Prevalence of Palatally Displaced Canines and Their Association with Dental and Skeletal Anomalies: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Study Design
2.3. Statistical Analysis
3. Results
3.1. Prevalence of PDC
3.2. Association of PDC with Dental Anomalies
3.3. Association of PDC with Skeletal Anomalies
3.4. Analysis of PDC by Type of Impaction
4. Discussion
Study Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PDC | Palatally displaced canines |
| CBCT | Cone beam computed tomography |
References
- Bharathi, R.; Jain, R.K.; Prasad, A.S. Association of vertical growth pattern with canine impactions in Dravidian subjects. J. Adv. Pharm. Technol. Res. 2022, 13 (Suppl. S1), S55–S58. [Google Scholar] [CrossRef] [PubMed]
- Dachi, S.F.; Howell, F.V. A survey of 3874 routine full-month radiographs: II. A study of impacted teeth. Oral. Surg. Oral. Med. Oral. Pathol. 1961, 14, 1165–1169. [Google Scholar] [CrossRef] [PubMed]
- Ericson, S.; Kurol, J. Radiographic examination of ectopically erupting maxillary canines. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Acar, Y.B.; Abuhan, E.; Boyacıyan, R.; Özdemir, F. Influence of facial type on attractiveness of vertical canine position from the perspective of orthodontists and laypeople. Angle Orthod. 2022, 92, 233–239. [Google Scholar] [CrossRef]
- Coulter, J.; Richardson, A. Normal eruption of the maxillary canine quantified in three dimensions. Eur. J. Orthod. 1997, 19, 171–183. [Google Scholar] [CrossRef]
- Haavikko, K. The formation and the alveolar and clinical eruption of the permanent teeth. An orthopantomographic study. Suom. Hammaslaak. Toim. 1970, 66, 103–170. [Google Scholar]
- Becker, A.; Zilberman, Y.; Tsur, B. Root length of lateral incisors adjacent to palatally-displaced maxillary cuspids. Angle Orthod. 1984, 54, 218–225. [Google Scholar] [CrossRef]
- Becker, A.; Chaushu, S. Etiology of maxillary canine impaction: A review. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 557–567. [Google Scholar] [CrossRef]
- Sacerdoti, R.; Baccetti, T. Dentoskeletal features associated with unilateral or bilateral palatal displacement of maxillary canines. Angle Orthod. 2004, 74, 725–732. [Google Scholar] [CrossRef]
- Becker, A.; Smith, P.; Behar, R. The incidence of anomalous maxillary lateral incisors in relation to palatally-displaced cuspids. Angle Orthod. 1981, 51, 24–29. [Google Scholar] [CrossRef]
- Oliver, R.G.; Mannion, J.E.; Robinson, J.M. Morphology of the maxillary lateral incisor in cases of unilateral impaction of the maxillary canine. Br. J. Orthod. 1989, 16, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Janani, A.; Asghari, M.; Maleki, A.; Ziaie, P.; Mahjoub, P. The prevalence of ectopically maxillary canine and related factors in an iranian population: A retrospective study. J. Dentomaxillofacial Radiol. Pathol. Surg. 2021, 10, 16–19. [Google Scholar]
- Rahamneh, A.; Al-Weshah, M.; Ghozlan, M.; Smadi, H.; Abu-Odeh, R. Prevalence and severity of ectopic maxillary canine impaction in Southern Jordanian population: A radiographic sector analysis. J. R. Med. Serv. 2017, 24, 38–44. [Google Scholar] [CrossRef]
- Cicek, O.; Gurel, T.; Demir Cicek, B. Investigation of the Relationship of Impacted Maxillary Canines with Orthodontic Malocclusion: A Retrospective Study. Children 2023, 10, 950. [Google Scholar] [CrossRef]
- Dash, B.P.; Ramanna, P.K.; Sam, G.; Santhakumari, P.P.; Naik, M.K.; Das, A. Prevalence of Ectopic Canine in Different Sagittal and Vertical Skeletal Patterns. J. Contemp. Dent. Pract. 2023, 24, 268–273. [Google Scholar] [CrossRef]
- Lövgren, M.L.; Dahl, O.; Uribe, P.; Ransjö, M.; Westerlund, A. Prevalence of impacted maxillary canines-an epidemiological study in a region with systematically implemented interceptive treatment. Eur. J. Orthod. 2019, 41, 454–459. [Google Scholar] [CrossRef]
- Al Balbeesi, H.O.; Al Kawari, H.M.; Al Tamimi, A.S.; Al Mubarak, I.; Al Ibrahim, K.I.; Divakar, D.D. Association Between Canine Impaction and Skeletal Pattern in the Sagittal and Vertical Planes. Int. J. Periodontics Restor. Dent. 2020, 40, 253–259. [Google Scholar] [CrossRef]
- Katsnelson, A.; Flick, W.G.; Susarla, S.; Tartakovsky, J.V.; Miloro, M. Use of panoramic x-ray to determine position of impacted maxillary canines. J. Oral. Maxillofac. Surg. 2010, 68, 996–1000. [Google Scholar] [CrossRef]
- Ravi, I.; Srinivasan, B.; Kailasam, V. Radiographic predictors of maxillary canine impaction in mixed and early permanent dentition—A systematic review and meta-analysis. Int. Orthod. 2021, 19, 548–565. [Google Scholar] [CrossRef]
- Shin, J.H.; Oh, S.; Kim, H.; Lee, E.; Lee, S.M.; Ko, C.C.; Kim, Y.I. Prediction of maxillary canine impaction using eruption pathway and angular measurement on panoramic radiographs. Angle Orthod. 2022, 92, 18–26. [Google Scholar] [CrossRef]
- Bishara, S.E. Impacted maxillary canines: A review. Am. J. Orthod. Dentofac. Orthop. 1992, 101, 159–171. [Google Scholar] [CrossRef]
- Sambataro, S.; Baccetti, T.; Franchi, L.; Antonini, F. Early predictive variables for upper canine impaction as derived from posteroanterior cephalograms. Angle Orthod. 2005, 75, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Alqerban, A.; Jacobs, R.; Fieuws, S.; Willems, G. Comparison of two cone beam computed tomographic systems versus panoramic imaging for localization of impacted maxillary canines and detection of root resorption. Eur. J. Orthod. 2011, 33, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Alqerban, A.; Jacobs, R.; Fieuws, S.; Willems, G. Radiographic predictors for maxillary canine impaction. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Dilip Kumar, M.; Bhadrinath, S.; Balika, J.C.; Umamageshwari, A.; Deepa, S. Prediction of Favorability of Maxillary Canine Impaction Using Artificial Intelligence Algorithm. J. Indian. Orthod. Soc. 2024, 58, 291–302. [Google Scholar] [CrossRef]
- Becker, A.; Gillis, I.; Shpack, N. The etiology of palatal displacement of maxillary canines. Clin. Orthod. Res. 1999, 2, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Peck, S.; Peck, L.; Kataja, M. The palatally displaced canine as a dental anomaly of genetic origin. Angle Orthod. 1994, 64, 249–256. [Google Scholar] [CrossRef]
- Mossey, P.A.; Campbell, H.M.; Luffingham, J.K. The palatal canine and the adjacent lateral incisor: A study of a west of Scotland population. Br. J. Orthod. 1994, 21, 169–174. [Google Scholar] [CrossRef]
- Zilberman, Y.; Cohen, B.; Becker, A. Familial trends in palatal canines, anomalous lateral incisors, and related phenomena. Eur. J. Orthod. 1990, 12, 135–139. [Google Scholar] [CrossRef]
- Jang, E.; Lee, K.; An, S.; Song, J.; Ra, J. Retrospective Study of Association between Displacement of Maxillary Canine and Tooth Agenesis. J. Clin. Pediatr. Dent. 2015, 39, 488–492. [Google Scholar] [CrossRef]
- Stahl, F.; Grabowski, R. Maxillary canine displacement and genetically determined predisposition to disturbed development of the dentition. J. Orofac. Orthop. 2003, 64, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Sajnani, A.K.; King, N.M. Dental anomalies associated with buccally- and palatally-impacted maxillary canines. J. Investig. Clin. Dent. 2014, 5, 208–213. [Google Scholar] [CrossRef]
- Leifert, S.; Jonas, I.E. Dental anomalies as a microsymptomof palatal canine displacement. J. Orofac. Orthop. 2003, 64, 108–120. [Google Scholar] [CrossRef]
- Al-Nimri, K.; Gharaibeh, T. Space conditions and dental and occlusal features in patients with palatally impacted maxillary canines: An aetiological study. Eur. J. Orthod. 2005, 27, 461–465. [Google Scholar] [CrossRef]
- Baccetti, T. A controlled study of associated dental anomalies. Angle Orthod. 1998, 68, 267–274. [Google Scholar] [CrossRef]
- Herrera-Atoche, J.R.; Agüayo-de-Pau, M.D.; Escoffié-Ramírez, M.; Aguilar-Ayala, F.J.; Carrillo-Ávila, B.A.; Rejón-Peraza, M.E. Impacted Maxillary Canine Prevalence and Its Association with Other Dental Anomalies in a Mexican Population. Int. J. Dent. 2017, 2017, 7326061. [Google Scholar] [CrossRef]
- Segura, J.J.; Hattab, F.; Ríos, V. Maxillary canine transpositions in two brothers and one sister: Associated dental anomalies and genetic basis. ASDC J. Dent. Child. 2002, 69, 54–58. [Google Scholar] [PubMed]
- Jacoby, H. The etiology of maxillary canine impactions. Am. J. Orthod. 1983, 84, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E. Clinical management of impacted maxillary canines. Semin. Orthod. 1998, 4, 87–98. [Google Scholar] [CrossRef]
- Becker, A.; Chaushu, S. Dental age in maxillary canine ectopia. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 657–662. [Google Scholar] [CrossRef]
- Pirinen, S.; Arte, S.; Apajalahti, S. Palatal displacement of canine is genetic and related to congenital absence of teeth. J. Dent. Res. 1996, 75, 1742–1746. [Google Scholar] [CrossRef] [PubMed]
- Larsen, H.J.; Sørensen, H.B.; Artmann, L.; Christensen, I.J.; Kjaer, I. Sagittal, vertical and transversal dimensions of the maxillary complex in patients with ectopic maxillary canines. Orthod. Craniofacial Res. 2010, 13, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Cernochova, P.; Izakovicova-Holla, L. Dentoskeletal characteristics in patients with palatally and buccallydisplaced maxillary permanent canines. Eur. J. Orthod. 2012, 34, 754–761. [Google Scholar] [CrossRef]
- Pop, S.I.; Contac, L.R.; Ghiman, A.; Moldovan, D.; Suciu, V.; Kantor, J.; Bratu, D.C.; Buduru, S.D. Evaluation of the correlation between impacted canine and malocclusions. Acta Stomatol. Marisiensis J. 2020, 3, 275–281. [Google Scholar] [CrossRef]
- Basdra, E.K.; Kiokpasoglou, M.; Stellzig, A. The Class II Division 2 craniofacial type is associated with numerous congenital tooth anomalies. Eur. J. Orthod. 2000, 22, 529–535. [Google Scholar] [CrossRef]
- Ajami, S.; Shahidi, S.; Azadeh, N.; Nasr Jalali, H.; Zare, M. Difficulty of palatal impacted canine treatment in different sagittal and vertical skeletal malocclusions: A retrospective 3D evaluation. Int. Orthod. 2020, 18, 89–95. [Google Scholar] [CrossRef]
- Jiménez-Silva, A.; Carnevali-Arellano, R.; Vivanco-Coke, S.; Tobar-Reyes, J.; Araya-Díaz, P.; Palomino-Montenegro, H. Prediction methods of maxillary canine impaction: A systematic review. Acta Odontol. Scand. 2022, 80, 51–64. [Google Scholar] [CrossRef]
- Kolokitha, O.E.; Balli, D.; Zarkadi, A.E.; Gizani, S. Association between maxillary canine impaction and other dental anomalies: Radiological study of a mixed dentition children’s cohort from an orthodontic clinic. Eur. Arch. Paediatr. Dent. 2023, 24, 401–407. [Google Scholar] [CrossRef]
- Laurenziello, M.; Montaruli, G.; Gallo, C.; Tepedino, M.; Guida, L.; Perillo, L.; Troiano, G.; Lo Muzio, L.; Ciavarella, D. Determinants of maxillary canine impaction: Retrospective clinical and radiographic study. J. Clin. Exp. Dent. 2017, 9, e1304–e1309. [Google Scholar] [CrossRef]
- Willems, G.; Butaye, C.; Raes, M.; Zong, C.; Begnoni, G.; Cadenas de Llano-Pérula, M. Early prevention of maxillary canine impaction: A randomized clinical trial. Eur. J. Orthod. 2023, 45, 359–369. [Google Scholar] [CrossRef]
- Uzunçıbuk, H.; Marrapodi, M.M.; Fiorillo, L.; Meto, A.; Cicciù, M.; Minervini, G. The influence of orthopedic rapid maxillary expansion on the deviation of the nasal septum. J. Clin. Pediatr. Dent. 2024, 48, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Aktı, A.; Dolunay, U.; Kaya, D.I.; Gürses, G.; Yeşil, D. Evaluation of the Relationship between Impacted Maxillary Canine Teeth and Root Resorption in Adjacent Teeth: A Cross-Sectional Cone Beam Computed Tomography Study. Diagnostics 2024, 14, 1470. [Google Scholar] [CrossRef] [PubMed]
- Golez, A.; Vrcon, C.; Ovsenik, M. Jaw Morphology and Factors Associated with Upper Impacted Canines: Case-Controlled Trial. Appl. Sci. 2024, 14, 7700. [Google Scholar] [CrossRef]
- Kuftinec, M.M.; Shapira, Y. The impacted maxillary canine: I. Review of concepts. ASDC J. Dent. Child. 1995, 62, 317–324. [Google Scholar]
- Bazargani, F.; Magnuson, A.; Lennartsson, B. Effect of interceptive extraction of deciduous canine on palatally displaced maxillary canine: A prospective randomized controlled study. Angle Orthod. 2014, 84, 3–10. [Google Scholar] [CrossRef]
- Law, C.S. Management of premature primary tooth loss in the child patient. J. Calif. Dent. Assoc. 2013, 41, 612–618. [Google Scholar] [CrossRef]
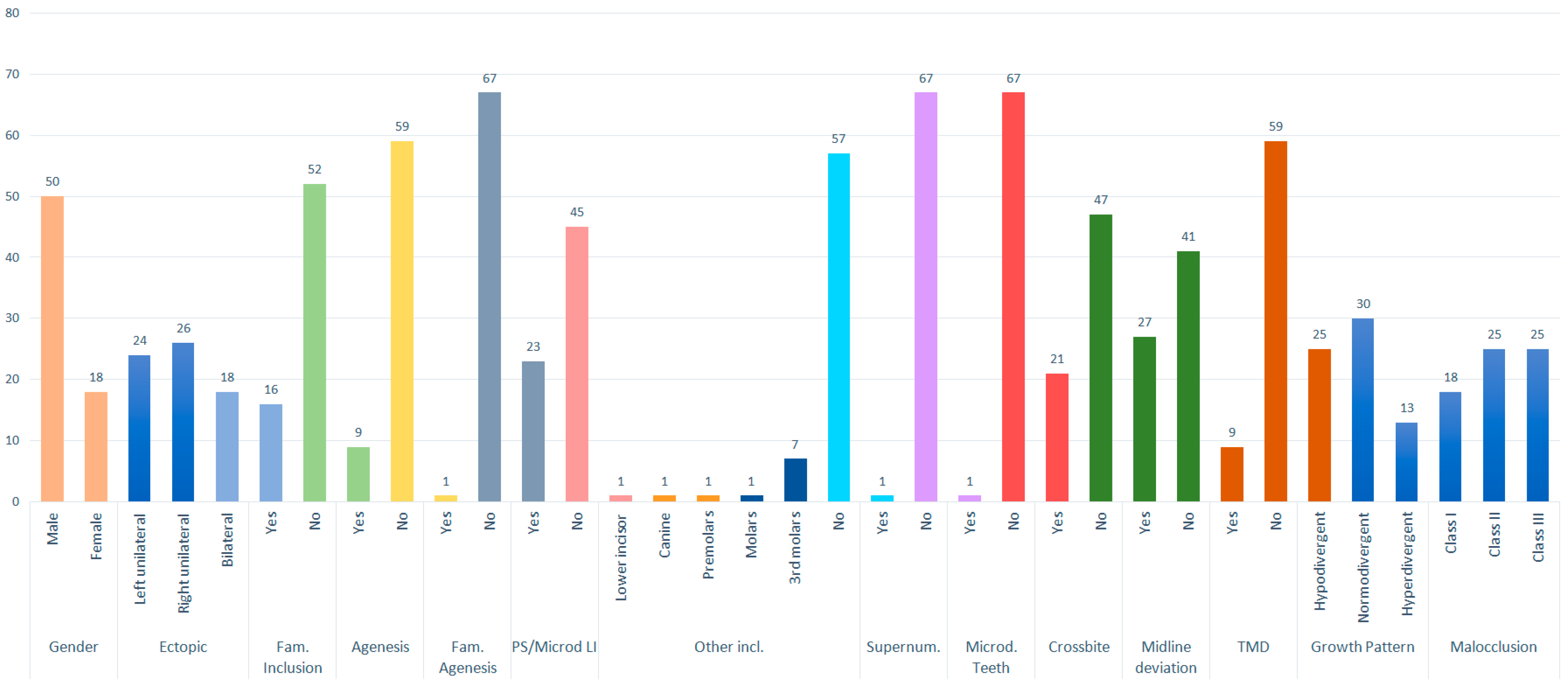
| Prevalence | Percent | ||
|---|---|---|---|
| Gender | Female | 50 | 73.5 |
| Male | 18 | 26.5 | |
| Total | 68 | 100.0 | |
| Ectopic | Left unilateral | 24 | 35.3 |
| Right unilateral | 26 | 38.2 | |
| Bilateral | 18 | 26.5 | |
| Total | 68 | 100.0 | |
| Family history of canine impaction | Yes | 16 | 23.5 |
| No | 52 | 76.5 | |
| Total | 68 | 100.0 | |
| Presence of agenesis | Yes | 9 | 13.2 |
| No | 59 | 86.8 | |
| Total | 68 | 100.0 | |
| Family history of agenesis | Yes | 1 | 1.5 |
| No | 67 | 98.5 | |
| Total | 68 | 100.0 | |
| Conoid or microdontic lateral incisors | Yes | 23 | 33.8 |
| No | 45 | 66.2 | |
| Total | 68 | 100.0 | |
| Other inclusions | Lateral incisor | 1 | 1.5 |
| Lower canine | 1 | 1.5 | |
| Premolars | 1 | 1.5 | |
| Molars | 1 | 1.5 | |
| Third molars | 7 | 10.2 | |
| No | 57 | 83.8 | |
| Total | 68 | 100.0 | |
| Supernumerary teeth | Yes | 1 | 1.5 |
| No | 67 | 98.5 | |
| Total | 68 | 100.0 | |
| Microdontic dentition | Yes | 1 | 1.5 |
| No | 67 | 98.5 | |
| Total | 68 | 100.0 | |
| Crossbite | Yes | 21 | 30.8 |
| No | 47 | 69.1 | |
| Total | 68 | 100.0 | |
| Upper dental midline deviation | Yes | 27 | 39.7 |
| No | 41 | 60.3 | |
| Total | 68 | 100.0 | |
| Growth pattern | Hypodivergent | 25 | 36.8 |
| Normodivergent | 30 | 44.1 | |
| Hyperdivergent | 13 | 19.1 | |
| Total | 68 | 100.0 | |
| Malocclusion | Class I | 18 | 26.47 |
| Class II | 25 | 36.76 | |
| Class III | 25 | 36.76 | |
| Total | 68 | 100.0 |
| Palatally Displaced Canines | |||||||
| 13–23 | 13 | 23 | Total | Fisher | p-value | ||
| Gender | Female | 28.0% | 34.0% | 38.0% | 100% | 1.38 | p = 0.51 |
| Male | 22.2% | 50.0% | 27.8% | 100% | |||
| Upper dental midline deviation | Right | 11.1% | 83.3% | 5.6% | 100% | 17.04 | p < 0.05 * |
| Left | 0% | 18.2% | 81.8% | 100% | |||
| Family history | No | 28.8% | 26.9% | 44.2% | 100% | 12.56 | p < 0.05 * |
| Yes | 18.8% | 75.0% | 6.3% | 100% | |||
| Agenesis | No | 26.8% | 39.3% | 33.9% | 100% | 0.36 | p = 0.92 |
| Yes | 25.0% | 33.3% | 41.7% | 100% | |||
| Conoid incisors | No | 33.3% | 44.4% | 22.2% | 100% | 9.58 | p < 0.05 * |
| Yes | 13.0% | 26.1% | 60.9% | 100% | |||
| Crossbite | No | 27.6% | 42.6% | 29.8% | 100% | 2.07 | p = 0.36 |
| Yes | 23.8% | 28.6% | 47.6% | 100% | |||
| Growth pattern | Hypodivergent | 31.2% | 37.5% | 31.3% | 100% | 2.11 | p = 0.76 |
| Normodivergent | 27.2% | 45.5% | 27.2% | 100% | |||
| Hyperdivergent | 14.3% | 28.6% | 57.1% | 100% | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-González, A.; Montes-Díaz, M.E.; Gallardo-López, N.E.; Colino-Gallardo, P.; Criado-Pérez, L.; Alvarado-Lorenzo, A. Prevalence of Palatally Displaced Canines and Their Association with Dental and Skeletal Anomalies: A Retrospective Study. Appl. Sci. 2025, 15, 5862. https://doi.org/10.3390/app15115862
Martínez-González A, Montes-Díaz ME, Gallardo-López NE, Colino-Gallardo P, Criado-Pérez L, Alvarado-Lorenzo A. Prevalence of Palatally Displaced Canines and Their Association with Dental and Skeletal Anomalies: A Retrospective Study. Applied Sciences. 2025; 15(11):5862. https://doi.org/10.3390/app15115862
Chicago/Turabian StyleMartínez-González, Alicia, María Elena Montes-Díaz, Nuria Esther Gallardo-López, Pedro Colino-Gallardo, Laura Criado-Pérez, and Alfonso Alvarado-Lorenzo. 2025. "Prevalence of Palatally Displaced Canines and Their Association with Dental and Skeletal Anomalies: A Retrospective Study" Applied Sciences 15, no. 11: 5862. https://doi.org/10.3390/app15115862
APA StyleMartínez-González, A., Montes-Díaz, M. E., Gallardo-López, N. E., Colino-Gallardo, P., Criado-Pérez, L., & Alvarado-Lorenzo, A. (2025). Prevalence of Palatally Displaced Canines and Their Association with Dental and Skeletal Anomalies: A Retrospective Study. Applied Sciences, 15(11), 5862. https://doi.org/10.3390/app15115862







