Color Variation in 3D-Printed Orthodontic Aligners as a Compliance Indicator: A Prospective Pilot Study
Abstract
1. Introduction
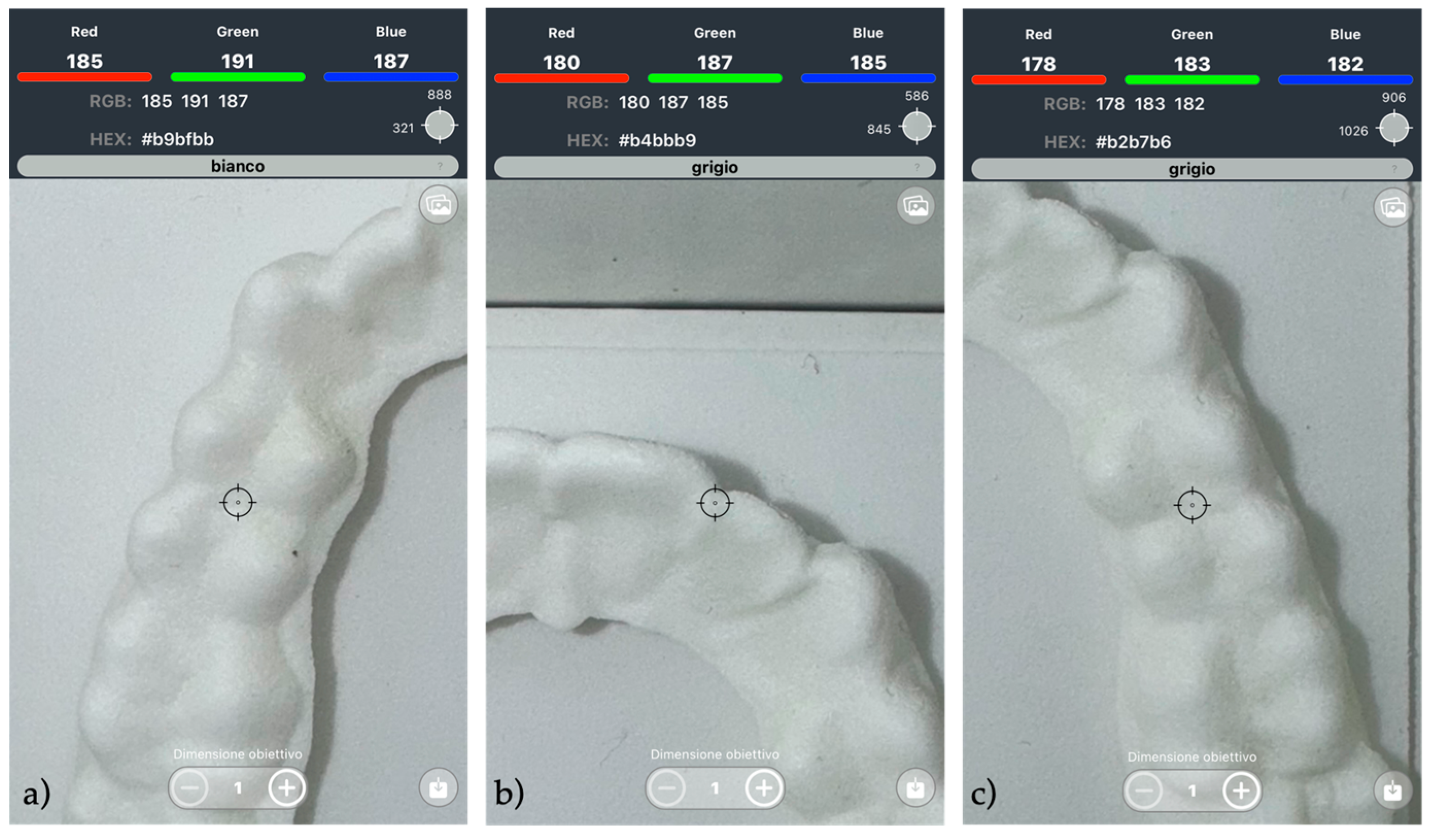
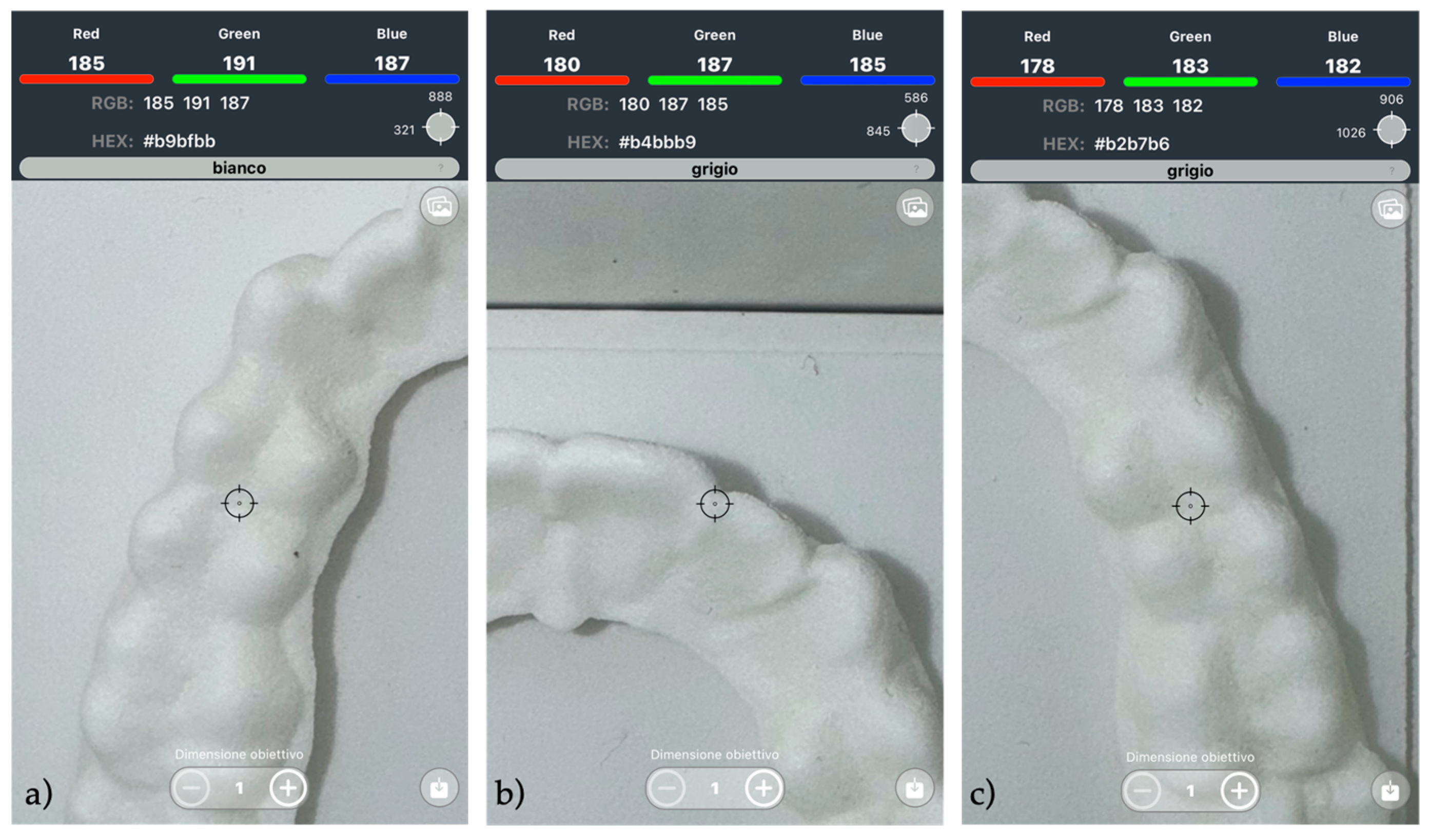
2. Materials and Methods
- First pair: worn for 7 h per day (7 H protocol)
- Second pair: worn for 12 h per day (12 H protocol)
Statistical Analysis
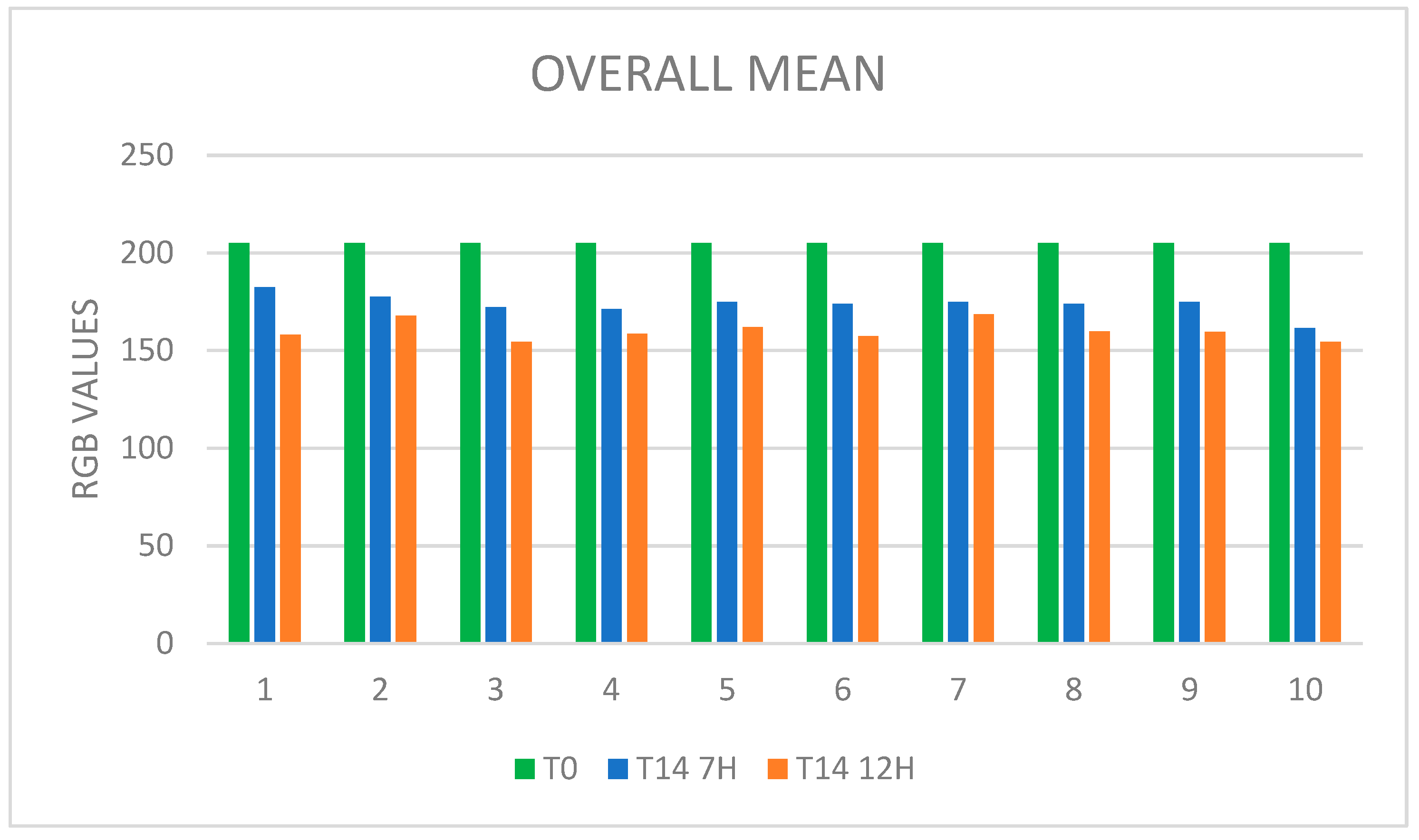
3. Results
3.1. Descriptive Statistics
3.2. Paired t-Test
4. Discussion
5. Conclusions
- A strong and statistically significant correlation was observed between aligner wear duration and polyamide discoloration, as indicated by decreasing RGB values.
- The progressive reduction in RGB values reflected increased yellowing of the aligner, supporting the potential use of this method as an indirect indicator of wear time.
- This method is readily implementable through smartphone-based applications, enabling the accessible and real-time monitoring of patient compliance without the need for invasive procedures.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PA | Aliphatic polyamide |
| RGB | Red, green, blue |
| CMYK | Cyan, Magenta, Yellow, Key |
| HEX | Hexadecimal |
| HSL | Hue, Saturation, Lightness |
References
- Weir, T. Clear Aligners in Orthodontic Treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef]
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores Mir, C. Effectiveness of Clear Aligner Therapy for Orthodontic Treatment: A Systematic Review. Orthod. Craniofacial Res. 2020, 23, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Kohda, N.; Iijima, M.; Muguruma, T.; Brantley, W.A.; Ahluwalia, K.S.; Mizoguchi, I. Effects of Mechanical Properties of Thermoplastic Materials on the Initial Force of Thermoplastic Appliances. Angle Orthod. 2013, 83, 476–483. [Google Scholar] [CrossRef]
- Cremonini, F.; Karami Shabankare, A.; Guiducci, D.; Lombardo, L. Compliance with Headgear Evaluated by Force- and Temperature-Sensitive Monitoring Device: A Case-Control Study. Bioengineering 2024, 11, 789. [Google Scholar] [CrossRef] [PubMed]
- Al-Moghrabi, D.; Salazar, F.C.; Pandis, N.; Fleming, P.S. Compliance with Removable Orthodontic Appliances and Adjuncts: A Systematic Review and Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 17–32. [Google Scholar] [CrossRef] [PubMed]
- Schott, T.C.; Meyer-Gutknecht, H.; Mayer, N.; Weber, J.; Weimer, K. A Comparison Between Indirect and Objective Wear-Time Assessment of Removable Orthodontic Appliances. Eur. J. Orthod. 2017, 39, 170–175. [Google Scholar] [CrossRef]
- Timm, L.H.; Farrag, G.; Baxmann, M.; Schwendicke, F. Factors Influencing Patient Compliance During Clear Aligner Therapy: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 3103. [Google Scholar] [CrossRef]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and Geometric Properties of Thermoformed and 3D Printed Clear Dental Aligners. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef]
- Skidmore, K.J.; Brook, K.J.; Thomson, W.M.; Harding, W.J. Factors Influencing Treatment Time in Orthodontic Patients. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 230–238. [Google Scholar] [CrossRef]
- Alansari, R.A. Youth Perception of Different Orthodontic Appliances. Patient Prefer. Adherence 2020, 14, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Försch, M.; Krull, L.; Hechtner, M.; Rahimi, R.; Wriedt, S.; Wehrbein, H.; Jacobs, C.; Jacobs, C. Perception of Esthetic Orthodontic Appliances: An Eye Tracking and Cross-Sectional Study. Angle Orthod. 2020, 90, 109–117. [Google Scholar] [CrossRef]
- Cremonini, F.; Brucculeri, L.; Pepe, F.; Palone, M.; Lombardo, L. Comparison of Stress Relaxation Properties between 3-Dimensional Printed and Thermoformed Orthodontic Aligners: A Pilot Study of In Vitro Simulation of Two Consecutive 8-Hours Force Application. APOS Trends Orthod. 2024, 14, 225–234. [Google Scholar] [CrossRef]
- Palone, M.; Longo, M.; Arveda, N.; Nacucchi, M.; De Pascalis, F.; Spedicato, G.A.; Siciliani, G.; Lombardo, L. Micro-Computed Tomography Evaluation of General Trends in Aligner Thickness and Gap Width After Thermoforming Procedures Involving Six Commercial Clear Aligners: An In Vitro Study. Korean J. Orthod. 2021, 51, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Henry, W.F.; David, M.S.; James, L.A. Contemporary Orthodontics, 5th ed.; Elsevier: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Hahn, W.; Dathe, H.; Fialka-Fricke, J.; Fricke-Zech, S.; Zapf, A.; Kubein-Meesenburg, D.; Sadat-Khonsari, R. Influence of Thermoplastic Appliance Thickness on the Magnitude of Force Delivered to a Maxillary Central Incisor During Tipping. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 12.e1–12.e7. [Google Scholar] [CrossRef] [PubMed]
- Tsomos, G.; Ludwig, B.; Grossen, J.; Pazera, P.; Gkantidis, N. Objective Assessment of Patient Compliance with Removable Orthodontic Appliances: A Cross-Sectional Cohort Study. Angle Orthod. 2014, 84, 56–61. [Google Scholar] [CrossRef]
- Arreghini, A.; Trigila, S.; Lombardo, L.; Siciliani, G. Objective Assessment of Compliance with Intra- and Extraoral Removable Appliances. Angle Orthod. 2017, 87, 88–95. [Google Scholar] [CrossRef]
- van der Bie, M.R.; Bos, A.; Joseph Mathieu Bruers, J.; Edwin Gaston Jonkman, R. ARTICLE OPEN Patient Adherence in Orthodontics: A Scoping Review. BDJ Open 2024, 10, 58. [Google Scholar] [CrossRef]
- Ragain, J.C. A Review of Color Science in Dentistry: Colorimetry and Color Space. J. Dent. Oral. Disord. Ther. 2016, 4, 1–5. Available online: www.symbiosisonlinepublishing.com (accessed on 12 September 2024). [CrossRef]
- Olteanu, N.D.; Taraboanta, I.; Panaite, T.; Balcos, C.; Rosu, S.N.; Vieriu, R.M.; Dinu, S.; Zetu, I.N. Color Stability of Various Orthodontic Clear. Aligner Systems After Submersion in Different Staining Beverages. Materials 2024, 17, 4009. [Google Scholar] [CrossRef]
- Ajwa, N.; Radhi, F.; Aloraini, R.; AlSaydalani, G. Comparative Color Stability Assessment of Orthodontic Clear Aligners: An In Vitro Study. Sci. Rep. 2025, 15, 2041. [Google Scholar] [CrossRef] [PubMed]
- Filippone, G.; Carroccio, S.C.; Mendichi, R.; Gioiella, L.; Dintcheva, N.T.; Gambarotti, C. Time-Resolved Rheology as a Tool to Monitor the Progress of Polymer Degradation in the Melt State—Part I: Thermal and Thermo-Oxidative Degradation of Polyamide 11. Polymer 2015, 72, 134–141. [Google Scholar] [CrossRef]
- Powell, A.W.; Stavrinadis, A.; Christodoulou, S.; Quidant, R.; Konstantatos, G. On-Demand Activation of Photochromic Nanoheaters for High Color Purity 3D Printing. Nano Lett. 2020, 20, 3485–3491. [Google Scholar] [CrossRef] [PubMed]
- Meissner, H.; Vacquier, M.; Kresse-Walczak, K.; Boening, K. Mechanical, Optical and Surface Properties of 3D-Printed and Conventionally Processed Polyamide 12. Dent. Med. Probl. 2024, 61, 729–738. [Google Scholar] [CrossRef]
- Schott, T.C.; Göz, G. Color Fading of the Blue Compliance Indicator Encapsulated in Removable Clear Invisalign Teen® Aligners. Angle Orthod. 2011, 81, 185–191. [Google Scholar] [CrossRef]
- Tuncay, O.C.; Jay Bowman, S.; Nicozisis, J.L.; Amy, B.D. Effectiveness of a Compliance Indicator for Clear Aligners. J. Clin. Orthod. 2009, 43, 263–268. Available online: www.jco-online.com (accessed on 19 December 2024).
- Marks, J.; Freer, E.; Ong, D.; Lam, J.; Miles, P. Evaluating Dental Monitoring Effectiveness Compared with Conventional Monitoring of Clear Aligner Therapy Using the Peer Assessment Rating Index. Am. J. Orthod. Dentofac. Orthop. 2024, 166, 350–355. [Google Scholar] [CrossRef]
- Timm, L.H.; Farrag, G.; Wolf, D.; Baxmann, M.; Schwendicke, F. Effect of Electronic Reminders on Patients’ Compliance During Clear Aligner Treatment: An Interrupted Time Series Study. Sci. Rep. 2022, 12, 16652. [Google Scholar] [CrossRef]
- Eliades, T.; Bourauel, C. Intraoral Aging of Orthodontic Materials: The Picture We Miss and Its Clinical Relevance. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 403–412. [Google Scholar] [CrossRef]
- Nicita, F.; D’Amico, C.; Filardi, V.; Spadaro, D.; Aquilio, E.; Mancini, M.; Fiorillo, L. Chemical-Physical Characterization of PET-G-Based Material for Orthodontic Use: Preliminary Evaluation of Micro-Raman Analysis. Eur. J. Dent. 2023, 18, 228–235. [Google Scholar] [CrossRef]
- Wieckiewicz, M.; Opitz, V.; Richter, G.; Boening, K.W. Physical Properties of Polyamide-12 Versus PMMA Denture Base Material. Biomed Res. Int. 2014, 2014, 150298. [Google Scholar] [CrossRef] [PubMed]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Adult patients (aged from 25 to 31 years) | Patients with systemic diseases |
| Good systemic health | Heavy smokers (>7 cigarettes/day) |
| Patients not undergoing orthodontic treatment | Patients undergoing treatment with antihistamines or anticholinergic drugs |
| Good oral hygiene | Patients with habitual consumption of pigmented beverage |
| Patients unable to perform home oral hygiene procedures | |
| Patients with hyposalivation |
| Patient | Control | Tooth 24 | Tooth 14 | Tooth 21 | Mean | SD | Median |
|---|---|---|---|---|---|---|---|
| 1 | 205 | 179 | 185 | 182 | 182 | 3 | 182 |
| 2 | 205 | 165 | 185 | 175 | 175 | 10 | 175 |
| 3 | 205 | 185 | 167 | 160 | 170.67 | 12.9 | 167 |
| 4 | 205 | 183 | 172 | 163 | 172.67 | 10.02 | 172 |
| 5 | 205 | 168 | 183 | 176 | 175.67 | 7.51 | 176 |
| 6 | 205 | 165 | 163 | 180 | 169.33 | 9.29 | 165 |
| 7 | 205 | 167 | 176 | 186 | 176.33 | 9.5 | 176 |
| 8 | 205 | 163 | 188 | 167 | 172.67 | 13.43 | 167 |
| 9 | 205 | 168 | 180 | 174 | 174 | 6 | 174 |
| 10 | 205 | 148 | 178 | 153 | 159.67 | 16.07 | 153 |
| Patient | Control | Tooth 34 | Tooth 41 | Tooth 44 | Mean | SD | Median |
|---|---|---|---|---|---|---|---|
| 1 | 205 | 177 | 187 | 184 | 182.67 | 5.13 | 184 |
| 2 | 205 | 185 | 175 | 180 | 180 | 5 | 180 |
| 3 | 205 | 170 | 170 | 181 | 173.67 | 6.35 | 170 |
| 4 | 205 | 171 | 166 | 172 | 169.67 | 3.21 | 171 |
| 5 | 205 | 180 | 173 | 169 | 174 | 5.57 | 173 |
| 6 | 205 | 179 | 173 | 184 | 178.67 | 5.51 | 179 |
| 7 | 205 | 174 | 163 | 183 | 173.33 | 10.02 | 174 |
| 8 | 205 | 180 | 172 | 173 | 175 | 4.36 | 173 |
| 9 | 205 | 174 | 170 | 184 | 176 | 7.21 | 174 |
| 10 | 205 | 161 | 157 | 172 | 163.33 | 7.68 | 161 |
| Patient | Control | Tooth 24 | Tooth 14 | Tooth 21 | Mean | SD | Median |
|---|---|---|---|---|---|---|---|
| 1 | 205 | 165 | 164 | 145 | 158 | 11.27 | 164 |
| 2 | 205 | 159 | 162 | 165 | 162 | 3 | 162 |
| 3 | 205 | 150 | 149 | 152 | 150.33 | 1.53 | 150 |
| 4 | 205 | 167 | 153 | 166 | 162 | 7.81 | 166 |
| 5 | 205 | 157 | 165 | 164 | 162 | 4.36 | 164 |
| 6 | 205 | 164 | 151 | 140 | 151.67 | 12.01 | 151 |
| 7 | 205 | 165 | 180 | 170 | 171.67 | 7.64 | 170 |
| 8 | 205 | 159 | 162 | 153 | 158 | 4.58 | 159 |
| 9 | 205 | 168 | 159 | 155 | 160.67 | 6.66 | 159 |
| 10 | 205 | 176 | 144 | 148 | 156 | 17.44 | 148 |
| Patient | Control | Tooth 34 | Tooth 41 | Tooth 44 | Mean | SD | Median |
|---|---|---|---|---|---|---|---|
| 1 | 205 | 155 | 153 | 166 | 158 | 7 | 155 |
| 2 | 205 | 178 | 163 | 180 | 173.67 | 9.29 | 178 |
| 3 | 205 | 163 | 148 | 165 | 158.67 | 9.29 | 163 |
| 4 | 205 | 158 | 161 | 147 | 155.33 | 7.37 | 158 |
| 5 | 205 | 160 | 163 | 163 | 162 | 1.73 | 163 |
| 6 | 205 | 154 | 173 | 162 | 163 | 9.53 | 162 |
| 7 | 205 | 161 | 166 | 170 | 165.67 | 4.51 | 166 |
| 8 | 205 | 173 | 150 | 162 | 161.67 | 11.5 | 162 |
| 9 | 205 | 158 | 163 | 155 | 158.67 | 4.04 | 158 |
| 10 | 205 | 144 | 156 | 158 | 152.67 | 7.57 | 156 |
| Patient | Control | Mean | SD | Median |
|---|---|---|---|---|
| 1 | 205 | 182.33 | 3.77 | 183 |
| 2 | 205 | 177.5 | 7.58 | 177.5 |
| 3 | 205 | 172.17 | 9.24 | 170 |
| 4 | 205 | 171.17 | 6.85 | 171.5 |
| 5 | 205 | 174.83 | 5.98 | 174.5 |
| 6 | 205 | 174 | 8.53 | 176 |
| 7 | 205 | 174.83 | 8.88 | 175 |
| 8 | 205 | 173.83 | 9.02 | 172.5 |
| 9 | 205 | 175 | 6.03 | 174 |
| 10 | 205 | 161.5 | 11.47 | 159 |
| Patient | Control | Mean | SD | Median |
|---|---|---|---|---|
| 1 | 205 | 158 | 8.39 | 159.5 |
| 2 | 205 | 167.83 | 8.89 | 164 |
| 3 | 205 | 154.5 | 7.5 | 151 |
| 4 | 205 | 158.67 | 7.7 | 159.5 |
| 5 | 205 | 162 | 2.97 | 163 |
| 6 | 205 | 157.33 | 11.52 | 158 |
| 7 | 205 | 168.67 | 6.5 | 168 |
| 8 | 205 | 159.83 | 8.08 | 160.5 |
| 9 | 205 | 159.67 | 5.05 | 158.5 |
| 10 | 205 | 154.33 | 12.16 | 152 |
| Control | 7 H Average | Average of Differences | SD of Differences | Test Statistic | p Value | |
|---|---|---|---|---|---|---|
| Overall Mean | 205 | 173.72 | −31.28 | 5.28 | −18.73 | <0.001 |
| Upper Arch | 205 | 172.8 | −32.2 | 5.78 | −17.62 | <0.001 |
| Lower Arch | 205 | 174.64 | −30.37 | 5.45 | −17.63 | <0.001 |
| Control | 12 H Average | Average of Differences | SD of Differences | Test Statistic | p Value | |
|---|---|---|---|---|---|---|
| Overall Mean | 205 | 160.08 | −44.92 | 4.9 | −29.01 | <0.001 |
| Upper Arch | 205 | 159.23 | −45.77 | 6.05 | −23.92 | <0.001 |
| Lower Arch | 205 | 160.93 | −44.07 | 5.86 | −23.78 | <0.001 |
| 7 H Average | 12 H Average | Average of Differences | SD of Differences | Test Statistic | p Value | |
|---|---|---|---|---|---|---|
| Overall Mean | 173.72 | 160.09 | −13.6333 | 5.3563 | −8.0489 | <0.001 |
| Upper Arch | 172.8 | 159.23 | −13.5667 | 6.3129 | −6.7958 | <0.001 |
| Lower Arch | 174.64 | 160.93 | −13.7 | 5.1889 | −8.3492 | <0.001 |
| Upper Arch | Lower Arch | Average of Differences | SD of Differences | Test Statistic | p Value | |
|---|---|---|---|---|---|---|
| 7 H | 172.8 | 174.63 | 1.8333 | 3.8241 | 1.52 | >0.1 |
| 12 H | 159.23 | 160.93 | 1.7 | 6.7831 | 0.7925 | >0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cremonini, F.; Chiusolo, G.; Pepe, F.; Lombardo, L. Color Variation in 3D-Printed Orthodontic Aligners as a Compliance Indicator: A Prospective Pilot Study. Appl. Sci. 2025, 15, 6409. https://doi.org/10.3390/app15126409
Cremonini F, Chiusolo G, Pepe F, Lombardo L. Color Variation in 3D-Printed Orthodontic Aligners as a Compliance Indicator: A Prospective Pilot Study. Applied Sciences. 2025; 15(12):6409. https://doi.org/10.3390/app15126409
Chicago/Turabian StyleCremonini, Francesca, Giuseppe Chiusolo, Filippo Pepe, and Luca Lombardo. 2025. "Color Variation in 3D-Printed Orthodontic Aligners as a Compliance Indicator: A Prospective Pilot Study" Applied Sciences 15, no. 12: 6409. https://doi.org/10.3390/app15126409
APA StyleCremonini, F., Chiusolo, G., Pepe, F., & Lombardo, L. (2025). Color Variation in 3D-Printed Orthodontic Aligners as a Compliance Indicator: A Prospective Pilot Study. Applied Sciences, 15(12), 6409. https://doi.org/10.3390/app15126409







