Impact of COVID-19 on Ureteroscopy Management of Urolithiasis: Retrospective Comparative Study Before and After Pandemic
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
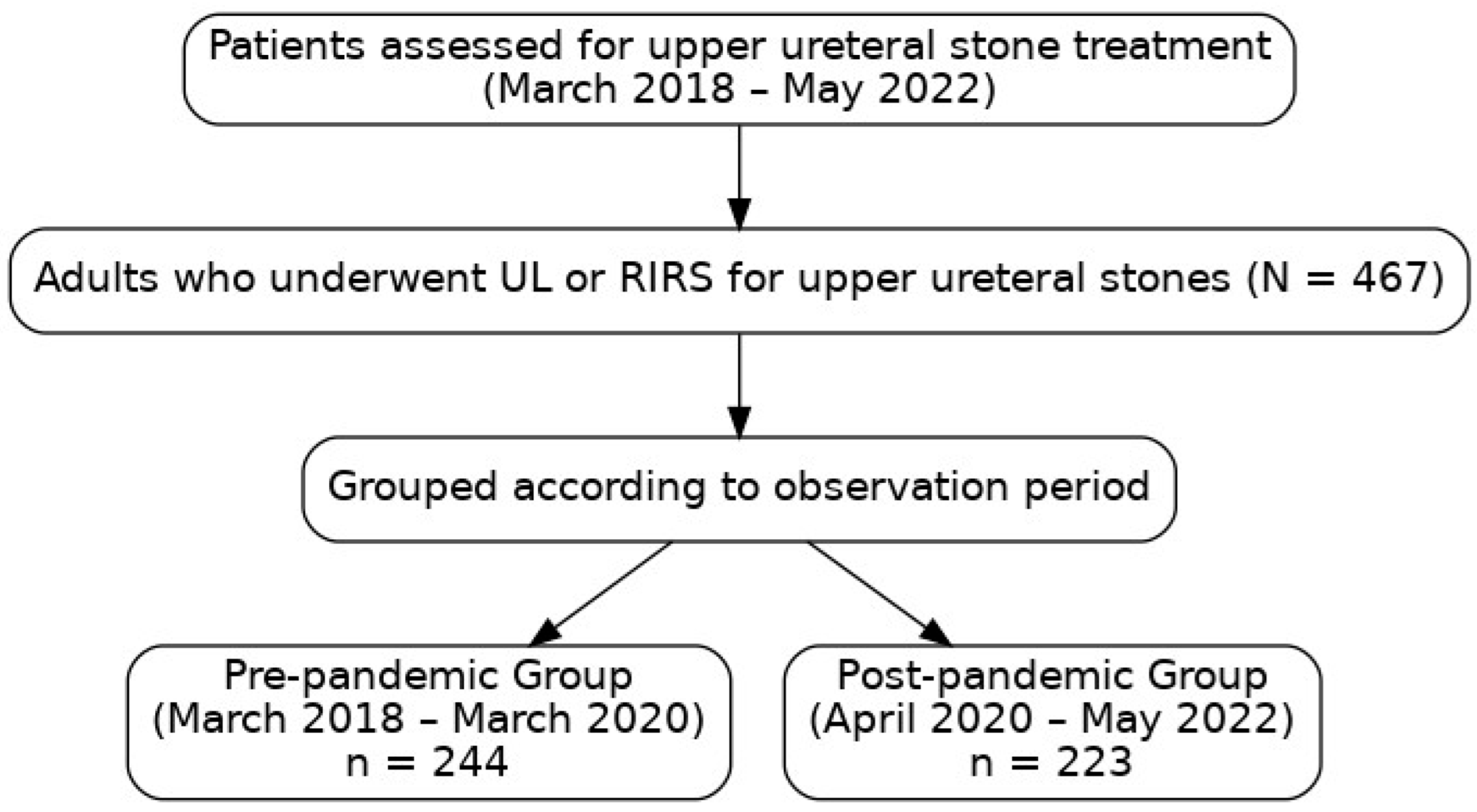
2.1. Study Design and Population
2.2. Data Collection
2.3. Statistical Analysis
2.4. Ethical Considerations
3. Results
3.1. Patient Demographics and Clinical Characteristics
3.2. Perioperative Parameters
3.3. Treatment Outcomes and Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CI | Confidence interval |
| IQR | Interquartile Range |
| RIRS | Retrograde Intrarenal Surgery |
| SIRS | Systemic Inflammatory Response Syndrome |
| UL | Ureteroscopic Lithotripsy |
References
- Ficarra, V.; Novara, G.; Abrate, A.; Bartoletti, R.; Crestani, A.; De Nunzio, C.; Giannarini, G.; Gregori, A.; Liguori, G.; Mirone, V.; et al. Urology practice during the COVID-19 pandemic. Minerva Urol. Nephrol. 2020, 72, 369–375. [Google Scholar] [CrossRef]
- Yasseri, A.F.; Aghamir, S.M.K. Urinary stone management during the COVID-19 pandemic: A suggested approach and review of literature. Ther. Adv. Urol. 2020, 12, 1–5. [Google Scholar] [CrossRef]
- Proietti, S.; Gaboardi, F.; Giusti, G. Endourological stone management in the era of the COVID-19. Eur. Urol. 2020, 78, 131–133. [Google Scholar] [CrossRef] [PubMed]
- Mazzon, G.; Zhang, X.; Yang, X.; Cheng, F.; Liu, Y.; Zeng, G. The effect of COVID-19 outbreak on urological procedures for urinary stones: Data from three high-volume centers in China. Urolithiasis 2023, 51, 5. [Google Scholar] [CrossRef] [PubMed]
- Castellani, D.; Ragonese, M.; Di Rosa, M.; Marzio, V.; Di Gianfrancesco, L.; Bassi, P.; De Dominicis, M.; Dellabella, M.; Antonucci, M. An Italian multicenter analysis of emergency admissions and treatment of upper tract urolithiasis during the lockdown and reopening phases of the COVID-19 pandemic: Are we ready for a second wave of the outbreak? Int. J. Urol. 2021, 28, 950–954. [Google Scholar] [CrossRef] [PubMed]
- Kachroo, N.; Wright, H.C.; Sivalingam, S. A Tale of Two Eras: The Effect of the COVID-19 Pandemic on Stone Disease Presentations. Urology 2020, 144, 270–272. [Google Scholar] [CrossRef]
- Ansari Jafari, A.; Javanmard, B.; Rahavian, A.; Rafiezadeh, A.R.; Borumandnia, N.; Hojjati, S.A.; Hosseininia, S.M.; Karami, H. Impact of COVID-19 pandemic on emergency department referrals with urologic complaints; A retrospective cross-sectional study. Arch. Acad. Emerg. Med. 2022, 10, e37. [Google Scholar] [CrossRef]
- Jiang, T.; Osadchiy, V.; Weinberger, J.M.; Zheng, M.H.; Owen, M.H.; Leonard, S.A.; Mills, J.N.; Kachroo, N.; Eleswarapu, S.V. Impact of the COVID-19 pandemic on patient preferences and decision making for symptomatic urolithiasis. J. Endourol. 2021, 35, 1250–1256. [Google Scholar] [CrossRef]
- Romantini, F.; Saldutto, P.; Maselli, G.; Ferritto, M.; Ranieri, M.; Castellani, D.; Vicentini, C. Patient’s fear of being infected, another complication of COVID-19 outbreak: A lesson learned from a case of life-threatening urolithiasis. J. Endourol. Case Rep. 2020, 6, 402–404. [Google Scholar] [CrossRef]
- Silva, A.B.; Freschi, G.; Carrera, R.V.; Astolfi, R.H.; Berti, F.F.; Gattas, N.; Meller, A. COVID-19 pandemic impact on clinical outcomes of patients with obstructive pyelonephritis. Int. Urol. Nephrol. 2021, 53, 627–633. [Google Scholar] [CrossRef]
- Gul, M.; Kaynar, M.; Yildiz, M.; Batur, A.F.; Akand, M.; Kilic, O.; Goktas, S. The increased risk of complicated ureteral stones in the era of COVID-19 pandemic. J. Endourol. 2020, 34, 882–886. [Google Scholar] [CrossRef]
- Jones, D.; Neal, R.D.; Duffy, S.R.G.; Scott, S.E.; Whitaker, K.L.; Brain, K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: The view from primary care. Lancet Oncol. 2020, 21, 748–750. [Google Scholar] [CrossRef] [PubMed]
- Dinmohamed, A.G.; Visser, O.; Verhoeven, R.H.A.; Louwman, M.W.J.; van Nederveen, F.H.; Willems, S.M.; Merkx, M.A.W.; Lemmens, V.E.P.P.; Nagtegaal, I.D.; Siesling, S. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol. 2020, 21, 750–751. [Google Scholar] [CrossRef]
- Leventhal, R. COVID-19 and the Massive Primary Care Challenge. Healthcare Innovation. 2 June 2020. Available online: https://www.hcinnovationgroup.com/covid-19/article/21140624/covid19-and-the-massive-primary-care-challenge (accessed on 20 April 2025).
- Goldman, H.B.; Haber, G.P. Recommendations for tiered stratification of urological surgery urgency in the COVID-19 era. J. Urol. 2020, 204, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Ribal, M.J.; Cornford, P.; Briganti, A.; Knoll, T.; Gravas, S.; Babjuk, M.; Harding, C.; Breda, A.; Bex, A.; Guidelines Office Rapid Reaction Group (GORRG); et al. European Association of Urology Guidelines Office Rapid Reaction Group: An Organisation-wide Collaborative Effort to Adapt the European Association of Urology Guidelines Recommendations to the Coronavirus Disease 2019 Era. Eur. Urol. 2020, 78, 21–28. [Google Scholar] [CrossRef]
- Japanese Urological Association COVID-19 Task Force. Clinical Practice Guidelines for Urological Care During the COVID-19 Pandemic. May 2020. (In Japanese). Available online: https://www.urol.or.jp/lib/files/info/info_covid-19_guideline.pdf (accessed on 20 April 2025).
- Yang, Y.; Tang, Y.; Bai, Y.; Wang, X.; Feng, D.; Han, P. Preoperative double-J stent placement can improve the stone-free rate for patients undergoing ureteroscopic lithotripsy: A systematic review and meta-analysis. Urolithiasis 2018, 46, 493–499. [Google Scholar] [CrossRef]
- Law, Y.X.T.; Teoh, J.Y.C.; Castellani, D.; Lim, E.J.; Chan, E.O.T.; Wroclawski, M.; Pirola, G.M.; Giulioni, C.; Rubilotta, E.; Gubbioti, M.; et al. Role of pre-operative ureteral stent on outcomes of retrograde intra-renal surgery (RIRS): Systematic review and meta-analysis of 3831 patients and comparison of Asian and non-Asian cohorts. World J. Urol. 2022, 40, 1377–1389. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Ren, H. The development and application of a triage system for urolithiasis during COVID-19. World J. Urol. 2022, 40, 577–583. [Google Scholar] [CrossRef]
- Yuk, H.D.; Park, J.; Cho, S.Y.; Sung, L.H.; Jeong, C.W. The effect of preoperative ureteral stenting in retrograde intrarenal surgery: A multicenter, propensity score-matched study. BMC Urol. 2020, 20, 147. [Google Scholar] [CrossRef]
- Lumma, P.P.; Schneider, P.; Strauss, A.; Plothe, K.D.; Thelen, P.; Ringert, R.H.; Loertzer, H. Impact of ureteral stenting prior to ureterorenoscopy on stone-free rates and complications. World J. Urol. 2013, 31, 855–859. [Google Scholar] [CrossRef]
- Yildiz, A.K.; Bayraktar, A.; Kacan, T.; Keseroğlu, B.B.; Ozgur, B.C.; Doluoglu, O.G.; Karakan, T. Optimal dwelling time for ureteral stents placed for passive dilation after impassable ureteroscopy. Urol. Int. 2023, 107, 772–777. [Google Scholar] [CrossRef] [PubMed]
- Militaru, A.; Bulai, C.A.; Ene, C.; Popescu, R.I.; Cozma, C.; Mares, C.; Balacescu, S.; Moldoveanu, C.; Georgescu, D.A.; Geavlete, P.A.; et al. Double J Stents and Reno–Ureteral Lithiasis: Dynamic Changes in Management during the COVID-19 Pandemic. Life 2023, 13, 2113. [Google Scholar] [CrossRef] [PubMed]
- Nevo, A.; Mano, R.; Baniel, J.; Lifshitz, D.A. Ureteric stent dwelling time: A risk factor for post-ureteroscopy sepsis. BJU Int. 2017, 120, 117–122. [Google Scholar] [CrossRef]
- Joshi, H.B.; Stainthorpe, A.; MacDonagh, R.P.; Keeley, F.X.; Timoney, A.G.; Barry, M.J. Indwelling ureteral stents: Evaluation of symptoms, quality of life and utility. J. Urol. 2003, 169, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.; Sternberg, K.M.; Averch, T.D. Preoperative stenting decreases operative time and reoperative rates of ureteroscopy. J. Endourol. 2011, 25, 751–754. [Google Scholar] [CrossRef]
- Rubenstein, R.A.; Zhao, L.C.; Loeb, S.; Shore, D.M.; Nadler, R.B. Prestenting improves ureteroscopic stone-free rates. J. Endourol. 2007, 21, 1277–1280. [Google Scholar] [CrossRef]
| Variables | Total (N = 467) |
|---|---|
| Sex (Male/Female), n (%) | 303 (64.9)/164 (35.1) |
| Age (years), median (IQR) | 61 (21.0) |
| BMI (kg/m2), median (IQR) | 24.5 (5.5) |
| ECOG-PS ≥ 2, n (%) | 14 (3.0) |
| Medical history, n (%) | |
| Prior urolithiasis | 269 (57.6) |
| Diabetes mellitus | 94 (20.1) |
| Hyperparathyroidism | 12 (2.6) |
| Medication use, n (%) | |
| Anticoagulant/antiplatelet agents | 33 (7.1) |
| Corticosteroid, n (%) | 13 (2.8) |
| Upper ureteral stones: | |
| Max stone size (mm), median (IQR) | 11.9 (10.5) |
| Laterality (right/left/bilateral) | 211 (49.2)/230 (45.2)/26 (5.6) |
| Renal stones, n (%) | 88 (18.8) |
| Preoperative SIRS, n (%) | 63 (13.5) |
| Preoperative stenting, n (%) | 169 (36.2) |
| Hospital stay (days), median (IQR) | 5 (2) |
| Surgical waiting day (days), median (IQR) | 33 (29) |
| Operative time (min), median (IQR) | 70 (49) |
| Postoperative fever, n (%) | 32 (6.9) |
| Postoperative SIRS, n (%) | 27 (5.8) |
| Stone free rates, n (%) | 291 (62.3) |
| Referral patterns: | |
| Emergency department at our institution, n (%) | 82 (18) |
| From primary care clinics, n (%) | 157 (34) |
| From secondary/tertiary care hospitals, n (%) | 112 (24) |
| Others, n (%) | 116 (18) |
| Variables N = 467 | Before the COVID-19 n = 244 | After the COVID-19 n = 223 | p Value |
|---|---|---|---|
| Sex (Female), n (%) | 83 (34.0) | 81 (36.3) | 0.602 |
| Age (years), median (IQR) | 61 (19.0) | 60 (22.0) | 0.442 |
| BMI (kg/m2), median (IQR) | 24.5 (6.5) | 24.5 (4.7) | 0.200 |
| ECOG-PS ≥2, n (%) | 4 (1.6) | 10 (4.5) | 0.072 |
| Medical history, n (%) | |||
| Prior urolithiasis | 151 (61.9) | 118 (52.9) | 0.062 |
| Diabetes mellitus | 46 (18.9) | 48 (21.5) | 0.472 |
| Hyperparathyroidism | 4 (1.6) | 8 (3.6) | 0.300 |
| Medication use, n (%) | |||
| Anticoagulant/antiplatelet agents | 18 (7.4) | 15 (6.7) | 0.784 |
| Corticosteroid | 5 (2.0) | 8 (3.6) | 0.467 |
| Upper ureteral stones: | |||
| Max stone size (mm), median (IQR) | 12.0 (11.8) | 11.9 (10.2) | 0.073 |
| Renal stones, n (%) | 50 (20.5) | 38 (17.0) | 0.34 |
| Preoperative SIRS, n (%) | 29 (11.9) | 34 (15.3) | 0.288 |
| Preoperative stenting, n (%) | 74 (30.3) | 95 (42.6) | 0.006 |
| Hospital stay (days), median (IQR) | 5 (3.0) | 5 (1.0) | 0.032 |
| Surgical waiting day (days), median (IQR) | 36 (30) | 28 (28) | 0.005 |
| Operative times (min), median (IQR) | 77 (51.8) | 67 (43.0) | 0.018 |
| Postoperative fever, n (%) | 19 (7.8) | 13 (5.8) | 0.403 |
| Postoperative SIRS, n (%) | 15 (6.2) | 12 (5.4) | 0.723 |
| Stone free rates, n (%) | 160 (65.6) | 131 (58.7) | 0.128 |
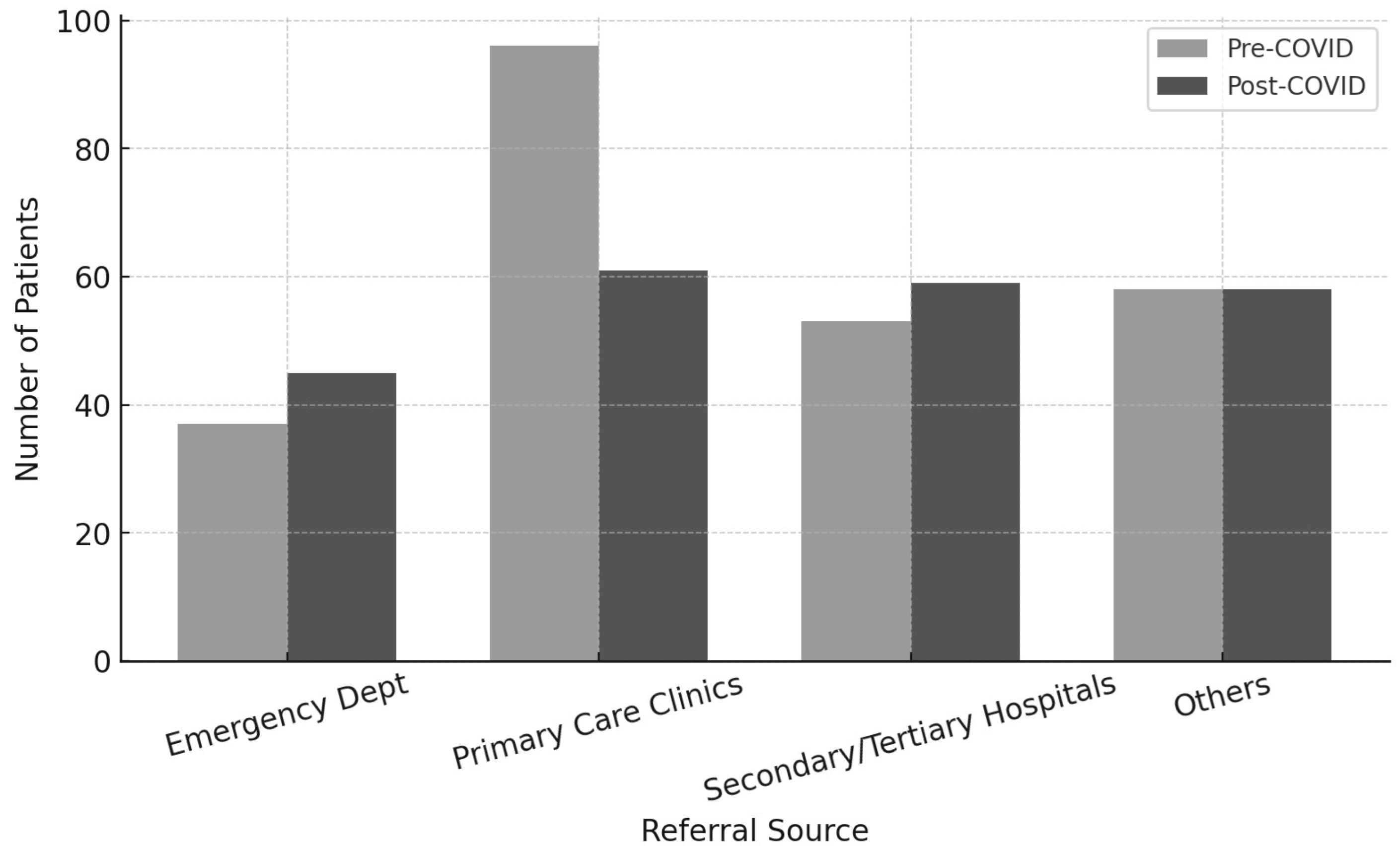
| Referral patterns: | 0.045 | ||
| Emergency department at our institution, n (%) | 37 (15) | 45 (20) | |
| From primary care clinics, n (%) | 96 (39) | 61 (27) | |
| From secondary/tertiary care hospitals, n (%) | 53 (22) | 59 (27) | |
| Others, n (%) | 58 (24) | 58 (26) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iijima, S.; Utsumi, T.; Ishitsuka, N.; Noro, T.; Suzuki, Y.; Sugizaki, Y.; Somoto, T.; Oka, R.; Endo, T.; Kamiya, N.; et al. Impact of COVID-19 on Ureteroscopy Management of Urolithiasis: Retrospective Comparative Study Before and After Pandemic. Appl. Sci. 2025, 15, 6101. https://doi.org/10.3390/app15116101
Iijima S, Utsumi T, Ishitsuka N, Noro T, Suzuki Y, Sugizaki Y, Somoto T, Oka R, Endo T, Kamiya N, et al. Impact of COVID-19 on Ureteroscopy Management of Urolithiasis: Retrospective Comparative Study Before and After Pandemic. Applied Sciences. 2025; 15(11):6101. https://doi.org/10.3390/app15116101
Chicago/Turabian StyleIijima, Shota, Takanobu Utsumi, Naoki Ishitsuka, Takahide Noro, Yuta Suzuki, Yuka Sugizaki, Takatoshi Somoto, Ryo Oka, Takumi Endo, Naoto Kamiya, and et al. 2025. "Impact of COVID-19 on Ureteroscopy Management of Urolithiasis: Retrospective Comparative Study Before and After Pandemic" Applied Sciences 15, no. 11: 6101. https://doi.org/10.3390/app15116101
APA StyleIijima, S., Utsumi, T., Ishitsuka, N., Noro, T., Suzuki, Y., Sugizaki, Y., Somoto, T., Oka, R., Endo, T., Kamiya, N., & Suzuki, H. (2025). Impact of COVID-19 on Ureteroscopy Management of Urolithiasis: Retrospective Comparative Study Before and After Pandemic. Applied Sciences, 15(11), 6101. https://doi.org/10.3390/app15116101







