Abstract
Telemedicine has the potential to support healthy aging in older adults; however, many applications fail to consider their specific needs and preferences, resulting in a limited number of effective options. This study systematically reviews the existing literature on interface design elements, attempts to link the elements with a Technology Acceptance Model (TAM), evaluates their usability for the elderly population, and highlights the social sustainability of telemedicine systems. A comprehensive search was conducted across the Web of Science, Scopus, PubMed, and CINAHL databases to identify existing research pertaining to the factors influencing usability, evaluation methodologies, and recommendations for telemedicine interfaces specifically designed for older adults. A total of 41 studies were analyzed, yielding a comprehensive summary of research methodologies and interface design elements from four key dimensions: the functional framework, interaction logic, visual design, and user experience. Our analysis identified prevalent usability challenges and provided actionable recommendations. Although the majority of studies focused on existing applications and usability testing, there was a notable gap in research addressing the cognitive and emotional needs of older users. Furthermore, many studies fell short in offering a comprehensive and detailed examination of design elements relevant to this user group. Based on the existing literature, this paper summarizes interface design elements suitable for elderly users, offering insights into user experience and usability. This study provides guidance for the interface design and development of telemedicine for old adults, offers suggestions on interface usability for practitioners in the medical industry, and also provides a reference value for the government in formulating relevant medical policies and for entrepreneurs in making investments.
1. Introduction
The elderly population is rapidly increasing, with projections indicating it will reach 1.4 billion by 2030 and 2.1 billion by 2050, with pronounced growth in developing countries [1]. This demographic shift has led to a rise in chronic diseases, putting additional strain on healthcare systems and highlighting the importance of the elderly as a crucial user group for telemedicine [2]. The World Health Organization defines telemedicine as “the use of information and communication technologies to provide healthcare, diagnose and prevent disease and injury, treat patients, and conduct research and evaluation remotely.” [3].
Telemedicine is transforming the dynamics of patient–provider relationships by adopting a patient-centered approach that eliminates the barriers of time and location [4]. This mode of healthcare delivery enables patients to actively participate in their care while integrating audio, video, and monitoring features to enhance remote observation and maintain the continuity of healthcare without the need for physical visits [5]. As a result, telemedicine reduces travel and wait times for medical appointments, improving healthcare accessibility [6]. Telemedicine effectively facilitates patient triage, problem diagnosis, and both pre- and post-treatment care, increasing the efficiency of offline doctors. It offers a wide range of applications for the elderly, including chronic disease management, vital sign monitoring, and medical consultations [6]. Additionally, it delivers high-quality medical advice at lower costs through telephone consultations and video conferencing, resulting in greater benefits and higher patient satisfaction [7]. However, despite these advantages, the acceptance and use of telemedicine among older adults remain low, as many platforms do not adequately consider their unique characteristics, preferences, and abilities [8].
Compared to younger individuals, older adults experience declines in mental perception, motor coordination, physical health, memory, attention, vision, and hearing [7]. This situation is further aggravated by a shortage of specialized medical care providers [6,9]. Wildenbos [10] found that the usability issues encountered by older adults mainly stem from motivational barriers and cognitive impairments, followed by perceptual and physical ability barriers. These challenges hinder the elderly’s ability to use internet technology, impede the effective communication of information, and negatively affect their daily lives. Moreover, many older adults have limited experience with the Internet and smartphones, which can obstruct their ability to utilize telemedicine unless they are aware of its benefits [11] or have the capability and capacity to engage. The health status and habits of the elderly can significantly influence the usability of telemedicine, especially when designers fail to recognize them as potential users and overlook usability issues in the interface design [7], for example, the use of technical jargon or unfamiliar medical terminology, which may hinder comprehension [12]. Older adults often face difficulties when using mobile apps due to complex menu structures, small font sizes, and various other usability barriers [13]. Therefore, it is necessary to gain an in-depth understanding of the causes and impacts of the usability issues encountered by older adult patients, and to adapt the design of telemedicine interfaces to meet the needs and characteristics of patients [10]. It is essential to design telemedicine interfaces that consider the physical coordination as well as the psychological and emotional needs of the elderly to enhance their quality of life and support sustainable healthy aging.
Usability refers to the degree to which a product can effectively, efficiently, and satisfactorily achieve specific goals within a given usage environment [14,15]. Usability goals provide interaction designers with a specific method to evaluate interactive products and user experience through dimensions such as effectiveness, efficiency, safety, utility, learnability, memorability, and satisfaction [16]. The MOLD-US framework identifies several barriers to usability for the elderly, including perception, cognition, motivation, and physical abilities. These barriers encompass aspects such as vision, memory, digital literacy, and fine motor skills [17]. Key challenges associated with current mobile health technologies include the absence of user manuals, unfriendly interfaces, confusing health data visualizations, cognitive overload, and concerns regarding the health record accuracy [18]. The usability of the interface design is closely linked to its design elements. Essential design components of the mobile health interface, such as the layout, images, colors, fonts, language, and buttons, should be convenient, clear, and straightforward to facilitate task completion for elderly users as effectively as possible [12,19]. Ten usability themes have been identified: satisfaction, ease of use, navigation, simplicity, usefulness, helpfulness, representation, efficiency, errors, excitement, and acceptance [20].
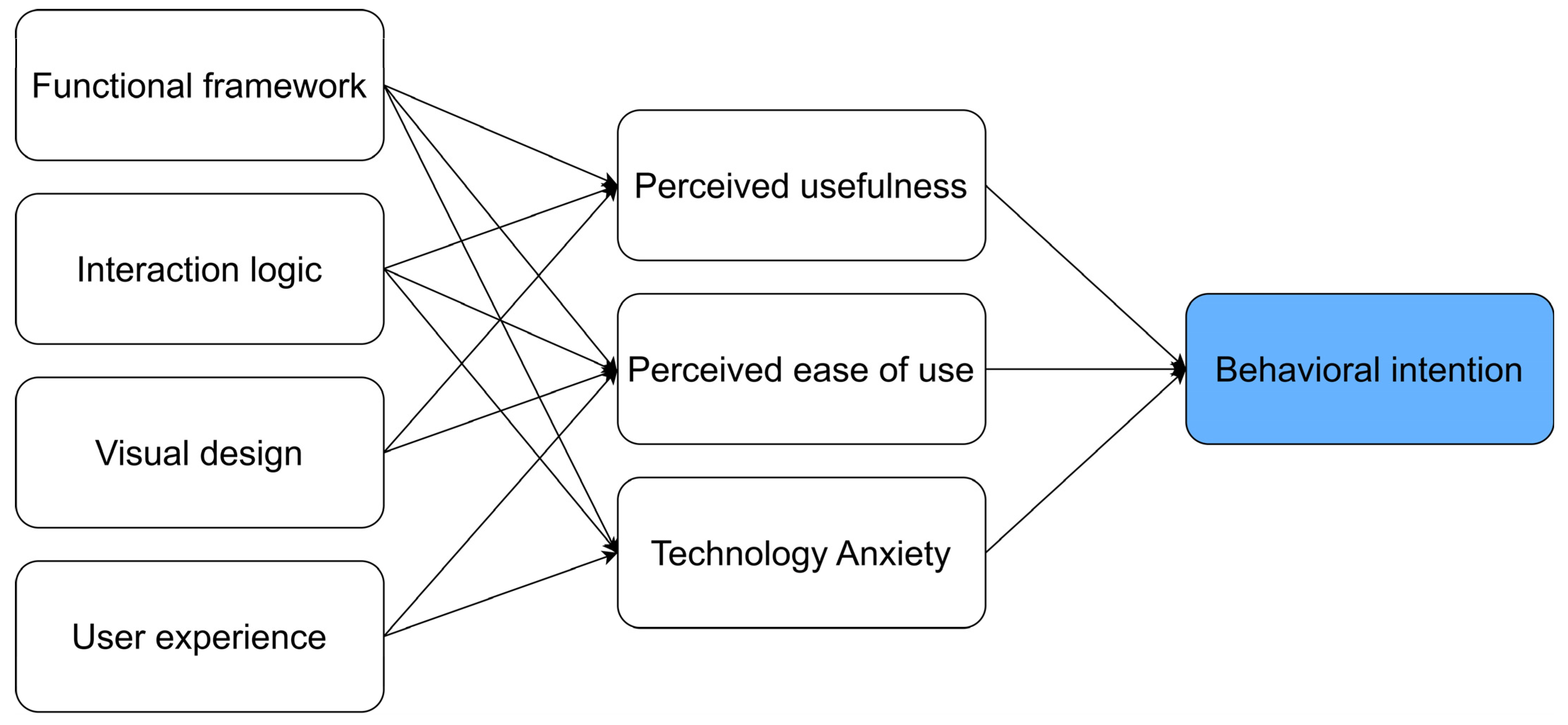
The application’s final design, encompassing its features, functionality, information architecture, interactive components, and visual esthetics, was primarily shaped by user-centered design activities grounded in participatory design principles [21]. Based on the MOLD-US framework and design elements, this study categorizes four groups of factors: the functional framework, interaction logic, visual design, and user experience. The functional framework mainly refers to information architecture, which streamlines information retrieval and task completion, ensuring intuitive navigation for actions like accessing specific blood test results [21]. Interaction design focuses on input–output methods, status displays, and feedback mechanisms, covering both local and global responses [22]. Visual design emphasizes the interface’s perceptual attributes, including visual, auditory, and tactile characteristics, and follows basic visual language principles such as hierarchy, spacing, alignment, and color usage [22,23]. User experience encompasses the full emotional, cognitive, and behavioral responses that occur before, during, and after interacting with a product, aiming to ensure the device is user-friendly, comfortable, visually appealing, and capable of fostering sustained user engagement [16,24].
Over the past decade, numerous systematic reviews on telemedicine for the elderly have concentrated on summarizing mobile applications for specific diseases rather than addressing telemedicine interface design or usability. These reviews encompass studies on the usability in pain management [25], health outcomes for cognitively impaired patients [26], mobile technology for spinal disorders [27], telemedicine monitoring for head and neck cancer [28], improving medication adherence in patients with affective disorders [29], and examining the mental health of older adults to help reduce social isolation among them [30]. Many review articles also examine telemedicine for the elderly through the perspective of influencing factors, utilizing the Technology Acceptance Model (TAM) and Unified Theory of Acceptance and Use of Technology (UTAUT) to analyze acceptance and its determinants [31,32,33,34], but these studies did not link the influencing factors into interface design recommendations or strategies.
The Technology Acceptance Model (TAM) is proposed by Davis for understanding receiving information and technology systems [35]. It has three key factors: perception, behavior intention and actual system use. The perceived usefulness (the belief that a system enhances the performance) and perceived ease of use (the belief that minimal effort is required) are key factors in technology acceptance [36,37]. Patients perceive telemedicine as beneficial only if it improves the service speed, reduces examination costs, optimizes records, and shortens the consultation time [38], all of which are closely related to interface design. On the contrary, when patients experience worry and fear while using telemedicine, it can hinder the use of telemedicine [37]. The causes of such concerns may include system complexity, unreasonable interaction, and poor experience. The TAM framework is linked to the behavioral intention to continue using mobile healthcare applications, yet whether user experience or interface design represents a potential differentiator remains unclear [39]. Park [40] highlighted that perceived usefulness and ease of use are key factors influencing cancer survivors’ adherence to commercial healthcare applications, emphasizing the critical role of user interface design and the application content in digital health management. Therefore, TAM provides a suitable theoretical foundation for analyzing the usability and acceptance of telemedicine interfaces among older adults in this review. Before designing and implementing telemedicine services, understanding elderly users’ perceptions, needs, and preferences is essential [41], as these factors significantly impact the acceptance of telemedicine services.
While prior studies have identified influencing factors for elderly telemedicine adoption, they fail to explore how these models can be applied in design practice. More importantly, there is no clear discussion on how to translate the findings from influencing factor models into concrete design strategies. Given the physiological decline and higher susceptibility to illness among older adults, they should be the primary beneficiaries of telemedicine services. However, current telemedicine systems do not adequately consider elderly users’ characteristics and preferences, making them unsuitable for this demographic. Also, very few articles have investigated mobile health applications for the elderly from the standpoint of interface and functional design [42]. There is a notable lack of comprehensive reviews that address factors affecting the usability of telemedicine interface design for older adults in previous studies. An absence of detailed guidelines also exists to instruct designers or developers in the design of telemedicine interfaces for the elderly.
The introduction of AI and 5G technology has brought innovative changes to telemedicine. However, current AI advancements focus mainly on functionality, often neglecting elderly users’ interaction and interface simplicity [43]. While 5G enhances telemedicine’s efficiency and stability, it frequently overlooks the user–interface interaction, with complex designs and processes posing barriers for elderly adoption [44].
Product design is crucial because it serves as the user’s “gateway” into the product and directly influences the user’s perception and experience by highlighting the style, quality, esthetics, ease of use, and reliability [45]. This paper attempts to combine the TAM with interface design, and proposes telemedicine interface design strategies that are suitable for the needs of the elderly, thereby improving the acceptance of telemedicine among the elderly. To achieve this, it is necessary to identify factors influencing interface usability, evaluate usability assessment methods, and provide recommendations for improving the usability of these interfaces. This review paper aims to answer the following questions:
- What design elements should be considered for older adults’ telemedicine interface design?
- What methods are used to evaluate the usability of interface design?
2. Methods
This review combines relevant articles from the domains of telemedicine, human–computer interactions, and usability evaluation. To ensure the comprehensiveness and accuracy of the sample data, retrieval strategies, methods, and principles were established [42,46]. Adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist, a systematic review on telemedicine for older adults was conducted to identify key elements for improving interfaces and assessing their usability. PRISMA offers researchers a clear reporting standard that includes a 27-item checklist and a flowchart, designed to improve transparency and integrity in research design, implementation, and analysis [47]. The PRISMA framework is employed to refine the research scope and identify key areas for peer review.
The analysis covered application description, health domains, and main findings. These included both quantitative and qualitative research, as well as mixed methods, without restrictions on design or outcome [48]. In alignment with the research objectives, each article was evaluated based on its research focus, objectives, methodologies, and key conclusions. For qualitative studies, reliability indicators were analyzed, while for quantitative studies, statistical analyses of the basic data were performed. Each article provided information on its research purpose, methods, target groups, and sample sizes. To ensure thoroughness, both forward and backward citation analyses were performed by reviewing references and citing articles, which resulted in the identification of one relevant article from the references.
2.1. Information Sources
The literature search for this review focused on four major databases: Scopus, Web of Science, PubMed, and CINAHL. Scopus is recognized as the largest database of peer-reviewed literature, covering various fields including health sciences, natural sciences, humanities, social sciences, and life sciences. Web of Science is an authoritative source that encompasses a broad range of disciplines from natural sciences to humanities. PubMed is a leading database for global medical and biomedical literature. CINAHL is specially tailored for nursing, allied health sciences, and related fields. To explore the influencing factors and usability of telemedicine interface design for the elderly, Boolean operations (AND) were used to combine keywords. The final search query was defined as: “TS = ((“elder*” OR “older adult*” OR “old people” OR “seniors” OR “aging” OR “the aged” OR “Geriatric”) AND (“telemedicine” OR “mobile application*” OR “telehealth” OR “mobile health” OR “mhealth” OR “ehealth” OR “digital health”) AND (“interface design” OR “user interface” OR “APP design” OR “application design” OR “UI” OR “UX” OR “user experience” OR “usability” OR “efficiency” OR “human factor” OR “design guidelines”))”. All terms were searched across titles, keywords, abstracts, and full text.
2.2. Eligibility Criteria
The databases Web of Science, Scopus, PubMed, and CINAHL were searched for articles related to the design of telemedicine interface for the elderly. The retrieved literature was exported into EndNote X20 software, where the first two authors screened the titles and abstracts of all retrieved studies, assessed the full texts of potentially eligible studies, and independently recorded the documents according to the screening criteria. Any discrepancies or disagreements during the screening and selection process were resolved through three researchers’ group discussion until consensus was reached. Inclusion and exclusion criteria were established based on the PICOS (Population, Intervention, Comparison, Outcome, Study design) framework (see Table 1) [49]. All articles included in this review were peer-reviewed and published between 2019 and 2024. The titles and abstracts of the papers were independently searched, followed by a thorough evaluation of the retrieved articles according to the inclusion criteria.

Table 1.
Inclusion and exclusion criteria based on the PICOS model.
2.3. Data Extraction and Analysis
Data extraction and analysis were conducted using tables that highlighted study characteristics, including authors, study design, participant characteristics, sample size, and country of origin. Grey literature and conference papers are often preliminary or exploratory in nature and typically do not undergo peer review. Moreover, it is relatively difficult to obtain and systematically collect such documents. Therefore, to ensure the quality and reliability of the selected literature, this study excluded grey literature and conference papers.
3. Results
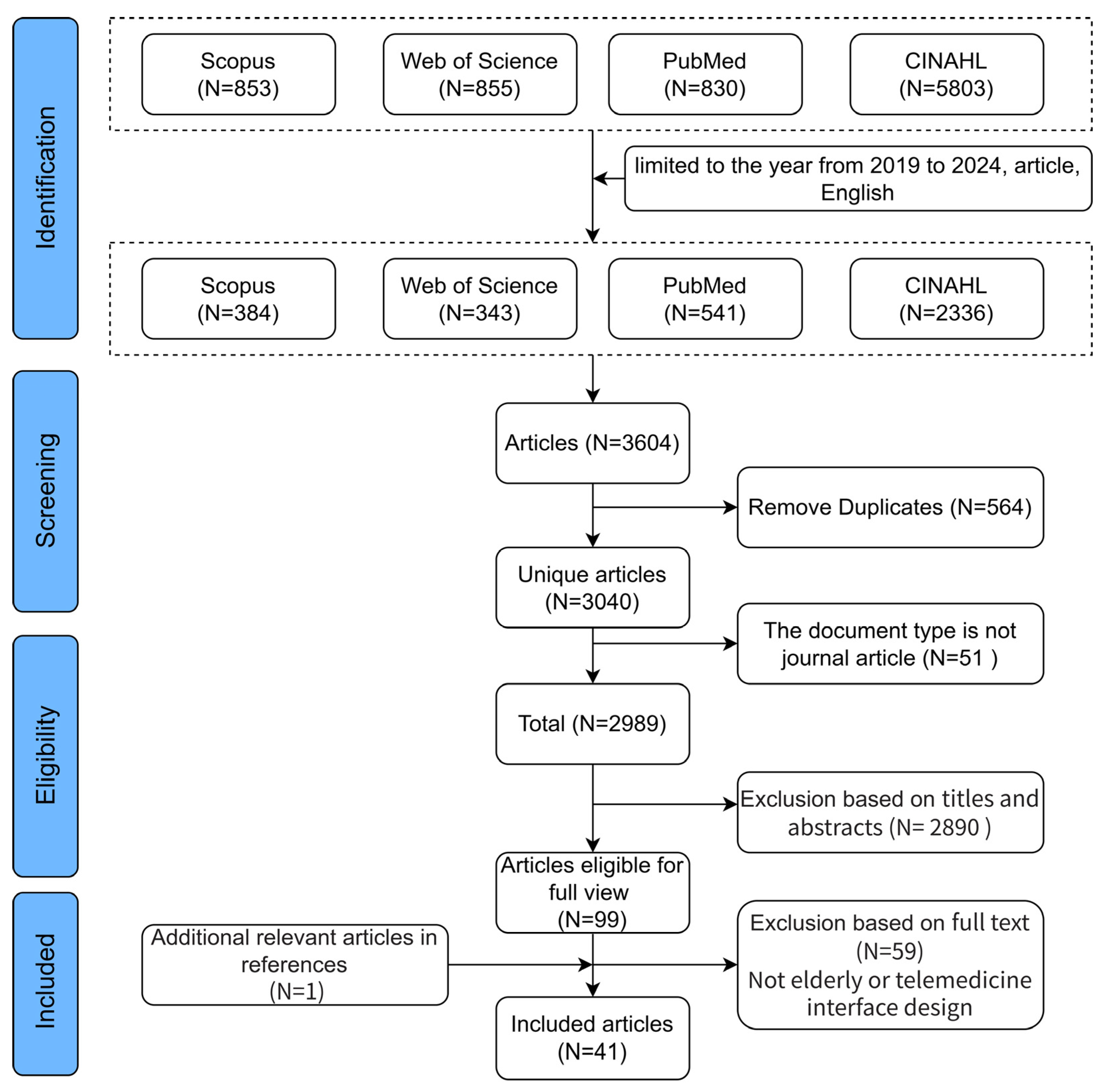
Data collection based on the outlined criteria was completed as of 18 August 2024. A topic search string was utilized with a time frame set from 2019 to 2024 to capture the most recent developments in telemedicine usability, particularly following the widespread adoption during the COVID-19 pandemic [4], limiting document types to “article” and language to “English”. A total of 384 articles were retrieved from Scopus. Similarly, 343 documents were obtained from the Web of Science, 541 publications were identified from PubMed, and 2336 publications were retrieved from CINAHL. In total, 3604 documents from the four databases were imported into EndNote for deduplication. After removing duplicates and excluding non-article document types, 2990 articles remained for title and abstract review. The study selection flowchart is shown in Figure 1. The following findings are derived from the systematic search and review of the selected studies.
Figure 1.
Study selection flowchart.
3.1. Study Characteristics
A summary table was developed to systematically capture relevant information from the 41 publications, including the author’s name, research method, country, sample size, participant characteristics, application description, main field, and main findings (Supplementary Material S1). This is supported by [46]. Among the 41 studies, 21 focused on health management, 6 on cognitive health, 4 on medication management, 4 on electronic health records, 3 on rehabilitation, 2 on behavioral medicine, 1 on health habits, and 1 on health information management.
In terms of research methodologies, 14 articles employed mixed methods, 13 utilized qualitative research, 10 conducted quantitative research, and 4 adopted experimental research. In terms of participant numbers, most studies included fewer than 100 participants. Specifically, 3 studies had between 4 and 7 elderly participants; in 15 studies, the sample size ranged from 10 to 20; in 14 studies, it ranged from 21 to 100; and in 9 studies, the number of participants exceeded 100.
3.2. Factors Affecting the Usability of Interface Design
The usefulness of a system for patients largely depends on whether its functions meet user needs [37]. In the design process, it is crucial to ensure that the system’s features meet the requirements of older adults, such as teleconsultation, health monitoring, and medication reminders, to enhance the perceived value. Clear interaction logic and effective visual design are critical to enhancing the perceived usefulness in telemedicine systems for older adults, as they facilitate efficient task completion, reduce errors, and strengthen users’ belief in the system’s effectiveness [16].
The perceived ease of use refers to users’ subjective perception of how easy or difficult it is to use telemedicine services, and the clarity and rationality of the design influence the level of effort required to use the technology. Effective interaction design can reduce the cognitive load, lower the learning curve [16], and improve the ease of learning by simplifying operation processes, incorporating voice interaction, streamlining interface hierarchies, using large fonts, and employing familiar icon-based buttons. These strategies help older users quickly locate target functions and improve their confidence in using the system. The user experience encompasses users’ emotional responses, satisfaction, and perceptions of usability during interactions [24]. A well-designed user experience, achieved by integrating emotional design elements and personalized assistance features, not only strengthens the perceived ease of use, but also enhances the overall user satisfaction [41].
Conversely, technology anxiety may be influenced by functional frameworks, interaction logic, and the overall user experience. Based on the reviewed studies, the TAM was integrated with key interface design elements (as shown in Figure 2) to bridge the identified research gap between influencing factor models and design practices. Additionally, it addresses the lack of detailed design guidelines in existing telemedicine systems, which often fail to fully consider the characteristics and preferences of older users. In the following sections, the findings from the search and review are organized and presented according to the four key design elements of interface design illustrated in Figure 2.
Figure 2.
Telemedicine technology acceptance model for older adults.
3.2.1. Functional Framework
To accommodate the cognitive and navigation limitations of older adults, telemedicine application design should simplify functionality, minimize complex visuals, and optimize touch interface operations to reduce the interference and learning burden [19,20]. Systems can automatically recommend health topics of interest, including diseases, symptoms, treatments, medications, diet plans, and alternative therapies [13]. Telemedicine services encompass remote consultations, treatment, health management, medication sales, and monitoring, supported by functional frameworks emphasizing medication schedules, dosages, instructions, and disease information analysis [19]. For seniors’ behavioral health, telemedicine applications should integrate goal setting, behavior planning, emergency management, data recording, disease information, medical calculators [13,51], monitoring, feedback mechanisms, social support, reminders, and health outcome tracking [52]. Additionally, these applications facilitate appointment scheduling, status tracking, troubleshooting, exercise reminders, educational resources, dietary advice, social communication [20], and instructional video guidance [53].
Interaction and reminder functions are critical for medication management applications for older adults, enabling users to display, mark, snooze, skip, and add medications, as well as generate reports [54]. Key features should include medication and risk management, health information sharing, communication tools, stroke components, rapid synchronization, and immediate system modifications upon failure [55,56]. Essential design attributes include large fonts, simple operations, timely reminders, reliable hardware, WeChat integration for drug instructions, enhanced system sensitivity, and an extended battery life [57]. Although older adults often overlook app instructions [58], messaging features can improve engagement [59], while start or stop reminders help address memory impairments and concerns about polypharmacy [13,60]. Notifications conveying status changes, combined with confirmation buttons or voice broadcasts [61], along with timer and progress bar functions for the real-time tracking of appointments and tasks [62], further enhance usability. Additionally, sound-effect prompts can assist users in navigating registrations, consultations, and payment confirmations.
For elderly individuals, especially those living alone, emotional support, cognitive wellness, and motivation are critical. Social interaction features should be prioritized, as they provide older adults with opportunities to connect with others, enhancing their sense of recognition and encouraging healthier behaviors through praise and rewards [50,55]. A well-designed app with flexible scheduling and peer interactions, such as those demonstrated in cancer survivor programs, can increase participation in health programs [63]. Additionally, feedback mechanisms, motivation tools, monitoring capabilities, and alarm features have proven effective in engaging older adults with insomnia [59]. Telemedicine applications should incorporate interactive features, voice feedback, automatic monitoring, disease tracking, and visual health reports. Including a home screen icon to explain app functions can enhance user understanding, while the automatic identification of user interests can minimize the manual input [59,64]. Disease tracking and concise summary reports linking daily mood changes with relevant symptoms and actionable steps will further improve the user experience [60].
3.2.2. Interaction Logic
For the elderly, both motor control precision and manual dexterity are impacted by aging [65,66]. Accidental touches are the most common issue hindering effective operation [67]. Navigation challenges are a primary concern [68,69], where seniors often struggle to navigate through app features, leading to a disconnect between perceived usability and actual usability [69]. Researchers and designers must recognize the physical limitations of the elderly, allowing users to transfer data to other devices and input information retroactively [20]. System navigation and feedback are essential components of the application’s interactive logic.
Feedback should include both visual and auditory cues, as elderly users often seek confirmation of task completion to enhance their confidence in using applications [66]. The accuracy and sensitivity of voice interaction systems can significantly improve the user experience in mobile health applications [18]. Feedback should integrate visual changes with sound cues, allowing users to adjust the volume, enable vibration, and access audio–visual instructions [54,70]. Utilizing family members’ voices for reminders can add a personal touch [54]. An Arabic-based health app employs a tagging and notification system for progress and providing positive feedback [12,19]. Personalized information and timely notifications can enhance telemedicine usage [71], while the app should support multiple languages and avoid technical jargon [13,58,72]. While positive feedback and clear training messages can motivate users [72], excessive reminders should be avoided [70].
Given that older adults often struggle to process large amounts of information, app navigation should be consistent, concise, and clear. A step-by-step approach with minimal steps and straightforward interaction instructions is essential [13,66,73]. An intuitive user interface, along with a clear background and easy-to-navigate design, enhances readability [60,73]. “Breadcrumb” navigation can assist users with poor short-term memory by minimizing steps and confirmation messages, avoiding complex gestures, and ensuring quick response times [13]. The interface should display only task-related information, avoiding parallel tasks, pop-ups, and dialog boxes [65], while providing spacious click areas and clearly visible buttons for improved accessibility [70]. Considering older adults’ health knowledge, the app should feature intuitive navigation, visual feedback, a simple registration process, interactive tutorials, and multiple access methods such as a table of contents, link lists, and search functions [18,66,70]. Clear buttons for returning to the home screen, proceeding, canceling, or completing tasks should guide users effectively [58,74]. Additionally, users should be able to recall steps using photos or illustrations. Voice recognition can assist with voice-to-text conversion for easier information retrieval, navigation, emergency requests, and updates [13].
To address input method challenges for older users, developers should implement larger touch targets and identify touch-sensitive areas [70]. Utilizing gesture-based controls and incorporating predictive text input can reduce effort and minimize error [69], allowing the system to anticipate input content in advance [75].
3.2.3. Visual Design
The telemedicine interface for the elderly should be clear and straightforward, incorporating effective layouts, graphics, colors, fonts, language, and icons to facilitate the quick completion of medical tasks. It must address the visual, technical, physical, emotional, and cognitive needs of elderly users by utilizing large fonts, clear outlines, and high-contrast colors to enhance the readability [76]. Five key considerations that should be considered when designing interfaces specifically tailored for older adults are as follows:
(1) Colors. Choosing appropriate colors for older users requires the careful consideration of both their preferences and visual abilities. Older adults generally favor blue and pink fonts on blue or turquoise backgrounds, and it is advisable to limit the color scheme to three colors while categorizing information and respecting cultural beliefs, such as the use of blue, green, and black in Arabic mobile health applications [19,54]. High-contrast combinations, like red text on neutral backgrounds, improve the readability and recognition, whereas yellow text is harder to discern and should be avoided [58,60,77]. To enhance accessibility, designs should use vivid, high-contrast colors, large fonts, a cohesive color palette, and ensure screen reader compatibility [60,66]. Additionally, color schemes should align with content meaning, such as using pain scale colors to reflect severity levels, where the yellow-to-red gradient is a recognized sequence [73].
(2) Shape, icon buttons, and labels. Compared to round shapes, older adults generally prefer rectangular shapes [54]. The interface design should be concise and clear, featuring distinct labels and themes [13]. Icons should combine simple, multi-functional symbols with accompanying text and use large buttons for easy clicking, while ensuring visual appeal [73]. Skeuomorphic designs that mimic real-world objects are particularly effective for older users, improving comprehension compared to minimalist styles [61]. Since older adults tend to favor text labels over abstract icons, icon designs should adopt familiar styles [77]. Additionally, live links must be clearly distinguished from icons and text to prevent accidental clicks, and links should avoid opening in new windows to reduce confusion [13].
(3) Font. Font size plays a significant role in interface readability, with larger fonts enhancing the usability for older users [58,59,78]. A minimum font size of 18 pt is recommended, with Proxima Nova and Arial being the preferred sans-serif fonts due to their high recognition [54]. While some studies suggest 12 pt for body text and 14 pt for titles [12], employing a font size of 22 pt can reduce the operation time for seniors, improving their performance to levels comparable to younger users [67]. Factors such as font appearance, spacing, alignment, and background also influence the readability. It is advisable to use adjustable fonts, clear text, bold key information, contextual explanations, and ensure good contrast between the text and background [13,60,69,70]. Font size standards may vary by language, which can affect the legibility.
(4) Layout. The layout design should consider users’ reading and writing habits, such as the right-to-left orientation preferred in Arabic culture [19]. The content must be logically organized to ensure a clear reading order and task flow, with a consistent placement of logos and buttons [70]. Each page should include navigation buttons, and the functional layout should prioritize the portability [60]. Familiar interfaces enhance the predictability and comprehension; therefore, maintaining a consistent layout and standard page design is essential for improving the usability [13].
(5) Data visualization. Data visualization is crucial for self-tracking technology as it aids in identifying trends and promoting behavioral changes. However, design guidelines for the elderly remain unclear and require empirical research [77]. Users prefer bar charts for clarity and accuracy in data feedback [77,79], and it is suggested that emojis be used instead of charts, as they serve as a universal language for most users [77,79].
3.2.4. User Experience
Older adults face barriers to telehealth due to limited computer experience, unfamiliarity with e-health applications, and mismatched needs [74]. They often struggle with comprehension, data entry, and terminology, while the screen design significantly impacts their satisfaction [12,74]. Security and privacy concerns can also hinder their willingness to use these services [56]. Addressing these issues, along with cultural adaptation, a simple design, and clear content, can enhance user satisfaction [12]. The system should ensure accessibility and provide a sense of control by centralizing information for monitoring health, checking medications, and accessing data [56]. Shah [70] proposed eight usability structures, including a readable design, text style, layout, navigation, learning, memory load, user guidance, and error handling. Additionally, in gait test applications, incorporating background music can improve the user experience, and including reference ranges for gait parameters with clear explanations is essential [78].
To address these challenges and improve the overall user experience for older adults in telehealth applications, six key strategies can be implemented:
(1) Gamification. Gamification has become an increasingly popular approach in various fields, particularly in healthcare technology. Gamification enhances user interest and engagement by making experiences enjoyable and is commonly used as a motivation strategy [72]. It should consider users’ disease characteristics and preferences while balancing the need to improve both the gaming experience and interface usability. Elements such as rewards and competition can motivate older adults [66], while features like a flashing “done” button or task countdown can further boost engagement [58].
(2) Sociability. Elderly individuals often experience loneliness and social isolation due to mobility or health issues [42]. Barriers to using health websites include navigation difficulties [68,80], hard-to-understand accents, poor accessibility, and low digital literacy [80]. Key intrinsic motivations for using health service apps include maintaining health, independence, social connection, and caring for others. Extrinsic motivations include saving time, accessing health information, and receiving rewards [81].
(3) Personalization. Addressing the personalized technology needs of the elderly can help bridge the digital divide and enhance satisfaction with telemedicine services [57]. Technology enables engaging and tailored interventions that can boost physical activity among older adults [71]. When designing telemedicine applications, it is essential to consider factors such as gender, health information needs, and the usage frequency to create personalized strategies for those who may be less attentive to health information [50]. Providing credible, high-quality, tailored information effectively promotes healthy lifestyles in older adults [63].
(4) Ease of use. Elderly users often struggle with complex functions, thus, apps should be simple, engaging, and user-friendly [58]. They should utilize large, clearly visible buttons and intuitive interfaces [64]. The system must facilitate smooth navigation with easy-to-understand content [69], allowing users to quickly learn its operations [13,70]. To minimize the memory load and mental effort, the app should be task-focused, providing ample time for users to read and respond while keeping instructions visible at the top of the screen to guide them through tasks [70]. Given their tendency toward forgetfulness and risk aversion, elderly users often rely on clear operational instructions or assistance from others [68].
(5) Fault tolerance. The application should include error correction capabilities, quick input responses, and user guidance for handling mistakes while avoiding complex error messages [13]. It must highlight common options, allow users to skip irrelevant queries, and support information clearing or restoration [70]. Clear explanations, tutorials, or contact information should be provided for errors [13], along with enhanced accessibility features such as text-to-speech, a high contrast mode, and a simplified interface for users with varying abilities [69].
(6) User-centered. Telemedicine interfaces for the elderly should prioritize a user-centered design by involving older consumers in the development process to meet their specific needs and preferences [69]. Applications must be accessible, easy to use, and efficient [66], promoting the acceptance of telemedicine and enhancing independent living. Tailoring the design to the unique characteristics and habits of older adults is crucial to ensure rapid response times and minimal loading delays for an optimal user experience [61,69,74]. The application should function as intended to prevent negative emotions or self-blame [68].
Based on the above analysis, the interface design guidelines for the elderly have been organized based on functional design, interaction logic, visual design, and user experience, as shown in Table 2.

Table 2.
Summary of factors affecting telemedicine interfaces design for the elderly.
3.3. Usability Evaluation Methods for Interface Design
After examining the key factors affecting the usability of telemedicine interfaces for older adults, including a functional framework, interaction logic, visual design, and user experience, it becomes evident that these design elements directly impact users’ perceived usefulness, perceived ease of use, operational efficiency, and overall satisfaction. However, merely analyzing the design factors influencing the interface usability is not sufficient. It is essential to systematically assess these factors using scientific usability evaluation methods to verify whether the interface truly meets the needs of older users. Understanding the elements that impact usability provides a solid foundation for ensuring that interface designs align with user needs and expectations. To translate these insights into actionable improvements, a structured approach to usability evaluation is required.
The System Usability Scale (SUS) is widely recognized for evaluating usability. This is consistent with the review by Takano [24], as SUS is simple and effective in evaluating the user experience of data health for the elderly. Among the 41 studies included in this review, 12 utilized the SUS scale for the usability assessment, while 3 conducted usability testing experiments. Additionally, two studies employed the User Experience Questionnaire (UEQ) and another two used the Mobile App Rating Scale (MARS). Other methods included the modified Computer Self-Efficacy Scale (mCSES), Usability Metric for User Experience (UMUX), eHealth Impact Questionnaire (eHIQ), Computer System Usability Questionnaire (CSUQ), Questionnaire for User Interface Satisfaction (QUIS), Nielsen’s usability model, Suitability Assessment of Materials (SAM), and Health Information Technology Usability Evaluation Scale (H-ITUES), with each of these methods being represented by a single study in the evaluations. One study did not specify the usability evaluation scale clearly, but relied solely on questionnaires to assess the usability from various dimensions. Furthermore, 18 studies did not conduct clear usability evaluations. A summary of usability testing methods is provided in Table 3.

Table 3.
Summary of existing usability evaluation methods.
4. Discussion
To facilitate the application of the results of this study in the development of telemedicine applications, we provide a design elements checklist in Table 2. These elements can be used to develop design guidelines and offer recommendations and identify factors that influence the interface usability across various levels of abstraction, covering the functional framework, interaction logic, visual design, and user experience in telemedicine. This makes them accessible for interface designers and developers. For each category, specific implementation and design elements relevant to telemedicine applications for the elderly were analyzed to facilitate the ease of use by designers and software developers. These design elements are applicable to various telemedicine applications aimed at older adults. This study indicates that the System Usability Scale (SUS) is the most commonly used evaluation method for telemedicine, although there remains a need to strengthen the experimental verification and evaluation.
The research also revealed that only five studies were grounded in theory, including the User Center Design [73,76,88], Technology Acceptance Model (TAM) [19], Grounded Theory [86], and the Kano model [57]. However, existing studies primarily use theoretical models as design tools or analyze factors influencing acceptance, without closely integrating theoretical frameworks with interface design elements. Given that functionality, interactivity, esthetics, and user experience significantly impact the acceptance and usability of new technologies, this study aims to enhance the elderly acceptance of telemedicine. For the first time, it integrates key interface design elements with the TAM to develop a conceptual framework (Figure 2), guiding designers in creating effective telemedicine systems for older adults. Future studies should adopt theory-driven applied design to uncover the mechanisms behind design features relevant to aging theory. Current studies predominantly rely on interviews, focus groups, and questionnaires, with limited experimental evidence and a lack of comparison groups. Often, these studies evaluate entire applications rather than individual design elements, as noted by Liu [42].
Given the diverse health and medical needs of older adults compared to younger individuals, it is essential to create an aging-friendly version of telemedicine interfaces. While some scholars argue against developing separate versions [14], we advocate for a user-centered approach that tailors functions specifically for older users, thereby enhancing the design applicability to meet their needs. This process should involve exploring user requirements and conducting usability testing, as user participation is crucial for successful information technology design, ultimately improving satisfaction and usage. Although many studies emphasize simplicity to reduce complexity, this principle benefits users of all ages, including younger individuals.
To ensure these design principles effectively enhance the usability, systematic evaluation methods must be employed to validate their effectiveness and refine the interface based on user needs. Currently, most studies assess interface design usability using questionnaires, while only a few employ experimental evaluations. Although questionnaires allow for a multidimensional assessment, they are inevitably influenced by testers’ subjectivity. In contrast, experimental evaluations, despite being time-consuming and labor-intensive, provide greater objectivity and accuracy. Only a few studies have suggested the need for more comprehensive evaluations of health information systems using mixed methods, including user interface design and user experience, semi-structured interviews, observation, and think-aloud methods [51]. Nielsen’s heuristic evaluation suggests providing step-by-step assistance and documentation for elderly users to facilitate their understanding of system instructions [13,66,89]. This article presents six usability recommendations aimed at improving the interface design, namely, intuitive and simplified navigation, timely multi-sensory feedback, information visualization, personalized settings, social interaction, and enhanced health literacy.
The usability of telemedicine interface design is vital for improving the user experience and medical service quality for the elderly, while also impacting economic policy and investment decisions. Firstly, better interface usability reduces healthcare costs by improving elderly users’ operational efficiency, minimizing errors and misdiagnoses. Enhanced usability also promotes broader adoption, alleviating healthcare pressures from an aging population, increasing service supply, easing resource shortages, and stimulating growth in related industries. Secondly, the aging population creates a large market for elderly telemedicine services. Investors should focus on companies with strong interface designs, as these can quickly capture the market share. User-friendly designs attract elderly users and enhance engagement, encouraging long-term service use.
However, despite the promising prospects and benefits, designing highly usable telemedicine interfaces for the elderly still faces several critical challenges that must be addressed. The main challenges in mobile app design include the timing of stakeholder involvement, overcoming designer assumptions, adapting to end users, and managing stakeholder diversity [88]. To improve telemedicine usability for the elderly, it is essential to focus on key design aspects. The following recommendations are proposed to enhance the interface design for usability for elderly users:
(1) Intuitive navigation: Implement a concise navigation system with clear text labels or icons, progressive guidance, and dynamic prompts to help elderly users understand functions and operation processes [13,73]. Simplify input methods, increase fault tolerance, and provide a touch-friendly design that includes multiple input options such as text, voice, and image recognition to minimize reliance on buttons [69]. Navigation should prioritize primary functions, minimize secondary features to reduce the cognitive load, and ensure responsive feedback mechanisms to enhance accessibility and usability [72].
(2) Multi-sensory feedback: Enable user feedback for continuous interface improvements and service quality enhancement. Integrate multi-sensory feedback (visual, auditory, and tactile) [54,70] and health reminders, ensure clear system feedback, provide voice or video communication options, obtain patient consent for video features, and send reminders before session completion to enhance user engagement and satisfaction [62].
(3) Information visualization design: When elderly patients need to make appointments without knowing the specific department or doctor, the system can guide them by allowing them to select a body part on a rotatable and scalable 3D model for detailed observation. The system should then recommend relevant specialists. Users should have control over the amount of information displayed about doctors and be able to easily comprehend health data, progress, and goals through data visualization in user reports [62].
(4) Personalized settings: Allow users to manage their health information, customize fonts and color schemes, and arrange homepage functions according to their individual needs. Also, users should be allowed to customize frequently used features to reduce distractions [89]. This customization facilitates quicker access to desired functions [69]. Instructional videos and brief tutorials can help elderly users learn the interface more efficiently. Accessible help resources, expanded service content, and improved effectiveness will promote mobile health service adoption [81].
(5) Social interaction and emotional support: To alleviate technological anxiety and reduce the lengthy learning curve for elderly users [58], applications should enable seniors to grant partial access to family members or caregivers. This feature provides simple social connection options that help them stay in touch with family, friends, and healthcare providers, fostering a sense of security [83]. A warm and friendly interface with compassionate language and supportive interactions can mitigate feelings of loneliness and anxiety [70].
(6) Improving health literacy: Since many elderly users are unfamiliar with technology and exhibit cognitive differences, telemedicine apps should offer tutorials, active help [14], and training specifically designed for older adults [68,75] to assist them in navigating the system effectively despite cognitive and physical challenges [63]. Research indicates that older patients spend more time using smartphones than younger patients [58]. Declining cognition, memory issues, and reduced finger sensitivity in the elderly can lead to increased errors, thus proper guidance and public awareness through mobile app marketing are essential for successful usage. Face-to-face assistance can also reduce technological anxiety and improve tech literacy [75,83]. Health data visualizations should align with users’ literacy levels [18]. Positive correlations exist between attitudes toward online health information, confidence, understanding, and motivation, and usability ratings of the learning platform. This indicates that eHealth literacy influences evaluations of eHealth coaches [87].
Finally, older individuals often overlook their privacy concerns [57]. It is crucial to strengthen user privacy and security by incorporating emergency contact functions, real-time monitoring capabilities, and integrating service platform resources. When designing mobile health research, it is important to consider the participants’ views on privacy, data confidentiality, and their willingness to share research results [64].
The selected studies reveal significant qualitative and quantitative differences, including the sample size, study setting, and population characteristics, for example, sample sizes range from small groups of 4 participants (e.g., Sweden-based fall prevention interventions) [65] to larger studies with over 600 participants (e.g., Saudi Arabia-based mobile user interface studies) [54]. Qualitative studies generally had smaller sample sizes and were often used to analyze or address specific diseases, such as fall prevention programs [52,65] and studies on blind and visually impaired individuals [18,82], while the target populations of quantitative studies were relatively broader. Study settings also vary from urban environments in the USA to culturally specific designs in Arab nations. Population characteristics, such as age range, gender distribution, and health conditions (e.g., Alzheimer’s disease [86], diabetes [20], or cognitive impairment [83]), further highlighted the heterogeneity. These differences may lead to biased conclusions, especially when generalizing the research findings to different populations. We observed that larger and more diverse samples tend to produce more universal insights, while smaller-scale or culturally specific studies provide in-depth but narrow perspectives. To address potential biases, future studies should strive to adopt standardized methods and enhance representativeness in both the environment and population.
Limitations
The first limitation of this study is the age restriction applied for the elderly population. Given the earlier onset of geriatric diseases, we set the minimum age at 50 years old and included as many studies as possible. However, user characteristics across different age ranges may lead to varying needs and results. Future research may stratify older adults into narrower age groups to allow for more targeted interface design strategies in telemedicine. Secondly, in terms of the literature review, we excluded conference papers, the gray literature, and unpublished articles, limiting our sources to journal articles written in English. Due to the substantial number of articles retrieved, only the literature from the past five years was considered, since design trends may evolve over time. We believe that the number of articles reviewed is sufficient for analysis. The use of only four databases may limit the screening, but it is believed that Web of Science, Scopus, PubMed, and CINAHL cover most papers on telemedicine for the elderly. Additionally, preliminary keywords were tested in multiple databases to avoid missing the relevant literature due to differing search strategies.
5. Conclusions
Extensive research indicates that mobile app design significantly improves usability for the elderly. This article provides a systematic review of the factors affecting the usability of telemedicine interface design for older adults, identifying key elements of effective interface design. Through thematic analysis, the elements are organized into four key areas affecting the usability of interface design, namely, the functional framework, interaction logic, visual design, and user experience. Given the close relationship between the interface design, acceptance, and usability, this study is the first to integrate the four key elements of interface design with the Technology Acceptance Model (TAM) to develop a new conceptual framework for elderly telemedicine acceptance. Future research can validate this framework by formulating hypotheses and analyzing data. It also summarizes usability evaluation methods and offers recommendations to enhance the interface usability for future design initiatives.
Most studies prioritize the System Usability Scale (SUS) for the usability evaluation, while relatively few rely on experimental assessments. Furthermore, many studies do not conduct usability evaluations on telemedicine applications. Although this design elements checklist does not guarantee perfect usability, it aims to support user-centered design and help bridge the digital divide. It can be used to develop design guidelines and guide designers and developers. These design elements and usability evaluation have an important reference value for governments in formulating telemedicine policies and for entrepreneurs investing in telemedicine.
It is noted that this paper mainly explores the universal design elements of mobile telemedicine. Remote medical applications for specific diseases may require differentiated adjustments. For example, for people with visual impairments, more voice guidance may be needed. For users with cognitive impairments, functions such as technical literacy and social interaction should be emphasized. And fall prevention applications need to provide health guidance and intervention. Further studies ought to concentrate on examining the particular effects and results linked to every kind of telemedicine, thereby facilitating a more refined comprehension of their individual merits and drawbacks. Future research can also focus on comparing telemedicine interface designs across different countries and conducting a comprehensive market evaluation. In subsequent studies, we will develop a telemedicine interface design guideline for the elderly based on this literature review, and explore the priority and importance of each design element. We will also verify the effectiveness of the design guideline through controlled experiments.
Promoting accessible and user-friendly telemedicine platforms for the elderly is crucial for fair healthcare access, digital inclusion, and aligns with the United Nations’ Sustainable Development Goals for 2030. This analysis fosters interdisciplinary studies and guides designers and policymakers in developing sustainable telemedicine solutions that improve healthcare services and the quality of life for the aging demographic worldwide. It also encourages ongoing research to guarantee the inclusivity and efficacy of these systems.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app15105458/s1.
Author Contributions
H.H.: Conceptualization, Methodology, Writing—Original Draft, Data Curation, Formal Analysis, Visualization. R.A.R.G.: Supervision, Methodology, Writing—Review and Editing. S.H.A.-R.: Supervision, Conceptualization, Writing—Reviewing and Editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Guangdong Provincial Philosophy and Social Sciences Planning 2023 Discipline Co-construction Project “Research on the Construction of Telemedicine Health Service System for the Elderly from the Perspective of Active Aging” (GD23XYS025). The 2024 Guangdong Technology College Student Innovation Training Program Provincial Project “Research on the Design of Telemedicine Service System for the Elderly under the Perspective of Active Aging” (S202413720025). 2025 Guangdong Technology College’s annual school-level research platform project “Artificial Intelligence-driven mobile medical emotional service system design” (2025YBSK039).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. The UN Decade of Healthy Ageing 2021–2030 in a Climate-Changing World; Decade of Healthy Ageing Connection Series; World Health Organization: Geneva, Switzerland, 2022; Volume 3. [Google Scholar]
- Chun, Y.J.; Patterson, P.E. A usability gap between older adults and younger adults on interface design of an Internet-based telemedicine system. Work-A J. Prev. Assess. Rehabil. 2012, 41, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Mulgund, P.; Sharman, R.; Rifkin, D.; Marrazzo, S. Design, Development, and Evaluation of a Telemedicine Platform for Patients with Sleep Apnea (Ognomy): Design Science Research Approach. JMIR Form. Res. 2021, 5, 15. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Abdul-Rashid, S.H.; Ghazilla, R.A.R. Research Trends and Hot Spots in Telemedicine for the Elderly: A Scientometric Analysis. Healthcare 2024, 12, 1853. [Google Scholar] [CrossRef] [PubMed]
- Clausen, T.C.; Greve, N.K.; Müller, K.I.; Kristoffersen, E.S.; Schytz, H.W. Telemedicine in headache care: A systematic review. Cephalalgia 2022, 42, 1397–1408. [Google Scholar] [CrossRef]
- Merrell, R.C. Geriatric telemedicine: Background and evidence for telemedicine as a way to address the challenges of geriatrics. Healthc. Inform. Res. 2015, 21, 223–229. [Google Scholar] [CrossRef][Green Version]
- Narasimha, S.; Madathil, K.C.; Agnisarman, S.; Rogers, H.; Welch, B.; Ashok, A.; Nair, A.; McElligott, J. Designing telemedicine systems for geriatric patients: A review of the usability studies. Telemed. E-Health 2017, 23, 459–472. [Google Scholar] [CrossRef]
- Meng, F.B.; Guo, X.T.; Peng, Z.Y.; Lai, K.H.; Zhao, X.L. Investigating the Adoption of Mobile Health Services by Elderly Users: Trust Transfer Model and Survey Study. JMIR Mhealth Uhealth 2019, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Chun, Y.J.; Patterson, P.E. A suggestion for future research on interface design of an internet-based telemedicine system for the elderly. Work-A J. Prev. Assess. Rehabil. 2012, 41, 353–356. [Google Scholar] [CrossRef]
- Wildenbos, G.A.; Jaspers, M.W.; Schijven, M.P.; Dusseljee-Peute, L. Mobile health for older adult patients: Using an aging barriers framework to classify usability problems. Int. J. Med. Inform. 2019, 124, 68–77. [Google Scholar] [CrossRef]
- Rogers, W.A.; Fisk, A.D. Toward a psychological science of advanced technology design for older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2010, 65, 645–653. [Google Scholar] [CrossRef]
- Alsswey, A.; Al-Samarraie, H.; Malak, M.Z. Older adults’ satisfaction with mHealth UI design-based culture: A case study of Jordan. J. Hum. Behav. Soc. Environ. 2023, 33, 565–577. [Google Scholar] [CrossRef]
- Tajudeen, F.P.; Bahar, N.; Tan, M.P.; Peer Mustafa, M.B.; Saedon, N.I.; Jesudass, J. Understanding user requirements for a senior-friendly mobile health application. Geriatrics 2022, 7, 110. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Hernandez, M.; Ferre, X.; Moral, C.; Villalba-Mora, E. Design guidelines of Mobile apps for older adults: Systematic review and thematic analysis. JMIR mHealth uHealth 2023, 11, e43186. [Google Scholar] [CrossRef]
- Barnum, C.M. Usability Testing Essentials: Ready, Set... Test; Morgan Kaufmann: Burlington, MA, USA, 2020. [Google Scholar]
- Sharp, H.; Rogers, Y.; Preece, J. Interaction Design: Beyond Human-Computer Interaction; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2023. [Google Scholar]
- Wildenbos, G.A.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Sajib, M.; Manzano, J.; Chlebek, C.J. mHealth Technology Experiences of Middle-Aged and Older Individuals With Visual Impairments: Cross-Sectional Interview Study. JMIR Form. Res. 2023, 7, 12. [Google Scholar] [CrossRef]
- Alsswey, A.; Al-Samarraie, H. Elderly users’ acceptance of mHealth user interface (UI) design-based culture: The moderator role of age. J. Multimodal User Interfaces 2020, 14, 49–59. [Google Scholar] [CrossRef]
- Alkawaldeh, M.Y.; Jacelon, C.S.; Jeungok, C. Usability testing of a tablet-based self-management application for older adults with T2DM: The ASSISTwell application. Gerontechnology 2020, 20, 1–13. [Google Scholar] [CrossRef]
- Saparamadu, A.A.D.N.S.; Fernando, P.; Zeng, P.; Teo, H.; Goh, A.; Lee, J.M.Y.; Lam, C.W.L. User-centered design process of an mHealth app for health professionals: Case study. JMIR mHealth uHealth 2021, 9, e18079. [Google Scholar] [CrossRef]
- Marcus, A. Dare we define user-interface design? Interactions 2002, 9, 19–24. [Google Scholar] [CrossRef]
- Blair-Early, A.; Zender, M. User interface design principles for interaction design. Des. Issues 2008, 24, 85–107. [Google Scholar] [CrossRef]
- Takano, E.; Maruyama, H.; Takahashi, T.; Mori, K.; Nishiyori, K.; Morita, Y.; Fukuda, T.; Kondo, I.; Ishibashi, Y. User Experience of Older People While Using Digital Health Technologies: A Systematic Review. Appl. Sci. 2023, 13, 12815. [Google Scholar] [CrossRef]
- Almeida, A.F.; Rocha, N.P.; Silva, A.G. Methodological quality of manuscripts reporting on the usability of mobile applications for pain assessment and management: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 785. [Google Scholar] [CrossRef]
- Bateman, D.R.; Srinivas, B.; Emmett, T.W.; Schleyer, T.K.; Holden, R.J.; Hendrie, H.C.; Callahan, C.M. Categorizing health outcomes and efficacy of mHealth apps for persons with cognitive impairment: A systematic review. J. Med. Internet Res. 2017, 19, e301. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, C.; Prando, B.C.; Dantas, L.O.; da Silva Serrão, P.R.M. Mobile health technologies for the management of spine disorders: A systematic review of mHealth applications in Brazil. Musculoskelet. Sci. Pract. 2022, 60, 102562. [Google Scholar] [CrossRef] [PubMed]
- da Silva, H.E.C.; Santos, G.N.M.; Ferreira Leite, A.; Mesquita, C.R.M.; de Souza Figueiredo, P.T.; Miron Stefani, C.; de Santos Melo, N. The feasibility of telehealth in the monitoring of head and neck cancer patients: A systematic review on remote technology, user adherence, user satisfaction, and quality of life. Support. Care Cancer 2022, 30, 8391–8404. [Google Scholar] [CrossRef]
- Leiz, M.; Pfeuffer, N.; Rehner, L.; Stentzel, U.; van den Berg, N. Telemedicine as a Tool to Improve Medicine Adherence in Patients with Affective Disorders–A Systematic Literature Review. Patient Prefer. Adherence 2022, 16, 3441–3463. [Google Scholar] [CrossRef] [PubMed]
- Sen, K.; Prybutok, G.; Prybutok, V. The use of digital technology for social wellbeing reduces social isolation in older adults: A systematic review. SSM-Population Health 2022, 17, 101020. [Google Scholar] [CrossRef]
- AlQudah, A.A.; Al-Emran, M.; Shaalan, K. Technology Acceptance in Healthcare: A Systematic Review. Appl. Sci. 2021, 11, 10537. [Google Scholar] [CrossRef]
- Binyamin, S.S.; Zafar, B.A. Proposing a mobile apps acceptance model for users in the health area: A systematic literature review and meta-analysis. Health Inform. J. 2021, 27, 1460458220976737. [Google Scholar] [CrossRef]
- Dash, D.M.; Shadangi, D.P.Y.; Kar, D.S.; Prusty, M.R. A Conceptual Model for Telemedicine Adoption: An Examination of Technology Acceptance Model. Int. J. Recent Technol. Eng. (IJRTE) 2019, 8, 1286–1288. [Google Scholar] [CrossRef]
- Rouidi, M.; Elouadi, A.; Hamdoune, A. Acceptance and use of telemedicine technology by health professionals: Development of a conceptual model. Digit Health 2022, 8, 20552076221081693. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Davis, F.D. User acceptance of information technology: System characteristics, user perceptions and behavioral impacts. Int. J. Man-Mach. Stud. 1993, 38, 475–487. [Google Scholar] [CrossRef]
- Kamal, S.A.; Shafiq, M.; Kakria, P. Investigating acceptance of telemedicine services through an extended technology acceptance model (TAM). Technol. Soc. 2020, 60, 101212. [Google Scholar] [CrossRef]
- Kitsiou, S.; Paré, G.; Jaana, M. Effects of home telemonitoring interventions on patients with chronic heart failure: An overview of systematic reviews. J. Med. Internet Res. 2015, 17, e63. [Google Scholar] [CrossRef] [PubMed]
- Shemesh, T.; Barnoy, S. Assessment of the Intention to Use Mobile Health Applications Using a Technology Acceptance Model in an Israeli Adult Population. Telemed. E-Health 2020, 26, 1141–1149. [Google Scholar] [CrossRef]
- Park, Y.E.; Tak, Y.W.; Kim, I.; Lee, H.J.; Lee, J.B.; Lee, J.W.; Lee, Y.R. User Experience and Extended Technology Acceptance Model in Commercial Health Care App Usage Among Patients with Cancer: Mixed Methods Study. J. Med. Internet Res. 2024, 26, e55176. [Google Scholar] [CrossRef]
- Ekstedt, M.; Kirsebom, M.; Lindqvist, G.; Kneck, Å.; Frykholm, O.; Flink, M.; Wannheden, C. Design and development of an ehealth service for collaborative self-management among older adults with chronic diseases: A theory-driven user-centered approach. Int. J. Environ. Res. Public Health 2022, 19, 391. [Google Scholar] [CrossRef]
- Liu, N.; Yin, J.; Tan, S.S.-L.; Ngiam, K.Y.; Teo, H.H. Mobile health applications for older adults: A systematic review of interface and persuasive feature design. J. Am. Med. Inform. Assoc. 2021, 28, 2483–2501. [Google Scholar] [CrossRef]
- Amjad, A.; Kordel, P.; Fernandes, G. A review on innovation in healthcare sector (telehealth) through artificial intelligence. Sustainability 2023, 15, 6655. [Google Scholar] [CrossRef]
- Cabanillas-Carbonell, M.; Pérez-Martínez, J.; Yáñez, J.A. 5G technology in the digital transformation of healthcare, a systematic Review. Sustainability 2023, 15, 3178. [Google Scholar] [CrossRef]
- Creusen, M.E.; Schoormans, J.P. The different roles of product appearance in consumer choice. J. Prod. Innov. Manag. 2005, 22, 63–81. [Google Scholar] [CrossRef]
- Paul, J.; Criado, A.R. The art of writing literature review: What do we know and what do we need to know? Int. Bus. Rev. 2020, 29, 101717. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. Bmj 2021, 372, n160. [Google Scholar] [CrossRef]
- Pati, D.; Lorusso, L.N. How to write a systematic review of the literature. HERD Health Environ. Res. Des. J. 2018, 11, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.Y.; Wen, T.T.; Yue, S.Y.; Zhao, X.R.; Huang, K.K. The influence of health information attention and app usage frequency of older adults on persuasive strategies in mHealth education apps. Digit. Health 2023, 9, 16. [Google Scholar] [CrossRef]
- Choi, K.S.; Chan, S.H.; Ho, C.L.; Matejak, M. Development of a Healthcare Information System for Community Care of Older Adults and Evaluation of Its Acceptance and Usability. Digit. Health 2022, 8, 20552076221109083. [Google Scholar] [CrossRef]
- Arkkukangas, M.; Cederbom, S.; Tonkonogi, M.; Umb Carlsson, Õ. Older adults’ experiences with mHealth for fall prevention exercise: Usability and promotion of behavior change strategies. Physiother. Theory Pract. 2021, 37, 1346–1352. [Google Scholar] [CrossRef]
- Bergquist, R.; Vereijken, B.; Mellone, S.; Corzani, M.; Helbostad, J.L.; Taraldsen, K. App-based Self-administrable Clinical Tests of Physical Function: Development and Usability Study. JMIR Mhealth Uhealth 2020, 8, 11. [Google Scholar] [CrossRef]
- Alnanih, R.; Balabid, A.; Bahmdean, L. Senior-centered design for mobile medication adherence applications based on cognitive and technology attributes. Univers. Access Inf. Soc. 2024, 23, 871–888. [Google Scholar] [CrossRef]
- Cao, W.; Wang, J.; Wang, Y.; Hassan, I.I.; Kadir, A.A. mHealth App to improve medication adherence among older adult stroke survivors: Development and usability study. Digit. Health 2024, 10, 20552076241236291. [Google Scholar] [CrossRef] [PubMed]
- Eriksson-Backa, K.; Hirvonen, N.; Enwald, H.; Huvila, I. Enablers for and barriers to using My Kanta—A focus group study of older adults’ perceptions of the National Electronic Health Record in Finland. Inform. Health Soc. Care 2021, 46, 399–411. [Google Scholar] [CrossRef]
- Mao, J.Y.; Xie, L.L.; Zhao, Q.H.; Xiao, M.Z.; Tu, S.T.; Sun, W.J.; Zhou, T.T. Demand analysis of an intelligent medication administration system for older adults with chronic diseases based on the Kano model. Int. J. Nurs. Sci. 2022, 9, 63–70. [Google Scholar] [CrossRef]
- Murabito, J.M.; Faro, J.M.; Zhang, Y.K.; Demalia, A.; Hamel, A.; Agyapong, N.; Liu, H.S.; Schramm, E.; McManus, D.; Borrelli, B. Smartphone App Designed to Collect Health Information in Older Adults: Usability Study. Jmir Hum. Factors 2024, 11, 13. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, I.; Lee, S.; Yu, S. Information and Communication Technology-Based Application for Cognitive Behavioral Therapy among Community-Dwelling Older Adults with Insomnia: Development and Validation Study. Healthcare 2024, 12, 106. [Google Scholar] [CrossRef]
- Sien, S.W.; Kobekyaa, F.K.; Puts, M.; Currie, L.; Tompson, M.; Hedges, P.; McGrenere, J.; Mariano, C.; Haase, K.R. Tailored Self-Management App to Support Older Adults with Cancer and Multimorbidity: Development and Usability Testing. JMIR Aging 2024, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Song, J. An empirical investigation into the preferences of the elderly for user interface design in personal electronic health record systems. Front. Digit. Health 2023, 5, 1289904. [Google Scholar] [CrossRef]
- Aldekhyyel, R.N.; Almulhem, J.A.; Binkheder, S. Usability of Telemedicine Mobile Applications during COVID-19 in Saudi Arabia: A Heuristic Evaluation of Patient User Interfaces. Healthcare 2021, 9, 1574. [Google Scholar] [CrossRef]
- Ivankova, N.V.; Rogers, L.Q.; Herbey, I.I.; Martin, M.Y.; Pisu, M.; Pekmezi, D.; Thompson, L.; Schoenberger-Godwin, Y.M.M.; Oster, R.A.; Fontaine, K.; et al. Features That Middle-aged and Older Cancer Survivors Want in Web-Based Healthy Lifestyle Interventions: Qualitative Descriptive Study. JMIR Cancer 2021, 7, 16. [Google Scholar] [CrossRef]
- Nebeker, C.; Zlatar, Z.Z. Learning From Older Adults to Promote Independent Physical Activity Using Mobile Health (mHealth). Front. Public Health 2021, 9, 11. [Google Scholar] [CrossRef]
- Arkkukangas, M. App-based strength and balance self-test in older adults: An exploratory study from a user perspective. BMC Res. Notes 2021, 14, 379. [Google Scholar] [CrossRef] [PubMed]
- da Silva Sobrinho, A.C.; de Oliveira Gomes, G.A.; Bueno Júnior, C.R. Developing a Multiprofessional Mobile App to Enhance Health Habits in Older Adults: User-Centered Approach. JMIR Form. Res. 2024, 8, e54214. [Google Scholar] [CrossRef]
- Yeh, P.C. Impact of button position and touchscreen font size on healthcare device operation by older adults. Heliyon 2020, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Lee, S.H.; Cho, N.B.; You, H.; Choi, T.; Kim, J. User-Dependent Usability and Feasibility of a Swallowing Training mHealth App for Older Adults: Mixed Methods Pilot Study. JMIR Mhealth Uhealth 2020, 8, 16. [Google Scholar] [CrossRef] [PubMed]
- Khamaj, A.; Ali, A.M. Examining the usability and accessibility challenges in mobile health applications for older adults. Alex. Eng. J. 2024, 102, 179–191. [Google Scholar] [CrossRef]
- Shah, U.E.M.; Chiew, T.K.; Mehmood, Y. A Usability Evaluation Instrument for Pain Management Mobile Applications: An Elderly’s Perspective. Int. J. Hum. Comput. Interact. 2024, 40, 2265–2281. [Google Scholar] [CrossRef]
- Niemiec, S.L.S.; Wagas, R.; Vigen, C.L.P.; Blanchard, J.; Barber, S.J.; Schoenhals, A. Preliminary User Evaluation of a Physical Activity Smartphone App for Older Adults. Health Policy Technol. 2022, 11, 7. [Google Scholar] [CrossRef]
- Androutsou, T.; Kouris, I.; Anastasiou, A.; Pavlopoulos, S.; Mostajeran, F.; Bamiou, D.E.; Genna, G.J.; Costafreda, S.G.; Koutsouris, D. A Smartphone Application Designed to Engage the Elderly in Home-Based Rehabilitation. Front. Digit. Health 2020, 2, 13. [Google Scholar] [CrossRef]
- Tran-Nguyen, K.; Berger, C.; Bennett, R.; Wall, M.; Morin, S.N.; Rajabiyazdi, F. Mobile App Prototype in Older Adults for Postfracture Acute Pain Management: User-Centered Design Approach. JMIR Aging 2022, 5, e37772. [Google Scholar] [CrossRef]
- Vergouw, J.W.; Smits-Pelser, H.; Kars, M.C.; Van Houwelingen, T.; Van Os-Medendorp, H.; Kort, H.; Bleijenberg, N. Needs, barriers and facilitators of older adults towards eHealth in general practice: A qualitative study. Prim. Health Care Res. Dev. 2020, 21, e54. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, B.; Sabharwal, J.K.; Chawla, S. Old age or cognitive decline? Examining the usability of a mobile health app for older Australians. Inform. Health Soc. Care 2024, 49, 83–97. [Google Scholar] [CrossRef] [PubMed]
- Abujarad, F.; Ulrich, D.; Edwards, C.; Choo, E.; Pantalon, M.V.; Jubanyik, K.; Dziura, J.; D’Onofrio, G.; Gill, T.M. Development and usability evaluation of VOICES: A digital health tool to identify elder mistreatment. J. Am. Geriatr. Soc. 2021, 69, 1469–1478. [Google Scholar] [CrossRef] [PubMed]
- Felberbaum, Y.; Lanir, J.; Weiss, P.L. Designing Mobile Health Applications to Support Walking for Older Adults. Int. J. Environ. Res. Public Health 2023, 20, 3611. [Google Scholar] [CrossRef]
- Zhong, R.T.; Rau, P.L.P. A Mobile Phone-Based Gait Assessment App for the Elderly: Development and Evaluation. JMIR Mhealth Uhealth 2020, 8, 17. [Google Scholar] [CrossRef]
- Le, T.; Reeder, B.; Yoo, D.; Aziz, R.; Thompson, H.J.; Demiris, G. An Evaluation of Wellness Assessment Visualizations for Older Adults. Telemed. E-Health 2015, 21, 9–15. [Google Scholar] [CrossRef]
- Garvelink, M.M.; Agbadjé, T.T.; Freitas, A.; Bergeron, L.; Petitjean, T.; Dugas, M.; Blair, L.; Archambault, P.; Roy, N.; Jones, A.; et al. Improving a Web-Based Tool to Support Older Adults to Stay Independent at Home: Qualitative Study. JMIR Mhealth Uhealth 2020, 8, e16979. [Google Scholar] [CrossRef]
- Pan, J.; Dong, H. mHealth Adoption Among Older Chinese Adults: A Conceptual Model With Design Suggestions. Int. J. Hum. Comput. Interact. 2023, 39, 1072–1083. [Google Scholar] [CrossRef]
- Choi, S.; Chlebek, C.J. Exploring mHealth design opportunities for blind and visually impaired older users. Mhealth 2024, 10, 17. [Google Scholar] [CrossRef]
- Christiansen, L.; Lindberg, C.; Berglund, J.S.; Anderberg, P.; Skär, L. Using Mobile Health and the Impact on Health-Related Quality of Life: Perceptions of Older Adults with Cognitive Impairment. Int. J. Environ. Res. Public Health 2020, 17, 2650. [Google Scholar] [CrossRef]
- Choi, H.K.; Lee, K.; Lee, S.H. Developmental Study on “Smart Silver Care”: A Mobile Application to Alleviate Loneliness in Older Adults within the Community. Healthcare 2023, 11, 2376. [Google Scholar] [CrossRef] [PubMed]
- Mansson, L.; Wiklund, M.; Öhberg, F.; Danielsson, K.; Sandlund, M. Co-Creation with Older Adults to Improve User-Experience of a Smartphone Self-Test Application to Assess Balance Function. Int. J. Environ. Res. Public Health 2020, 17, 3768. [Google Scholar] [CrossRef] [PubMed]
- Aljedaani, K.; Alnanih, R. Grounded Theory for Designing Mobile User Interfaces-Based on Space Retrieval Therapy. Int. J. Interact. Mob. Technol. 2021, 15, 104–124. [Google Scholar] [CrossRef]
- Perotti, L.; Stamm, O.; Dietrich, M.; Buchem, I.; Müller-Werdan, U. The usability and user experience of an interactive e-learning platform to empower older adults when using electronic personal health records: An online intervention study. Univers. Access Inf. Soc. 2024, 16. [Google Scholar] [CrossRef]
- Cornet, V.P.; Toscos, T.; Bolchini, D.; Rohani Ghahari, R.; Ahmed, R.; Daley, C.; Mirro, M.J.; Holden, R.J. Untold Stories in User-Centered Design of Mobile Health: Practical Challenges and Strategies Learned From the Design and Evaluation of an App for Older Adults with Heart Failure. JMIR Mhealth Uhealth 2020, 8, e17703. [Google Scholar] [CrossRef]
- Nielsen, J. Enhancing the explanatory power of usability heuristics. In Proceedings of the SIGCHI conference on Human Factors in Computing Systems, Boston, MA, USA, 24–28 April 1994. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).