1. Introduction
Dysphagia—stemming from brain and nervous system disorders like stroke and Parkinson’s disease or from age-related changes in swallowing-related organs—needs early screening and intervention to mitigate the worsening of symptoms. Dysphagia occurs when an individual experiences difficulty in the swallowing process, which involves intricate muscle movements of various body parts within the respiratory and digestive systems, such as the mouth, pharynx, and esophagus, facilitating the transport of food from the mouth to the stomach [
1]. Impairment in swallowing-related muscle movements often leads to food stagnation or impediments in successful food transport into the stomach [
2,
3]. Dysphagia is frequently observed in patients with cranial nerve system disorders, including stroke (37–78%), Parkinson’s disease (52–90%), and Alzheimer’s disease (75–84%) [
4,
5,
6]. In addition, in the elderly population, age-related declines in swallowing-related muscle function contribute to dysphagia, affecting 15% to 33.7% of individuals over 65 years old [
7,
8]. Prolonged dysphagia poses serious complications, such as dehydration, malnutrition, and aspiration pneumonia, potentially leading to fatal outcomes. Therefore, early screening and proactive interventions are imperative to mitigate symptoms and prevent complications [
1].
Mobile swallowing healthcare services leveraging advancements in information and communication technology (ICT) have emerged to evaluate dysphagia and alleviate associated symptoms. Specifically, dysphagia-related applications have been developed to aid in the assessment and management of swallowing functions. For instance, Porfirione [
9] proposed the “Daily Dysphagia” (DayD) application, which is linked to wearable devices for real-time remote monitoring. This application enables medical practitioners to identify potential choking hazards in patients and respond accordingly. The DayD monitoring system tracks patients’ eating habits in real-time, collecting parameters such as dietary choices, motor skills, coughing frequency, oxygen saturation levels, and speech alterations during mealtime. Similarly, Constantinescu et al. [
10] utilized surface electromyography (sEMG) to introduce the Mobile-T system, which connects a wearable device with an at-home swallowing training app. This system encourages patients to engage in self-training by facilitating recording and analysis of sEMG signals during gamified maneuver training.
An investigation of comprehensive service requirements and their importance across various stakeholders is needed to develop systematic swallowing healthcare services because previous studies are limited to examining individual service requirements for senior citizens, patients, and caregivers in swallowing healthcare. For instance, Brockbank et al. [
11] investigated the views on pretreatment information among 24 patients with dysphagia. Govender et al. [
12] examined the acceptability and engagement of video-animation on dysphagia among 13 patients with head and neck cancer. Nund et al. [
13] investigated the support needs of 12 caregivers of patients with dysphagia. Additionally, Shrestha et al. [
14] conducted a survey with 33 hospital employees to gather opinions on a hypertension and diabetes prevention program, illustrating the necessity of stakeholder engagement in various fields. Given that existing studies were limited in terms of subject group and investigation scope, it is necessary to understand the comprehensive requirements and their importance across diverse stakeholders to streamline the overall requirements for the future development of swallowing healthcare services.
This study endeavors to identify service requirements and their importance among different stakeholder groups through stakeholder surveys and interviews and to propose service features for the future development of comprehensive swallowing healthcare services that may be useful to various stakeholders. Survey-based interviews were conducted with healthy seniors, individuals at risk, patients, guardians, and medical professionals to understand the swallowing healthcare requirements of various stakeholders in a comprehensive manner. Subsequently, a questionnaire assessing the importance of each identified requirement was administered. Finally, key service features were prioritized for the development of mobile swallowing healthcare services in the future.
2. Methods
2.1. Participants
Participants were recruited from five groups (healthy seniors, individuals at risk, patients, guardians, and medical professionals) to identify the requirements of various stakeholders in swallowing healthcare services, as shown in
Table 1. The healthy, at-risk, and patient groups were categorized based on their risk of dysphagia and diagnostic status as those requiring swallowing healthcare services. The healthy group consisted of individuals aged 65 and above without swallowing problems, scoring less than 3 out of 40 on the 10-item Eating Assessment Tool (EAT-10) [
15]. The risk group was selected from patients with a history of cerebral nervous system disease who were diagnosed as not having dysphagia. The patient group comprised patients diagnosed with dysphagia due to cerebral nervous system disease. The guardian group was recruited from families or caregivers of patients with dysphagia. Lastly, the medical professional group included rehabilitation medicine doctors, speech therapists, and occupational therapists. A total of 35 participants were recruited for the stakeholder groups for a survey of identifying requirements in swallowing healthcare services, and 125 participants were recruited for a separate survey of evaluating the importance of each identified requirement. Participants for individuals at risk, guardians, and patients were recruited with the help of hospital staff at a participating hospital, while those of healthy seniors were recruited at senior citizen centers and through the distribution of flyers.
2.2. Apparatus
A requirement survey questionnaire was developed to identify stakeholders’ inconveniences and wishes in existing swallowing healthcare services. It was tailored to investigate requirements in each of the three stages of swallowing healthcare: prevention/screening, evaluation/diagnosis, and treatment/training. Questions for each stage were formulated through discussions among four experts in rehabilitation medicine, language pathology, social welfare, and ergonomics, focusing on the general procedure of swallowing healthcare services experienced by healthy seniors, individuals at risk, and patients with dysphagia.
Subsequently, an importance evaluation questionnaire was prepared to examine the perceived importance of 46 requirements identified from the needs survey. This importance questionnaire consisted of three parts: prevention/screening (16 requirements), evaluation/diagnosis (12 requirements), and treatment/training (18 requirements). Participants were provided with an importance questionnaire containing relevant questionnaire parts based on their group type. As shown in
Table 2, the importance evaluation of prevention/screening service requirements was performed for heathy seniors, individuals at risk, and medical professionals, while the importance evaluations of evaluation/diagnosis and treatment/training service requirements were assessed for patients, guardians, and medical professionals. The importance of requirements was assessed using a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree).
2.3. Procedure
A survey was conducted to identify requirements for swallowing healthcare services in three stages: (1) introduction, (2) interview, and (3) debriefing. In the introduction stage, participants received a general overview of the survey and submitted a signed consent form for the study. During the interview stage, participants first completed a questionnaire designed to investigate the requirements in swallowing healthcare services. One-on-one interviews were administered for healthy seniors, individuals at risk, patients, guardians, and doctors, while group interviews were conducted for therapists. Finally, in the debriefing stage, supplementary feedback on the questionnaire responses was collected. The entire needs survey took about one hour to administer.
To evaluate the importance of each identified swallowing healthcare requirement, a telephone, web survey, or in-person survey was conducted in consideration of participants’ accessibility and survey efficiency. Healthy seniors and medical experts used the web survey; however, participants unfamiliar with the web survey responded via telephone. Individuals at risk, patients, and guardians participated in the in-person survey with the assistance of healthcare professionals. The importance survey took about half an hour to complete. The present study was approved by the Institutional Review Board (IRB) of the Pohang University of Science and Technology (PIRB-2019-E022) and Pohang Stroke and Spine Hospital (IRB no. PSSH0475-202006-HR-008-04).
2.4. Analysis
A hierarchical structural analysis of the needs survey results was performed to identify the overall requirements for swallowing healthcare services. Initially, ergonomic experts reviewed the identified requirements, merging similar and overlapping requirements into unified representative requirements. The service requirements were then classified into three stages according to the healthcare service flow: prevention/screening, evaluation/diagnosis, and treatment/training. These derived service requirements underwent cross-checking and refinement by four experts in speech pathology, social welfare, and ergonomics.
For a comparative analysis of the importance of requirements by stakeholder group, the Kruskal Wallis test was conducted at α = 0.05 using SPSS v. 18.0 (International Business Machines Inc., Armonk, NY, USA). The average importance scores were categorized as high, moderate, or low, allowing for a comprehensive understanding of the varying degrees of importance attributed to each requirement. Criteria for importance classification were set to “High” for requirements scoring 6 points or above, “Moderate” for those scoring between 4 and 6 points, and “Low” for those scoring below 4 points. Homogeneity in the importance of requirements across stakeholder groups was assessed using the Kruskal–Wallis test.
3. Results
3.1. Requirements for Swallowing Health Services
As shown in
Appendix A, a total of 46 requirements concerning prevention/screening, evaluation/diagnosis, and treatment/training were identified through the needs survey for swallowing health services. As for the requirements related to prevention/screening, 16 items were identified, encompassing accessibility, customization, usability, practicality, engagement, information, feedback, and psychosocial support. Detailed requirements include services easily accessible in daily life, customized services according to swallowing health status, self-management services, reasonable test time and cost, incorporation of game elements, guidance on how to act in case of risk of dysphagia, analysis of pre- and post-training changes, and professional support for psychosocial issues.
For evaluation/diagnosis requirements, 12 items were identified, encompassing accessibility, safety, customization, usability, practicality, information, and communication. Exemplar requirements include the need for an easily accessible dysphagia evaluation system, safe examination procedures, provision of diagnosis standards based on patient characteristics, user-friendly diagnostic system, reasonable examination time and cost, identification of aspiration and penetration, and effective information exchange among stakeholders.
Finally, as requirements for treatment/training, 18 items were identified, encompassing accessibility, safety, customization, usability, practicality, engagement, information, feedback, communication, and psychosocial support. Detailed items include services easily accessible in daily life, warning in case of danger during treatment, tailored treatment/training recommendations, user-friendly guides, reasonable treatment/training time and cost, incorporation of game elements, provision of useful information for patient management, real-time feedback during treatment, effective information exchange between stakeholders, and professional support for psychosocial issues.
3.2. Importance of Requirements for Swallowing Health Services
The importance of each requirement for swallowing health services was identified, as detailed in
Table 3,
Table 4 and
Table 5 through an analysis of stakeholder requirements’ importance. Across all stakeholder groups, the average response range regarding the importance of each requirement varied from 5.0 points (indicating slight agreement) to 6.6 points (indicating agreement). Notably, requirements related to evaluation/diagnosis were consistently rated as highly important, with scores ranging from 6.0 to 6.6. Similarly, requirements associated with treatment/training also received high importance ratings, ranging from 6.2 to 6.5. Conversely, requirements pertaining to prevention/screening were classified as having moderate importance, with scores ranging from 5.0 to 5.7.
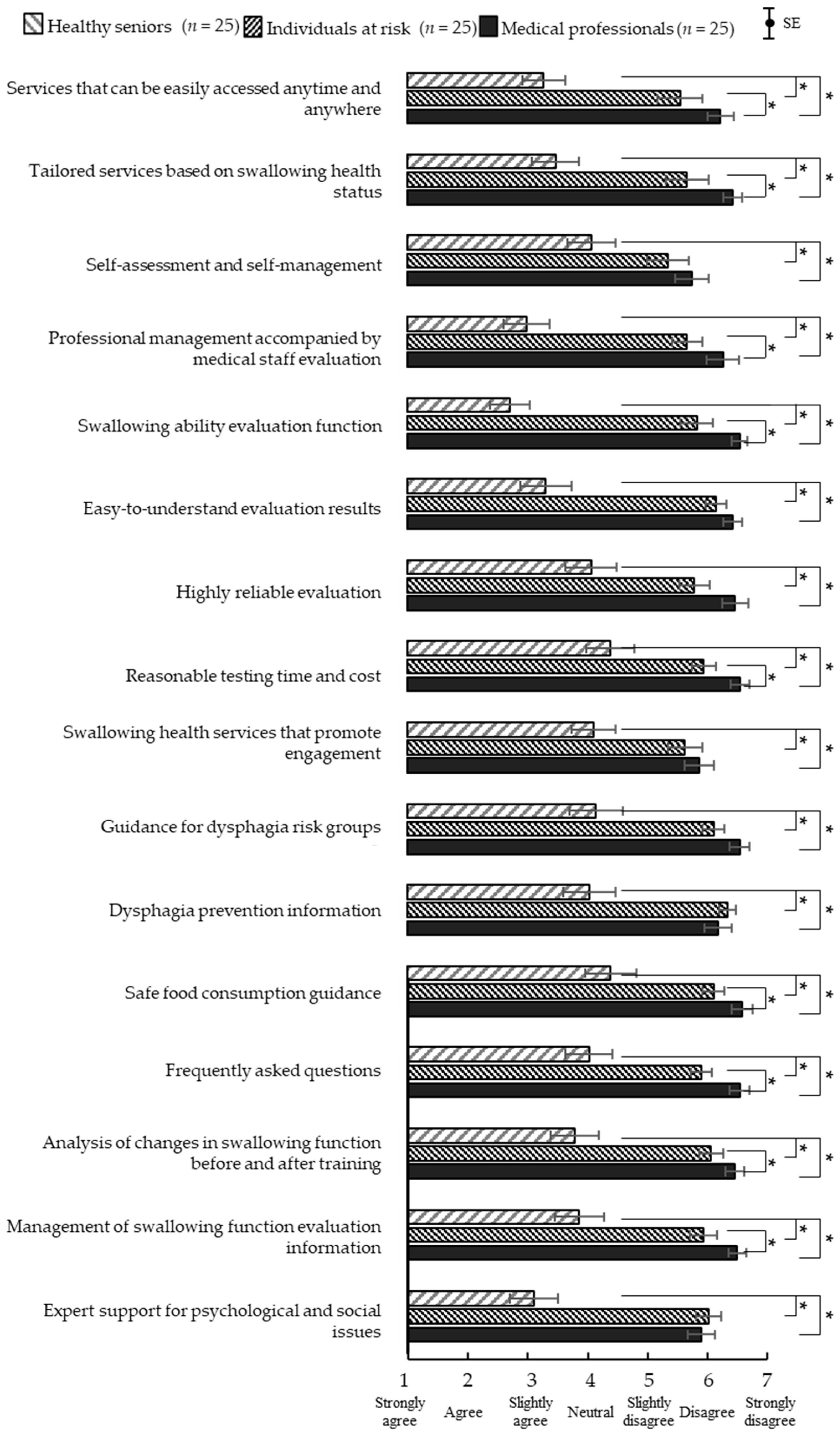
The analysis conducted for cross-group comparisons in the assessment of the importance of each swallowing healthcare requirement revealed significant differences in importance between stakeholder groups. For prevention/screening requirements, as shown in
Figure 1, the importance ratings were significantly higher (
p < 0.01) in the medical professional group (5.8–6.6) and the individuals at risk group (5.4–6.4) than the healthy senior group (2.7–4.4). Regarding evaluation/diagnosis requirements, as displayed in
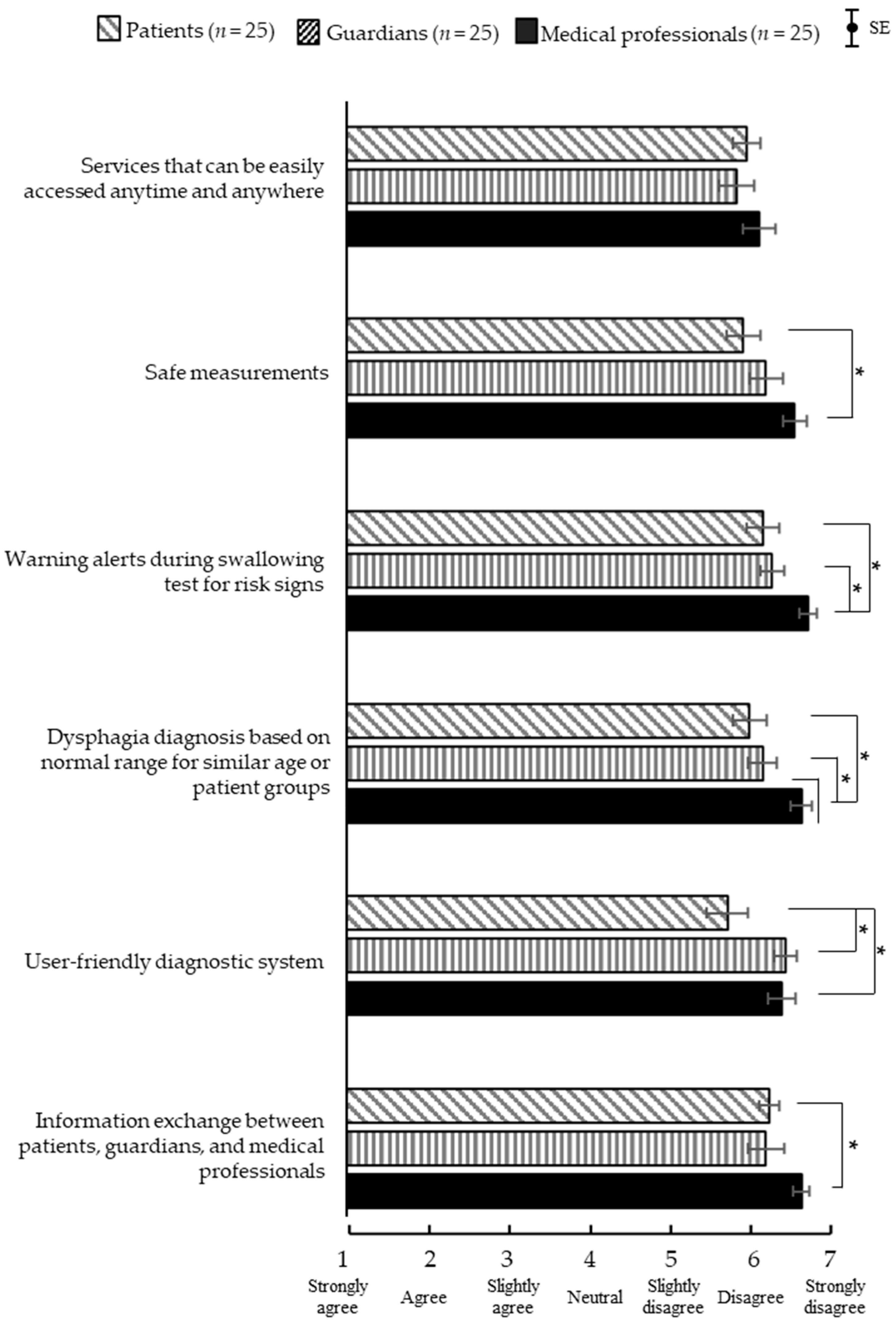
Figure 2, significant mean differences (
p < 0.05) were identified in the items of safe testing, warning alerts during swallowing tests, dysphagia diagnosis norms, and easy use of the dysphagia diagnosis system. Further analysis revealed that the importance of providing safe tests, warning alerts during swallowing tests, and provision of diagnosis standards for dysphagia was higher among the medical professional group (6.0–6.7) than in the patient group (5.9–6.2). However, the importance of the easy use of the dysphagia diagnosis system was higher in the guardian group (6.4) and the medical professional group (6.4) than in the patient group (5.7). Lastly, for treatment/training requirements, as depicted in
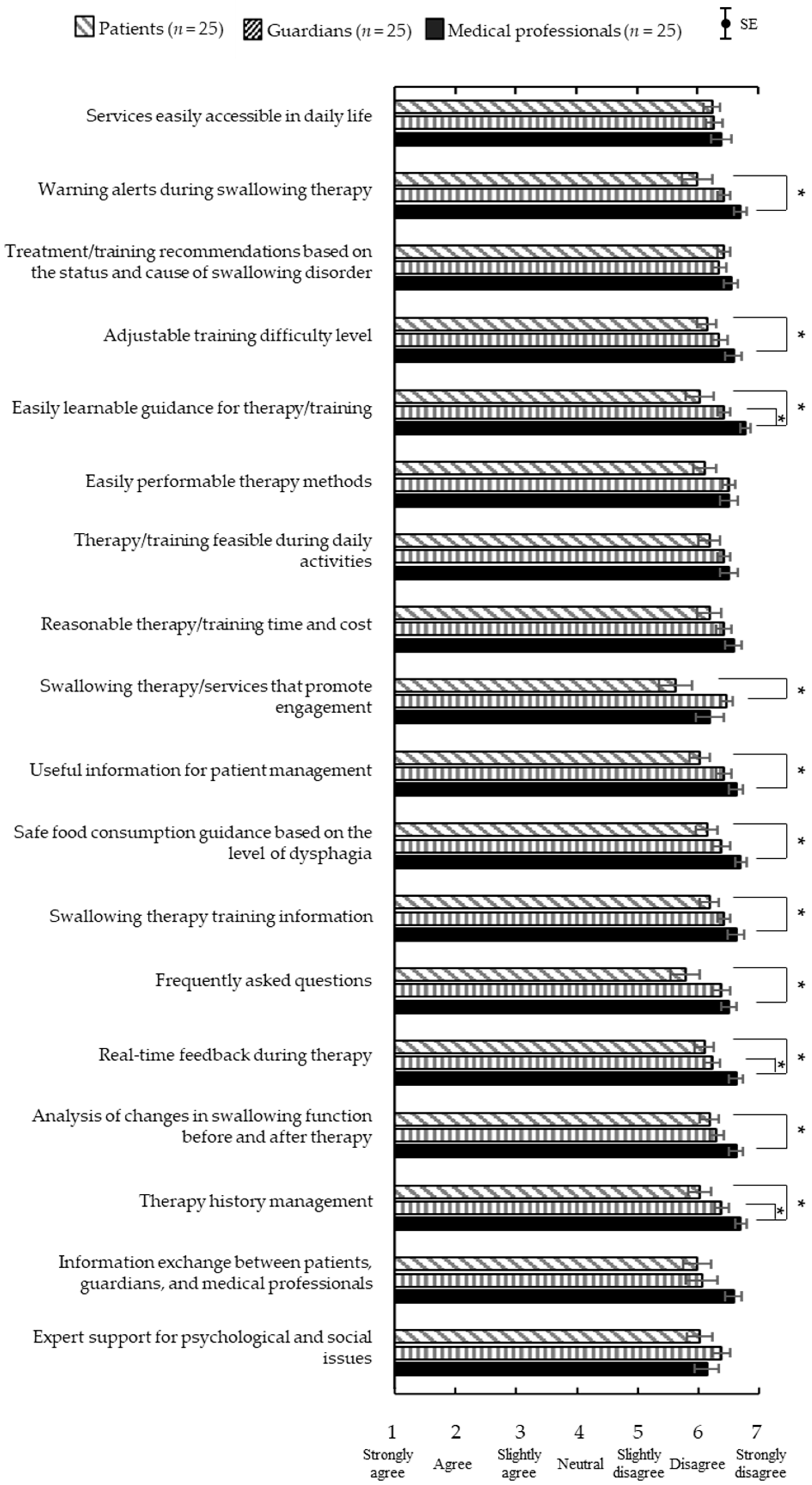
Figure 3, significant mean differences (
p < 0.05) were identified in the items of warning alerts in case of danger, treatment/training information, patient management information, guidance on safe food intake by the level of dysphagia, frequently asked questions, real-time feedback, treatment/training record management, and incorporation of game elements. Detailed analysis showed that the importance of warning alerts in case of danger, treatment/training guidance, patient management information, safe food intake guidance by the level of dysphagia, frequently asked questions, real-time feedback, and treatment/training records were significantly higher in the medical professional group (6.2~3.8) than in the patient group (5.6~6.2). Regarding the incorporation of game elements, the guardian group (6.5) rated them higher than the patient group (5.6).
4. Discussion
The present study presents a comprehensive investigation of the requirements of diverse stakeholders pertinent to the development of swallowing healthcare services, coupled with an evaluation of the importance attributed to each requirement. Existing research lacks a holistic understanding of the multifaced stakeholder requirements, because these studies have focused on investigating the needs of specific groups, such as the elderly, patients, and caregivers [
11,
12,
13]. In this study, the scope of service stakeholders, the requirements questionnaire, and survey methods and procedures were established through discussions with experts in rehabilitation medicine, speech pathology, social welfare, and ergonomics. Notably, this research constitutes an original attempt to discern the requirements of diverse stakeholders and evaluate the importance of each requirement via structured surveys. The resultant findings offer specific stakeholder requirements across three stages of the swallowing healthcare continuum: prevention/screening, evaluation/diagnosis, and treatment/training.
The identified requirements for evaluation/diagnosis and treatment/training entail the imperative for continuous examination and management of patients, which could serve as foundational elements for integration into self-care service features in healthcare service development. While self-management poses challenges for the elderly [
16], technological solutions, particularly mobile applications, offer promising avenues for facilitation. However, the presence of adherence issues among the elderly warrants comprehensive investigation. Among the four primary categories (cognition, motivation, physical function, and perception) influencing the usability of mobile health (mHealth) applications in the elderly, motivation emerges as paramount [
17]. The findings of this study underscore significant differences in the perceived importance of requirements for swallowing healthcare services among the stakeholder groups. For instance, healthy individuals tend to rate the overall necessity lower, while medical professionals assess the overall necessity as higher compared to patients. This can be interpreted as healthy individuals having fewer opportunities to use healthcare services [
18], and medical professionals possessing more information compared to patients [
19]. Consequently, based on these research findings, specialized swallowing training programs tailored to address the unique service requirements of patients and guardians may be envisaged for future investigation. Moreover, the stakeholder requirements identified from the present study hold potential applicability in the development of bespoke swallowing services, including customized rehabilitation or exercise programs tailored to accommodate variations in the severity of swallowing problems and the nutritional status of healthy seniors or patients with swallowing difficulties. In particular, the requirements in the aspects of evaluation/diagnosis and treatment/training all indicate high importance, suggesting they could serve as key service features.
Dysphagia healthcare programs aimed at addressing geriatric swallowing problems necessitate the integration of psychosocial services. The service requirements identified from the survey results indicate that a holistic approach encompassing both psychosocial support and direct swallowing treatment services is essential for effectively addressing swallowing issues. Previous research explored the relationship between dysphagia and the patients’ psychological wellbeing, highlighting the importance of offering psychosocial support. Studies have demonstrated a positive association between dysphagia and conditions such as depression and anxiety [
20,
21,
22], placing patients at an elevated risk of self-neglect [
23]. Moreover, Nguyen [
24] found that the severity of dysphagia was positively correlated with anxiety and depression, accentuating the importance of psychosocial interventions supplemented with informational support in dysphagia management. Furthermore, interventions addressing the psychological aspects of dysphagia have been introduced and proven efficacious. For instance, a support group led by speech pathologists showed an enhanced perceived quality of life by receiving both informational and psychosocial support [
25]. Consequently, the incorporation of psychological interventions into swallowing healthcare services is imperative to address patients’ psychological concerns effectively and foster motivation to engage in treatment.
This study has limitations, including a lack of the analysis on the reliability of the importance evaluation questionnaire and a possibility of participant recruitment not properly representing age and gender. Two types of questionnaires (requirement survey questionnaire and importance evaluation questionnaire) were used in the study. The construct and content validities of the questionnaires were supported because the questions were prepared through discussions among four experts in rehabilitation medicine, language pathology, social welfare, and ergonomics, focusing on the general procedure of swallowing healthcare services experienced by healthy seniors, individuals at risk, and patients with dysphagia. However, the reliability of the importance evaluation questionnaire was not examined in the study. Additionally, the majority of participants recruited were from older age groups without considering age distribution, and most therapists were female, leading to an absence of analysis on the effects due to gender and age. Consequently, future studies should recruit participants by differentiating between gender, age, and medical history and analyze the potential differences based on these factors to ensure a more systematic analysis of the results.
The present study requires supplementation in terms of regional and cultural diversity, given that the survey area was confined to Korea. The study encompassed swallowing healthcare recipients (including those in the healthy group, risk group, and patient group), their guardians, and medical professionals in Korea, thereby inherently reflecting the distinctive medical service environment and cultural attributes specific to Korea. Nonetheless, to provide effective healthcare services to patients from different ethnic or cultural backgrounds, it is crucial to implement appropriate adjustments that account for cultural disparities [
26,
27]. Individuals from different regional or cultural backgrounds may exhibit distinct service requirements and varying levels of importance for the same healthcare service requirements due to disparate perceptions of health and disease [
28,
29]. Therefore, when developing swallowing healthcare services intended for diverse geographic regions, further research is warranted to investigate the requirements among stakeholders from various regional and cultural backgrounds, thereby ensuring alignment with overseas service requirements.