1. Introduction
Hygiene and infection control are essential in dental practices. Because of the increased risk of cross-contamination and infection transmission, rigorous disinfection protocols are essential to protect patients’ and dental staff’s health. Studies have highlighted the potential spread of infections if protocols are not rigorously enforced, emphasizing that effective disinfection of equipment and surfaces is important in minimizing the risk of healthcare-associated infections [
1,
2,
3]. Dental professionals increasingly rely on chemical disinfectants for air and surface sterilization [
4,
5]. Although rigorous hygiene in dental offices is essential for preventing nosocomial infections, the frequent use of chemical disinfectants may pose risks to staff and patients, and caution and standardization of their use are needed [
6]. The widespread implementation of surface disinfection protocols in medical and dental settings has been significantly intensified following the COVID-19 pandemic. While these measures aim to reduce microbial transmission, the increased use of potent chemical disinfectants—particularly those containing peracetic acid (PA), hydrogen peroxide (HA), and acetic acid (AA)—has raised important concerns about occupational exposure and its potential short- and long-term health effects on healthcare personnel [
7,
8,
9].
Oxycide™ (Ecolab, Copenhagen, Denmark) is a powerful air and surface oxidative disinfectant for medical and dental facilities. Oxycide™ is composed of PAA (0.13%), HA (0.64%), and acetic acid (AA) (0.16%). This combination allows it to effectively target and kill a broad spectrum of pathogens, including bacteria, viruses, and spores, making it valuable and often used in healthcare environments with a high risk of infection transmission. Oxycide™’s oxidative mechanism of action allows rapid destruction of microbial cell structures, thus providing enhanced antimicrobial activity against highly resistant pathogens, such as Clostridium difficile, methicillin-resistant Staphylococcus aureus (MRSA), and vancomycin-resistant enterococci (VRE) [
10,
11,
12]. In healthcare environments, occupational exposure to PAA, HP, and AA can cause various health problems for workers in the short and long term. Acute exposure to PAA, HP, and AA can cause immediate respiratory symptoms such as nasal and throat irritation, cough, wheezing, and shortness of breath. Other studies have reported that although Oxycide™ is advertised as effective and biodegradable, repeated exposure has been associated with airway irritation, allergic reactions, and skin damage in people who come into contact with it [
7,
10,
13,
14]. Regarding long-term health effects, prolonged exposure to PAA and HP can lead to chronic respiratory conditions, including occupational asthma [
15,
16,
17]. This is due to the sensitization mechanism triggered by repeated exposure to these chemicals, which can cause persistent inflammation and hyperreactivity of the airways [
18,
19]. While exposure levels in healthcare settings are often below established occupational exposure limits, continuous monitoring and assessment are crucial to ensuring safety [
15,
20]. Despite some manufacturers’ claims that no PPE is required when using diluted products, appropriate PPE, such as masks and gloves, is recommended to minimize exposure and protect workers’ health [
14,
21]. Exploring non-chemical disinfection technologies could reduce reliance on these hazardous chemicals and decrease the associated health risks for healthcare workers [
7]. Additionally, the implementation of robust occupational health programs and regular health surveillance can help identify at-risk workers early and mitigate potential health issues [
21].
In addition to disinfectant agents, dental practice involves using various other materials—such as endodontic irrigants [
22], impression compounds, and restorative materials [
23]—that may carry health risks upon exposure. These materials can release irritant or sensitizing compounds.
The rationale for conducting this study stemmed from a series of informal reports and recurrent complaints from dental staff regarding respiratory, ocular, and dermal symptoms following routine disinfection procedures. These observations raised concerns about potential occupational exposure to disinfectant vapors, particularly in treatment rooms lacking proper mechanical ventilation. Although these symptoms were not formally documented earlier, their frequency and consistency across clinics prompted us to investigate whether a broader pattern was linked to disinfectant use—specifically Oxycide™. These observations led us to hypothesize that safety protocols and ventilation were violated. It formed the basis for rigorously assessing dental staff symptom prevalence, PPE use, and ambient circumstances.
According to the manufacturer, Oxycide™ should be diluted using Ecolab’s automated system at a ratio of 23 mL per 1 L of water. The solution is to be applied using wipes, ensuring that surfaces remain visibly wet for at least five minutes for effective microbial action. Adequate ventilation during and after application is essential to prevent the accumulation of vapors and ensure a safe working environment [
24]. While some manufacturers suggest that PPE is not required for diluted solutions, the use of gloves, masks, and eye protection is recommended to minimize exposure [
24].
This study aims to investigate the potential link between insufficient protection and improper application of Oxycide™ and the incidence of acute health symptoms in dental personnel in light of the growing dependence on chemical disinfectants in dental environments, given the increased reliance on chemical disinfectants in dental settings; it is essential to balance infection control with occupational safety. Based on existing research on PAA and HP exposure, this study examines the relationship between inadequate use of PPE, improper use of Oxycide™, and acute symptoms among dental personnel. The authors hypothesize that poor compliance with safety protocols and lack of proper ventilation significantly contribute to the risk and duration of these adverse effects.
2. Materials and Methods
This observational cross-sectional study was conducted between January and March 2025, involving a sample of 200 dental assistants actively working in dental clinics, with a minimum of three months’ employment at the current dental clinic prior to participation, with exclusive use of Oxycide™ as disinfectant. Each participant personally prepared and applied the disinfectant to surfaces in the dental office between patients, such as dental chairs, countertops, instrument trays, work surfaces, and occasionally floors. Personal with pre-existing chronic respiratory or dermatological conditions that could confound the assessment of symptoms were excluded. Data were collected through an anonymous, structured questionnaire distributed online via Google Forms. The questionnaire included sections on demographic characteristics, the use of personal protective equipment (PPE), disinfectant usage practices, self-reported symptoms, and contextual environmental factors, primarily using closed-ended questions. All study participants confirmed that they were familiar with the Oxycide™ disinfectant protocol.
All participants in this study were adequately informed regarding the study’s objective, and consent was obtained prior to their participation.
The sample size of 200 participants was not determined through an a priori power analysis, as the study employed a non-probabilistic convenience sampling strategy via voluntary online responses from dental assistants. A post hoc power analysis was conducted on key chi-square tests to evaluate the statistical validity retrospectively. For example, one significant association (χ2(2) = 8.712, p = 0.013) yielded a Cramér’s V of 0.21, indicating a medium effect size. With N = 200 and α = 0.05, the estimated power was approximately 0.80. These results suggest that the study was adequately powered to detect medium-sized effects. Nonetheless, using non-random sampling limits the generalizability of the findings, which should be considered when interpreting the results.
Three dental professionals reviewed the questionnaire to ensure content validity. Based on their input, the items were improved for relevancy and clarity. A pilot test was conducted with 20 dental assistants (not included in the main study) to assess comprehensibility, internal consistency, and completion time. Minor adjustments were made based on the pilot findings. The variables recorded included demographics (sex, age), PPE usage (type and frequency), disinfection technique (dose compliance, drying time), symptoms (type and duration), symptom onset timing, and room characteristics (presence of ventilation).
Descriptive analysis was performed, and the frequencies of distribution were calculated in percentages. Proportions were compared using chi-squared tests, with p-values < 0.05 accepted as statistically significant. The data were analyzed using SPSS version 25 and Microsoft Excel 365. Cross-tabulations were performed to explore associations between variables such as duration of symptoms and room ventilation.
The participants in this study were 72% female and 28% male, ranging from 22 to 65 years old (
Table 1).
Symptoms were grouped into categories such as respiratory symptoms (irritation of the nasal mucosa, dry cough, rhinorrhea), ocular symptoms (burning), dermal symptoms (dermatitis), headache, and transient facial edema. The participants were asked to report the presence, type, and duration of any symptoms they experienced after using Oxycide™. Each symptom was self-reported using a structured checklist developed for this study.
4. Discussion
The present study highlights an important occupational health problem in dental offices: the health effects of exposure to Oxycide™ disinfectant among dental professionals, with a focus on symptom prevalence, contributing procedural and environmental factors, and the role of protective measures. The findings show that Oxycide™, a peracetic acid-based surface disinfectant, can cause a wide range of acute irritative symptoms, even under normal use conditions in dental settings. The proportion of affected staff (63%) is unusually high, suggesting that either Oxycide™ has a significant irritant potential or that the way it was used led to exposures above the level considered safe. These results are in line with reports in the literature on the adverse effects of disinfectants of this type on healthcare workers [
7,
13]. According to the product data sheet, Oxycide™ can cause severe eye and respiratory irritation when in contact with aerosols, and it is mandatory to wear appropriate protective equipment and ensure ventilation of the space during use [
25].
The most common symptoms mentioned were ocular irritation, dry cough, nasal mucosa pain, and rhinorrhea, which affected 63% of the subjects. Clinical reports and occupational health evaluations have recorded similar symptoms in healthcare workers exposed to PAA-based disinfectants, such as eye burning, throat irritation, and respiratory problems [
7,
26]. Hawley et al. found that healthcare workers who used PAA-hydrogen peroxide disinfectants frequently reported symptoms such as wet eyes and coughing after repeated use [
13]. Many studies have shown that extended exposure to disinfectants by healthcare workers has been linked to several long-term health consequences, with the skin and respiratory systems being the most affected. The need to uphold strict sanitation standards in order to prevent illnesses linked to healthcare exacerbates these consequences. In order to minimize the harmful effects of disinfectants on dental practice personnel, consistent use of personal protective equipment (PPE) is crucial, as it offers substantial protection against inhalation- and contact-related irritative effects during disinfection processes [
27]. For instance, a study by Blackley et al. found that the consistent use of gloves and masks significantly reduces respiratory and skin irritation among healthcare workers using chemical disinfectants in clinical settings [
7]. Insufficient ventilation and inadequate use of personal protective equipment (PPE) are key risk factors that exacerbate the health impacts of disinfectant exposure. Improving workplace ventilation and ensuring consistent use of PPE are critical strategies to mitigate these risks [
28,
29].
One of the most robust findings of this study is the statistically significant association between the level of personal protective equipment (PPE) used and the duration of symptoms following Oxycide™ exposure (χ
2 = 34.576, df = 4,
p < 0.001). Participants who used full PPE—including facial masks, gloves, and protective goggles—reported the lowest proportion of prolonged symptoms, with no cases exceeding 30 min. In contrast, those who used only gloves or no PPE at all experienced a markedly higher frequency of symptoms lasting more than 30 min. This outcome aligns with international occupational safety recommendations, which emphasize the importance of PPE in minimizing chemical exposure risk [
30]. Our findings reinforce these guidelines, demonstrating that complete and consistent use of PPE offers substantial protection against inhalation- and contact-related irritative effects during Oxycide™ application. Ventilation also plays a protective role. Ventilation was found to play a statistically significant protective role. The results revealed a significant association between room ventilation and symptom duration (χ
2(2, N = 200) = 8.712,
p = 0.013). Participants who worked in ventilated rooms (i.e., rooms with windows) were significantly more likely to report either no symptoms or symptoms of short duration. In contrast, individuals working in non-ventilated environments exhibited a higher proportion of prolonged symptoms. These findings support the notion that adequate ventilation can help reduce both the incidence and persistence of symptoms related to chemical disinfectant exposure. This aligns with previous research highlighting the importance of air exchange rates in environments where such substances are used, reinforcing the recommendation to keep treatment areas well-ventilated during and after disinfectant application. Previous studies have emphasized the importance of air exchange rates in rooms where chemical disinfectants are used [
20]. In this case, the evidence supports practical suggestions to maintain treatment rooms aired during and after disinfectant application.
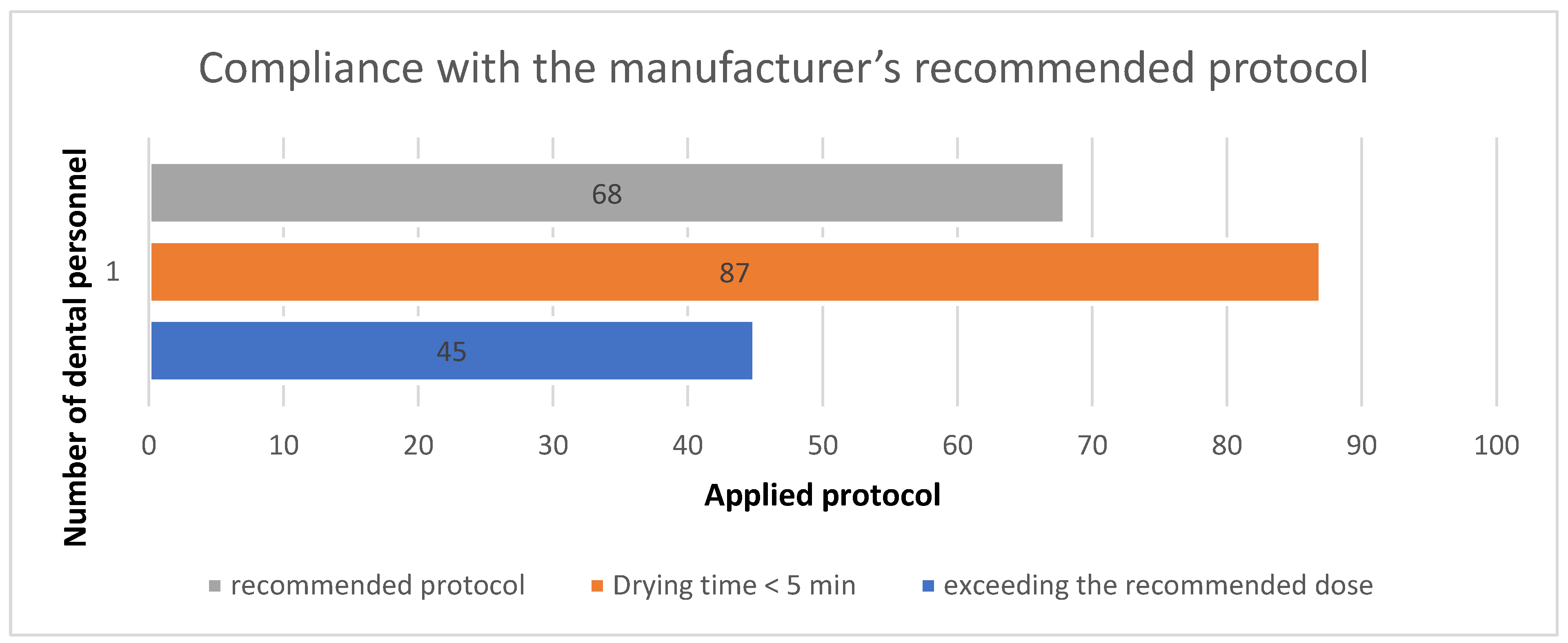
While protocol compliance—particularly with regard to recommended dose and drying time—was initially hypothesized to influence symptom onset, the statistical analysis did not confirm a significant association (χ
2(4) = 9.20,
p = 0.056). Nonetheless, the distribution of responses indicates a potential trend: personnel who deviated from the recommended protocol, either by exceeding the dose or allowing insufficient drying time, reported a higher proportion of early symptom onset (within 0–4 min). Although these results did not reach statistical significance, they remain consistent with previous findings suggesting that improper application techniques may elevate airborne concentrations of irritants and increase the likelihood of acute mucosal responses. Importantly, these findings do not undermine the value of the recommended protocol; on the contrary, proper adherence continues to represent a best practice for minimizing the risk of adverse effects. This is consistent with previous reports suggesting that improper application of high-level disinfectants (e.g., overdosing or aerosolizing) increases airborne irritant concentrations and contributes to acute mucosal reactions [
31]. Several occupational safety assessments have discouraged spray application of PAA disinfectants and recommend wipe-based techniques instead, precisely to reduce aerosol formation [
32]. In this study, a wipe-based application was used for applying the OxyCide™ disinfectant. All participants reported applying the disinfectant manually using cloths or wipes soaked in the diluted solution, not via spray bottles or aerosolized systems. This is consistent with occupational safety guidelines that discourage spray application of peracetic acid (PAA)-based disinfectants due to the risk of aerosol formation and increased inhalation exposure. However, despite using wipes, symptoms were still reported—likely due to excessive volume applied, insufficient drying time, and poor ventilation, all of which can still result in the off-gassing of irritant vapors.
The distribution of reported symptoms following Oxycide™ exposure highlights the predominance of mucosal and respiratory irritation, with burning sensation in the eyes, irritative dry cough, and nasal mucosa irritation being the most frequently cited. However, the chi-square test did not reveal a statistically significant association between the type of personal protective equipment (PPE) used and the specific symptoms reported (χ2(28, N = 200) = 25.20, p = 0.617). This lack of statistical association suggests that within this sample, the type of PPE worn may not have significantly influenced the manifestation of specific symptoms. It is possible that exposure occurred despite PPE use, due to improper application or limitations in protective efficacy. Further studies with larger samples and more balanced symptom distribution are needed to better understand the role of PPE in modulating the types of symptoms experienced.
A notable aspect is the occurrence of symptoms even in people with no allergic history, suggesting a predominantly irritant (non-immunologic) mechanism of the reactions. Peracetic acid and hydrogen peroxide vapors may act as direct irritants, triggering local mucosal inflammation, irrespective of allergic predisposition. At the same time, severe cases (such as angioedema) raise the suspicion that in some individuals, there may also be a component of hypersensitization or a particular individual vulnerability. Differences in the onset and duration of symptoms observed (immediate in some, delayed, and persistent in others) can be explained by varying levels of exposure and individual sensitivity [
8]. Another important factor to be discussed is the lack of clear post-disinfection instructions in the Oxycide™ product documentation, which has led to uncertainty about the steps to follow after the contact time has expired. The absence of a surface wiping or rinsing step and explicit recommendations to ventilate rooms meant that irritating residues persisted on surfaces and in the air, coming into contact with the skin and mucous membranes of staff and patients. Standardizing these steps could significantly reduce unnecessary exposure. Overall, it is suggested that the problems identified are caused not only by the disinfectant but also by the way of application and compliance with appropriate protective measures. By addressing both aspects (product choice and use procedures), a safer working environment can be achieved [
31].
While some factors (for example, room ventilation) approached significance without meeting standard thresholds, such patterns remain useful in occupational health research. In chemical exposure settings, even little changes in ambient conditions or procedure compliance can result in measurable symptom decreases. These findings support simple, low-cost interventions—such as respecting drying time, boosting air exchange, and using the proper dose—that can significantly improve worker safety in dentistry clinics.
One of the primary limitations of this study is the absence of a control group, which compromises our capacity to ascribe the stated symptoms to the use of Oxycide™ disinfectant. It is difficult to tell the difference between the effects of Oxycide™ and other possible environmental or occupational variables without a reference group of dental professionals not exposed to this disinfectant. The study’s cross-sectional design also precludes us from determining causal links between symptom severity, techniques of disinfectant administration, and PPE use. Self-reported data, which may be affected by recall bias or misreporting, especially concerning symptom frequency and severity, is another restriction.
Future studies should seek to solve these constraints by including a control group, including dentistry practitioners operating under varying disinfection policies or those not utilizing Oxycide™. Longitudinal studies could offer an insightful analysis of the long-term consequences of regular disinfectant contact and PPE use. Furthermore, objective exposure measurements like air quality monitoring or direct measurement of volatile component levels would provide more knowledge of the link between disinfectant use, PPE compliance, and symptom onset. Increasing the sample size would also improve the generalizability of the results.
5. Conclusions
This study highlights a significant occupational health concern in dental practices: exposure to the disinfectant Oxycide™ is associated with a considerable incidence of acute symptoms, particularly respiratory and skin irritation. Data collected from 200 dental assistants indicate that improper use of the product—combined with inadequate personal protection and insufficient ventilation—contributes to the onset of adverse health effects. This study revealed that a worrying proportion of exposed staff were affected, highlighting the importance of monitoring working conditions and the safety of chemicals used in dentistry.
Complete personal protective equipment (PPE), including masks, gloves, and protective goggles, proved to have a strong protective effect, reducing symptoms’ incidence and duration. Moreover, strict adherence to the manufacturer’s instructions—such as correct dosage and proper drying time—was associated with a lower likelihood of rapid symptom onset, emphasizing the importance of standardized protocols.
This study found a statistically significant association between room ventilation and the duration of symptoms following Oxycide™ exposure. Participants working in ventilated rooms were more likely to report either no symptoms or symptoms of short duration, whereas those in unventilated environments reported a higher frequency of prolonged symptoms. These findings highlight the protective role of adequate ventilation in reducing both the incidence and persistence of irritative effects associated with chemical disinfectants. Ensuring proper airflow, particularly through the presence of windows or mechanical ventilation systems, should be considered a key preventive measure in occupational safety protocols. In conclusion, ensuring a healthy working environment in dental offices requires a careful balance between infection control requirements and protecting staff from the side effects of the chemical agents used. The risks identified in this study can be significantly reduced through proactive monitoring and preventive measures. It is recommended that occupational health policymakers and dental clinic managers consider the findings and develop clear policies on the use of disinfectants, including safety criteria for staff, thus ensuring safe and sustainable dental practice.