1. Introduction
We are witnessing a growing demand from individuals seeking orthodontic treatment with the aspiration of achieving a beautiful smile. However, most of them are hesitant about extracting healthy teeth, especially premolars, or undergoing surgical procedures. It is crucial to be aware of the advantages and disadvantages of all methods so the doctor can select the best option for the patient. Different methods can have varying impacts on the profile, periodontium, position of incisors, smile, TMJ (temporomandibular joint) or the respiratory tract [
1,
2,
3,
4]. Therefore, it is essential to individualize the decision on the orthodontic treatment method, considering all these factors. The unique multifunctional characteristics of the new beta titanium alloy known as Gummetal make it nearly ideal for use in a new method of three-dimensional teeth movement, which is very similar to the MEAW method but easier, and more pleasant for the patient. It can help resolve discrepancies in some cases and is effective in closing anterior open bites or altering the occlusal plane to correct Class II or III malocclusions using tip-back bends, torque, and toe-in on Gummetal wires, along with the use of short elastics. This approach contributes to rebuilding the TMJ and to improving profile. However, it is important to be aware of the limitations of this method. Similar effects were observed over the years with the orthodontic MEAW technique [
5,
6]. However, the bends used in that technique are intricate, requiring extensive training for wire bending. Maintaining ideal oral hygiene is also challenging, and the procedure is less comfortable for the patient. The new Gummetal wires are an excellent material that can be used for three-dimensional control of teeth without the need for very complicated bends.
Just as the development of nickel–titanium wires marked the beginning of a new era in orthodontics about fifty years ago, nowadays it seems that the new beta titanium alloy called Gummetal is introducing new possibilities in orthodontic treatment.
Nickel–titanium (NiTi) wires possess superelasticity and the ability to retain a memory of a shape, but they cannot be easily bent. Consequently, they are mainly used in the initial stages of orthodontic treatment to nivelate the teeth, especially round ones with 0.016 inches diameter [
7]. However, their usage is limited in treating individuals with nickel allergies. Titanium–molybdenum alloy (TMA) wires are known for their high strength and springiness, making them excellent for auxiliary springs and finishing archwires, but they produce high friction between the archwire and the bracket [
7,
8,
9].
The unique characteristics of Gummetal make it suitable for treating the early stages of crowding with very low orthodontic force even when displacement is high. Due to very early torque control, the leveling time is shorter and the number of orthodontic visits is lower. Additionally, Gummetal helps to minimize pain by using the appropriate orthodontic force. Cleaning teeth with these wires is very easy for the patient. Orthodontists using them do not need to possess a masterful hand technique but can achieve precise three-dimensional control of teeth from the beginning of the treatment with an uncomplicated appliance [
8,
9,
10].
2. Materials and Methods
In the review of the relevant literature that qualified for our study, we conducted a search and included the publications from the PUBMED database, along with one position paper on the topic of Gummetal from the journal literature.
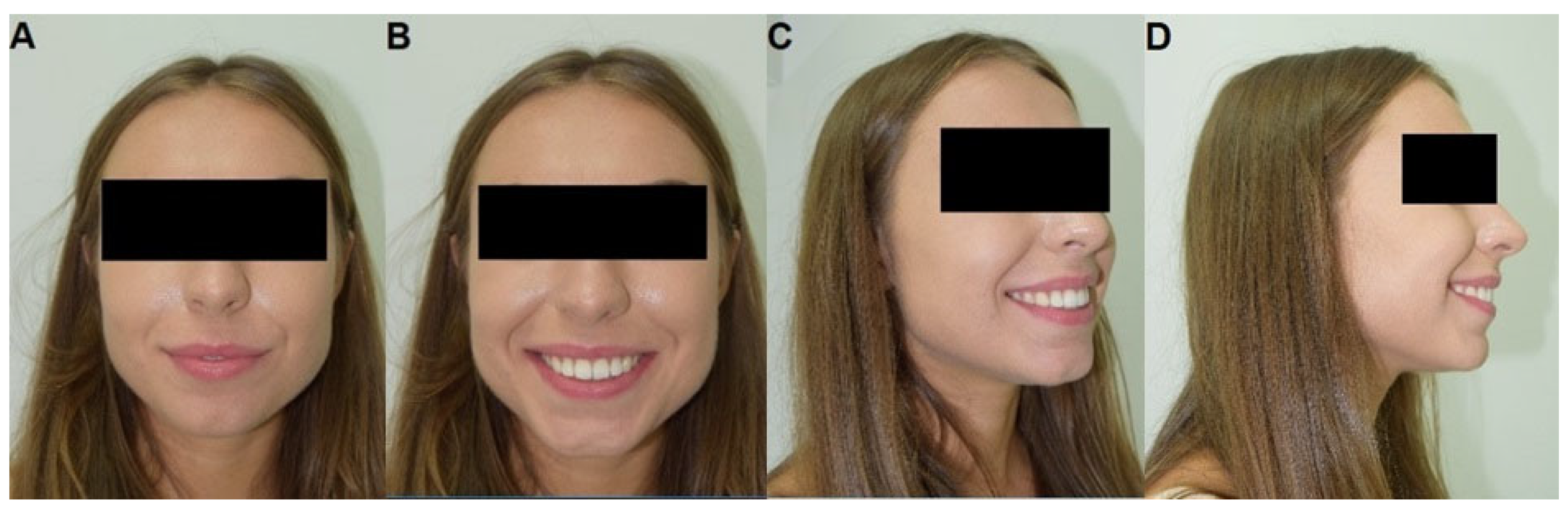
Case report: The patient sought an orthodontic consultation due to pain and clicking in the temporomandibular joint (TMJ) and a malocclusion. During the interview, she reported using a therapeutic splint for approximately a year, which successfully alleviated the symptoms. The patient had not undergone any orthodontic treatment before.
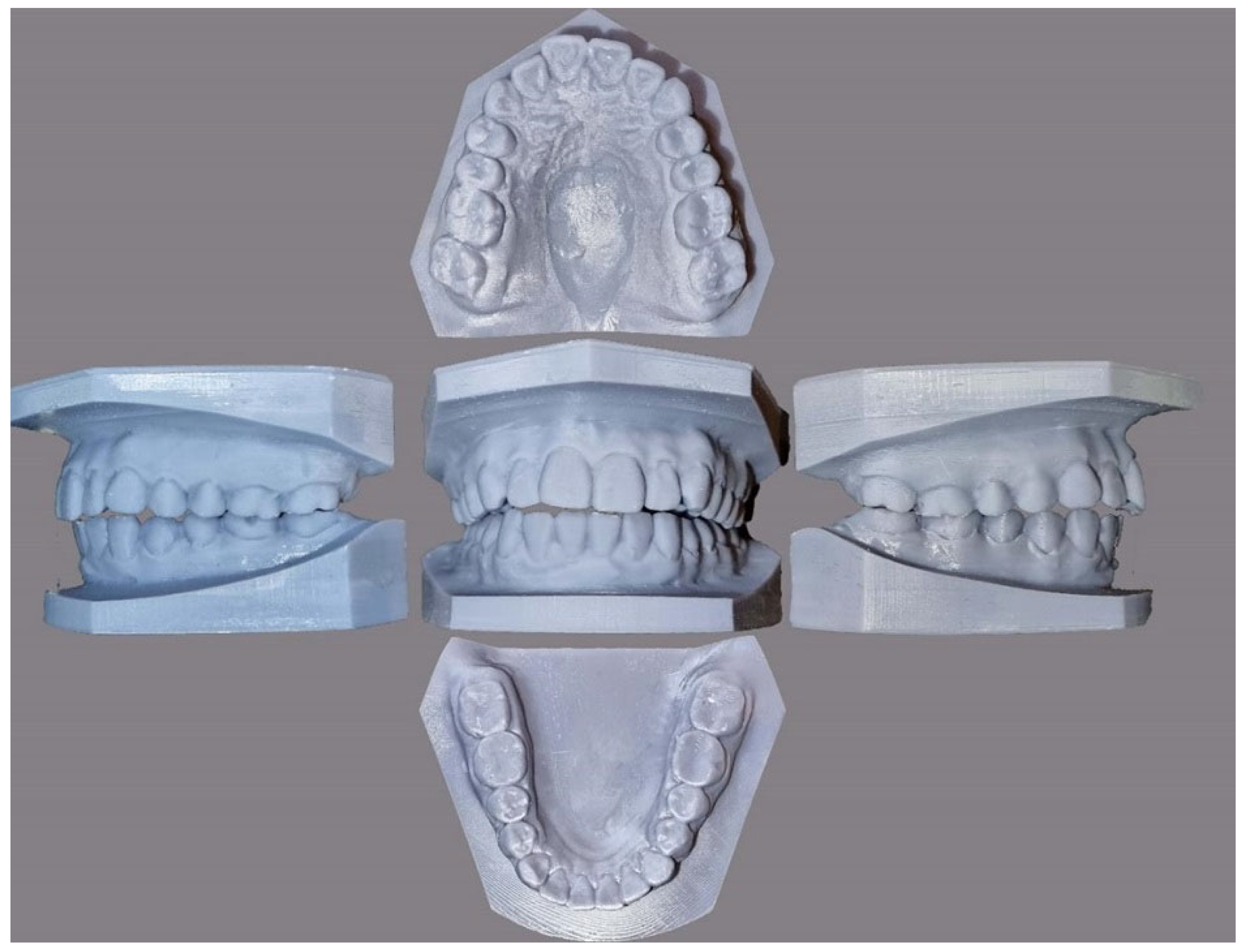
Extraoral and intraoral examination revealed an anterior open bite with minor crowding (
Figure 1 and
Figure 2). Functional evaluation indicated the absence of incisal and canine guidance and all mandibular movements resulted in traumatic nodes on the molars. Angle’s Class I relationship was present on both sides in the molars. However, the occlusal planes of the upper and lower arch were found to be divergent (
Figure 3).
All permanent teeth were visible in the panoramic image (
Figure 4). The patient had the eighth tooth extracted. The lateral telerentgenogram of the head before treatment and the results of the cephalometric analysis are shown in
Figure 5 and
Table 1.
The patient presented with a Class II skeletal defect (WITS = 2.1, ANB = 7.2) exhibiting an orthognathic facial type, a normal skull base angle, lower incisor protrusion, a reduced intermaxillary angle and a normal vertical intermaxillary relationship. The distance of the lower incisors from the Pogonion point was excessive (4.8 mm).
The treatment goal was to close the anterior open bite and achieve functional occlusion, including the establishment of incisal and canine guidance while eliminating occlusal trauma on the molars. In the sagittal dimension, there was a need to tilt the upper and lower incisors to achieve proper vertical and horizontal occlusion.
Upon reviewing the patient’s case history, it was recommended that she should be treated with traditional metal wired braces, utilizing appropriately contoured Gummetal (J. Morita Corp., Osaka, Japan) arches for the correction of plane rotation and occlusal closure.
Since both the maxillary and mandibular alveolar process were narrow, retraction of the incisors after extractions could result in contact with the palatal plate and incisive canal, causing undesirable side effects.
The patient accepted and understood the need to continuously wear the light elastics necessary for this treatment method.
After the initial leveling with 0.014, 0.018, and 0.017 × 0.025 NiTi archwires in both arches, the 0.018 × 0.025 Gummetal tip-backs were bent at about 60 degrees with an active progressive torque of about 45 degrees. The recommended treatment plan included 24/7 wearing of light 3/16 2.5 oz intermaxillary elastics in the anterior segment, intended to eliminate the intrusive effect of the arches on the anterior segment. There was a very rapid occlusal closure within 3 months (
Figure 6). The arches were then aligned with the simultaneous continuation of the elastics to verticalize the roots. In the final stage, straight TMA 0.019 × 0.025 arches were used to stabilize the occlusion. The treatment resulted in maximal intercuspation and functional occlusion. The patient did not report any TMJ complaints either during or after treatment.
The lateral telerentgenogram of the head, taken after the active phase of treatment, shows improvement in the inclinations of the lower incisors, the inter-incisal angle and rotation of the occlusal plane with verticalization and intrusion of the upper and lower molars (
Figure 7,
Table 2).
The final result (
Figure 8,
Figure 9 and
Figure 10) was satisfactory to the patient from both aesthetic and functional perspectives.
Physicochemical properties: X-ray Powder Diffraction (XRPD) technique was used to analyze the crystal structure of the materials by means of an X’Pert PRO X-ray diffractometer (Cu Kα1, 1.54060 Å) (Malvern Panalytical Ltd., Mavern, UK). The obtained patterns were analyzed by Match! software version 3.11.1.183 (Crystal Impact, Bonn, Germany). The energy dispersive spectroscopy (EDS) was performed on a FEI Nova NanoSEM 230 microscope equipped with an EDAX PegasusXM4 add-on (Hillsboro, OR, USA).
3. Results
Four companies took part in the development of Gummetal for orthodontic therapy with the primary role played by Professor Shin Hasegawa of Kanagawa Dental University in Japan.
According to Professor Shin Hasegawa [
10], Gummetal possesses the following characteristics:
- –
Possesses a very low modulus of elasticity—a Young’s modulus of approximately 40 GPa., providing high flexibility and superelasticity;
- –
Exhibits ductility approximately 10 times greater than that of conventional metals, making Gummetal superelastic and easy to bend and handle;
- –
Enables easy control of orthodontic force, as superelastic deformation represents true elastic deformation without hysteresis;
- –
Does not deform via a dislocation-free plastic deformation mechanism, and intraoral breakage is rare;
- –
Is biocompatible and non-toxic, being free of nickel;
- –
Has a low coefficient of friction, making it an excellent choice for the sliding mechanism of orthodontic tooth movement.
Murakami et al. compared three types of β-Titianium wires (TMA, Resolve, Gummetal) and found that Gummetal wire is characterized by the lowest bending strength, fatigue limit and elastic modulus. Furthermore, the resilience is the highest [
11].
In the research conducted by Schmeidl et al., Gummetal exhibited similar frictional resistance to cobalt–chromium and nickel–titanium archwires. When comparing the frictional properties of different alloys, Gummetal falls in between. It is superior to stainless steel alloy wire and inferior to titanium–molybdenum alloy wire [
12]. Considering its low friction, Kopsahilis et al. stated that Gummetal is a helpful addition in daily orthodontic practice [
13].
Another study revealed that the frictional resistance forces of Gummetal wire are comparable to stainless steel alloy wire and therefore useful in space closuring with sliding mechanics [
14].
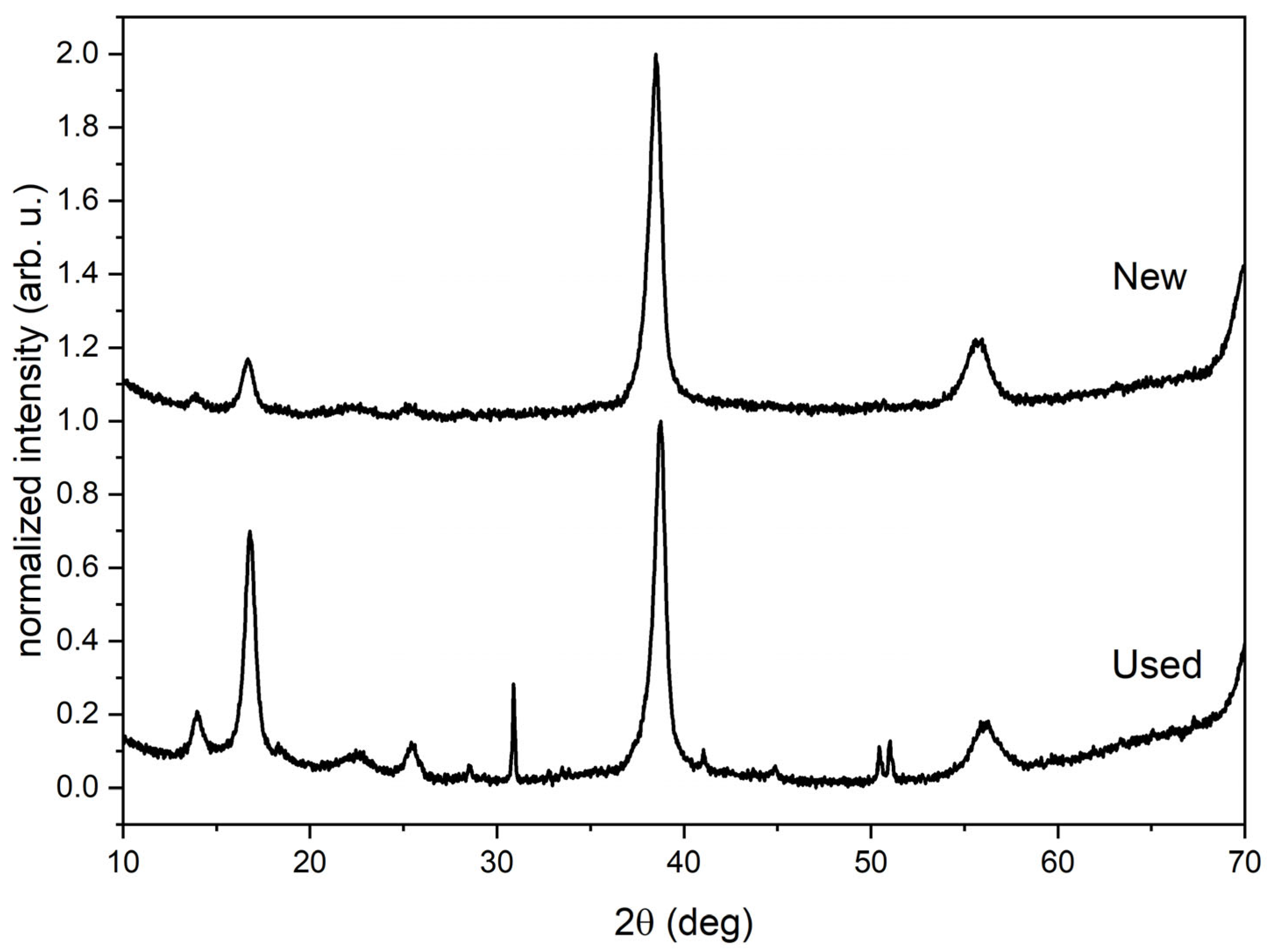
Some physicochemical properties of new and used Gummetal were studied by the X-ray powder diffraction and energy dispersive spectroscopy measurements. The XRD diagrams visible in
Figure 11 show that for the new Gummetal sample, only peaks from Ti, Nb, and Ta are visible (2θ = 38.5°, 55.7° and 70°), while for used Gummetal sample some additional peaks appear at 2θ = 30.8°, 41°, 44.8°, 50.4°, and 51°. These additional peaks are results of chemical processes which occur in the patient’s mouth.
According to the EDS measurements, the new Gummetal sample is composed of 62.5% of Ti, 31.5% of Nb, 3.6% of Zr, and 2.4% of Ta, while the used Gummetal sample is composed of 62.4% of Ti, 31.3% of Nb, 3.9% of Zr, and 2.4% of Ta. Additionally, elements such K, O, C, Cl, and P were discovered on the used Gummetal samples.
4. Discussion
An anterior open bite can be dental or skeletal and there is a difference between the occlusal planes in both types. Skeletal anterior open bite is mainly caused by the overgrowth of the posterior dental alveolar of maxilla in the molar region, while dental open anterior bite is due to two small dental alveolar in the anterior region [
15,
16,
17,
18]. The treatment of anterior open bite is challenging due to a very high relapse date and should relate to the etiology of the malocclusion. Bad habits such as tongue pressing, mouth breathing or thumb sucking [
19] can also be taken into account. Mouth breathing can produce long-face syndrome or adenoid facies and is often caused by allergy. Such patients may have a weak biting force and insufficient growth of the mandibular condyle.
This type of malocclusion is primarily treated by surgery or with camouflage, involving a change in the occlusal plane with the intrusion of the molar region and the extrusion of incisors. Camouflage treatment includes the use of Tads, the MEAW technique, high-pull headgear, teeth extractions, and now, the utilization of Gummetal wires to facilitate en-block teeth movement. With the introduction of TADs as an effective treatment modality, orthognathic surgery may be avoidable in selected anterior open bite cases [
20]. Additionally, TADs are one of the most effective methods for torque control during en-block incisor retraction [
21].
Young H. Kim could not find cephalometric evidence of any measurable reduction in the distance from the molars to the hard palate using high-pull headgear. He also notes that vertical elastics in the anterior region, which are used to close the bite by extruding the incisors, produced an unstable relationship, leading to common relapse of the teeth [
19].
According to studies by Koji Kojima during MEAW treatment, the results in the retrusion and extrusion of the maxillary incisors, the distal movement of the maxillary first molars, and the uprighting of the maxillary first premolars and the mandibular first molars were better in the group with the extraction of the second upper molar teeth than without extraction [
22].
In non-extraction treatment of anterior open bite using MEAW technique, the uprighting and retrusion of the premolars and molars and the extrusion, uprighting and retrusion of the incisors and canines played important roles [
23].
Analysis of the post-treatment and follow-up cephalometric radiographs proved that the treatment results obtained by this therapy were very stable [
24].
In camouflage treatment, the edges of the maxillary central incisors should serve as the guide for the anterior limit of the upper occlusal plane. Their position relative to the lip line must be at or near the 4 mm norm, as measured cephalometrically [
19]. We should identify whether the lower, upper, or both occlusal planes require correction.
Sometimes the extraction of second molars is necessary to eliminate the blocking effect. Additionally, the extraction of first molars has been prescribed for open bite treatment, but soon after such an extraction, the maxillary sinus descends and creates a cortical lining along the sinus surface [
19]. Therefore, if the first molars are healthy and not malformed, they should be preserved in the occlusion.
The MEAW technique is effective in the treatment of open bite but it is very difficult and requires professional and time-consuming bends.
The new Gummetal wires give us an easier way to upright inclined mesially teeth, extrude the incisors, and intrude the molars, ultimately closing the open bite. The new concept of en-block teeth movement by Hasegawa requires tip-back bends about of 60 degrees on both 0.018 × 0.022 or 0.018 × 0.025 arches, and the use of intermaxillary light elastics on the anterior teeth to oppose the intrusive force on this segment and prevent flareout. It is mandatory to bend an active progressive torque by about 45 degrees.
This uprighting of teeth rotates the mandible and closes the bite. After that, it should take two or three stages to partially straighten the wire to achieve an intercuspation. Hasegawa shows that the open bite temporarily worsened during the initial stage of the treatment, but in the active part, the bite closes. As he also demonstrates in his book, the treated cases with pre- and post-treatment panoramic radiograph and cephalogram show a slight closing rotation of the mandible, intrusion of the molars, and a changed inclination of the incisors. There seems to be no extrusion of the incisors. The change in incisor edges is only with their recline and with the overall rotation of the mandible [
10].
The easy and effective operation of that method may be due to the individual properties of Gummetal [
25,
26,
27]. Sabbagh et al. noticed that Gummetal archwire has similar behavior to a force plateau, but in contrast to Niti archwires, this plateau was located at very high force values. Additionally, they show hysteresis, which indicates a phase transformation in the material [
27].
Due to the great interest in aesthetic orthodontics, there is a demand for white archwires, which means they come with special aesthetic coatings. Zhou et al. has studied Gummetal wires with the application of epoxy, polytetrafluoroethylene, clear ceramic, white ceramic, and silicone. They showed that coated wires have lower frictional forces than uncoated stainless wires when they are used with ceramic braces, but the frictional forces are similar in coated and uncoated Gummetal and stainless wires with metal brackets. They also proved that coated Gummetal wires have good wear resistance after friction testing and provided corrosion resistance to low pH saliva [
28].
On the other hand, the comparison of sliding mechanics using stainless steel and Gummetal archwires showed no differences between either, and similar movement [
29]
The treatment has been completed without the use of miniscrews, thus avoiding risks of root injuries [
30], failure [
31], or fracture [
32].
The limitations of this publication mainly include a single clinical case as well as a follow-up period of only 12 months after treatment. It is important to take into account the individual conditions of the patient’s oral environment, which can modify the physicochemical properties of the orthodontic material in specific ways. Another limitation of the study is the use of a single time variable for XRD testing of the ‘overworked’ Gummetal samples. The physicochemical testing of the alloy was carried out only after six weeks of application in the oral cavity.
5. Conclusions
The decision regarding the method of orthodontic treatment should be made after very detailed diagnosis. It should depend on the manual skills of the orthodontist, because some methods require very precise bends on the wires. In some cases, orthognathic surgery can be replaced by camouflage treatment with very similiar effects and the new method of ‘en block’ movement of teeth using Gummetal wire seems to be quite an easy way to achieve a good occlusion. It is not manually complicated and not time-consuming.
However, this method requires good cooperation with the patient due to the necessity of using elastics throughout the day. According to Hasegawa, in cases of anterior open bite, the use of Gummetal wires can lead to good occlusion by changing the occlusion plane. The results of using this method on Hasegawa’s patients, as shown in his book, are promising, but more research should be conducted to ensure reliability. There are only a few publications in Japanese, making it impossible to draw conclusions based on them. There is also no research about the stability of such treatment. However, we can expect that the results should be similar to the research on the MEAW or GEAW technique due to a similar way of changing the occlusal plane but using easier bends.
Author Contributions
Conceptualization, A.E.K., J.K. and J.N.; methodology, J.K. and A.W.; software, A.E.K., J.N. and A.W.; validation, M.D., A.W. and R.J.W.; formal analysis, A.W.; investigation, J.K., J.N. and A.W.; resources, B.K.; data curation, A.W.; writing—original draft preparation, J.K., M.D., A.W. and M.S.; writing—review and editing, M.D., A.W. and R.J.W.; visualization, M.S., J.L. and B.K.; supervision, M.S., J.L. and B.K.; project administration, M.D. and R.J.W.; funding acquisition, M.D. and R.J.W. All authors have read and agreed to the published version of the manuscript.
Funding
The authors would like to acknowledge the National Science Centre Poland (NCN) for financial support within the Project ‘Biocompatible materials with theranostics’ properties for precision medical application’ (No. UMO-2021/43/B/ST5/02960).
Institutional Review Board Statement
This manuscript is a case report in which the patient cannot be identified, and therefore the requirement for obtaining informed consent from the patient was waived. The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from the patient involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
The authors would like to give thanks to Ewa Bukowska for XRD measurements and to Damian Szymanski for EDS measurements.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Raposo, R.; Peleteiro, B.; Paço, M.; Pinho, T. Orthodontic Camouflage versus Orthodontic-Orthognathic Surgical Treatment in Class II Malocclusion: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Surg. 2018, 47, 445–455. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Zhang, L.; Hu, M.; Huang, Y.; Li, W. Alveolar Bone Changes in Maxillary and Mandibular Anterior Teeth during Orthodontic Treatment: A Systematic Review and Meta-analysis. Orthod. Craniofacial Res. 2021, 24, 165–179. [Google Scholar] [CrossRef]
- Hu, Z.; Yin, X.; Liao, J.; Zhou, C.; Yang, Z.; Zou, S. The Effect of Teeth Extraction for Orthodontic Treatment on the Upper Airway: A Systematic Review. Sleep Breath. 2015, 19, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Leite, R.A.; Rodrigues, J.F.; Sakima, M.T.; Sakima, T. Relationship between Temporomandibular Disorders and Orthodontic Treatment: A Literature Review. Dent. Press J. Orthod. 2013, 18, 150–157. [Google Scholar] [CrossRef]
- Farahani, M.; Farimani, R.M.; Eskandarloo, F. Treatment for Severe Class II Open Bite Using a Bonded Hyrax Expander, IZC Mini-Implants, and MEAW Technique in an Adolescent Patient. Case Rep. Dent. 2023, 2023, 8833818. [Google Scholar] [CrossRef] [PubMed]
- Al-Saleh, M.A.Q.; Alsufyani, N.; Flores-Mir, C.; Nebbe, B.; Major, P.W. Changes in Temporomandibular Joint Morphology in Class II Patients Treated with Fixed Mandibular Repositioning and Evaluated through 3D Imaging: A Systematic Review. Orthod. Craniofacial Res. 2015, 18, 185–201. [Google Scholar] [CrossRef]
- Sarul, M.; Kawala, B.; Kawala, M.; Antoszewska-Smith, J. Do the NiTi Low and Constant Force Levels Remain Stable in Vivo? Eur. J. Orthod. 2015, 37, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.-P.; Tseng, Y.-C. A Novel β-Titanium Alloy Orthodontic Wire. Kaohsiung J. Med. Sci. 2018, 34, 202–206. [Google Scholar] [CrossRef] [PubMed]
- Schmeidl, K.; Janiszewska-Olszowska, J.; Grocholewicz, K. Clinical Features and Physical Properties of Gummetal Orthodontic Wire in Comparison with Dissimilar Archwires: A Critical Review. Biomed. Res. Int. 2021, 2021, 6611979. [Google Scholar] [CrossRef]
- Hasegawa, S. A Concept of “En Bloc” Movement of Teeth Using GUMMETAL Wire; Quintessence Publishing: Tokyo, Japan, 2014. [Google Scholar]
- Murakami, T.; Iijima, M.; Muguruma, T.; Yano, F.; Kawashima, I.; Mizoguchi, I. High-Cycle Fatigue Behavior of Beta-Titanium Orthodontic Wires. Dent. Mater. J. 2015, 34, 189–195. [Google Scholar] [CrossRef]
- Schmeidl, K.; Wieczorowski, M.; Grocholewicz, K.; Mendak, M.; Janiszewska-Olszowska, J. Frictional Properties of the TiNbTaZrO Orthodontic Wire-A Laboratory Comparison to Popular Archwires. Materials 2021, 14, 6233. [Google Scholar] [CrossRef] [PubMed]
- Kopsahilis, I.E.; Drescher, D. Friction Behavior of the Wire Material Gummetal®. J. Orofac. Orthop. 2022, 83, 59–72. [Google Scholar] [CrossRef] [PubMed]
- Albawardi, A.; Warunek, S.; Makowka, S.; Al-Jewair, T. Friction Forces Generated by Aesthetic Gummetal® (Ti-Nb) Orthodontic Archwires: A Comparative in Vitro Study. Int. Orthod. 2022, 20, 100683. [Google Scholar] [CrossRef]
- Ngan, P.; Fields, H.W. Open Bite: A Review of Etiology and Management. Pediatr. Dent. 1997, 19, 91–98. [Google Scholar] [PubMed]
- Schendel, S.A.; Eisenfeld, J.; Bell, W.H.; Epker, B.N.; Mishelevich, D.J. The Long Face Syndrome: Vertical Maxillary Excess. Am. J. Orthod. 1976, 70, 398–408. [Google Scholar] [CrossRef] [PubMed]
- Nanda, R. Esthetics and Biomechanics in Orthodontics: Second Edition; Elsevier Inc.: Amsterdam, The Netherlands, 2014; ISBN 9781455750856. [Google Scholar]
- Isaacson, J.R.; Isaacson, R.J.; Speidel, T.M.; Worms, F.W. Extreme Variation in Vertical Facial Growth and Associated Variation in Skeletal and Dental Relations. Angle Orthod. 1971, 41, 219–229. [Google Scholar] [PubMed]
- Kim, Y.H. Anterior Openbite and Its Treatment with Multiloop Edgewise Archwire. Angle Orthod. 1987, 57, 290–321. [Google Scholar] [PubMed]
- Reichert, I.; Figel, P.; Winchester, L. Orthodontic Treatment of Anterior Open Bite: A Review Article—Is Surgery Always Necessary? Oral Maxillofac. Surg. 2014, 18, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Kuc, A.E.; Kotuła, J.; Nahajowski, M.; Warnecki, M.; Lis, J.; Amm, E.; Kawala, B.; Sarul, M. Methods of Anterior Torque Control during Retraction: A Systematic Review. Diagnostics 2022, 12, 1611. [Google Scholar] [CrossRef]
- Kojima, K.; Endo, T.; Shimooka, S. Effects of Maxillary Second Molar Extraction on Dentofacial Morphology before and after Anterior Open-Bite Treatment: A Cephalometric Study. Odontology 2009, 97, 43–50. [Google Scholar] [CrossRef]
- Endo, T.; Kojima, K.; Kobayashi, Y.; Shimooka, S. Cephalometric Evaluation of Anterior Open-Bite Nonextraction Treatment, Using Multiloop Edgewise Archwire Therapy. Odontology 2006, 94, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Han, U.K.; Lim, D.D.; Serraon, M.L. Stability of Anterior Openbite Correction with Multiloop Edgewise Archwire Therapy: A Cephalometric Follow-up Study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Gordin, D.M.; Ion, R.; Vasilescu, C.; Drob, S.I.; Cimpean, A.; Gloriant, T. Potentiality of the “Gum Metal” Titanium-Based Alloy for Biomedical Applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 44, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Jácome, F.; Ramos, F.; Romero, G.; Zarta, A.; Pacheco, D.; Barrera, J. Stresses and Deformations in the Arch, Bracket and Dentoalveolarunit, Using Blue and Arches Elgiloy and Gummetal, with and Withoutelastic: Finite Element Analysis. J. Odont. Col. 2016, 9, 34–45. [Google Scholar]
- Sabbagh, H.; Janjic Rankovic, M.; Martin, D.; Mertmann, M.; Hötzel, L.; Wichelhaus, A. Load Deflection Characteristics of Orthodontic Gummetal® Wires in Comparison with Nickel-Titanium Wires: An In Vitro Study. Materials 2024, 17, 533. [Google Scholar] [CrossRef] [PubMed]
- Zhou, A.; Makowka, S.; Warunek, S.; Chen, M.-Y.; Al-Jewair, T. Effects of Various Coating Methods on the Mechanical, Physical, and Aesthetic Properties of GUMMETAL® Archwires: In Vitro Study. Int. Orthod. 2023, 21, 100753. [Google Scholar] [CrossRef] [PubMed]
- Ravlyk, L.; Warunek, S.; Covell, D., Jr.; Tanberg, W.; Al-Jewair, T. Comparison of GUMMETAL® and Stainless Steel Alloy during Canine Retraction: A Pilot Split-Mouth Randomized Controlled Trial. Int. Orthod. 2023, 21, 100810. [Google Scholar] [CrossRef] [PubMed]
- Montasser, M.A.; Scribante, A. Root Injury During Interradicular Insertion Is the Most Common Complication Associated with Orthodontic Miniscrews. J. Evid.-Based Dent. Pract. 2022, 22, 101688. [Google Scholar] [CrossRef] [PubMed]
- Xin, Y.; Wu, Y.; Chen, C.; Wang, C.; Zhao, L. Miniscrews for Orthodontic Anchorage: Analysis of Risk Factors Correlated with the Progressive Susceptibility to Failure. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e192–e202. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Gandini, P.; Alcozer, R.; Vallittu, P.K.; Scribante, A. Failure Load and Stress Analysis of Orthodontic Miniscrews with Different Transmucosal Collar Diameter. J. Mech. Behav. Biomed. Mater. 2018, 87, 132–137. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).