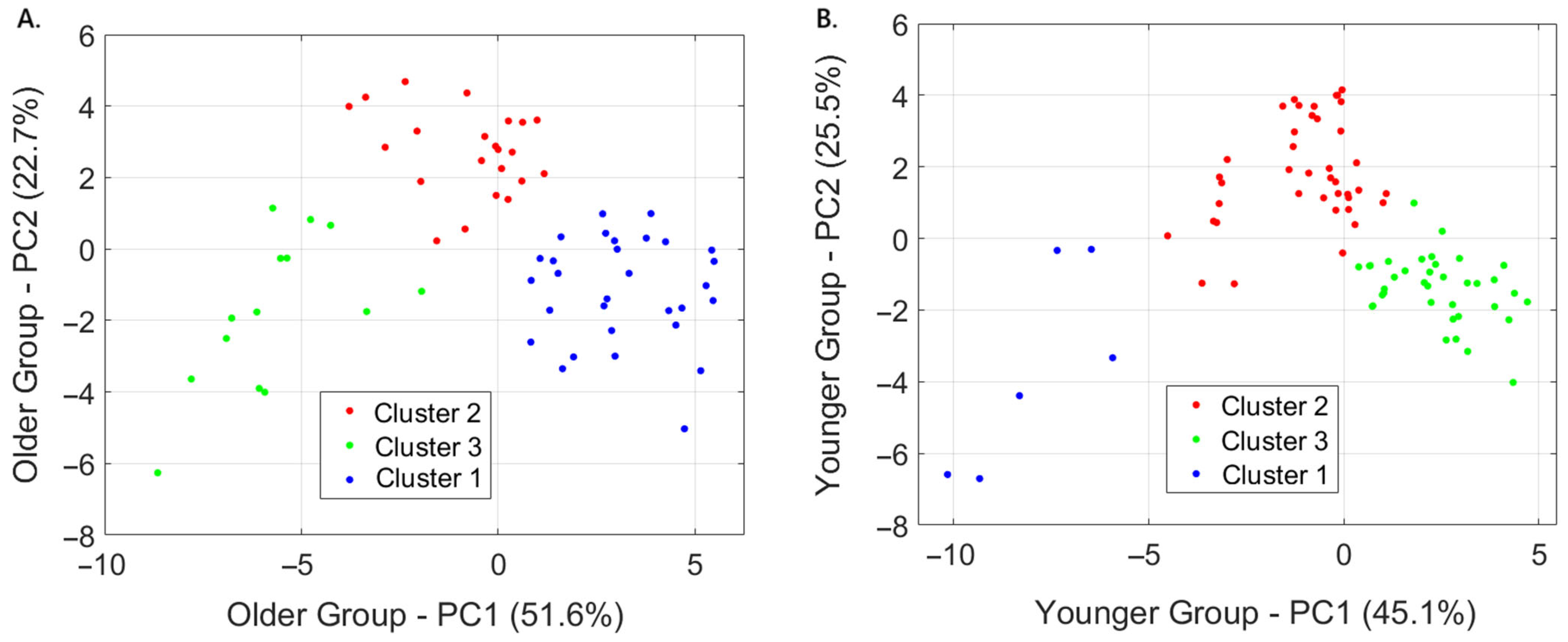
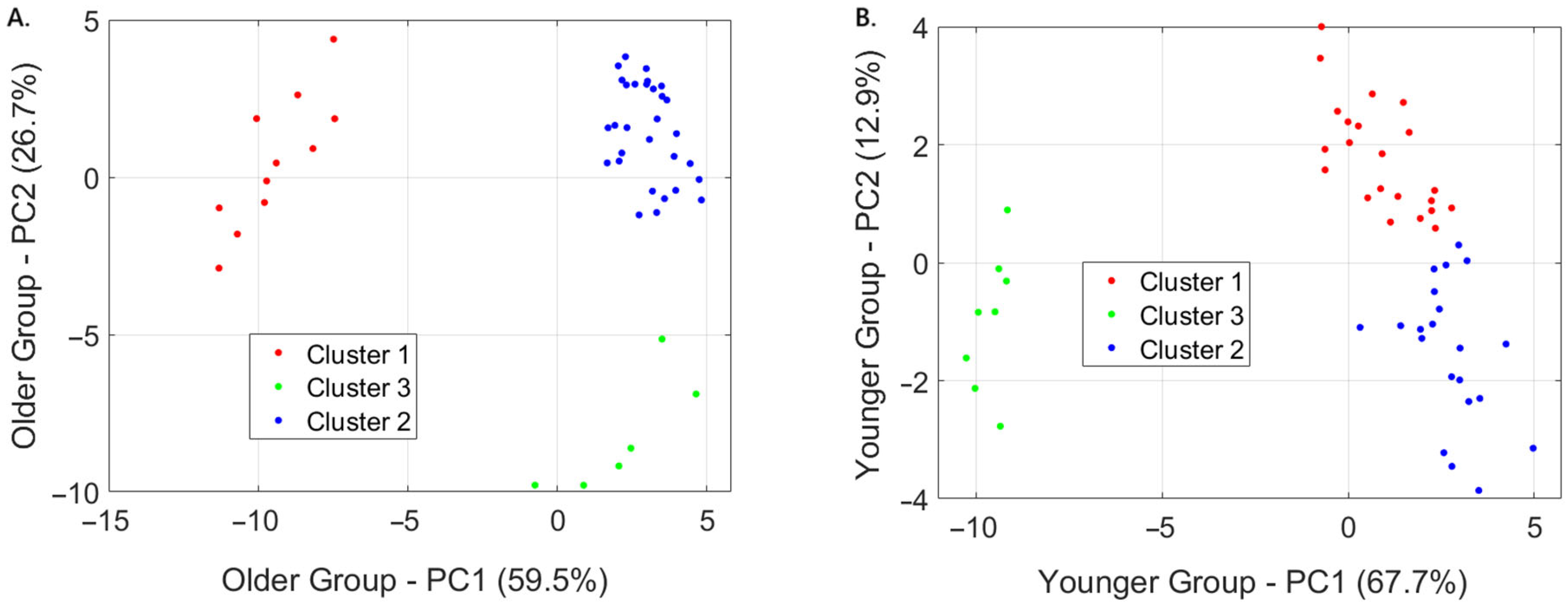
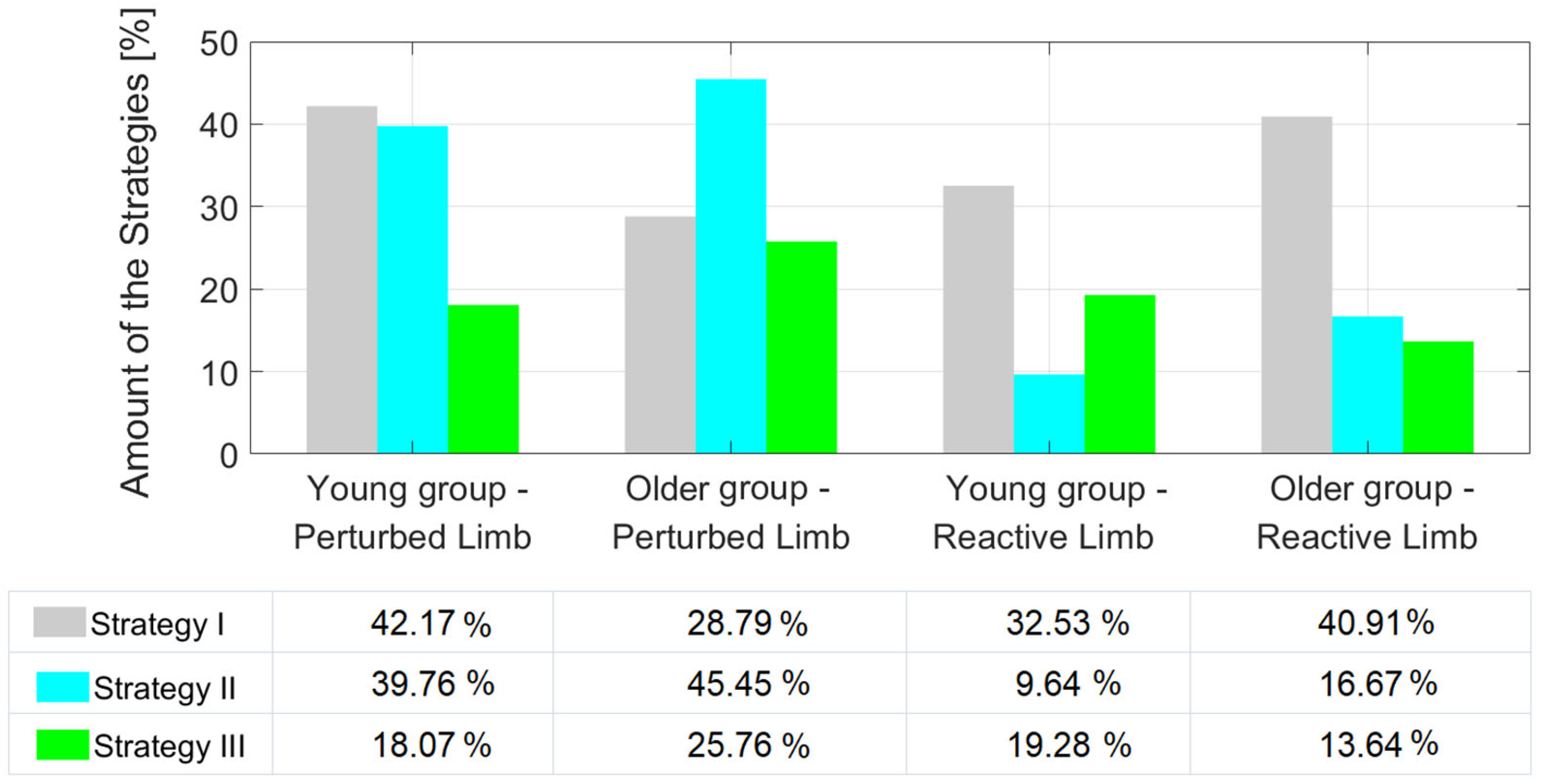
3.4. Amount of Strategies in Studied Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Borkowski, R.; Błażkiewicz, M. Postural reactions to external mediolateral perturbations: A review. Appl. Sci. 2023, 13, 1696. [Google Scholar] [CrossRef]
- Hadamus, A.; Gulatowska, M.; Ferenc, A.; Shahnazaryan, K.; Brzuszkiewicz-Kuźmicka, G.; Błażkiewicz, M. Influence of leg dominance on the symmetry in body balance measurements. Phys. Act. Rev. 2025, 13, 88–96. [Google Scholar] [CrossRef]
- Rogers, M.W.; Mille, M.-L. Chapter 5—Balance perturbations. In Handbook of Clinical Neurology; Day, B.L., Lord, S.R., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; Volume 159, pp. 85–105. [Google Scholar]
- Amboni, M.; Barone, P.; Hausdorff, J.M. Cognitive contributions to gait and falls: Evidence and implications. Mov. Disord. 2013, 28, 1520–1533. [Google Scholar] [CrossRef] [PubMed]
- Taylor, Z.; Walsh, G.S.; Hawkins, H.; Inacio, M.; Esser, P. Perturbations during Gait: A Systematic Review of Methodologies and Outcomes. Sensors 2022, 22, 5927. [Google Scholar] [CrossRef]
- Chodkowska, K.; Borkowski, R.; Błażkiewicz, M. Perturbations During Gait on a Split-Belt Treadmill: A Scoping Review. Appl. Sci. 2024, 14, 9852. [Google Scholar] [CrossRef]
- Sakthivadivel, V.; Geetha, J.; Gaur, A.; Kaliappan, A. Performance-Oriented Mobility Assessment test and Timed Up and Go test as predictors of falls in the elderly—A cross-sectional study. J. Fam. Med. Prim. Care 2022, 11, 7294–7298. [Google Scholar] [CrossRef]
- Talbot, L.A.; Musiol, R.J.; Witham, E.K.; Metter, E.J. Falls in young, middle-aged and older community dwelling adults: Perceived cause, environmental factors and injury. BMC Public Health 2005, 5, 86. [Google Scholar] [CrossRef]
- Rice, P.E.; Needle, A.R.; Leicht, Z.S.; Zwetsloot, K.A.; McBride, J.M. Bone health, muscle properties and stretch-shortening cycle function of young and elderly males. J. Musculoskelet. Neuronal Interact. 2019, 19, 389–395. [Google Scholar]
- Xing, L.; Bao, Y.; Wang, B.; Shi, M.; Wei, Y.; Huang, X.; Dai, Y.; Shi, H.; Gai, X.; Luo, Q.; et al. Falls caused by balance disorders in the elderly with multiple systems involved: Pathogenic mechanisms and treatment strategies. Front. Neurol. 2023, 14, 1128092. [Google Scholar] [CrossRef]
- Rasooli, A.; Adab, H.Z.; Van Ruitenbeek, P.; Weerasekera, A.; Chalavi, S.; Cuypers, K.; Levin, O.; Dhollander, T.; Peeters, R.; Sunaert, S.; et al. White matter and neurochemical mechanisms underlying age-related differences in motor processing speed. iScience 2023, 26, 106794. [Google Scholar] [CrossRef]
- Bednarczuk, G. Changes in balance and fall risk in female members of the Third Age University aged 60 and older. Adv. Rehabil. 2020, 34, 15–21. [Google Scholar] [CrossRef]
- Bobowik, P.; Wiszomirska, I. Diagnostic dependence of muscle strength measurements and the risk of falls in the elderly. International journal of rehabilitation research. Internationale Zeitschrift fur Rehabilitationsforschung. Int. J. Rehabil. Res. 2020, 43, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Hortobágyi, T.; Rider, P.; Gruber, A.H.; DeVita, P. Age and muscle strength mediate the age-related biomechanical plasticity of gait. Eur. J. Appl. Physiol. 2016, 116, 805–814. [Google Scholar] [CrossRef] [PubMed]
- Franz, J.R. The Age-Associated Reduction in Propulsive Power Generation in Walking. Exerc. Sport Sci. Rev. 2016, 44, 129–136. [Google Scholar] [CrossRef]
- Ahsan, M.; Feroz, M.A.; Alzahrani, A. Impact of a pre-competition aerobic and anaerobic training on the maximal aerobic capacity, anaerobic power, dynamic balance, and visual-motor coordination of rugby and soccer players. Phys. Act. Rev. 2023, 11, 99–111. [Google Scholar] [CrossRef]
- Tideiksaar, R. Reducing the risk of falls and injury in older persons: Contribution of a falls and immobility clinic. L’Année Gérontologique (Ed. Française) 1996, 60, 163–182. [Google Scholar]
- Larsen, E.R.; Mosekilde, L.; Foldspang, A. Correlates of falling during 24 h among elderly Danish community residents. Prev. Med. 2004, 39, 389–398. [Google Scholar] [CrossRef]
- Campbell, A.J.; Borrie, M.J.; Spears, G.F.; Jackson, S.L.; Brown, J.S.; Fitzgerald, J.L. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 1990, 19, 136–141. [Google Scholar] [CrossRef]
- Lee, M.; Lee, S.-J.; Robinson, S. How did the COVID-19 pandemic impact the relationship between residential environments and older rural adults’ physical activity levels? Phys. Act. Rev. 2025, 13, 48–61. [Google Scholar] [CrossRef]
- Çelikhisar, H.; Demir, F. The relationship between physical activity and oxidative stress biomarkers in older adults. Phys. Act. Rev. 2023, 11, 34–41. [Google Scholar] [CrossRef]
- Winter, D.A. Human balance and posture control during standing and walking. Gait Posture 1995, 3, 193–214. [Google Scholar] [CrossRef]
- Ren, X.; Lutter, C.; Kebbach, M.; Bruhn, S.; Bader, R.; Tischer, T. Lower extremity joint compensatory effects during the first recovery step following slipping and stumbling perturbations in young and older subjects. BMC Geriatr. 2022, 22, 656. [Google Scholar] [CrossRef] [PubMed]
- Ren, X.; Lutter, C.; Kebbach, M.; Bruhn, S.; Yang, Q.; Bader, R.; Tischer, T. Compensatory Responses During Slip-Induced Perturbation in Patients with Knee Osteoarthritis Compared with Healthy Older Adults: An Increased Risk of Falls? Front. Bioeng. Biotechnol. 2022, 10, 893840. [Google Scholar] [CrossRef] [PubMed]
- Promsri, A.; Longo, A.; Haid, T.; Doix, A.M.; Federolf, P. Leg Dominance as a Risk Factor for Lower-Limb Injuries in Downhill Skiers-A Pilot Study into Possible Mechanisms. Int. J. Environ. Res. Public Health 2019, 16, 3399. [Google Scholar] [CrossRef]
- Zeni, J.A.; Richards, J.G.; Higginson, J.S. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture 2008, 27, 710–714. [Google Scholar] [CrossRef]
- Sloot, L.H.; van den Noort, J.C.; van der Krogt, M.M.; Bruijn, S.M.; Harlaar, J. Can Treadmill Perturbations Evoke Stretch Reflexes in the Calf Muscles? PLoS ONE 2015, 10, e0144815. [Google Scholar] [CrossRef]
- Błażkiewicz, M.; Hadamus, A. Influence of Perturbation’s Type and Location on Treadmill Gait Regularity. Appl. Sci. 2024, 14, 493. [Google Scholar] [CrossRef]
- Feldhege, F.; Richter, K.; Bruhn, S.; Fischer, D.C.; Mittlmeier, T. MATLAB-based tools for automated processing of motion tracking data provided by the GRAIL. Gait Posture 2021, 90, 422–426. [Google Scholar] [CrossRef]
- Pataky, T.C. Generalized n-dimensional biomechanical field analysis using statistical parametric mapping. J. Biomech. 2010, 43, 1976–1982. [Google Scholar] [CrossRef]
- Adler, R.J.; Taylor, J.E. Random Fields and Geometry; Springer: Berlin/Heidelberg, Germany, 2007; Volume 80. [Google Scholar]
- Rosnow, R.L. Effect sizes for experimenting psychologists. Can. J. Exp. Psychol.=Rev. Can. Psychol. Exp. 2003, 57, 221–237. [Google Scholar] [CrossRef]
- Berg, W.P.; Alessio, H.M.; Mills, E.M.; Tong, C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing 1997, 26, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Lurie, J.D.; Zagaria, A.B.; Ellis, L.; Pidgeon, D.; Gill-Body, K.M.; Burke, C.; Armbrust, K.; Cass, S.; Spratt, K.F.; McDonough, C.M. Surface Perturbation Training to Prevent Falls in Older Adults: A Highly Pragmatic, Randomized Controlled Trial. Phys. Ther. 2020, 100, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.R.; Leclercq, S.; Lockhart, T.E.; Haslam, R. State of science: Occupational slips, trips and falls on the same level. Ergonomics 2016, 59, 861–883. [Google Scholar] [CrossRef] [PubMed]
- Grabiner, M.D.; Donovan, S.; Bareither, M.L.; Marone, J.R.; Hamstra-Wright, K.; Gatts, S.; Troy, K.L. Trunk kinematics and fall risk of older adults: Translating biomechanical results to the clinic. J. Electromyogr. Kinesiol. 2008, 18, 197–204. [Google Scholar] [CrossRef]
- Allum, J.H.; Carpenter, M.G.; Honegger, F.; Adkin, A.L.; Bloem, B.R. Age-dependent variations in the directional sensitivity of balance corrections and compensatory arm movements in man. J. Physiol. 2002, 542, 643–663. [Google Scholar] [CrossRef]
- El-Din Mahmoud, L.S.; Aly, S.M.; Shafeek, M.M.; Battesha, H.H.M. Effect of CoDuSe and step square exercises on risk of fall in multiple sclerosis: A randomized controlled trial. Phys. Act. Rev. 2022, 10, 2022. [Google Scholar] [CrossRef]
- McCrum, C.; Karamanidis, K.; Willems, P.; Zijlstra, W.; Meijer, K. Retention, savings and interlimb transfer of reactive gait adaptations in humans following unexpected perturbations. Commun. Biol. 2018, 1, 230. [Google Scholar] [CrossRef]
- Song, P.Y.H.; Sturnieks, D.L.; Davis, M.K.; Lord, S.R.; Okubo, Y. Perturbation-Based Balance Training Using Repeated Trips on a Walkway vs. Belt Accelerations on a Treadmill: A Cross-Over Randomised Controlled Trial in Community-Dwelling Older Adults. Front. Sports Act. Living 2021, 3, 702320. [Google Scholar] [CrossRef]
- Sessoms, P.H.; Wyatt, M.; Grabiner, M.; Collins, J.D.; Kingsbury, T.; Thesing, N.; Kaufman, K. Method for evoking a trip-like response using a treadmill-based perturbation during locomotion. J. Biomech. 2014, 47, 277–280. [Google Scholar] [CrossRef]
- McCrum, C.; Gerards, M.H.G.; Karamanidis, K.; Zijlstra, W.; Meijer, K. A systematic review of gait perturbation paradigms for improving reactive stepping responses and falls risk among healthy older adults. Eur. Rev. Aging Phys. Act. 2017, 14, 3. [Google Scholar] [CrossRef]
- Epro, G.; McCrum, C.; Mierau, A.; Leyendecker, M.; Brüggemann, G.P.; Karamanidis, K. Effects of triceps surae muscle strength and tendon stiffness on the reactive dynamic stability and adaptability of older female adults during perturbed walking. J. Appl. Physiol. 2018, 124, 1541–1549. [Google Scholar] [CrossRef] [PubMed]
- King, S.T.; Eveld, M.E.; Martínez, A.; Zelik, K.E.; Goldfarb, M. A novel system for introducing precisely-controlled, unanticipated gait perturbations for the study of stumble recovery. J. Neuroeng. Rehabil. 2019, 16, 69. [Google Scholar] [CrossRef] [PubMed]
- Roeles, S.; Rowe, P.J.; Bruijn, S.M.; Childs, C.R.; Tarfali, G.D.; Steenbrink, F.; Pijnappels, M. Gait stability in response to platform, belt, and sensory perturbations in young and older adults. Med. Biol. Eng. Comput. 2018, 56, 2325–2335. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.C.; Kim, C.S.; Seo, K.H. The Body’s Compensatory Responses to Unpredictable Trip and Slip Perturbations Induced by a Programmable Split-Belt Treadmill. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 1389–1396. [Google Scholar] [CrossRef]
- Ciunelis, K.; Borkowski, R.; Błażkiewicz, M. The Impact of Induced Acceleration Perturbations in Selected Phases of the Gait Cycle on Kinematic and Kinetic Parameters. Appl. Sci. 2024, 14, 4849. [Google Scholar] [CrossRef]
- Ferreira, R.N.; Ribeiro, N.F.; Figueiredo, J.; Santos, C.P. Provoking Artificial Slips and Trips towards Perturbation-Based Balance Training: A Narrative Review. Sensors 2022, 22, 9254. [Google Scholar] [CrossRef]
- Downey, R.J.; Richer, N.; Gupta, R.; Liu, C.; Pliner, E.M.; Roy, A.; Hwang, J.; Clark, D.J.; Hass, C.J.; Manini, T.M.; et al. Uneven terrain treadmill walking in younger and older adults. PLoS ONE 2022, 17, e0278646. [Google Scholar] [CrossRef]
- Schmitt, A.C.; Baudendistel, S.T.; Lipat, A.L.; White, T.A.; Raffegeau, T.E.; Hass, C.J. Walking indoors, outdoors, and on a treadmill: Gait differences in healthy young and older adults. Gait Posture 2021, 90, 468–474. [Google Scholar] [CrossRef]
- Monaco, V.; Macrì, G.; Dario, P.; Micera, S. Kinematics and kinetics analysis of gait on treadmill: A comparison between the performance of young and elderly people. Gait Posture 2006, 24, S1–S2. [Google Scholar] [CrossRef]
- Golyski, P.R.; Vazquez, E.; Leestma, J.K.; Sawicki, G.S. Onset timing of treadmill belt perturbations influences stability during walking. J. Biomech. 2022, 130, 110800. [Google Scholar] [CrossRef]
- Madehkhaksar, F.; Klenk, J.; Sczuka, K.; Gordt, K.; Melzer, I.; Schwenk, M. The effects of unexpected mechanical perturbations during treadmill walking on spatiotemporal gait parameters, and the dynamic stability measures by which to quantify postural response. PLoS ONE 2018, 13, e0195902. [Google Scholar] [CrossRef] [PubMed]
- Onushko, T.; Boerger, T.; Van Dehy, J.; Schmit, B.D. Dynamic stability and stepping strategies of young healthy adults walking on an oscillating treadmill. PLoS ONE 2019, 14, e0212207. [Google Scholar] [CrossRef] [PubMed]


| Groups | Age [Years] | Body Weight [kg] | Body Height [cm] |
|---|---|---|---|
| Young (Y: n = 21) | 21.38 ± 1.32 | 61.38 ± 6.48 | 165.9 ± 4.53 |
| Old (O: n = 21) | 67.75 ± 4.7 | 73.36 ± 11.06 | 161.5 ± 5.18 |
| Ankle [deg] | Knee [deg] | Hip [deg] | ||||
|---|---|---|---|---|---|---|
| min − pf | max − df | min − ext | max − flx | min − ext | max − flx | |
| Young | ||||||
| I–n | 2.66 (min) | −3.02 (min) | 4.32 (mean) | −2.47 (min) | 5.78 (max) | 4.44 (min) |
| II–n | −6.1 (mean) | −4.64 (mean) | 4.67 (max) | 12.72 (mean) | 3.21 (min) | 11.61 (mean) |
| III–n | −9.37 (max) | −5.48 (max) | 1.64 (min) | 14.65 (max) | 3.46 (mean) | 12.6 (max) |
| Elderly | ||||||
| I–n | 8.66 (max) | 3.53 (min) | 6.2 (mean) | 4.46 (min) | 19.28 (max) | 15.82 (min) |
| II–n | 2.38 (mean) | 5.18 (mean) | 4.38 (min) | 10.42 (mean) | 18.32 (mean) | 26.86 (max) |
| III–n | −0.45 (min) | 6.12 (max) | 7.27 (max) | 19.42 (max) | 14.46 (min) | 23.3 (mean) |
| Ankle [Nm/kg] | Knee [Nm/kg] | Hip [Nm/kg] | ||||
|---|---|---|---|---|---|---|
| min − df | max − pf | min − flx | min − df | max − pf | min − flx | |
| Young | ||||||
| I–n | 0.01 (min) | −0.03 (min) | −0.29 (mean) | 0.79 (max) | −0.03 (min) | 0.62 (mean) |
| II–n | −0.12 (max) | 0.39 (mean) | −0.29 (mean) | 0.42 (mean) | −1.22 (max) | 0.68 (max) |
| III–n | −0.05 (mean) | 0.58 (max) | −0.25 (min) | 0.2 (min) | −0.8 (mean) | 0.49 (min) |
| Elderly | ||||||
| I–n | 0 (min) | −0.14 (min) | −0.22 (min) | 0.47 (max) | 0 (min) | 0.51 (mean) |
| II–n | −0.19 (mean) | 0.24 (mean) | −0.25 (mean) | 0.23 (min) | −0.55 (mean) | 0.47 (min) |
| III–n | −0.19 (mean) | 0.58 (max) | −0.33 (max) | 0.3 (mean) | −0.73 (max) | 0.65 (max) |
| Ankle [deg] | Knee [deg] | Hip [deg] | ||||
|---|---|---|---|---|---|---|
| min − pf | max − df | min − ext | max − flx | min − ext | max − flx | |
| Young | ||||||
| I–n | 7.1 (mean) | −0.88 (max) | 5.65 (min) | −0.81 (mean) | 25.91 (max) | 30.01 (mean) |
| II–n | 4.24 (min) | 0.13 (min) | 8.45 (mean) | 0.69 (min) | 14.68 (min) | 23.8 (min) |
| III–n | 13.41 (max) | 0.31 (mean) | 9.33 (max) | 3.31 (max) | 25.23 (mean) | 30.41 (max) |
| Elderly | ||||||
| I–n | 10.42 (max) | 4.19 (mean) | 8.21 (mean) | 1.25 (min) | 14.33 (max) | 8.03 (mean) |
| II–n | 0.35 (min) | 3.75 (min) | 4.09 (min) | 3.53 (mean) | 1.41 (min) | 8.2 (max) |
| III–n | 3.68 (mean) | 4.42 (max) | 9.01 (max) | 9.39 (max) | 10.97 (mean) | 8 (min) |
| Ankle [Nm/kg] | Knee [Nm/kg] | Hip [Nm/kg] | ||||
|---|---|---|---|---|---|---|
| min − df | max − pf | min − flx | min − df | max − pf | min − flx | |
| Young | ||||||
| I–n | −0.18 (mean) | 0.13 (min) | −0.29 (min) | 0.89 (max) | −0.24 (min) | 1.13 (min) |
| II–n | −0.05 (min) | 0.73 (max) | −0.44 (max) | 0.7 (mean) | −0.67 (max) | 1.29 (mean) |
| III–n | −0.23 (max) | 0.14 (mean) | −0.38 (mean) | 0.65 (min) | −0.53 (mean) | 1.44 (max) |
| Elderly | ||||||
| I–n | −0.1 (mean) | 0.12 (mean) | −0.28 (max) | 0.19 (mean) | −0.26 (mean) | 1.28 (max) |
| II–n | −0.22 (max) | 0.48 (max) | −0.27 (mean) | 0.57 (max) | −0.44 (max) | 1.16 (mean) |
| III–n | 0.04 (min) | −0.08 (min) | −0.08 (min) | 0.02 (min) | −0.09 (min) | 0.23 (min) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chodkowska, K.; Błażkiewicz, M.; Mroczkowski, A.; Wąsik, J. Age-Related Compensatory Gait Strategies During Induced Perturbations in the Pre-Swing Gait Phase: A Kinematic and Kinetic Analysis. Appl. Sci. 2025, 15, 6885. https://doi.org/10.3390/app15126885
Chodkowska K, Błażkiewicz M, Mroczkowski A, Wąsik J. Age-Related Compensatory Gait Strategies During Induced Perturbations in the Pre-Swing Gait Phase: A Kinematic and Kinetic Analysis. Applied Sciences. 2025; 15(12):6885. https://doi.org/10.3390/app15126885
Chicago/Turabian StyleChodkowska, Katarzyna, Michalina Błażkiewicz, Andrzej Mroczkowski, and Jacek Wąsik. 2025. "Age-Related Compensatory Gait Strategies During Induced Perturbations in the Pre-Swing Gait Phase: A Kinematic and Kinetic Analysis" Applied Sciences 15, no. 12: 6885. https://doi.org/10.3390/app15126885
APA StyleChodkowska, K., Błażkiewicz, M., Mroczkowski, A., & Wąsik, J. (2025). Age-Related Compensatory Gait Strategies During Induced Perturbations in the Pre-Swing Gait Phase: A Kinematic and Kinetic Analysis. Applied Sciences, 15(12), 6885. https://doi.org/10.3390/app15126885







