A Systematic Review of the Usability of Telemedicine Interface Design for Older Adults
Abstract
1. Introduction
- What design elements should be considered for older adults’ telemedicine interface design?
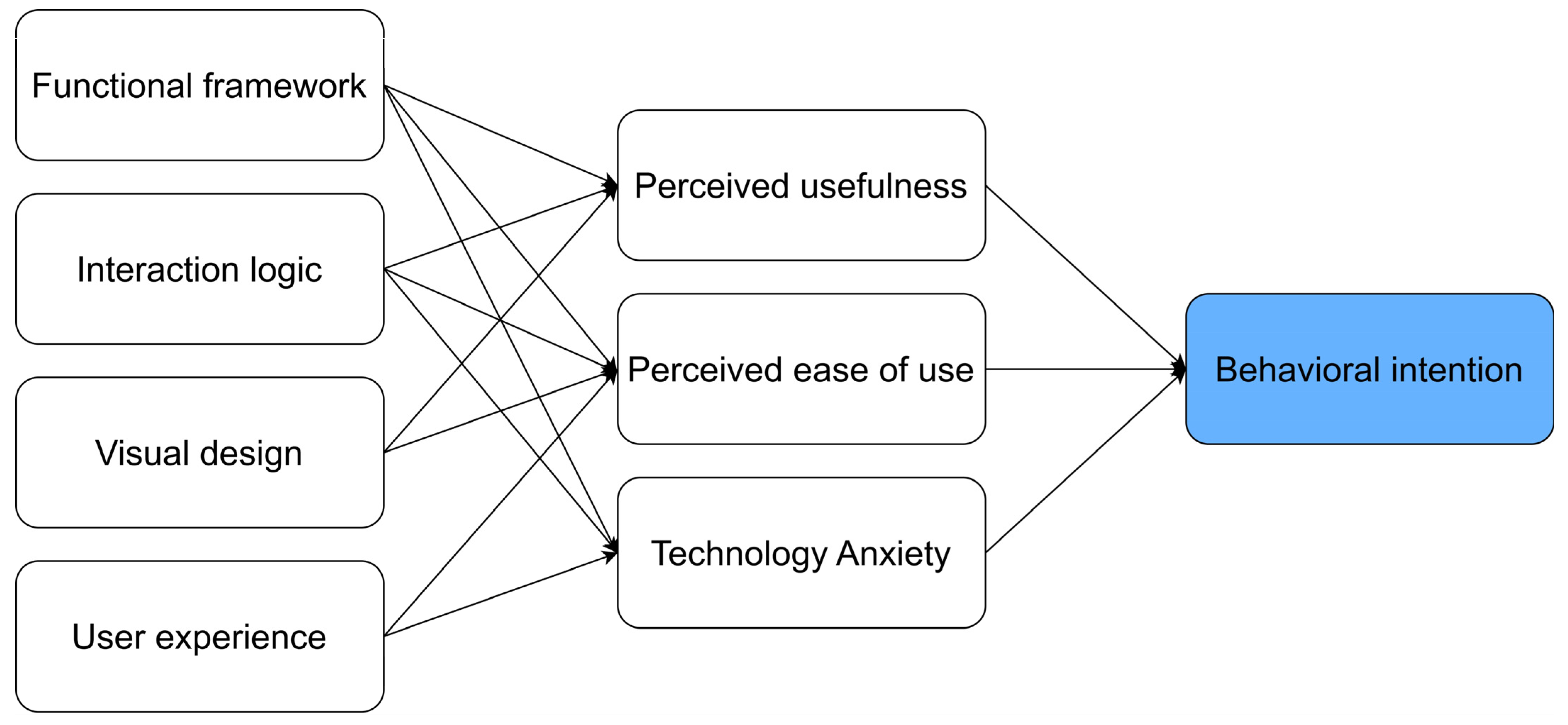
- What methods are used to evaluate the usability of interface design?
2. Methods
2.1. Information Sources
2.2. Eligibility Criteria
2.3. Data Extraction and Analysis
3. Results
3.1. Study Characteristics
3.2. Factors Affecting the Usability of Interface Design
3.2.1. Functional Framework
3.2.2. Interaction Logic
3.2.3. Visual Design
3.2.4. User Experience
3.3. Usability Evaluation Methods for Interface Design
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. The UN Decade of Healthy Ageing 2021–2030 in a Climate-Changing World; Decade of Healthy Ageing Connection Series; World Health Organization: Geneva, Switzerland, 2022; Volume 3. [Google Scholar]
- Chun, Y.J.; Patterson, P.E. A usability gap between older adults and younger adults on interface design of an Internet-based telemedicine system. Work-A J. Prev. Assess. Rehabil. 2012, 41, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Mulgund, P.; Sharman, R.; Rifkin, D.; Marrazzo, S. Design, Development, and Evaluation of a Telemedicine Platform for Patients with Sleep Apnea (Ognomy): Design Science Research Approach. JMIR Form. Res. 2021, 5, 15. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Abdul-Rashid, S.H.; Ghazilla, R.A.R. Research Trends and Hot Spots in Telemedicine for the Elderly: A Scientometric Analysis. Healthcare 2024, 12, 1853. [Google Scholar] [CrossRef] [PubMed]
- Clausen, T.C.; Greve, N.K.; Müller, K.I.; Kristoffersen, E.S.; Schytz, H.W. Telemedicine in headache care: A systematic review. Cephalalgia 2022, 42, 1397–1408. [Google Scholar] [CrossRef]
- Merrell, R.C. Geriatric telemedicine: Background and evidence for telemedicine as a way to address the challenges of geriatrics. Healthc. Inform. Res. 2015, 21, 223–229. [Google Scholar] [CrossRef]
- Narasimha, S.; Madathil, K.C.; Agnisarman, S.; Rogers, H.; Welch, B.; Ashok, A.; Nair, A.; McElligott, J. Designing telemedicine systems for geriatric patients: A review of the usability studies. Telemed. E-Health 2017, 23, 459–472. [Google Scholar] [CrossRef]
- Meng, F.B.; Guo, X.T.; Peng, Z.Y.; Lai, K.H.; Zhao, X.L. Investigating the Adoption of Mobile Health Services by Elderly Users: Trust Transfer Model and Survey Study. JMIR Mhealth Uhealth 2019, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Chun, Y.J.; Patterson, P.E. A suggestion for future research on interface design of an internet-based telemedicine system for the elderly. Work-A J. Prev. Assess. Rehabil. 2012, 41, 353–356. [Google Scholar] [CrossRef]
- Wildenbos, G.A.; Jaspers, M.W.; Schijven, M.P.; Dusseljee-Peute, L. Mobile health for older adult patients: Using an aging barriers framework to classify usability problems. Int. J. Med. Inform. 2019, 124, 68–77. [Google Scholar] [CrossRef]
- Rogers, W.A.; Fisk, A.D. Toward a psychological science of advanced technology design for older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2010, 65, 645–653. [Google Scholar] [CrossRef]
- Alsswey, A.; Al-Samarraie, H.; Malak, M.Z. Older adults’ satisfaction with mHealth UI design-based culture: A case study of Jordan. J. Hum. Behav. Soc. Environ. 2023, 33, 565–577. [Google Scholar] [CrossRef]
- Tajudeen, F.P.; Bahar, N.; Tan, M.P.; Peer Mustafa, M.B.; Saedon, N.I.; Jesudass, J. Understanding user requirements for a senior-friendly mobile health application. Geriatrics 2022, 7, 110. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Hernandez, M.; Ferre, X.; Moral, C.; Villalba-Mora, E. Design guidelines of Mobile apps for older adults: Systematic review and thematic analysis. JMIR mHealth uHealth 2023, 11, e43186. [Google Scholar] [CrossRef]
- Barnum, C.M. Usability Testing Essentials: Ready, Set... Test; Morgan Kaufmann: Burlington, MA, USA, 2020. [Google Scholar]
- Sharp, H.; Rogers, Y.; Preece, J. Interaction Design: Beyond Human-Computer Interaction; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2023. [Google Scholar]
- Wildenbos, G.A.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Sajib, M.; Manzano, J.; Chlebek, C.J. mHealth Technology Experiences of Middle-Aged and Older Individuals With Visual Impairments: Cross-Sectional Interview Study. JMIR Form. Res. 2023, 7, 12. [Google Scholar] [CrossRef]
- Alsswey, A.; Al-Samarraie, H. Elderly users’ acceptance of mHealth user interface (UI) design-based culture: The moderator role of age. J. Multimodal User Interfaces 2020, 14, 49–59. [Google Scholar] [CrossRef]
- Alkawaldeh, M.Y.; Jacelon, C.S.; Jeungok, C. Usability testing of a tablet-based self-management application for older adults with T2DM: The ASSISTwell application. Gerontechnology 2020, 20, 1–13. [Google Scholar] [CrossRef]
- Saparamadu, A.A.D.N.S.; Fernando, P.; Zeng, P.; Teo, H.; Goh, A.; Lee, J.M.Y.; Lam, C.W.L. User-centered design process of an mHealth app for health professionals: Case study. JMIR mHealth uHealth 2021, 9, e18079. [Google Scholar] [CrossRef]
- Marcus, A. Dare we define user-interface design? Interactions 2002, 9, 19–24. [Google Scholar] [CrossRef]
- Blair-Early, A.; Zender, M. User interface design principles for interaction design. Des. Issues 2008, 24, 85–107. [Google Scholar] [CrossRef]
- Takano, E.; Maruyama, H.; Takahashi, T.; Mori, K.; Nishiyori, K.; Morita, Y.; Fukuda, T.; Kondo, I.; Ishibashi, Y. User Experience of Older People While Using Digital Health Technologies: A Systematic Review. Appl. Sci. 2023, 13, 12815. [Google Scholar] [CrossRef]
- Almeida, A.F.; Rocha, N.P.; Silva, A.G. Methodological quality of manuscripts reporting on the usability of mobile applications for pain assessment and management: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 785. [Google Scholar] [CrossRef]
- Bateman, D.R.; Srinivas, B.; Emmett, T.W.; Schleyer, T.K.; Holden, R.J.; Hendrie, H.C.; Callahan, C.M. Categorizing health outcomes and efficacy of mHealth apps for persons with cognitive impairment: A systematic review. J. Med. Internet Res. 2017, 19, e301. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, C.; Prando, B.C.; Dantas, L.O.; da Silva Serrão, P.R.M. Mobile health technologies for the management of spine disorders: A systematic review of mHealth applications in Brazil. Musculoskelet. Sci. Pract. 2022, 60, 102562. [Google Scholar] [CrossRef] [PubMed]
- da Silva, H.E.C.; Santos, G.N.M.; Ferreira Leite, A.; Mesquita, C.R.M.; de Souza Figueiredo, P.T.; Miron Stefani, C.; de Santos Melo, N. The feasibility of telehealth in the monitoring of head and neck cancer patients: A systematic review on remote technology, user adherence, user satisfaction, and quality of life. Support. Care Cancer 2022, 30, 8391–8404. [Google Scholar] [CrossRef]
- Leiz, M.; Pfeuffer, N.; Rehner, L.; Stentzel, U.; van den Berg, N. Telemedicine as a Tool to Improve Medicine Adherence in Patients with Affective Disorders–A Systematic Literature Review. Patient Prefer. Adherence 2022, 16, 3441–3463. [Google Scholar] [CrossRef] [PubMed]
- Sen, K.; Prybutok, G.; Prybutok, V. The use of digital technology for social wellbeing reduces social isolation in older adults: A systematic review. SSM-Population Health 2022, 17, 101020. [Google Scholar] [CrossRef]
- AlQudah, A.A.; Al-Emran, M.; Shaalan, K. Technology Acceptance in Healthcare: A Systematic Review. Appl. Sci. 2021, 11, 10537. [Google Scholar] [CrossRef]
- Binyamin, S.S.; Zafar, B.A. Proposing a mobile apps acceptance model for users in the health area: A systematic literature review and meta-analysis. Health Inform. J. 2021, 27, 1460458220976737. [Google Scholar] [CrossRef]
- Dash, D.M.; Shadangi, D.P.Y.; Kar, D.S.; Prusty, M.R. A Conceptual Model for Telemedicine Adoption: An Examination of Technology Acceptance Model. Int. J. Recent Technol. Eng. (IJRTE) 2019, 8, 1286–1288. [Google Scholar] [CrossRef]
- Rouidi, M.; Elouadi, A.; Hamdoune, A. Acceptance and use of telemedicine technology by health professionals: Development of a conceptual model. Digit Health 2022, 8, 20552076221081693. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Davis, F.D. User acceptance of information technology: System characteristics, user perceptions and behavioral impacts. Int. J. Man-Mach. Stud. 1993, 38, 475–487. [Google Scholar] [CrossRef]
- Kamal, S.A.; Shafiq, M.; Kakria, P. Investigating acceptance of telemedicine services through an extended technology acceptance model (TAM). Technol. Soc. 2020, 60, 101212. [Google Scholar] [CrossRef]
- Kitsiou, S.; Paré, G.; Jaana, M. Effects of home telemonitoring interventions on patients with chronic heart failure: An overview of systematic reviews. J. Med. Internet Res. 2015, 17, e63. [Google Scholar] [CrossRef] [PubMed]
- Shemesh, T.; Barnoy, S. Assessment of the Intention to Use Mobile Health Applications Using a Technology Acceptance Model in an Israeli Adult Population. Telemed. E-Health 2020, 26, 1141–1149. [Google Scholar] [CrossRef]
- Park, Y.E.; Tak, Y.W.; Kim, I.; Lee, H.J.; Lee, J.B.; Lee, J.W.; Lee, Y.R. User Experience and Extended Technology Acceptance Model in Commercial Health Care App Usage Among Patients with Cancer: Mixed Methods Study. J. Med. Internet Res. 2024, 26, e55176. [Google Scholar] [CrossRef]
- Ekstedt, M.; Kirsebom, M.; Lindqvist, G.; Kneck, Å.; Frykholm, O.; Flink, M.; Wannheden, C. Design and development of an ehealth service for collaborative self-management among older adults with chronic diseases: A theory-driven user-centered approach. Int. J. Environ. Res. Public Health 2022, 19, 391. [Google Scholar] [CrossRef]
- Liu, N.; Yin, J.; Tan, S.S.-L.; Ngiam, K.Y.; Teo, H.H. Mobile health applications for older adults: A systematic review of interface and persuasive feature design. J. Am. Med. Inform. Assoc. 2021, 28, 2483–2501. [Google Scholar] [CrossRef]
- Amjad, A.; Kordel, P.; Fernandes, G. A review on innovation in healthcare sector (telehealth) through artificial intelligence. Sustainability 2023, 15, 6655. [Google Scholar] [CrossRef]
- Cabanillas-Carbonell, M.; Pérez-Martínez, J.; Yáñez, J.A. 5G technology in the digital transformation of healthcare, a systematic Review. Sustainability 2023, 15, 3178. [Google Scholar] [CrossRef]
- Creusen, M.E.; Schoormans, J.P. The different roles of product appearance in consumer choice. J. Prod. Innov. Manag. 2005, 22, 63–81. [Google Scholar] [CrossRef]
- Paul, J.; Criado, A.R. The art of writing literature review: What do we know and what do we need to know? Int. Bus. Rev. 2020, 29, 101717. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. Bmj 2021, 372, n160. [Google Scholar] [CrossRef]
- Pati, D.; Lorusso, L.N. How to write a systematic review of the literature. HERD Health Environ. Res. Des. J. 2018, 11, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.Y.; Wen, T.T.; Yue, S.Y.; Zhao, X.R.; Huang, K.K. The influence of health information attention and app usage frequency of older adults on persuasive strategies in mHealth education apps. Digit. Health 2023, 9, 16. [Google Scholar] [CrossRef]
- Choi, K.S.; Chan, S.H.; Ho, C.L.; Matejak, M. Development of a Healthcare Information System for Community Care of Older Adults and Evaluation of Its Acceptance and Usability. Digit. Health 2022, 8, 20552076221109083. [Google Scholar] [CrossRef]
- Arkkukangas, M.; Cederbom, S.; Tonkonogi, M.; Umb Carlsson, Õ. Older adults’ experiences with mHealth for fall prevention exercise: Usability and promotion of behavior change strategies. Physiother. Theory Pract. 2021, 37, 1346–1352. [Google Scholar] [CrossRef]
- Bergquist, R.; Vereijken, B.; Mellone, S.; Corzani, M.; Helbostad, J.L.; Taraldsen, K. App-based Self-administrable Clinical Tests of Physical Function: Development and Usability Study. JMIR Mhealth Uhealth 2020, 8, 11. [Google Scholar] [CrossRef]
- Alnanih, R.; Balabid, A.; Bahmdean, L. Senior-centered design for mobile medication adherence applications based on cognitive and technology attributes. Univers. Access Inf. Soc. 2024, 23, 871–888. [Google Scholar] [CrossRef]
- Cao, W.; Wang, J.; Wang, Y.; Hassan, I.I.; Kadir, A.A. mHealth App to improve medication adherence among older adult stroke survivors: Development and usability study. Digit. Health 2024, 10, 20552076241236291. [Google Scholar] [CrossRef] [PubMed]
- Eriksson-Backa, K.; Hirvonen, N.; Enwald, H.; Huvila, I. Enablers for and barriers to using My Kanta—A focus group study of older adults’ perceptions of the National Electronic Health Record in Finland. Inform. Health Soc. Care 2021, 46, 399–411. [Google Scholar] [CrossRef]
- Mao, J.Y.; Xie, L.L.; Zhao, Q.H.; Xiao, M.Z.; Tu, S.T.; Sun, W.J.; Zhou, T.T. Demand analysis of an intelligent medication administration system for older adults with chronic diseases based on the Kano model. Int. J. Nurs. Sci. 2022, 9, 63–70. [Google Scholar] [CrossRef]
- Murabito, J.M.; Faro, J.M.; Zhang, Y.K.; Demalia, A.; Hamel, A.; Agyapong, N.; Liu, H.S.; Schramm, E.; McManus, D.; Borrelli, B. Smartphone App Designed to Collect Health Information in Older Adults: Usability Study. Jmir Hum. Factors 2024, 11, 13. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, I.; Lee, S.; Yu, S. Information and Communication Technology-Based Application for Cognitive Behavioral Therapy among Community-Dwelling Older Adults with Insomnia: Development and Validation Study. Healthcare 2024, 12, 106. [Google Scholar] [CrossRef]
- Sien, S.W.; Kobekyaa, F.K.; Puts, M.; Currie, L.; Tompson, M.; Hedges, P.; McGrenere, J.; Mariano, C.; Haase, K.R. Tailored Self-Management App to Support Older Adults with Cancer and Multimorbidity: Development and Usability Testing. JMIR Aging 2024, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Song, J. An empirical investigation into the preferences of the elderly for user interface design in personal electronic health record systems. Front. Digit. Health 2023, 5, 1289904. [Google Scholar] [CrossRef]
- Aldekhyyel, R.N.; Almulhem, J.A.; Binkheder, S. Usability of Telemedicine Mobile Applications during COVID-19 in Saudi Arabia: A Heuristic Evaluation of Patient User Interfaces. Healthcare 2021, 9, 1574. [Google Scholar] [CrossRef]
- Ivankova, N.V.; Rogers, L.Q.; Herbey, I.I.; Martin, M.Y.; Pisu, M.; Pekmezi, D.; Thompson, L.; Schoenberger-Godwin, Y.M.M.; Oster, R.A.; Fontaine, K.; et al. Features That Middle-aged and Older Cancer Survivors Want in Web-Based Healthy Lifestyle Interventions: Qualitative Descriptive Study. JMIR Cancer 2021, 7, 16. [Google Scholar] [CrossRef]
- Nebeker, C.; Zlatar, Z.Z. Learning From Older Adults to Promote Independent Physical Activity Using Mobile Health (mHealth). Front. Public Health 2021, 9, 11. [Google Scholar] [CrossRef]
- Arkkukangas, M. App-based strength and balance self-test in older adults: An exploratory study from a user perspective. BMC Res. Notes 2021, 14, 379. [Google Scholar] [CrossRef] [PubMed]
- da Silva Sobrinho, A.C.; de Oliveira Gomes, G.A.; Bueno Júnior, C.R. Developing a Multiprofessional Mobile App to Enhance Health Habits in Older Adults: User-Centered Approach. JMIR Form. Res. 2024, 8, e54214. [Google Scholar] [CrossRef]
- Yeh, P.C. Impact of button position and touchscreen font size on healthcare device operation by older adults. Heliyon 2020, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, S.H.; Cho, N.B.; You, H.; Choi, T.; Kim, J. User-Dependent Usability and Feasibility of a Swallowing Training mHealth App for Older Adults: Mixed Methods Pilot Study. JMIR Mhealth Uhealth 2020, 8, 16. [Google Scholar] [CrossRef] [PubMed]
- Khamaj, A.; Ali, A.M. Examining the usability and accessibility challenges in mobile health applications for older adults. Alex. Eng. J. 2024, 102, 179–191. [Google Scholar] [CrossRef]
- Shah, U.E.M.; Chiew, T.K.; Mehmood, Y. A Usability Evaluation Instrument for Pain Management Mobile Applications: An Elderly’s Perspective. Int. J. Hum. Comput. Interact. 2024, 40, 2265–2281. [Google Scholar] [CrossRef]
- Niemiec, S.L.S.; Wagas, R.; Vigen, C.L.P.; Blanchard, J.; Barber, S.J.; Schoenhals, A. Preliminary User Evaluation of a Physical Activity Smartphone App for Older Adults. Health Policy Technol. 2022, 11, 7. [Google Scholar] [CrossRef]
- Androutsou, T.; Kouris, I.; Anastasiou, A.; Pavlopoulos, S.; Mostajeran, F.; Bamiou, D.E.; Genna, G.J.; Costafreda, S.G.; Koutsouris, D. A Smartphone Application Designed to Engage the Elderly in Home-Based Rehabilitation. Front. Digit. Health 2020, 2, 13. [Google Scholar] [CrossRef]
- Tran-Nguyen, K.; Berger, C.; Bennett, R.; Wall, M.; Morin, S.N.; Rajabiyazdi, F. Mobile App Prototype in Older Adults for Postfracture Acute Pain Management: User-Centered Design Approach. JMIR Aging 2022, 5, e37772. [Google Scholar] [CrossRef]
- Vergouw, J.W.; Smits-Pelser, H.; Kars, M.C.; Van Houwelingen, T.; Van Os-Medendorp, H.; Kort, H.; Bleijenberg, N. Needs, barriers and facilitators of older adults towards eHealth in general practice: A qualitative study. Prim. Health Care Res. Dev. 2020, 21, e54. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, B.; Sabharwal, J.K.; Chawla, S. Old age or cognitive decline? Examining the usability of a mobile health app for older Australians. Inform. Health Soc. Care 2024, 49, 83–97. [Google Scholar] [CrossRef] [PubMed]
- Abujarad, F.; Ulrich, D.; Edwards, C.; Choo, E.; Pantalon, M.V.; Jubanyik, K.; Dziura, J.; D’Onofrio, G.; Gill, T.M. Development and usability evaluation of VOICES: A digital health tool to identify elder mistreatment. J. Am. Geriatr. Soc. 2021, 69, 1469–1478. [Google Scholar] [CrossRef] [PubMed]
- Felberbaum, Y.; Lanir, J.; Weiss, P.L. Designing Mobile Health Applications to Support Walking for Older Adults. Int. J. Environ. Res. Public Health 2023, 20, 3611. [Google Scholar] [CrossRef]
- Zhong, R.T.; Rau, P.L.P. A Mobile Phone-Based Gait Assessment App for the Elderly: Development and Evaluation. JMIR Mhealth Uhealth 2020, 8, 17. [Google Scholar] [CrossRef]
- Le, T.; Reeder, B.; Yoo, D.; Aziz, R.; Thompson, H.J.; Demiris, G. An Evaluation of Wellness Assessment Visualizations for Older Adults. Telemed. E-Health 2015, 21, 9–15. [Google Scholar] [CrossRef]
- Garvelink, M.M.; Agbadjé, T.T.; Freitas, A.; Bergeron, L.; Petitjean, T.; Dugas, M.; Blair, L.; Archambault, P.; Roy, N.; Jones, A.; et al. Improving a Web-Based Tool to Support Older Adults to Stay Independent at Home: Qualitative Study. JMIR Mhealth Uhealth 2020, 8, e16979. [Google Scholar] [CrossRef]
- Pan, J.; Dong, H. mHealth Adoption Among Older Chinese Adults: A Conceptual Model With Design Suggestions. Int. J. Hum. Comput. Interact. 2023, 39, 1072–1083. [Google Scholar] [CrossRef]
- Choi, S.; Chlebek, C.J. Exploring mHealth design opportunities for blind and visually impaired older users. Mhealth 2024, 10, 17. [Google Scholar] [CrossRef]
- Christiansen, L.; Lindberg, C.; Berglund, J.S.; Anderberg, P.; Skär, L. Using Mobile Health and the Impact on Health-Related Quality of Life: Perceptions of Older Adults with Cognitive Impairment. Int. J. Environ. Res. Public Health 2020, 17, 2650. [Google Scholar] [CrossRef]
- Choi, H.K.; Lee, K.; Lee, S.H. Developmental Study on “Smart Silver Care”: A Mobile Application to Alleviate Loneliness in Older Adults within the Community. Healthcare 2023, 11, 2376. [Google Scholar] [CrossRef] [PubMed]
- Mansson, L.; Wiklund, M.; Öhberg, F.; Danielsson, K.; Sandlund, M. Co-Creation with Older Adults to Improve User-Experience of a Smartphone Self-Test Application to Assess Balance Function. Int. J. Environ. Res. Public Health 2020, 17, 3768. [Google Scholar] [CrossRef] [PubMed]
- Aljedaani, K.; Alnanih, R. Grounded Theory for Designing Mobile User Interfaces-Based on Space Retrieval Therapy. Int. J. Interact. Mob. Technol. 2021, 15, 104–124. [Google Scholar] [CrossRef]
- Perotti, L.; Stamm, O.; Dietrich, M.; Buchem, I.; Müller-Werdan, U. The usability and user experience of an interactive e-learning platform to empower older adults when using electronic personal health records: An online intervention study. Univers. Access Inf. Soc. 2024, 16. [Google Scholar] [CrossRef]
- Cornet, V.P.; Toscos, T.; Bolchini, D.; Rohani Ghahari, R.; Ahmed, R.; Daley, C.; Mirro, M.J.; Holden, R.J. Untold Stories in User-Centered Design of Mobile Health: Practical Challenges and Strategies Learned From the Design and Evaluation of an App for Older Adults with Heart Failure. JMIR Mhealth Uhealth 2020, 8, e17703. [Google Scholar] [CrossRef]
- Nielsen, J. Enhancing the explanatory power of usability heuristics. In Proceedings of the SIGCHI conference on Human Factors in Computing Systems, Boston, MA, USA, 24–28 April 1994. [Google Scholar]

| Dimension | Inclusion and Exclusion Criteria |
|---|---|
| Population | This review defines older adults as individuals aged 50 and over, while the World Health Organization (WHO) defines the elderly as those aged 65 and older. With the onset of geriatric conditions occurring at increasingly younger ages, individuals over 50 with chronic illnesses often begin to experience health-related challenges [10,50]. Additionally, younger members of the older adult population generally exhibit a higher rate of adoption of internet-based technologies compared to their more senior counterparts. |
| Interventions | This study includes telemedicine platform interfaces available on mobile phones, devices, computers, and smart TVs, but excludes wearable devices and robotic interfaces intended for smart homes or elderly care. |
| Comparisons | There are no specific comparison criteria excluded from this review. |
| Outcomes | Research that focuses exclusively on influencing factors, framework construction, or software development without addressing interface design will be excluded. |
| Study designs | To maintain consistency and comparability, the research was restricted to peer-reviewed journal articles published in English. Studies that are (1) not in English, (2) design works, reports, review papers, conference speeches, or extended abstracts, (3) journal-collected materials, and (4) outside the current time range or unrelated to the research topic are excluded. |
| Modules | Elements | Specification/Definition | Reference | Numbers of Papers |
|---|---|---|---|---|
| Functional Design | Reminder | Include overdose warnings, personalized musical alarms, scheduled medication reminders, and safety precautions | [20,53,55,57,59,70,73] | 7 |
| Set reminders to foster healthy habits and prompt target behaviors | [20,50,82] | 3 | ||
| Reminder notifications for appointments, vaccinations, and prescription refills | [13,20,56,83] | 4 | ||
| Pain logging reminders | [73] | 1 | ||
| Use a family member’s voice for delivering reminder messages | [54] | 1 | ||
| Interaction | Enhance social engagement with family, friends, healthcare professionals, and fellow patients through chat and communication services | [20,55,56,83] | 4 | |
| Offer communication and social support for learning and comparison | [50,66] | 2 | ||
| Provide transcripts for the hearing-impaired, along with interactive video content | [80] | 1 | ||
| Features that can be controlled with notes to aid device familiarity, such as dragging instead of tapping | [70] | 1 | ||
| Edit | Editable user profile featuring account access, a toolbar, and a comments section | [20,82] | 2 | |
| Health management | Includes gymnastics, walking routines, dietary plans, healthy eating suggestions, carbohydrate tracking, daily intake logging, and a goal-oriented to-do list | [13,20,84] | 3 | |
| Emotional support | Offer an AI speaker, video calls, access to an online community, and music for emotional well-being | [84] | 1 | |
| Cognitive Management | Features a calendar, alarm, games, multiple response options, and scheduling tools | [84] | 1 | |
| Health information/ data | Provides knowledge on stroke, hypertension, diabetes, and vital signs, along with extensive health information on diseases and risk factors | [13,55,80,81,84] | 5 | |
| Ensures urgent medical information is visible and easily accessible | [73] | 1 | ||
| Display color-coded information on the medication screen for clarity | [54] | 1 | ||
| Accurately records medical data in a digital format | [13,18,51] | 3 | ||
| Medical calculator | Includes health risk calculators for seniors with reference ranges | [13,78] | 2 | |
| Medication tacker | Monitors health status and disease progression | [73] | 1 | |
| Interaction Logic | Navigation | Incorporate instructional videos with voice-overs, real-time feedback, clear navigation aids, contextual help, spacious click-sensitive areas, and intuitive page navigation. Maintain flexible control with persistent instructions at the top to avoid dropdown menus and complex gestures | [13,20,53,54,56,58,60,68,69,70,73,75,80,85,86] | 15 |
| Feedback | Provides audible error notifications, audio alerts from voice assistants, visual cues, voice recognition capabilities, and multiple feedback modes including visual feedback, vibration alerts, and audio signals | [18,54,61,66,70,75,82] | 7 | |
| Incorporates humorous feedback elements | [20] | 1 | ||
| Establish a feedback loop system where user input informs continuous updates and improvements | [69] | 1 | ||
| Ensure fast response times for quick online results | [13,74] | 2 | ||
| Features a female narrator with slower narration and animation speed for better understanding | [76] | 1 | ||
| Highlights important information using clear and inclusive language | [73] | 1 | ||
| Offers textual feedback when the effects of movements are unclear | [72] | 1 | ||
| Data input and output | Allows flexible data entry and presentation with offline functionality to address connectivity issues | [69,82] | 2 | |
| Streamlines operations by minimizing task completion steps for ease of use | [57,70,73] | 3 | ||
| Includes predictive spelling with a ‘done’ box at the end of the entries | [75] | 1 | ||
| Enables users to print and export data to other devices, and allows retrospective data entry | [20] | 1 | ||
| Features automatic entry linking the person’s account to the caregiver’s account via QR code for convenience | [54] | 1 | ||
| Visual Design | Color | Utilizes vivid, high-contrast colors with outlines for better recognition while avoiding overly bright colors like yellow and red, and ensuring uniformity with user-friendly alternatives | [13,54,55,58,60,61,66,76] | 8 |
| Provides audible color information and adaptive customization for visual needs, employs different color schemes to enhance interest | [76,82] | 2 | ||
| Matches pain color indicators to the severity of pain experienced | [73] | 1 | ||
| Preferences indicate older adults favor blue and pink for fonts and blue and turquoise for backgrounds | [54] | 1 | ||
| Use culturally relevant colors (e.g., blue, green, black) | [19] | 1 | ||
| Shape | Adopts a rectangular for the pill box instead of circular design for practicality | [54] | 1 | |
| Icons and buttons | Utilizes large buttons with clear labels and simple icons. Employs skeuomorphic design and universally recognized symbols to minimize selection errors, with essential buttons at the top while distinguishing between active and disabled button states | [13,54,55,61,64,70,72,77] | 8 | |
| Ensures proper placement of action button for intuitive use | [74] | 1 | ||
| Uses simple icons to represent different concepts clearly | [72] | 1 | ||
| Fonts and text | Implements large, consistent font sizes, stepwise brief information (max three screens), high-contrast text, larger touch targets while minimizing on-screen text clutter | [12,55,57,58,59,66,69,72,75,76,77] | 11 | |
| Font Size | Uses a readable font size of 12–14 points, with customizable options for text and headings | [12,13,19,60,69,70,76,77,78,86] | 10 | |
| A minimum text size of 18 points is set in the application | [54] | 1 | ||
| Font recommendation | Employs suitable typefaces (e.g., San Serif) | [13] | 1 | |
| Font (Proxima Nova and Arial) | [54] | 1 | ||
| Includes Arabic font types of “ةعقرلا” or “الرقعة” | [12,19] | 2 | ||
| Language | Ensures language is simple and clear in users’ native language, avoiding technical terms, jargon, and medical terminology, while using positive statements and active voice | [13,54,55,70,77,80] | 6 | |
| Supports multiple languages to cater to diverse user populations | [58] | 1 | ||
| Picture | Incorporate intuitive animations, illustrations, and relevant photos to create clear, engaging visual aids that enhance understanding | [13,55,59,73] | 4 | |
| Layout | Streamline navigation by addressing pain points in user experience and optimizing menu structures and button placements to ensure a clear, consistent, and esthetically pleasing layout with standardized page designs | [13,59,69,70] | 4 | |
| Centralizes all important data and buttons for easy access | [86] | 1 | ||
| Adapting layouts to the cultural reading and writing habits | [12] | 1 | ||
| Menu | Uses an icon-centric menu with segmented block-grid layouts that combine the ease of list-style navigation with the clarity of grid-style content-oriented navigation | [54,61,86] | 3 | |
| Ensures pop-up windows are displayed longer in smartphone applications or avoided altogether | [54,72] | 2 | ||
| Maximizing spacing between elements for usability | [72] | 1 | ||
| Label | Employ text labels rather than icons alone, ensure familiar icon styles are used, and separate live links to prevent accidental clicks while avoiding opening links in new windows to reduce confusion among users | [13,77] | 2 | |
| Data Visualization | Simplify health data visualizations by comparing metrics to standards, providing overviews and explanations, monitoring exercise progress, and using emojis instead of graphs for pain data representation | [18,60,68,73,77,82] | 6 | |
| User Experience | Gamification | Utilize rewards systems and competition to motivate elderly users, and incorporate a flashing “done” button along with task countdowns to enhance engagement levels | [58,66,72] | 3 |
| Sociability | Enhance user engagement through social dimensions that foster a sense of belonging within the application environment | [66,81] | 2 | |
| Personalization | Customize the main page layout while offering personalized health feedback and content, integrating accessibility features like screen reader compatibility, adjustable contrast, audio prompts, and tailored notifications to meet individual needs | [50,63,69,74,82] | 5 | |
| Provide links to external sites for personalized medical information related to injuries or conditions | [73] | 1 | ||
| Ease of use | Organize information in a logical and straightforward manner suitable for all cognitive levels, creating an intuitive interface that is easy to read and learn without prior experience. Ensure that tasks are uncomplicated and easily transferable | [58,60,63,70,81,85] | 6 | |
| Simplicity | Develop a cohesive and consistent design featuring familiar buttons and menus, utilizing clear and recognizable images along with straightforward language. Avoid clutter and unnecessary complexity to maintain clarity | [13,19,20,63,66,68,70,73,82,85] | 10 | |
| Fault Tolerance | Implement immediate error correction, provide timely feedback, offer help resources, and ensure easy recovery options. Additionally, make support readily accessible for troubleshooting and assistance | [13,20,55,63,68,70] | 6 | |
| Security | Guarantee data protection, privacy, and user safety through professional practices and robust system safeguards | [56,63,64,76,85] | 5 | |
| Emotional | Create a realistic experience that evokes an emotional response and promotes a sense of achievement on the first attempt | [68,70,80] | 3 | |
| User Center | Recognize the accomplishments of older users with praise and rewards, provide extra incentives, organize contacts for easier access, and incorporate automated features to enhance overall performance | [50,65,73,74,81] | 5 |
| Evaluation Method | Evaluation Dimension and Rating Items (Define) | Reference |
|---|---|---|
| Usability testing experiment | Effectiveness, productivity, error safety | [54] |
| Ease of use, personalization, communication facilitator (overall impression) | [73] | |
| Occasionally using VS, regularly using tunneling, similarity, liking, suggestions and reminders, social role, simulation, self-monitoring, reduction, personalization, rewards, social learning, social comparison, praise | [50] | |
| The total number of actions per screen, the number of incorrect clicks per task, and the time (in seconds) to complete each task successfully | [86] | |
| System Usability Scale (SUS) | Assess satisfaction, ease of use and navigation, simplicity, usefulness, presentation, efficiency, and acceptance while addressing application errors and fostering excitement | [20,53,55,60,66,68,72,75,76,77,78,87] |
| modified Computer Self-Efficacy Scale (mCSES) | Internal consistency, reliability, construct validity, and acceptance | [68] |
| User Experience Questionnaire (UEQ) | Attractiveness, perspicuity, efficiency, dependability, stimulation, novelty | [53,87] |
| Usability Metric for User Experience (UMUX) | Functionality meets requirements, frustration in usage, ease of use, time spent correcting | [55] |
| eHealth Impact Questionnaire (eHIQ) | Attitudes, confidence and identification, information and presentation, understanding and motivation. | [87] |
| Computer System Usability Questionnaire (CSUQ) | System usefulness, information quality, interface quality, overall satisfaction | [51] |
| Questionnaire for User Interface Satisfaction (QUIS) | Readable design/typography, text writing style, layout, navigation, learn and use, memory load and mental effort, user guidance and error handling, cues, instructions and user control | [70] |
| Nielsen’s usability model | Learnability, efficiency, memorability, error, and satisfaction | [13] |
| Mobile App Rating Scale (MARS) | Application quality, engagement, functionality, esthetics, information, subjective quality | [58,59] |
| Suitability assessment of materials (SAM) | Content, literacy demand, graphics, layout and typography, learning stimulation and motivation, cultural appropriateness | [66] |
| Health Information Technology Usability Evaluation Scale (H-ITUES) | Loyalty, interaction, usability feedback, and sentiment feedback | [71] |
| A questionnaire survey | Challenges, readability, reliability, features feel difficult, intuitive rating design, easy to navigate, rating, used health app before | [69] |
| No usability evaluation was conducted | [12,18,19,52,56,57,61,63,64,65,74,80,81,82,83,84,85,88] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, H.; Raja Ghazilla, R.A.; Abdul-Rashid, S.H. A Systematic Review of the Usability of Telemedicine Interface Design for Older Adults. Appl. Sci. 2025, 15, 5458. https://doi.org/10.3390/app15105458
He H, Raja Ghazilla RA, Abdul-Rashid SH. A Systematic Review of the Usability of Telemedicine Interface Design for Older Adults. Applied Sciences. 2025; 15(10):5458. https://doi.org/10.3390/app15105458
Chicago/Turabian StyleHe, Huiqian, Raja Ariffin Raja Ghazilla, and Salwa Hanim Abdul-Rashid. 2025. "A Systematic Review of the Usability of Telemedicine Interface Design for Older Adults" Applied Sciences 15, no. 10: 5458. https://doi.org/10.3390/app15105458
APA StyleHe, H., Raja Ghazilla, R. A., & Abdul-Rashid, S. H. (2025). A Systematic Review of the Usability of Telemedicine Interface Design for Older Adults. Applied Sciences, 15(10), 5458. https://doi.org/10.3390/app15105458






