Efficiency and Validity of the AI-Based rGMFM-66 in Assessing Gross Motor Function in Children with Cerebral Palsy
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Implementation
2.3. Statistical Analyses
3. Results
3.1. Study Population
3.2. Practicability of the rGMFM-66
- (a)
- Boxplot illustrating the application times for the GMFM-66 and rGMFM-66. The rGMFM-66 required significantly less time for administration compared to the GMFM-66 (p < 0.001).
- (b)
- Scatter plot showing the correlation between GMFM-66 and rGMFM-66 scores. Each point represents one participant. The dashed line represents the line of equality, indicating strong agreement between both measurements.
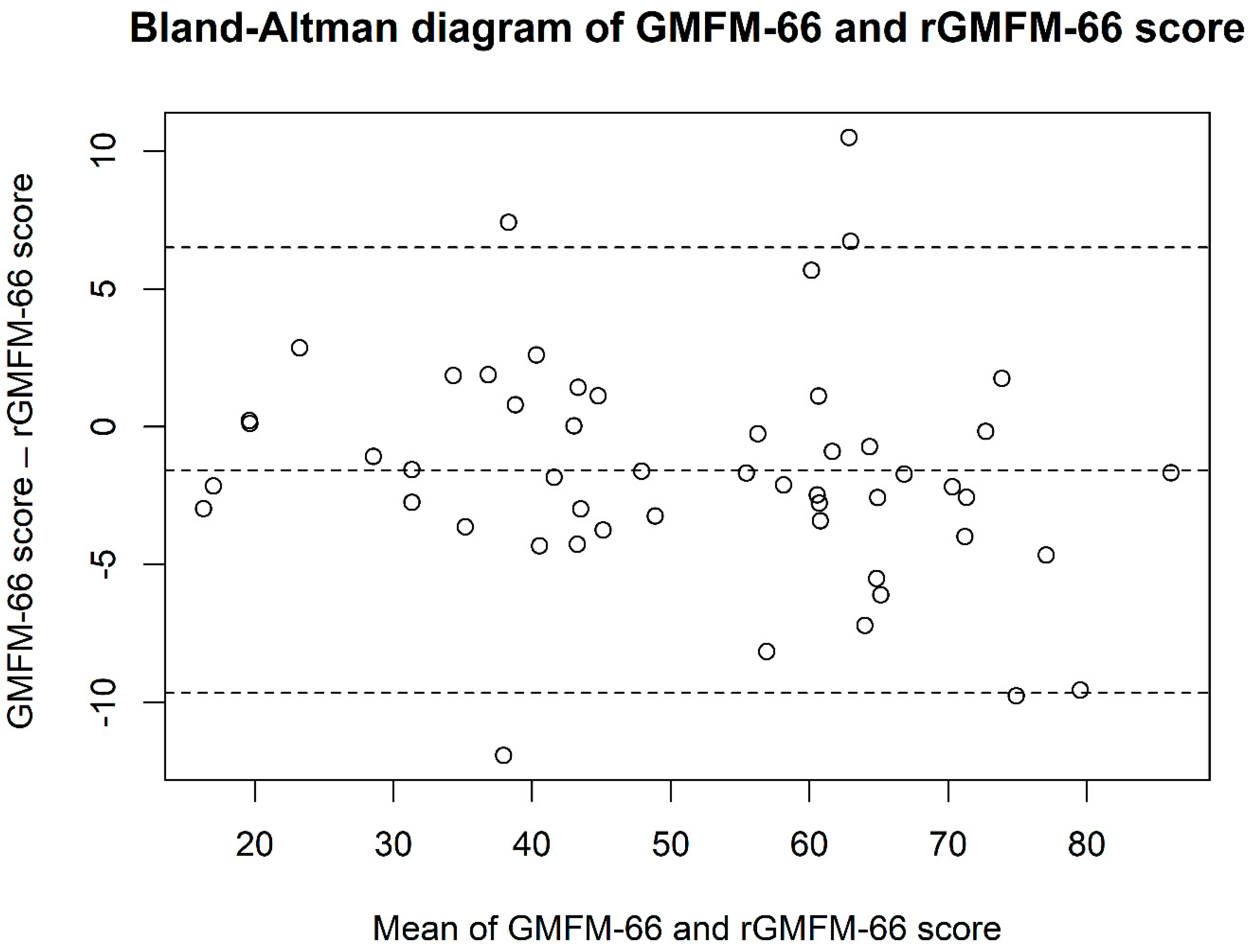
3.3. Criterion Validity of the rGMFM-66 Compared to the GMFM-66
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AI | Artificial Intelligence |
| CP | Cerebral Palsy |
| GMFM-66 | Gross Motor Functional Measurement-66 |
| ICC | Intraclass correlation coefficients |
| rGMFM-66 | reduced Gross Motor Functional Measurement-66 |
| WBV | Whole Body Vibration Training |
References
- Rosenbaum, P. Cerebral palsy: Is the concept still viable? Dev. Med. Child Neurol. 2017, 59, 564. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, W.; Stuhlfelder, U. Update Pädiatrie (2): Infantile Zerebralparese—Die häufigste Ursache für das Auftreten körperlicher Behinderungen im Kindesalter. VPT Mag. 2022, 8, 20–21. [Google Scholar] [CrossRef]
- Blauw-Hospers, C.H.; Hadders-Algra, M. A systematic review of the effects of early intervention on motor development. Dev. Med. Child Neurol. 2005, 47, 421–432. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.D. Reframing Cerebral Palsy as a Lifelong Physical Disability. N. Engl. J. Med. 2024, 391, 1668–1670. [Google Scholar] [CrossRef]
- Strassburg, H.M. (Ed.) Behandlungskonzept bei Kindern mit infantiler Zerebralparese. In Leitlinien Kinder- und Jugendmedizin; Elsevier: Amsterdam, The Netherlands, 2015; pp. R5.1–R5.6. [Google Scholar] [CrossRef]
- Russell, D.J.; Avery, L.M.; Rosenbaum, P.L.; Raina, P.S.; Walter, S.D.; Palisano, R.J. Improved Scaling of the Gross Motor Function Measure for Children with Cerebral Palsy: Evidence of Reliability and Validity. Phys. Ther. 2000, 80, 873–885. [Google Scholar] [CrossRef]
- Gross Motor Function Measure-66|RehabMeasures Database. 2017. Available online: https://www.sralab.org/rehabilitation-measures/gross-motor-function-measure-66 (accessed on 13 January 2025).
- Alotaibi, M.; Long, T.; Kennedy, E.; Bavishi, S. The efficacy of GMFM-88 and GMFM-66 to detect changes in gross motor function in children with cerebral palsy (CP): A literature review. Disabil. Rehabil. 2014, 36, 617–627. [Google Scholar] [CrossRef]
- van der Veen, S.; van der Leeden, M.; Geleijn, E.; Vossen, P.; Meskers, C.G.M.; Widdershoven, G.A.M. Artificial intelligence to improve rehabilitation care for children with developmental conditions: Some ethical considerations. Dev. Med. Child Neurol. 2023, 65, 12–13. [Google Scholar] [CrossRef]
- Ismail, L.; Materwala, H.; Karduck, A.P.; Adem, A. Requirements of Health Data Management Systems for Biomedical Care and Research: Scoping Review. J. Med. Internet Res. 2020, 22, e17508. [Google Scholar] [CrossRef]
- Puce, L.; Pallecchi, I.; Chamari, K.; Marinelli, L.; Innocenti, T.; Pedrini, R.; Mori, L.; Trompetto, C. Systematic Review of Fatigue in Individuals with Cerebral Palsy. Front. Hum. Neurosci. 2021, 15, 598800. [Google Scholar] [CrossRef]
- Shih, S.T.; Tonmukayakul, U.; Imms, C.; Reddihough, D.; Graham, H.K.; Cox, L.; Carter, R. Economic evaluation and cost of interventions for cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2018, 60, 543–558. [Google Scholar] [CrossRef]
- Duran, I.; Stark, C.; Saglam, A.; Semmelweis, A.; Lioba Wunram, H.; Spiess, K.; Schoenau, E. Artificial intelligence to improve efficiency of administration of gross motor function assessment in children with cerebral palsy. Dev. Med. Child Neurol. 2022, 64, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. 2007, 49, 8–14. [Google Scholar] [CrossRef]
- Han, O.; Tan, H.W.; Julious, S.; Sutton, L.; Jacques, R.; Lee, E.; Lewis, J.; Walters, S. A descriptive study of samples sizes used in agreement studies published in the PubMed repository. BMC Med. Res. Methodol. 2022, 22, 242. [Google Scholar] [CrossRef] [PubMed]
- Bonett, D.G. Sample size requirements for estimating intraclass correlations with desired precision. Stat. Med. 2002, 21, 1331–1335. [Google Scholar] [CrossRef]
- Schafmeyer, L.; Losch, H.; Bossier, C.; Lanz, I.; Wunram, H.L.; Schoenau, E.; Duran, I. Using artificial intelligence-based technologies to detect clinically relevant changes of gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 2023, 66, 226–232. [Google Scholar] [CrossRef]
- Berweck, S. Anhang: GMAE-Computerprogramm für die GMFM-66. In GMFM und GMFCS—Messung und Klassifikation Motorischer Funktionen; CD-ROM: The Gross Motor Function, Estimator; Russel, D.J., Rosenbaum, P.L., Avery, L.M., Lane, M., Eds.; Huber: Bern, Switzerland, 2006. [Google Scholar]
- McGraw, K.O.; Wong, S.P. Forming inferences about some intraclass correlation coefficients. Psychol. Methods 1996, 1, 30–46. [Google Scholar] [CrossRef]
- Surveillance of Cerebral Palsy in Europe. Surveillance of cerebral palsy in Europe: A collaboration of cerebral palsy surveys and registers. Surveillance of Cerebral Palsy in Europe (SCPE). Dev. Med. Child Neurol. 2000, 42, 816–824. [Google Scholar] [CrossRef]
- Wang, H.-Y.; Yang, Y.H. Evaluating the Responsiveness of 2 Versions of the Gross Motor Function Measure for Children with Cerebral Palsy. Arch. Phys. Med. Rehabil. 2006, 87, 51–56. [Google Scholar] [CrossRef]
- Hanna, S.; Russell, D.; Bartlett, D.; Kertoy, M.; Rosenbaum, P.; Wynn, K. Measurement Practices in Pediatric Rehabilitation. Phys. Occup. Ther. Pediatr. 2007, 27, 25–42. [Google Scholar] [CrossRef]
- Kelly, C.J.; Brown, A.P.Y.; Taylor, J.A. Artificial Intelligence in Pediatrics. In Artificial Intelligence in Medicine; Lidströmer, N., Ashrafian, H., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 1029–1045. [Google Scholar] [CrossRef]
- Cai, X.; Qian, G.; Cai, S.; Wang, F.; Da, Y.; Ossowski, Z. The effect of whole-body vibration on lower extremity function in children with cerebral palsy: A meta-analysis. PLoS ONE 2023, 18, e0282604. [Google Scholar] [CrossRef]
- Adaikina, A.; Hofman, P.L.; Gusso, S. The effect of side-alternating vibration therapy on mobility and health outcomes in young children with mild to moderate cerebral palsy: Design and rationale for the randomized controlled study. BMC Pediatr. 2020, 20, 508. [Google Scholar] [CrossRef] [PubMed]
- Sellier, E.; Platt, M.J.; Andersen, G.L.; Krägeloh-Mann, I.; De La Cruz, J.; Cans, C.; Surveillance of Cerebral Palsy Network. Decreasing prevalence in cerebral palsy: A multi-site European population-based study, 1980 to 2003. Dev. Med. Child Neurol. 2016, 58, 85–92. [Google Scholar] [CrossRef]
- Schmitt, Y.S.; Hoffman, H.G.; Blough, D.K.; Patterson, D.R.; Jensen, M.P.; Soltani, M.; Carrougher, G.J.; Nakamura, D.; Sharar, S.R. A Randomized, Controlled Trial of Immersive Virtual Reality Analgesia during Physical Therapy for Pediatric Burn Injuries. Burns 2011, 37, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Pitre, T.; Kirsh, S.; Jassal, T.; Anderson, M.; Padoan, A.; Xiang, A.; Mah, J.; Zeraatkar, D. The impact of blinding on trial results: A systematic review and meta-analysis. Cochrane Evid. Synth. Methods 2023, 1, e12015. [Google Scholar] [CrossRef]
- Adeniyi, A.; Adeniyi, S. Revolutionizing Healthcare: The Impact of Machine learning and Artificial intelligence. E-Health Telecommun. Syst. Netw. 2024, 13, 87–91. [Google Scholar] [CrossRef]
- Avery, L.M.; Russell, D.J.; Rosenbaum, P.L. Criterion validity of the GMFM-66 item set and the GMFM-66 basal and ceiling approaches for estimating GMFM-66 scores. Dev. Med. Child Neurol. 2013, 55, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Weiner, E.B.; Dankwa-Mullan, I.; Nelson, W.A.; Hassanpour, S. Ethical challenges and evolving strategies in the integration of artificial intelligence into clinical practice. PLoS Digit. Health 2025, 4, e0000810. [Google Scholar] [CrossRef]
- Muralidharan, V.; Burgart, A.; Daneshjou, R.; Rose, S. Recommendations for the use of pediatric data in artificial intelligence and machine learning ACCEPT-AI. npj Digit. Med. 2023, 6, 166. [Google Scholar] [CrossRef]
- Chng, S.Y.; Tern, M.J.W.; Lee, Y.S.; Cheng, L.T.-E.; Kapur, J.; Eriksson, J.G.; Chong, Y.S.; Savulescu, J. Ethical considerations in AI for child health and recommendations for child-centered medical AI. npj Digit. Med. 2025, 8, 152. [Google Scholar] [CrossRef]

| Variable | Value (Mean ± SD) or n (%) |
|---|---|
| Age, years:months | 8:11 (±3:2) |
| Height, cm | 126.0 (±19.6) |
| BMI kg/m2 | 15.3 (±2.7) |
| Females | 14 (26.9%) |
| Males | 38 (73.1%) |
| CP subtype | |
| Bilateral spastic | 37 (71.2%) |
| Unilateral spastic | 7 (13.2%) |
| Dyskinetic | 3 (5.8%) |
| Ataxic | 2 (3.9%) |
| Mixed | 3 (5.8%) |
| GMFCS level | |
| Level I | 4 (7.7%) |
| Level II | 15 (28.8%) |
| Level III | 11 (21.2%) |
| Level IV | 16 (30.8%) |
| Level V | 6 (11.5%) |
| time saving | ||||
| GMFM-66 | rGMFM-66 | p-value | effect size | |
| implementation time, min | 38.5 (13.6) | 17.2 (5.2) | <0.001 | 1.9 |
| score agreement | ||||
| GMFM-66 | rGMFM-66 | p-value | effect size | |
| Score, points | 50.7 (17.4) | 52.2 (18.1) | 0.008 | −0.09 |
| ICC | 0.970 (95%KI 0.942; 0.983) | |||
| Upper limit (97.5%) | Lower Limit (2.5%) | |||
| Bland-Altman statistics | 6.5 (4.5; 8.5) | −9.7 (−11.6; −7.7) | ||
| Criterions | GMFM-66 | rGMFM-66 |
|---|---|---|
| Number of items | 66 items (full test range) | Approximately 34 items on average (selected individually) |
| Administration time | Approx. 30–45 min | Approx. 15–25 min |
| Validity | High; scientifically validated | Strong agreement with GMFM-66; supported by validation studies |
| Target population | Children with CP | Children with CP |
| Standardization | Internationally standardized | Based on retrospective data; prospectively validated |
| Practicality in daily use | Limited due to time requirements | Increased practicality through reduced assessment time |
| Technological support | Manual item selection and scoring by clinicians; score calculated after manual entry into software | AI-assisted item selection; items reviewed by clinicians; assessment via tablet/laptop with automated scoring |
| Application context | Research and clinical practice | Primarily clinical practice with focus on efficiency and reduced burden for the child |
| Ethical considerations | Minimal, as a manual and established procedure | Requires consideration of data protection, transparency, and responsibility in AI use |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steven, S.; Spiess, K.; Schafmeyer, L.; Buggisch, J.; Schoenau, E.; Luedtke, K.; Duran, I. Efficiency and Validity of the AI-Based rGMFM-66 in Assessing Gross Motor Function in Children with Cerebral Palsy. Appl. Sci. 2025, 15, 6527. https://doi.org/10.3390/app15126527
Steven S, Spiess K, Schafmeyer L, Buggisch J, Schoenau E, Luedtke K, Duran I. Efficiency and Validity of the AI-Based rGMFM-66 in Assessing Gross Motor Function in Children with Cerebral Palsy. Applied Sciences. 2025; 15(12):6527. https://doi.org/10.3390/app15126527
Chicago/Turabian StyleSteven, Stefanie, Karoline Spiess, Leonie Schafmeyer, Jonathan Buggisch, Eckhard Schoenau, Kerstin Luedtke, and Ibrahim Duran. 2025. "Efficiency and Validity of the AI-Based rGMFM-66 in Assessing Gross Motor Function in Children with Cerebral Palsy" Applied Sciences 15, no. 12: 6527. https://doi.org/10.3390/app15126527
APA StyleSteven, S., Spiess, K., Schafmeyer, L., Buggisch, J., Schoenau, E., Luedtke, K., & Duran, I. (2025). Efficiency and Validity of the AI-Based rGMFM-66 in Assessing Gross Motor Function in Children with Cerebral Palsy. Applied Sciences, 15(12), 6527. https://doi.org/10.3390/app15126527






