The Impact of Combined Scapular Stabilization and Breathing Training on Pain and Respiratory Function in Individuals with Upper Cross Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Procedure
2.3. Measurements
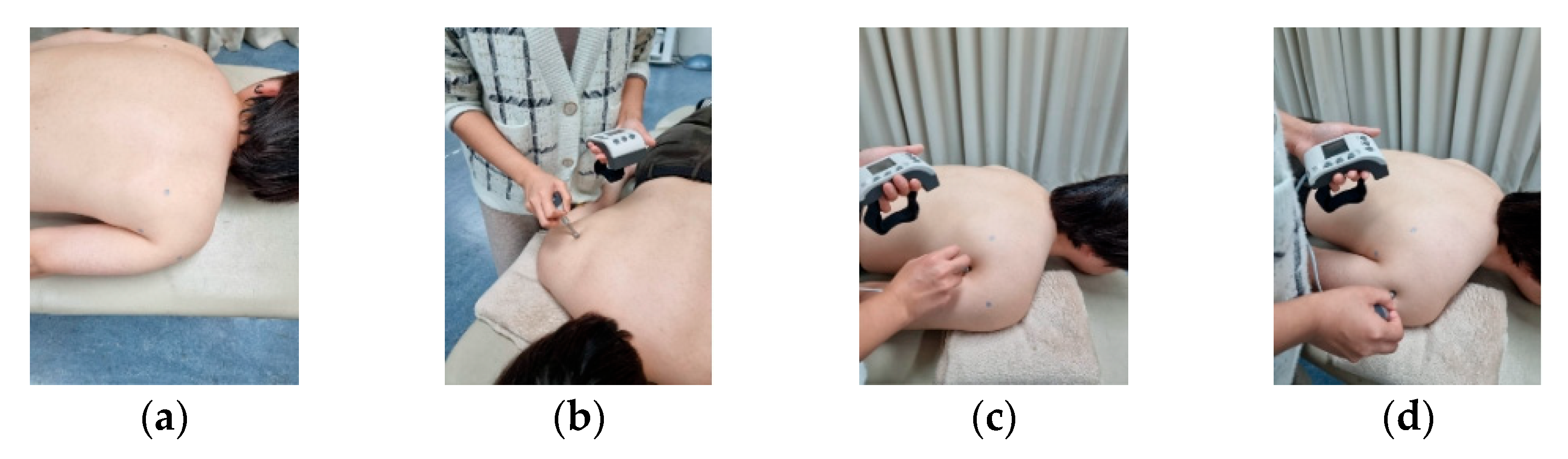
2.3.1. Measurement of the Muscle Pressure Pain Threshold
2.3.2. Measurement of Respiratory Function
2.3.3. Measurement of Lower Chest Expansion (LCE)
2.4. Intervention
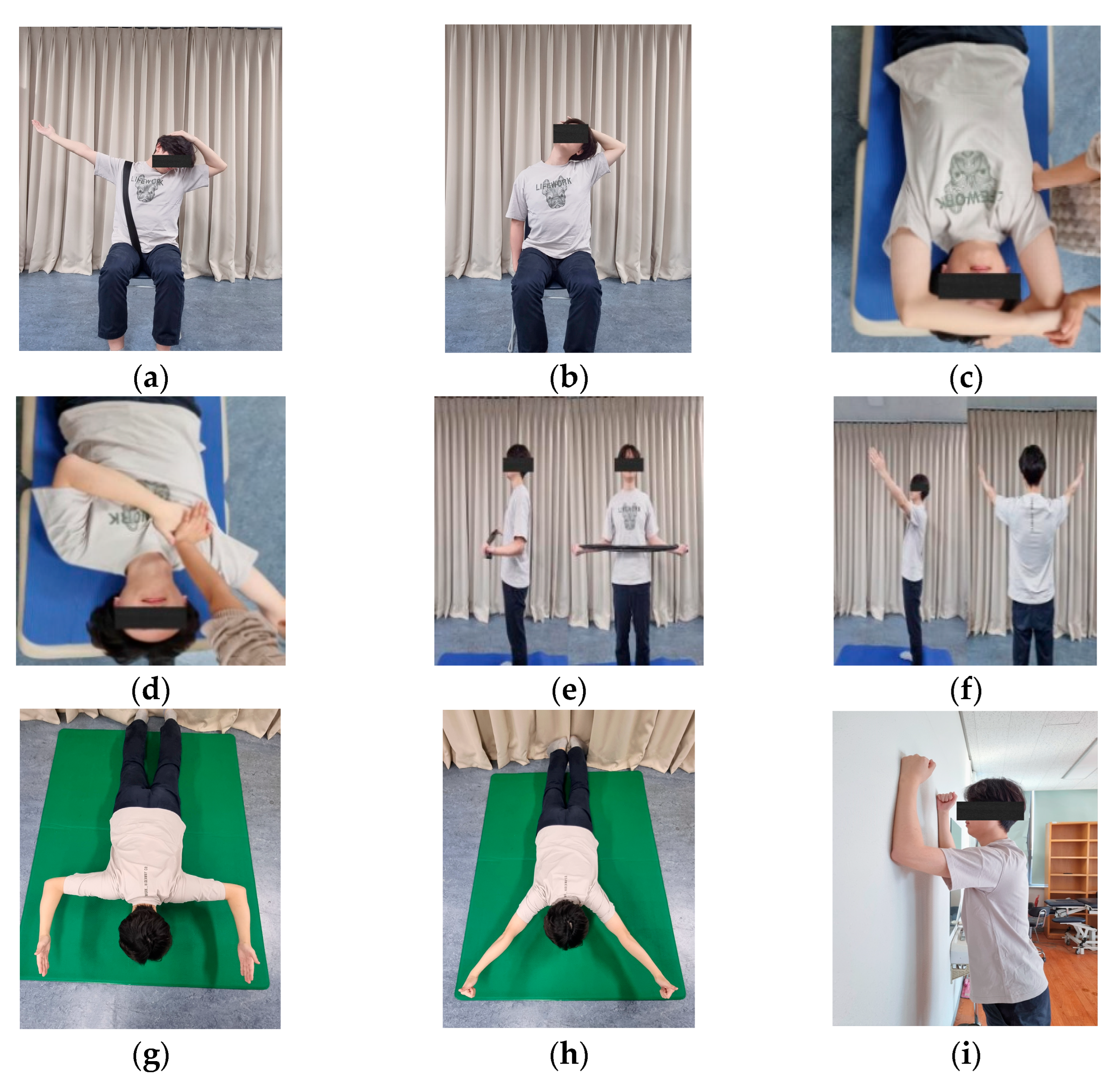
2.4.1. Scapular Stabilization Exercises
2.4.2. Breathing Training
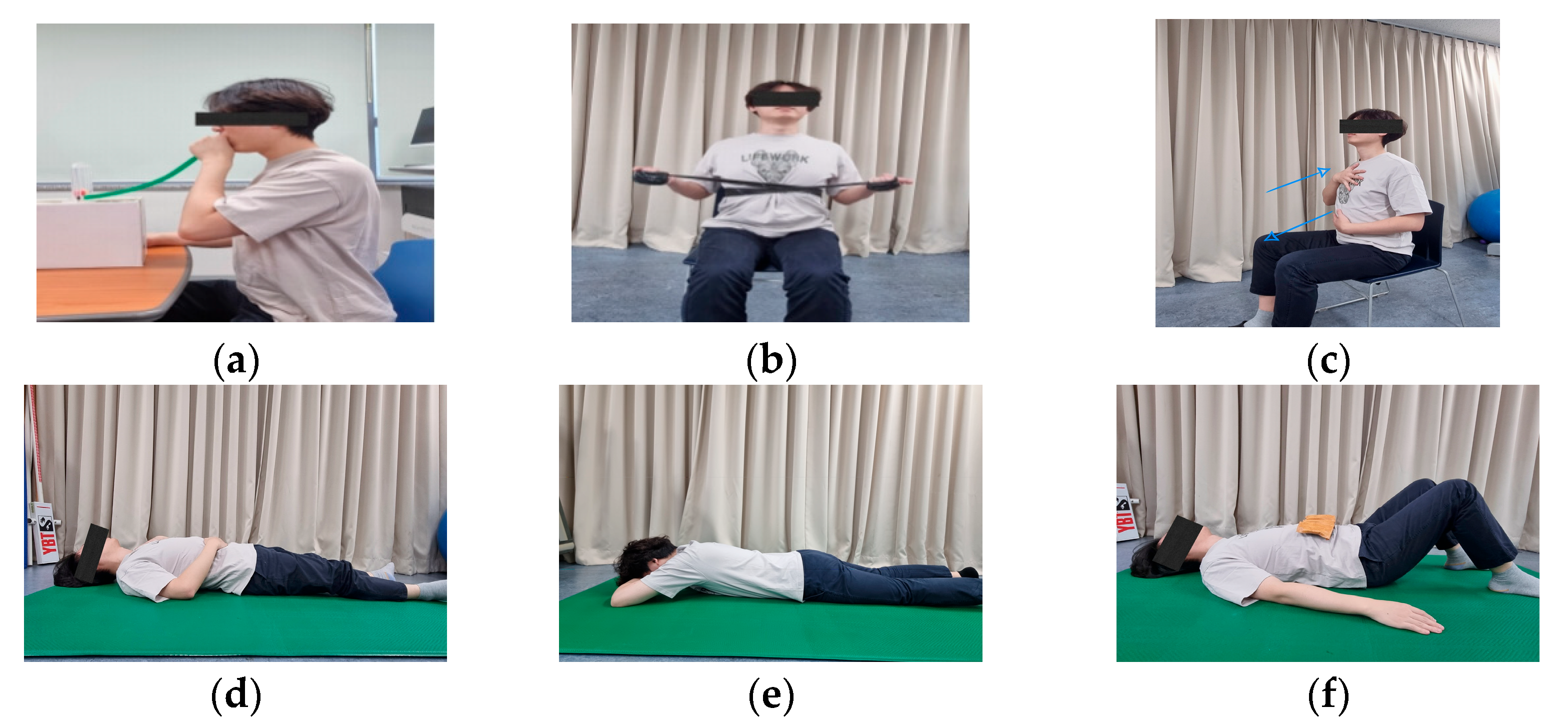
2.4.3. Thoracic Exercises
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sengupta, D.; Al-Khalifa, D. Pandemic imposed remote work arrangements and resultant work-life integration, future of work and role of leaders—A qualitative study of Indian millennial workers. Adm. Sci. 2022, 12, 162. [Google Scholar] [CrossRef]
- Kaur, S.; Chatterjee, S.; Goyal, M.; Popli, A.; Goyal, K.; Saha, M.; Garg, S.; Sushma, K.C. Physiotherapeutic approaches in upper cross syndrome: A systematic review of systematic reviews. J. Bodyw. Mov. Ther. 2025, 42, 756–762. [Google Scholar] [CrossRef]
- Chaudhuri, S.; Chawla, J.K.; Phadke, V. Physiotherapeutic Interventions for Upper Cross Syndrome: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e45471. [Google Scholar] [CrossRef] [PubMed]
- Csepregi, É.; Gyurcsik, Z.; Veres-Balajti, I.; Nagy, A.C.; Szekanecz, Z.; Szántó, S. Effects of classical breathing exercises on posture, spinal and chest mobility among female university students compared to currently popular training programs. Int. J. Environ. Res. Public. Health 2022, 19, 3728. [Google Scholar] [CrossRef]
- Lowry, V.; Desjardins-Charbonneau, A.; Roy, J.S.; Dionne, C.E.; Fremont, P.; MacDermid, J.C.; Desmeules, F. Efficacy of workplace interventions for shoulder pain: A systematic review and meta-analysis. J. Rehabil. Med. 2017, 49, 529. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, D.L. Evaluation and treatment of shoulder pain. Med. Clin. North. Am. 2014, 98, 487–504. [Google Scholar] [CrossRef] [PubMed]
- D’hondt, N.E.; Pool, J.J.; Kiers, H.; Terwee, C.B.; Veeger, H. Validity of clinical measurement instruments assessing scapular function: Insufficient evidence to recommend any instrument for assessing scapular posture, movement, and dysfunction—A systematic review. J. Orthop. Sports Phys. Ther. 2020, 50, 632–641. [Google Scholar] [CrossRef]
- Keshavarz, R.; Tajali, S.B.; Mir, S.M.; Ashrafi, H. The role of scapular kinematics in patients with different shoulder musculoskeletal disorders: A systematic review approach. J. Bodyw. Mov. Ther. 2017, 21, 386–400. [Google Scholar] [CrossRef]
- Giuseppe, L.U.; Laura, R.A.; Berton, A.; Candela, V.; Massaroni, C.; Carnevale, A.; Stelitano, G.; Schena, E.; Nazarian, A.; DeAngelis, J. Scapular dyskinesis: From basic science to ultimate treatment. Int. J. Environ. Res. Public. Health 2020, 17, 2974. [Google Scholar]
- Kibler, W.B.; Sciascia, A. Current concepts: Scapular dyskinesis. Br. J. Sports Med. 2010, 44, 300–305. [Google Scholar] [CrossRef]
- Santino, T.A.; Chaves, G.S.; Freitas, D.A.; Fregonezi, G.A.; Mendonça, K.M. Breathing exercises for adults with asthma. Cochrane Database Syst. Rev. 2020, 3, CD001277. [Google Scholar] [CrossRef] [PubMed]
- Srijessadarak, T.; Arayawichanon, P.; Kanpittaya, J.; Boonprakob, Y. Diaphragmatic Mobility and Chest Expansion in Patients with Scapulocostal Syndrome: A Cross-Sectional Study. Healthcare 2022, 10, 950. [Google Scholar] [CrossRef]
- Samosir, N.R.; Azizan, A. Effectiveness of Segmental Breathing and Expansion Thorax Exercise in Young to Middle-Aged Post-COVID Survivors. Int. J. Aging Health Mov. 2023, 5, 8–14. [Google Scholar]
- Dhaniwala, N.K.S.; Dasari, V.; Dhaniwala, M.N. Pranayama and Breathing Exercises-Types and Its Role in Disease Prevention & Rehabilitation. J. Evol. Med. Dent. Sci. 2020, 9, 3325–3331. [Google Scholar]
- Saito, H.; Harrold, M.E.; Cavalheri, V.; McKenna, L. Scapular focused interventions to improve shoulder pain and function in adults with subacromial pain: A systematic review and meta-analysis. Physiother. Theory Pract. 2018, 34, 653–670. [Google Scholar] [CrossRef]
- Pieters, L.; Lewis, J.; Kuppens, K.; Jochems, J.; Bruijstens, T.; Joossens, L.; Struyf, F. An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J. Orthop. Sports Phys. Ther. 2020, 50, 131–141. [Google Scholar] [CrossRef]
- Ghanbari, A.; Ghaffarinejad, F.; Mohammadi, F.; Khorrami, M.; Sobhani, S. Effect of forward shoulder posture on pulmonary capacities of women. Br. J. Sports Med. 2008, 42, 622–623. [Google Scholar] [PubMed]
- Kang, N.-Y.; Im, S.-C.; Kim, K. Effects of a combination of scapular stabilization and thoracic extension exercises for office workers with forward head posture on the craniovertebral angle, respiration, pain, and disability: A randomized-controlled trial. Turk. J. Phys. Med. Rehabil. 2021, 67, 291. [Google Scholar] [CrossRef]
- Intelangelo, L.; Bordachar, D.J.; Mendoza, C.I.; Imaz, F.; Barone, M.; Barbosa, A.W. Effect of different postures of the scapular girdle and arm on the pressure pain threshold in the infraspinatus muscle. J. Bodyw. Mov. Ther. 2021, 28, 276–282. [Google Scholar] [CrossRef]
- Barone, M.; Imaz, F.; Converso, G.; Bordachar, D.; Barbero, A.; Trucco, M.; Intelangelo, L. Immediate effects of rhythmic joint mobilization of the temporomandibular joint on pain, mouth opening and electromyographic activity in patients with temporomandibular disorders. J. Bodyw. Mov. Ther. 2021, 28, 563–569. [Google Scholar] [CrossRef]
- Park, K.-N.; Kwon, O.-Y.; Weon, J.-H.; Choung, S.-D.; Kim, S.-H. Comparison of the effects of local cryotherapy and passive cross-body stretch on extensibility in subjects with posterior shoulder tightness. J. Sports Sci. Med. 2014, 13, 84. [Google Scholar]
- Pirola, A.; De Mattia, E.; Lizio, A.; Sannicolo, G.; Carraro, E.; Rao, F.; Sansone, V.; Lunetta, C. The prognostic value of spirometric tests in Amyotrophic Lateral Sclerosis patients. Clin. Neurol. Neurosurg. 2019, 184, 105456. [Google Scholar] [CrossRef]
- Han, J.; Park, S.; Kim, Y.; Choi, Y.; Lyu, H. Effects of forward head posture on forced vital capacity and respiratory muscles activity. J. Phys. Ther. Sci. 2016, 28, 128–131. [Google Scholar] [CrossRef] [PubMed]
- Derasse, M.; Lefebvre, S.; Liistro, G.; Reychler, G. Chest Expansion and Lung Function for Healthy Subjects and Individuals with Pulmonary Disease. Respir. Care 2021, 66, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Kwon, O.-Y.; Kang, M.-H.; Kim, M.-H.; Kim, S.-J.; Kim, T.-H.; Park, K.-N.; Oh, J.-S.; Lee, W.-H.; Im, I.-Y.; Jang, J.-H.; et al. KEMA Approach for Analysis and Management of Motor Impairment 1; Hakjisa Medical: Seoul, Republic of Korea, 2022. [Google Scholar]
- Aneis, Y.M.; El-Badrawy, N.M.; El-Ganainy, A.A.; Atta, H.K. The effectiveness of a multimodal approach in the treatment of patients with upper crossed syndrome: A randomized controlled trial. J. Bodyw. Mov. Ther. 2022, 32, 130–136. [Google Scholar] [CrossRef]
- Arshadi, R.; Ghasemi, G.A.; Samadi, H. Effects of an 8-week selective corrective exercises program on electromyography activity of scapular and neck muscles in persons with upper crossed syndrome: Randomized controlled trial. Phys. Ther. Sport. 2019, 37, 113–119. [Google Scholar] [CrossRef]
- Shetty, N.; Samuel, S.R.; Alaparthi, G.K.; Amaravadi, S.K.; Joshua, A.M.; Pai, S. Comparison of Diaphragmatic Breathing Exercises, Volume, and—71—Flow-Oriented Incentive Spirometry on Respiratory Function in Stroke Subjects: A Non-randomized Study. Ann. Neurosci. 2020, 27, 232–241. [Google Scholar] [CrossRef]
- Tomas-Carus, P.; Branco, J.C.; Raimundo, A.; Parraca, J.A.; Batalha, N.; Biehl-Printes, C. Breathing exercises must be a real and effective intervention to consider in women with fibromyalgia: A pilot randomized controlled trial. J. Altern. Complement. Med. 2018, 24, 825–832. [Google Scholar] [CrossRef]
- Finocchietti, S.; Mørch, C.D.; Arendt-Nielsen, L.; Graven-Nielsen, T. Effects of adipose thickness and muscle hardness on pressure pain sensitivity: Correction. Clin. J. Pain. 2011, 27, 735–745. [Google Scholar] [CrossRef]
- Lee, H.S. The effects of aerobic exercise and strengthening exercise on pain pressure thresholds. J. Phys. Ther. Sci. 2014, 26, 1107–1111. [Google Scholar] [CrossRef]
- Lee, J.-H.; Cynn, H.-S.; Yoon, T.-L.; Choi, S.-A.; Choi, W.-J.; Choi, B.-S.; Ko, C.-H. Comparison of scapular posterior tilting exercise alone and scapular posterior tilting exercise after pectoralis minor stretching on scapular alignment and scapular upward rotators activity in subjects with short pectoralis minor. Phys. Ther. Sport. 2015, 16, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Thongchote, K.; Threetepchanchai, K.; Chuwijit, A.; Lapmanee, S. Pilot study on the improvement effects of scapulothoracic exercises on the respiratory functions in sedentary young female adult with forward shoulder posture: A randomized control trial. Adv. Rehabil. 2023, 37, 23–32. [Google Scholar] [CrossRef]
- Arsalan, A.; Waqar, M.; Ahmad, A.; Gillani, S.A. Immediate and prolonged effects of breathing exercises on pain, quality of life and functional disability in patients of upper cross Syndrome: A randomized controlled trial. J. Riphah Coll. Rehabil. Sci. 2023, 11, 34–39. [Google Scholar]
- Jeong, G.H.; Lee, B.H. Effects of telerehabilitation combining diaphragmatic breathing re-education and shoulder stabilization exercises on neck pain, posture, and function in young adult men with upper crossed syndrome: A randomized controlled trial. J. Clin. Med. 2024, 13, 1612. [Google Scholar] [CrossRef]


| SBG | STG | Time F(p) | Group F(p) | Time × GroupF (p) | ||
|---|---|---|---|---|---|---|
| PD | Pre | 9.49 ± 5.13 a | 9.20 ± 3.77 | 65.427 (0.000 *) | 0.107 (0.745) | 0.528 (0.473) |
| post | 12.39 ± 5.39 | 11.63 ± 3.98 | ||||
| t(p) | −5.649 (0.000 *) | −5.886 (0.000 *) | ||||
| TM | Pre | 8.55 ± 3.60 | 8.24 ± 3.65 | 88.943 (0.000 *) | 0.213 (0.648) | 0.947 (0.338) |
| Post | 11.52 ± 4.38 | 10.65 ± 3.31 | ||||
| t(p) | −6.093 (0.000 *) | −8.122 (0.000 *) | ||||
| IN | Pre | 9.57 ± 4.01 | 8.92 ± 3.15 | 54.415 (0.000 *) | 0.193 (0.663) | 0.029 (0.867) |
| Post | 11.60 ± 4.87 | 11.05 ± 3.68 | ||||
| t(p) | −4.845 (0.000 *) | −5.645 (0.000 *) |
| SBG | STG | TimeF (p) | Group F(p) | Time × Group F(p) | ||
|---|---|---|---|---|---|---|
| FVC(L) | Pre | 4.00 ± 1.04 a | 3.68 ± 0.73 | 33.322 (0.000 *) | 1.198 (0.282) | 2.111 (0.157) |
| Post | 4.17 ± 1.07 | 3.79 ± 0.70 | ||||
| t(p) | −4.933 (0.000 *) | −3.172 (0.006 *) | ||||
| FEV1(L) | Pre | 3.22 ± 0.89 | 3.01 ± 0.54 | 48.651 (0.000 *) | 1.207 (0.281) | 2.800 (0.105) |
| Post | 3.55 ± 0.84 | 3.21 ± 0.50 | ||||
| t(p) | −5.920 (0.000 *) | −3.881 (0.001 *) | ||||
| FEV1/FVC% | Pre | 80.52 ± 8.58 | 82.43 ± 8.46 | 13.726 (0.001 *) | 0.107 (0.745) | 0.955 (0.336) |
| Post | 85.71 ± 6.97 | 85.45 ± 7.07 | ||||
| t(p) | −2.741 (0.015 *) | −2.623 (0.019 *) | ||||
| LCE | Pre | 4.29 ± 0.62 | 4.58 ± 0.74 | 96.929 (0.000 *) | 0.150 (0.702) | 0.475 (0.496) |
| Post | 6.90 ± 1.59 | 6.86 ± 1.43 | ||||
| t(p) | −6.247 (0.000 *) | −8.514 (0.000 *) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, X.; Kim, T.-H. The Impact of Combined Scapular Stabilization and Breathing Training on Pain and Respiratory Function in Individuals with Upper Cross Syndrome. Appl. Sci. 2025, 15, 6147. https://doi.org/10.3390/app15116147
Yan X, Kim T-H. The Impact of Combined Scapular Stabilization and Breathing Training on Pain and Respiratory Function in Individuals with Upper Cross Syndrome. Applied Sciences. 2025; 15(11):6147. https://doi.org/10.3390/app15116147
Chicago/Turabian StyleYan, Xin, and Tae-Ho Kim. 2025. "The Impact of Combined Scapular Stabilization and Breathing Training on Pain and Respiratory Function in Individuals with Upper Cross Syndrome" Applied Sciences 15, no. 11: 6147. https://doi.org/10.3390/app15116147
APA StyleYan, X., & Kim, T.-H. (2025). The Impact of Combined Scapular Stabilization and Breathing Training on Pain and Respiratory Function in Individuals with Upper Cross Syndrome. Applied Sciences, 15(11), 6147. https://doi.org/10.3390/app15116147





